Abstract
Background.
Parental trust in their child’s health care provider and the number and type of vaccine information sources are important dimensions of vaccine hesitancy and may suggest intervention components for future research.
Method.
We conducted secondary analysis of survey data from mothers of healthy newborns in Washington State, and examined the association between parental trust in their child’s health care provider and vaccine information sources.
Results.
We found that mothers with less trust in their child’s health care provider used more sources, more informal sources, and were less likely to consider their child’s pediatrician their main source of vaccine information compared with more trusting mothers. However, less trusting mothers did not report more effort to read or watch stories about vaccines than more trusting mothers, nor were they more likely to report the internet as their main vaccine information source.
Conclusions.
Future interventions seeking to reduce parental vaccine hesitancy should consider intervention components focused on building or improving parent trust in their child’s health care provider.
Keywords: decision making, health beliefs, information sources, trust, vaccine hesitancy
Trust is an important component of parent-health provider relationships and can be defined as the “optimistic acceptance of a vulnerable situation in which [one] believes [another] will care for [one’s] interests” (Hall, Dugan, Zheng, & Mishra, 2001, p. 615). It has multiple dimensions, including fidelity, honesty, confidentiality, competence, and global trust, but tends to behave as a single construct (Hall et al., 2001). Trust plays a particularly critical role in parental vaccine decision making (Benin, Wisler-Scher, Colson, Shapiro, & Holmboe, 2006; Mills, Jadad, Ross, & Wilson, 2005). Parents who trust the vaccine information they receive from their child’s doctor and/or their health system generally accept vaccination for their child (Benin et al., 2006; Brown et al., 2012; Brunson, 2013; Dubé et al., 2016; Saada, Lieu, Morain, Zikmund-Fisher, & Wittenberg, 2015; Tickner, Leman, & Woodcock, 2007, 2010), and providers can play a key role in encouraging parents to follow the recommended vaccine schedule (Freed, Clark, Butchart, Singer, & Davis, 2011; Gust, Darling, Kennedy, & Schwartz, 2008; Kennedy, Lavail, Nowak, Basket, & Landry, 2011; McCauley, Kennedy, Basket, & Sheedy, 2012).
Although most parents trust their child’s doctor for vaccine information, a wide variety of other sources of vaccine information are also perceived as credible by many parents (Freed et al., 2011; Hilton, Petticrew, & Hunt, 2007). Use of nonphysician vaccine information sources, in turn, is associated with intentions to follow alternative vaccination schedules (Wheeler & Buttenheim, 2013). The number of and frequency in which parents who trust their child’s doctor use other vaccine information sources and how influential those vaccine information sources are on their vaccine decision making; however, is not well understood (Ames, Glenton, & Lewin, 2017).
In this study, we assess the association of a mother’s trust in their child’s health care provider and her use of alternative sources for vaccine information. We hypothesize the folowing:
Hypothesis 1: Mothers with lower levels of trust in their child’s health care provider will list more vaccine information sources compared with mothers with higher levels of trust.
Hypothesis 2: Mothers’ level of trust in their child’s health care provider will be associated with the type of vaccine information sources, with low trust associated with nonprovider vaccine information sources as a main source.
Method
Measures
We conducted a secondary analysis of baseline data collected in 2012 from mothers of healthy newborns at 47 clinics in Washington State as part of an intervention to address vaccine hesitancy (Henrikson et al., 2015). After obtaining verbal informed consent, surveys were conducted over the phone by trained interviewers using a standardized script 4 to 6 weeks after giving birth. Inclusion criteria were the following: age >18 years, English speaking, pregnancy more than 35 weeks of gestation, no medical complications related to birth, and intention to receive routine well-child care from a study clinic. This study was approved by the Kaiser Permanente Washington Region Institutional Review Board.
As part of the original study, participants were administered questions on demographics, vaccine hesitancy and vaccine information seeking. Maternal vaccine hesitancy was measured using the 15-item Parent Attitudes about Childhood Vaccines (PACV) survey (Opel et al., 2011). The PACV is scored from 0 to 100 (with 100 indicating high hesitancy), and we considered mothers who scored ≥50 to be hesitant and those who score <50 to be nonhesitant. This categorization is based on validation studies of the PACV in which parent vaccine behavior did not differ significantly from the referent group of parents who scored 0 to 49 on the PACV until a PACV score of 50, at which parents had significantly more under-immunized children than the referent group (Opel et al., 2013).
The three questions on vaccine information seeking were adapted from the 2011 National Immunization Survey (NIS; Centers for Disease Control and Prevention, 2011). Telephone interviewers prompted mothers with “I get vaccine information from …” and then gave them the chance to respond “yes” or “no” to the following options: “my child’s pediatrician,” “my family doctor,” “other medical doctors or specialists,” “a naturopathic doctor, homeopathic doctor, chiropractor, or acupuncturist,” “health care providers other than doctors,” “government agencies like the department of health or centers for disease control,” “the internet,” “TV, radio, books, and magazines,” “parents who believe their child was hurt by a vaccine,” “other parents,” “other friends and family,” and “any other sources of information about vaccines.” Free text responses in the “other” category were recoded by the study team as one of the listed sources. The interviewer read back to the respondent all of the sources of vaccine information she reported using and asked the mother to select one as her main source of vaccine information. In the third question, participants were asked to indicate their agreement with the statement “I make a point to read or watch stories about vaccines,” on a Likert-type scale from 0 (strongly agree) to 10 (strongly disagree). We dichotomized this response as scores of 6 and higher to those less than 6, based on the distribution of the data. However, we also analyzed this question using all 10 levels of the response. This did not change the significance of our results so we only report results using the dichotomized response.
Of four questions assessing trust, three were from the PACV and one was from the 2011 NIS (Centers for Disease Control and Prevention, 2011; Opel et al., 2011). Responses to the first two PACV questions (“Overall, I trust the information I receive about shots” and “I am able to openly discuss my concerns about shots with my child’s doctor”) were scored on a 5-point Likert-type scale from strongly agree to strongly disagree. Responses to the third PACV question (“All things considered, how much do you trust your child’s doctor?”) were scored from 0 to 10, with 0 representing do not trust at all and 10 representing completely trust. The question from the NIS (“In general, medical professionals in charge of vaccinations have my child’s best interests at heart”) also had answers on a 0 to 10 scale with 0 representing strongly disagree and 10 representing strongly agree. Since questions from the PACV were used to create the trust scale, we did not attempt to find an association between vaccine hesitancy and trust in physicians, or vaccine hesitancy and information sources.
We categorized race as self-reported White, Asian, Black, or other and ethnicity as Hispanic/non-Hispanic. Marital status was dichotomized into married or cohabitating with a partner versus single or divorced. We categorized level of education as college graduate or higher versus less than college graduate; annual household income as $75,000 or more and those earning less. We calculated the length of a mother’s relationship with her child’s doctor in months.
Analysis
Our primary predictor of interest for all analyses was maternal trust in her child’s pediatrician and in medical professionals. We assigned a numeric score to responses on the questions assessing trust, with a score of 0 for responses suggestive of high trust, a score of 1 for responses suggestive of intermediate trust, and a score of 2 for responses suggestive of low trust (Table 1). We then summed points from all four questions for each participant to create a scale ranging from 0, representing complete trust, to 8, representing low trust. Based on the distribution of the data, we dichotomized responses for analysis as 0 (trusting) and 1 through 8 (less trusting) for use as the primary predictor for all models. In a sensitivity analysis, we categorized mothers by quartiles on the trust scale to determine if our results changed. We found no change in the significance of our results so present only the results from trust as a dichotomized variable.
Table 1.
Numeric Score Assignments for Trust Scale.
| Survey question | Response assigned a score of 0 | Response assigned a score of 1 | Response assigned a score of 2 |
|---|---|---|---|
| Overall, I trust the information I receive about shots. | Agree, Strongly agree | Not sure | Disagree, strongly disagree |
| I am able to openly discuss my concerns about shots with my child’s doctor. | Agree, Strongly agree | Not sure | Disagree, strongly disagree |
| All things considered, how much do you trust your child’s doctor? | 8–10, 10 represents completely trust | 6, 7 | 0–5, 0 represents do not trust at all |
| In general, medical professionals in charge of vaccinations have my child’s best interests at heart. | 8–10, 10 represents strongly agree | 6, 7 | 0–5, 0 represents strongly disagree |
Note. Scores from all four questions were summed for each parent, to create a scale ranging from 0, representing high trust, to 8, representing low trust. The scale was then dichotomized such that scores of 0 were considered trusting and scores of 1 or higher were considered less trusting.
We tested for associations between our primary predictor and demographic covariates. We used chi-square analysis to test for differences in categorical variables and Fisher’s exact test for differences in race due to a small number of minority participants. A two-sample t test that allowed for unequal variances was used to test for differences on continuous variables between mothers grouped by level of trust. Associations between reported use of information source and trust level were assessed with chi-squared analysis.
The primary outcome for Hypothesis 1 was the total number of vaccine information sources. We used Poisson regression to assess the relationship between level of trust and the total number of vaccine information sources. The primary outcome of interest for Hypothesis 2 was citing “my child’s pediatrician” versus any other vaccine information source as a main source. Secondary outcomes were listing “the internet” versus any other main information source, and the dichotomized amount of effort a participant reported making to read or watch stories about vaccines. We used logistic regression to assess the association between trust in health care providers and main vaccine information source, as well as the association between trust and a pointed effort to seek information on vaccines.
For all analyses, we first ran unadjusted models to test for associations between trust and our outcomes and then assessed the independent association of trust and our outcomes using multivariable regression that controlled for covariates considered a priori to be potential confounders. These covariates included maternal age (Thom, Ribisl, Stewart, & Luke, 1999), level of education (Jones et al., 2012; Smith, Kennedy, Wooten, Gust, & Pickering, 2006), race and ethnicity (Voils et al., 2005), marital status (Voils et al., 2005), annual household income (Jones et al., 2012; Zheng, Hui, & Yang, 2017), number of children (Smith et al., 2006), and length of relationship with provider (Thom et al., 1999). Robust standard error estimates were used in all models. As a sensitivity analysis, we reran all analyses with the trust scale as a continuous predictor.
Finally, we conducted an exploratory analysis of patterns in the use of vaccine information sources. To do so, we first calculated pair-wise correlation coefficients between all 12 information source categories at the level of the individual. We then generated a matrix of these correlation coefficients to help visualize patterns.
Results
Sample Characteristics
We approached 700 mothers and enrolled 488 (69.7%). Of these, 391 (80.1%) completed the baseline survey and were included in our sample. The average age of respondents was 32 years, with 46% of the sample being a first-time parent (Table 2). Most parents (73%) had completed a college degree or higher, and 67% had an annual household income of $75,000 or higher. Mothers reported an average relationship of 28 months with their child’s doctor, with an interquartile range of 1 to 36 months. Nearly all the sample was married or cohabitating (90%), and 74% self-identified as White.
Table 2.
Descriptive Statistics of Women in Our Sample.
| Characteristic | Less Trusting (n = 134), n (%) | Trusting (n = 257), n (%) | Total (n = 391), n (%) |
|---|---|---|---|
| Maternal age (years) | |||
| <30 | 51 (38) | 62 (24) | 113 (29) |
| 30–34 | 41 (31) | 108 (42) | 149 (38) |
| ≥35 | 42 (31) | 87 (34) | 129 (33) |
| Marital statusa | |||
| Single/divorced | 16 (12) | 22 (9) | 38 (10) |
| Married/partnered | 118 (88) | 234 (91) | 352 (90) |
| No. of children, M (SD), range | 1.8 (1), 1–6 | 1.8 (1), 1–8 | 1.8 (1), 1–8 |
| First-time parent | 65 (49) | 116 (45) | 181 (46) |
| Educationa | |||
| <4-year college degree | 34 (25) | 71 (28) | 105 (27) |
| 4-year college or more | 100 (75) | 185 (72) | 285 (73) |
| Annual household incomea | |||
| <$75,000 | 45 (34) | 78 (31) | 123 (32) |
| ≥$75,000 | 86 (66) | 171 (69) | 257 (68) |
| Ethnicitya* | |||
| Non-Hispanic | 131 (98) | 236 (92) | 367 (94) |
| Hispanic | 3 (2) | 20 (8) | 23 (6) |
| Racea** | |||
| White | 88 (66) | 202 (79) | 290 (74) |
| Black/African American | 6 (4) | 5 (2) | 11 (3) |
| Asian | 27 (20) | 23 (9) | 50 (13) |
| Other/Mixed | 13 (10) | 27 (11) | 40 (10) |
| Duration of relationship with child’s doctora | |||
| < 1 month | 21 (16) | 41 (16) | 62 (16) |
| 1–12 months | 48 (37) | 84 (33) | 132 (34) |
| 1 to 5 years | 48 (37) | 85 (33) | 133 (35) |
| >5 years | 12 (9) | 46 (18) | 58 (15) |
| Vaccine hesitantb** | 35 (26) | 9 (4) | 44 (11) |
Note. Trusting reflects a score of 0 on the trust scale, and less trusting includes women with any non-zero score. Statistics are n (%) for categorical variables, and M (SD) min-max for continuous variables.
Information was missing for one participant on marital status, education, and ethnicity. Income information was missing from 11 individuals, and length of relationship with provider from 6.
Three of the four questions the trust scale was based on were items on the instrument used to assess vaccine hesitancy.
Difference between low- and high-trust mothers, p < .05 from chi-squared analysis for categorical variables, t test for continuous variables.
p < .01.
Survey Results
Most mothers (66%) were categorized as trusting by scoring a 0 on the trust scale. The remaining 34% were categorized as less trusting, with 17% scoring a 1, 11% scoring a 2, and 6% scoring 3 points or more. Demographic characteristics were similar between trusting and less trusting mothers (except for race and ethnicity, though cell sizes were small; Table 2).
The most common vaccine information source reported among both trusting and less trusting mothers was “my child’s pediatrician,” reported by 95% of women in both groups. Of the 21 women who reported an “other” source of vaccine information, 7 cited their own training as a health provider, and 5 mentioned research studies or peer-reviewed journals. Additional answers included insurance providers, the workplace, and newspapers. The most common main source of information reported was “my child’s pediatrician” for the entire sample (74%), followed by “the internet” (8%). No mothers reported “parents who believe their child was hurt by a vaccine” as their main vaccine information source. Forty-three percent (43%) of mothers reported making a strong effort to read or watch stories about vaccines.
Hypothesis 1: Mothers with lower levels of trust in their child’s health care provider will list more vaccine information sources compared with mothers with higher levels of trust.
Trusting mothers reported fewer average information sources than less trusting mothers (5.3 sources vs 5.9 sources, p < .01; Table 3). This difference persisted after adjusting for maternal age, level of education, race and ethnicity, marital status, annual household income, number of children, and length of relationship with provider (Table 4). Measuring trust on a continuous scale did not change outcomes significantly (not reported). The number of sources a mother reported using also increased with her level of education and number of children.
Hypothesis 2: Mothers’ level of trust in their child’s health care provider will be associated with the type of vaccine information sources, with low trust associated with nonprovider vaccine information sources as a main source.
Table 3.
Vaccine Information Seeking and Vaccine Information Sources (Survey Results).
| Variable | Less trusting (n = 134), n (%) | Trusting (n = 257), n (%) | Total (n = 391), n (%) | p |
|---|---|---|---|---|
| No. info sources, M (SD), range | 5.9 (2.1), 1–11 | 5.3 (2.1), 1–10 | 5.5 (2.1), 1–11 | <.05 |
| Makes a point to read or watch stories about vaccinesa | 57 (43) | 111 (43) | l68 (43) | .74 |
| Main information source | ||||
| Child’s pediatrician | 82 (61) | 206 (80) | 288 (74) | <.05 |
| Internet | 15 (11) | 17 (7) | 32 (8) | .09 |
| Friends and family | 5 (4) | 1 (<1) | 6 (2) | — |
| Other parents | 2 (1) | 0 (0) | 2 (1) | — |
| Government agency | 10 (7) | 6 (2) | 16 (4) | — |
| Media other than internet | 4 (3) | 7 (3) | 11 (3) | — |
| Family doctor | 10 (7) | 11 (4) | 21 (5) | — |
| Other doctor | 1 (1) | 3 (1) | 4 (1) | — |
| Parents of injured children | 0 (0) | 0 (0) | 0 (0) | — |
| Other health care provider | 1 (1) | 3 (1) | 4 (1) | — |
| Alt medicine provider | 3 (2) | 0 (0) | 3 (1) | — |
| Other | 1 (1) | 5 (2) | 6 (2) | — |
Note. Trusting reflects a score of 0 on the trust scale, and less trusting includes women with any nonzero score. p Values are from multivariable regression controlling for maternal age, level of education, race, ethnicity, marital status, annual household income, number of children, and length of relationship with provider.
One missing value.
Table 4.
Multivariable Estimates.
| Hypothesis 1 | Hypothesis 2 | |
|---|---|---|
| Characteristic | Incidence rate ratio [95% confidence interval] | Odds ratio [95% confidence interval] |
| Trust level | ||
| Less trusting | Referent | Referent |
| Trusting | 0.89 [0.82, 0.97]* | 2.47 [1.51, 4.04]* |
| Maternal age (1 year increment) | 1 [0.99, 1.0] | 0.96 [0.91, 1.02] |
| No. of children | 1.05 [1.00, 1.09]* | 1.18 [0.84, 1.66] |
| Marital status | ||
| Single or divorced | Referent | Referent |
| Married or partnered | 0.96 [0.80, 1.15] | 1.00 [0.38, 2.64] |
| Education | ||
| Less than 4-year college degree | Referent | Referent |
| 4-year college or more | 1.14 [1.02, 1.28]* | 1.10 [0.55, 2.19] |
| Annual household income | ||
| <$75,000 | Referent | Referent |
| ≥$75,000 | 0.98 [0.87, 1.04] | 1.40 [0.76, 2.58] |
| Ethnicity | ||
| Non-Hispanic | Referent | Referent |
| Hispanic | 0.98 [0.83, 1.16] | 0.40 [0.16, 1.03] |
| Race | ||
| White | Referent | Referent |
| Asian | 0.95 [0.85, 1.06] | 0.69 [0.34, 1.37] |
| Black | 1.02 [0.77, 1.37] | 3.37 [0.41, 27.59] |
| Mixed/other | 1.05 [0.92, 1.2] | 0.59 [0.26, 1.32] |
| Duration of relationship with doctor (months) | 1.0 [0.99, 1.0] | 1.0 [0.99, 1.0] |
Note. Characteristics associated with number of vaccine information sources used (Hypothesis 1) and listing child’s pediatrician as main vaccine information source (Hypothesis 2).
p < .05.
There was a higher proportion of less trusting (vs. trusting) mothers who reported the internet, other parents, parents of vaccine-injured children, other friends and family, and alternative medicine providers as sources of vaccine information (Figure 1). In multivariable analysis, a trusting mother had a 2.47 (95% confidence interval [1.51, 4.04], p < .05) increased odds of listing her child’s pediatrician as her main source of vaccine information as compared with a less trusting mother with a similar demographic background (Table 4). Results were similar between unadjusted and fully adjusted models. None of the demographic covariates were statistically significant.
Figure 1.
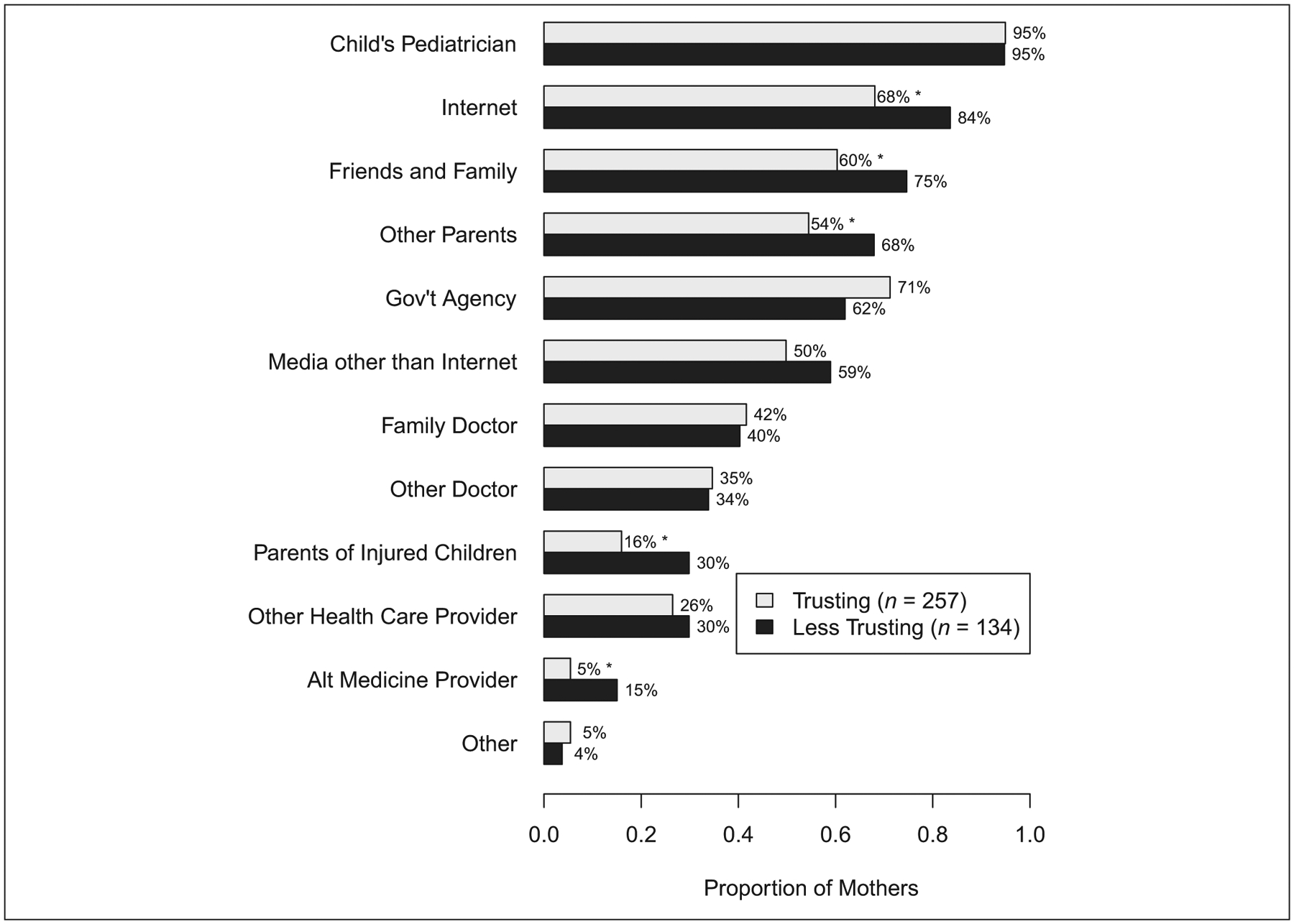
Use of vaccine information source by level of trust in child’s health care provider.
*Chi-square analysis showed a statistically significant difference (p < .05) for use of this vaccine information source between mothers with different levels of trust.
Trust was unrelated to reporting the internet as her main vaccine information source in either univariate or multivariable analyses. However, in the fully adjusted model, women of Hispanic origin had significantly increased odds of citing the internet as a main source and women who had a longer relationship with their child’s doctor had a significantly decreased odds of citing the internet as a main source. No Black mothers chose the internet as a main information source, so we were unable to estimate an association with race for this outcome.
Trust was not associated with reported behavior of making a point to read or watch stories about vaccines in either univariate or multivariable analyses. Reported effort did increase with the respondent’s number of children.
Exploratory Data Analysis
No clear patterns emerged in exploratory analysis of correlations between the types of vaccine information sources a participant reported using (see Supplemental Figure S1, available in the online version of this article). The majority (82%) of correlation coefficients fell between −0.1 and 0.1. Only two coefficients fell above 0.3, with use of “other parents” correlating with “friends and family” at 0.7, and “other parents” correlating with “parents who believe their child was hurt by a vaccine” at 0.4.
Discussion
We conducted a secondary analysis of survey data from mothers of healthy newborns in Washington State on their trust in physicians and vaccine information sources. We found that most parents reported their child’s pediatrician as their main source of vaccine information but less trusting (vs. trusting) mothers had both decreased odds of considering their child’s pediatrician as their main source of vaccine information and increased number of information sources used. These results are consistent with previous studies in which investigators have found pediatric providers as the most frequent (Kennedy, Basket, & Sheedy, 2011) or credible vaccine information source (Freed et al., 2011), yet parents who do not trust information conveyed by a provider are more likely to search for additional vaccine information (Austvoll-Dahlgren & Helseth, 2010). Though previous research has focused on vaccine information sources parents are using, and others have focused on trust in providers, this is the first to link trust in providers to vaccine information seeking.
Though we found a statistically significant difference in the number of vaccine information sources reported by trusting and less trusting mothers, numbers of sources cited was similar and may not reflect a meaningful difference. This, coupled with the lack of a difference we observed between trusting and less trusting mothers in their reported effort to read or watch stories on vaccines, suggests that vaccine information-seeking behavior may be similarly prevalent across groups. While most mothers seek out information on vaccines, the weight they give to different sources may vary with the amount of trust they place in those sources; future research should explore this in more detail. This is consistent with prior research suggesting that parental trust in a vaccine information source is potentially more important than the content of information that source provides (Guillaume & Bath, 2004).
Given the importance of trust to parental vaccine acceptance (Benin et al., 2006; Mills et al., 2005), an important implication of our findings is that future interventions explicitly address parental trust in their child’s provider, as well as understanding and measurement of parental vaccine information sources. However, it may be difficult to address parent-provider trust without also addressing institutional trust, as institutional and general interpersonal trust complement and influence patient-provider trust (Goold, 2001; Zheng et al., 2017). Similarly, distrust in the medical establishment coincides with distrust in the government and the pharmaceutical industry (Biss, 2015; Reich, 2016). Therefore, addressing vaccine hesitancy may require multilevel approaches to not only improve trust between parents and providers but also improve transparency and trust in vaccine development and delivery (Dubé, Gagnon, & MacDonald, 2015).
Limitations
Our study has several limitations. As a secondary analysis, the original measures were not designed to address these research questions, nor could we directly assess association between trust in health providers, vaccine information sources, and vaccine hesitancy as the questions in our trust scale were a subset of the ones used to assess hesitancy. One of the questions asked about overall trust in vaccine information, but not in health providers in particular. We performed a sensitivity analysis and removed six individuals who were classified as less trusting exclusively due to their response to that question. There was no significant change in results. Our sample had few participants at the least trusting levels of our scale, though this reflects the high levels of trust in physicians in the general population (Blendon, Benson, & Hero, 2014; Kennedy, Basket, et al., 2011). The small number of mothers with lower levels of trust led us to dichotomize the trust scale, so we were unable to distinguish any possible differences by gradation of trust. Our sample was predominantly White, high income, and highly educated, so these results may not be generalizable to fathers or other populations. Furthermore, our categories of vaccine information sources were not mutually exclusive and may have contributed to the lack of a significant difference by trust level for using the internet as a main source, as the Internet can be used to access a variety of materials. This is a limitation of many studies assessing vaccine information sources and should be modified in future research.
Finally, as this was a cross-sectional study, we cannot comment on directionality in our findings. While it is possible that a provider can build trust with new mothers while communicating about vaccine safety and efficacy, it may also be that a mother’s established trust in a health provider influences her perception of the vaccine information they provide; or her established beliefs influence her choice of pediatrician (Mergler et al., 2013; Reich, 2016). Longitudinal studies can provide insight into whether and how trust in health providers and vaccine information seeking may vary over time. However, 2-year follow-up of this same study cohort found a decline in vaccine hesitancy over time in both new and experienced mothers (Henrikson et al., 2017).
Implications
Future studies could explore which dimension of trust is especially relevant to interventions focused on vaccine information seeking and vaccine hesitancy. A review of interventions for improving patients’ trust in physicians found that only three randomized controlled trials had been conducted, with inconclusive results (McKinstry, Ashcroft, Car, Freeman, & Sheikh, 2006). As our study and others have reported greater reliance on alternative medicine providers among vaccine hesitant parents (Salmon et al., 2005; Smith, Marcuse, Seward, Zhao, & Orenstein, 2015), those providers may be a point of intervention. Although parent-provider relationships are likely to be key in decisions surrounding vaccination (Benin et al., 2006), since parents may find distrust in vaccine-manufacturing processes to be an issue, interventions to improve transparency and trust in the pharmaceutical industry and regulatory agencies may be needed to fully address public perceptions of vaccine safety.
Conclusions
We found that mothers with less trust in health providers report using more sources and more informal sources of vaccine information than mothers who trust health providers. Less trusting mothers are also less likely to report their child’s health provider as their main source of vaccine information than trusting mothers. We found no difference by trust level in use of the internet as a main information source or making an effort to read or watch stories about vaccines. Future research should focus on improving trust in health providers and the system that produces vaccines as a way to address vaccine hesitancy.
Supplementary Material
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Partial support for this research came from a Eunice Kennedy Shriver National Institute of Child Health and Human Development research infrastructure grant, R24 HD042828, as well as a Human Development training grant, T32 HD007543, to the Center for Studies in Demography & Ecology at the University of Washington. The parent study was supported by a grant from the Group Health Foundation.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental Figure S1 is available in the online version of this article at https://journals.sagepub.com/home/heb.
References
- Ames HM, Glenton C, & Lewin S (2017). Parents’ and informal caregivers’ views and experiences of communication about routine childhood vaccination: A synthesis of qualitative evidence. Cochrane Database Systematic Review, 2, CD011787. doi: 10.1002/14651858.CD011787.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austvoll-Dahlgren A, & Helseth S (2010). What informs parents’ decision-making about childhood vaccinations? Journal of Advanced Nursing, 66, 2421–2430. doi: 10.1111/j.1365-2648.2010.05403.x [DOI] [PubMed] [Google Scholar]
- Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, & Holmboe ES (2006). Qualitative analysis of mothers’ decision-making about vaccines for infants: The importance of trust. Pediatrics, 117, 1532–1541. doi: 10.1542/peds.2005-1728 [DOI] [PubMed] [Google Scholar]
- Biss E (2015). On immunity: An inoculation. Minneapolis, MN: Graywolf Press. [Google Scholar]
- Blendon RJ, Benson JM, & Hero JO (2014). Public trust in physicians: U.S. medicine in international perspective. New England Journal of Medicine, 371, 1570–1572. doi: 10.1056/NEJMp1407373 [DOI] [PubMed] [Google Scholar]
- Brown KF, Long SJ, Ramsay M, Hudson MJ, Green J, Vincent CA, … Sevdalis N (2012). U.K. parents’ decision-making about measles-mumps-rubella (MMR) vaccine 10 years after the MMR-autism controversy: A qualitative analysis. Vaccine, 30, 1855–1864. doi: 10.1016/j.vaccine.2011.12.127 [DOI] [PubMed] [Google Scholar]
- Brunson EK (2013). How parents make decisions about their children’s vaccinations. Vaccine, 31, 5466–5470. doi: 10.1016/j.vaccine.2013.08.104 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2011). National immunization survey. Retrieved from https://www.cdc.gov/nchs/nis/data_files.htm
- Dubé E, Gagnon D, & MacDonald NE (2015). Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine, 33, 4191–4203. doi: 10.1016/j.vaccine.2015.04.041 [DOI] [PubMed] [Google Scholar]
- Dubé E, Vivion M, Sauvageau C, Gagneur A, Gagnon R, & Guay M (2016). “Nature does things well, why should we interfere?”: Vaccine hesitancy among mothers. Qualitative Health Research, 26, 411–425. doi: 10.1177/1049732315573207 [DOI] [PubMed] [Google Scholar]
- Freed GL, Clark SJ, Butchart AT, Singer DC, & Davis MM (2011). Sources and perceived credibility of vaccine-safety information for parents. Pediatrics, 127(Suppl. 1), S107–S112. doi: 10.1542/peds.2010-1722P [DOI] [PubMed] [Google Scholar]
- Goold SD (2001). Trust and the ethics of health care institutions. Hastings Center Report, 31(6), 26–33. [PubMed] [Google Scholar]
- Guillaume LR, & Bath PA (2004). The impact of health scares on parents’ information needs and preferred information sources: A case study of the MMR vaccine scare. Health Informatics Journal, 10, 5–22. [Google Scholar]
- Gust DA, Darling N, Kennedy A, & Schwartz B (2008). Parents with doubts about vaccines: Which vaccines and reasons why. Pediatrics, 122, 718–725. doi: 10.1542/peds.2007-0538 [DOI] [PubMed] [Google Scholar]
- Hall MA, Dugan E, Zheng B, & Mishra AK (2001). Trust in physicians and medical institutions: What is it, can it be measured, and does it matter? Milbank Quarterly, 79, 613–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henrikson NB, Anderson ML, Opel DJ, Dunn J, Marcuse EK, & Grossman DC (2017). Longitudinal trends in vaccine hesitancy in a cohort of mothers surveyed in Washington State, 2013–2015. Public Health Report, 132, 451–454. doi: 10.1177/0033354917711175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henrikson NB, Opel DJ, Grothaus L, Nelson J, Scrol A, Dunn J, … Grossman DC (2015). Physician communication training and parental vaccine hesitancy: A randomized trial. Pediatrics, 136, 70–79. doi: 10.1542/peds.2014-3199 [DOI] [PubMed] [Google Scholar]
- Hilton S, Petticrew M, & Hunt K (2007). Parents’ champions vs. vested interests: Who do parents believe about MMR? A qualitative study. BMC Public Health, 7, 42. doi: 10.1186/1471-2458-7-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones AM, Omer SB, Bednarczyk RA, Halsey NA, Moulton LH, & Salmon DA (2012). Parents’ source of vaccine information and impact on vaccine attitudes, beliefs, and nonmedical exemptions. Advances of Preventive Medicine, 2012, 932741. doi: 10.1155/2012/932741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy A, Basket M, & Sheedy K (2011). Vaccine attitudes, concerns, and information sources reported by parents of young children: Results from the 2009 HealthStyles survey. Pediatrics, 127 (Suppl. 1), S92–S99. doi: 10.1542/peds.2010-1722N [DOI] [PubMed] [Google Scholar]
- Kennedy A, Lavail K, Nowak G, Basket M, & Landry S (2011). Confidence about vaccines in the United States: Understanding parents’ perceptions. Health Affairs, 30, 1151–1159. doi: 10.1377/hlthaff.2011.0396 [DOI] [PubMed] [Google Scholar]
- McCauley MM, Kennedy A, Basket M, & Sheedy K (2012). Exploring the choice to refuse or delay vaccines: A national survey of parents of 6- through 23-month-olds. Academic Pediatrics, 12, 375–383. doi: 10.1016/j.acap.2012.06.007 [DOI] [PubMed] [Google Scholar]
- McKinstry B, Ashcroft RE, Car J, Freeman GK, & Sheikh A (2006). Interventions for improving patients’ trust in doctors and groups of doctors. Cochrane Database Systematic Review, 3, CD004134. doi: 10.1002/14651858.CD004134.pub2 [DOI] [PubMed] [Google Scholar]
- Mergler MJ, Omer SB, Pan WK, Navar-Boggan AM, Orenstein W, Marcuse EK, … Salmon DA (2013). Association of vaccine-related attitudes and beliefs between parents and health care providers. Vaccine, 31, 4591–4595. doi: 10.1016/j.vaccine.2013.07.039 [DOI] [PubMed] [Google Scholar]
- Mills E, Jadad AR, Ross C, & Wilson K (2005). Systematic review of qualitative studies exploring parental beliefs and attitudes toward childhood vaccination identifies common barriers to vaccination. Journal of Clinical Epidemiology, 58, 1081–1088. [DOI] [PubMed] [Google Scholar]
- Opel DJ, Mangione-Smith R, Taylor JA, Korfiatis C, Wiese C, Catz S, & Martin DP (2011). Development of a survey to identify vaccine-hesitant parents: The parent attitudes about childhood vaccines survey. Human Vaccines, 7, 419–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opel DJ, Taylor JA, Zhou C, Catz S, Myaing M, & Mangione-Smith R (2013). The relationship between parent attitudes about childhood vaccines survey scores and future child immunization status: A validation study. JAMA Pediatrics, 167, 1065–1071. doi: 10.1001/jamapediatrics.2013.2483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reich JA (2016). Calling the shots: Why parents reject vaccines. New York: New York University Press. [Google Scholar]
- Saada A, Lieu TA, Morain SR, Zikmund-Fisher BJ, & Wittenberg E (2015). Parents’ choices and rationales for alternative vaccination schedules: A qualitative study. Clinical Pediatrics, 54, 236–243. doi: 10.1177/0009922814548838 [DOI] [PubMed] [Google Scholar]
- Salmon DA, Moulton LH, Omer SB, DeHart MP, Stokley S, & Halsey NA (2005). Factors associated with refusal of childhood vaccines among parents of school-aged children: A case-control study. Archives of Pediatrics & Adolescent Medicine, 159, 470–476. [DOI] [PubMed] [Google Scholar]
- Smith PJ, Kennedy AM, Wooten K, Gust DA, & Pickering LK (2006). Association between health care providers’ influence on parents who have concerns about vaccine safety and vaccination coverage. Pediatrics, 118, e1287–1292. [DOI] [PubMed] [Google Scholar]
- Smith PJ, Marcuse EK, Seward JF, Zhao Z, & Orenstein WA (2015). Children and adolescents unvaccinated against measles: Geographic clustering, parents’ beliefs, and missed opportunities. Public Health Report, 130, 485–504. doi: 10.1177/003335491513000512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thom DH, Ribisl KM, Stewart AL, & Luke DA (1999). Further validation and reliability testing of the Trust in Physician Scale. The Stanford Trust Study Physicians. Medical Care, 37, 510–517. [DOI] [PubMed] [Google Scholar]
- Tickner S, Leman PJ, & Woodcock A (2007). “It’s just the normal thing to do”: Exploring parental decision-making about the “five-in-one” vaccine. Vaccine, 25, 7399–7409. doi: 10.1016/j.vaccine.2007.08.008 [DOI] [PubMed] [Google Scholar]
- Tickner S, Leman PJ, & Woodcock A (2010). Parents’ views about pre-school immunization: An interview study in southern England. Child Care Health Development, 36, 190–197. doi: 10.1111/j.1365-2214.2009.01020.x [DOI] [PubMed] [Google Scholar]
- Voils CI, Oddone EZ, Weinfurt KP, Friedman JY, Schulman KA, & Bosworth HB (2005). Who trusts healthcare institutions? Results from a community-based sample. Ethnicity & Disease, 15, 97–103. [PubMed] [Google Scholar]
- Wheeler M, & Buttenheim AM (2013). Parental vaccine concerns, information source, and choice of alternative immunization schedules. Human Vaccines & Immunotherapeutics, 9, 1782–1789. doi: 10.4161/hv.25959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng S, Hui SF, & Yang Z (2017). Hospital trust or doctor trust? A fuzzy analysis of trust in the health care setting. Journal of Business Research, 78, 217–225. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


