We are not always absolutely certain that what we see on MRI truly represents tissue injury, but there are consistent changes in the images of the olfactory bulbs in patients with coronavirus disease 2019 (COVID-19).
We understand the reason for Dr Alex Mamourian’s questions and confess that initially, we also had the same doubts that he expressed in his letter, when for the first time, we were faced with the images of olfactory bulb injuries in these patients with COVID-19. The question arises about whether these are artifacts or do they truly represent an abnormality in the olfactory bulbs? To make sure that the findings we were identifying in the olfactory bulbs of patients with COVID-19 were real and abnormal, we reviewed healthy olfactory pathway of subjects from our data base with pre- and/or postcontrast fat-suppression T1WI and STIR of the orbit MRIs performed before the COVID-19 pandemic. We compared them with our data base because we did not find any article in the literature describing the normal aspect of the olfactory bulbs in pre- and postcontrast fat-suppression T1WI or on STIR.
We would like to reply to Dr Alex Mamourian, pointing out that all considerations regarding the difficulty of analyzing the olfactory bulbs were noted in our article in the last paragraph, which discusses the limitations1 of our retrospective study during this terrible pandemic, which is still threatening humanity.
This region is difficult to analyze with fat-suppression T1WI because of the susceptibility artifacts in the interface with the air, and we spoke about these in the last paragraph of the Discussion in our article.1 These artifacts are generally well-recognized by an experienced radiologist. In fact, if one reviews the image in Fig 1 of our article (case 1)1 (referred to by Dr Mamourian as an artifact), it seems that it does not correspond to an artifact. It is unilateral, located in the left bulb, with well-defined margins (the susceptibility artifacts usually have ill-defined margins that vanish, and they are often bilateral). Another important argument against the possibility of an artifact is that besides being seen in pre- and postcontrast fat-suppression T1WI (where susceptibility artifacts often appear), it is also clearly identified on the STIR image; thus, it would seem that it corresponds to a real image. STIR is not a sequence that identifies this kind of artifact.2 Moreover, if you read the legend, you will see that we stated “probable”1 methemoglobin.
In the other 4 cases (Fig 2 of our article), the bulbs seemed to enhance on the postcontrast series, but because there were no precontrast series, the differential diagnosis would be made with the presence of methemoglobin (this is also very clear in the Materials and Methods).1
The cases in our retrospective study did not have any coronal FLAIR, FIESTA, or CISS images because the olfactory bulbs and anosmia were not the reason for the investigation by brain MR imaging.1 Thus, our study cannot be compared with the other studies about presence of edema or an increase of volume, and we also spoke about this in the introduction.1 However, one of our new cases was also investigated using a 3D-FLAIR sequence, allowing clear evidence of damage to the olfactory bulb, corresponding to the alterations observed in the pre- and postcontrast spoiled gradient recalled (SPGR) T1WI, definitively ruling out the possibility of an artifact, at least in this particular case (Figure).
FIGURE.
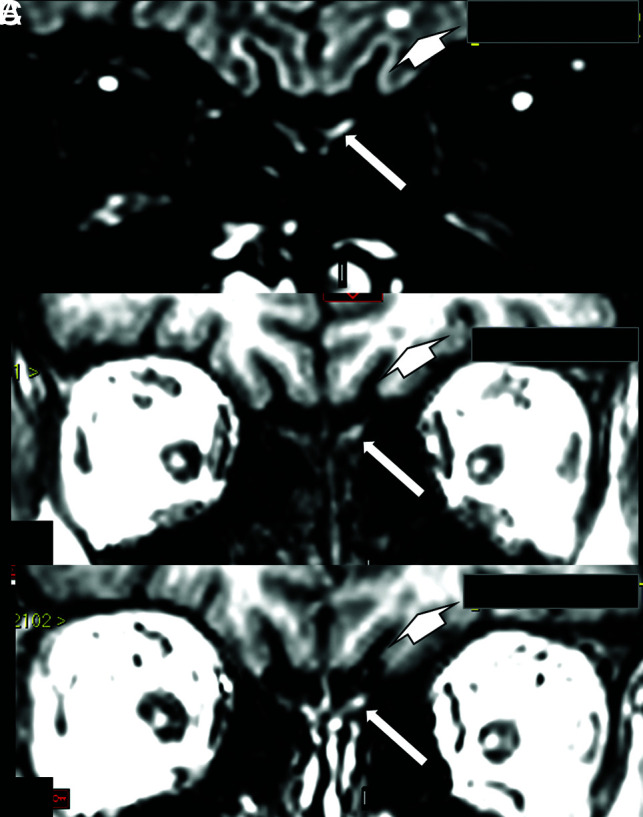
A woman in her 60s with confirmed COVID-19 for which MR imaging shows a hyperintense lesion on a coronal reconstruction of 3D-FLAIR (A, arrow) and also on pre- (B, arrow) and postcontrast SPGR T1WI (C, arrow). This is suggestive of a component of probably methemoglobin in this left olfactory bulb lesion, which seems to be a little larger and asymmetric compared with the apparently normal right olfactory bulb. This asymmetry is better seen on FLAIR. On FLAIR (A, short arrow), there is also a small round hyperintense lesion in the subcortical white matter in the left frontal lobe, which is hypointense on T1WI (B, short arrow) and does not enhance on postcontrast T1WI (C, short arrow), being no specific lesion area probably corresponding to gliosis. This patient also had some areas of brain parenchymal bleeding and microbleeding, and had around 50% of the bilateral pulmonary parenchyma compromised with typical COVID-19 lesions on chest CT, not shown in this figure.
Regarding another comment, the only case reported in our publication (case 5) that did not mention anosmia presenting on the MR imaging had suggestive enhancement only in the left olfactory bulb, which is also described in the Results.1 We also held a discussion about this and concluded (fourth paragraph), “The patient hardly perceives unilateral anosmia.”1 She probably had unilateral damage to the olfactory bulb that was not sufficient to clinically result in anosmia. The human olfactory pathway projects ipsilaterally to the brain, and the central processing of its information is initially also restricted to the same hemisphere. Later processing includes bilateral cortical activation.3 The clinical consequence of this is that unilateral olfactory deficits can remain asymptomatic and thus cannot be noticed. We did not use the olfactory test evaluation, only the patient's report, because our study was retrospective. However, even using smell tests measuring olfactory function mostly reflects the best side when testing bilaterally.
Unlike the pathologist who deals directly with the injured tissue, the radiologist tries to interpret on the image what may be happening in the tissue, evaluating a possible anatomofunctional correlation. Thus, it was not only in our study1 that a relationship between anosmia and apparent alteration of the MR image was observed in patients with COVID-19 even if other MR imaging sequences have been performed and analyzed.4–6 Our obligation is to present to the scientific community what we believe as an interpretation of a possible lesion demonstrated by the imaging. Obviously, we agree that there is always the risk of seeing what we want to see and not seeing what we do not want to see. Moreover, we have to always remember that in science, there are false-positives and false-negatives beyond the artifacts.
We think all would agree that anatomopathologic studies are necessary to better define neuroradiologic interpretation.
References
- 1.Aragão MF, Leal MC, Cartaxo Filho OQ, et al. Anosmia in COVID-19 associated with injury to the olfactory bulbs evident on MRI. AJNR Am J Neuroradiol 2020;41:1703–06 10.3174/ajnr.A6675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hong JH, Lee HY, Kang YH, et al. Improvement of fat suppression and artifact reduction using IDEAL technique in head and neck MRI at 3T. Investig Magn Reson Imaging 2016;20:44–52 10.13104/imri.2016.20.1.44 [DOI] [Google Scholar]
- 3.Lascano AM, Hummel T, Lacroix JS, et al. Spatio-temporal dynamics of olfactory processing in the human brain: an event-related source imaging study. Neuroscience 2010;167:700–08 10.1016/j.neuroscience.2010.02.013 [DOI] [PubMed] [Google Scholar]
- 4.Laurendon T, Radulesco T, Mugnier J, et al. Bilateral transient olfactory bulb edema during COVID-19-related anosmia. Neurology 2020;95:224–225 10.1212/WNL.0000000000009850 [DOI] [PubMed] [Google Scholar]
- 5.Chetrit A, Lechien JR, Ammar A, et al. Magnetic resonance imaging of COVID-19 anosmic patients reveals abnormalities of the olfactory bulb: preliminary prospective study. The Journal of Infection 2020. 10.1016/j.jinf.2020.07.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Strauss SB, Lantos JE, Heier LA, et al. Olfactory bulb signal abnormality in patients with COVID-19 who present with neurologic symptoms. American Journal of Neuroradiology 2020;41:1882–87 10.3174/ajnr.A6751 [DOI] [PMC free article] [PubMed] [Google Scholar]


