Abstract
Background
Anterior Cruciate Ligament (ACL) injury prevention interventions have used trained experts to ensure quality feedback. Dyad (peer) feedback may be a more cost-effective method to deliver feedback to athletes.
Purpose
To determine the immediate effects of dyad versus expert feedback on drop landing kinematics and kinetics in female athletes.
Study Design
Cohort study
Setting
College gymnasium
Methods
Two teams (one female basketball and one female volleyball), from a local college, were team randomized to dyad feedback (volleyball team) or expert feedback (basketball team) (13 expert, 19±0.87years, 1.7±0.09m, 68.04±7.21kg) (10 dyad 19.4±1.07years, 1.73±0.08m, 72.18±11.23kg). Participants completed drop vertical jumps at two different time points (pre- and post-feedback). Knee flexion and abduction displacement were assessed with Inertial Measurement Units (IMUs) and vertical ground reaction force (vGRF) was assessed with a force plate during the landing phase of the drop vertical jump and compared across groups and condition (pre- and post-feedback) with a repeated measures ANCOVA a priori α <0.02 was set for multiple tests conducted.
Results
There were no significant differences between groups for flexion displacement. There was a significant change pre- to post- (decrease 4.65˚ p=0.01) in abduction displacement, with no group effect. There was a significant interaction of group by condition (p=0.01) for vGRF with no difference between groups before feedback (p>0.05). Between groups there was a decrease of vGRF in the expert group (difference 0.45 N*bw-1, p=0.01) at post-feedback relative to dyad. Within the expert group there was a significant difference between pre- and post-feedback (difference 0.72 N*bw-1, p=0.01), while the dyad group did not change pre- to post-feedback (difference 0.18 N*bw-1, p=0.67).
Conclusion
Movement screening experts giving real-time feedback were successful in improving key injury-risk kinematics and kinetics in female athletes, while dyad feedback only improved kinematics, indicating that expert feedback may be needed to ensure changes in kinematics and kinetics.
Level of Evidence
2
Keywords: movement system, expert feedback, dyad feedback, drop vertical jump
INTRODUCTION
Anterior cruciate ligament (ACL) rupture is a common activity-related knee injury that usually requires surgical reconstruction to restore knee stability and function. The lifetime burden of ACL injury costs the US over seven billion dollars.1–3 The typical mechanism of an ACL injury involves a non-contact mechanism resulting from an error in motor control leading to excessive knee valgus, and increased ground reaction forces.4–8 Females are a unique group at an exceptionally high risk of sustaining an ACL injury.8 Adolescent females who participate in sports that involve pivoting and jumping often sustain ACL injuries at 4-6 times higher rate than their male counter parts in the same sports.8–11 The cause of this higher incidence of ACL injury in females is due to several contributing factors such as anatomical, including greater Q angle, narrower femoral notch and increased laxity,8,12 hormonal changes in ligament laxity8 and biomechanical in terms of neuromuscular control differences. The long-term outcomes of ACL injury are poor with high recurrence rates and osteoarthritis.2 While recent debate is ongoing regarding the nature of specific mechanics relation to injury risk, interventions targeting these risk factors do improve neuromuscular control and reduce injury risk.13–15 Thus, prevention is a priority especially in the higher risk female athlete and while ACL injury prevention programs are effective, compliance and widespread adoption are low as typically expert trainers or clinicians are needed to implement the program, especially when incorporating movement coordination feedback.1,16–20
Feedback is widely used to correct biomechanics that might be injurious during specific movements. Augmented feedback, for example, has been shown to change jump-landing biomechanics.21–23 A recent systematic review concluded that a combination of expert feedback and self-analysis modes have the greatest impact to reduce ground reaction forces during a jump-landing task.21 Nonetheless, the ideal mode or combination of feedback modes to reduce ACL injury rates has not yet been established. Real-time feedback is a tool that enables participants to track their actions and make biomechanical changes instantly. Several studies have shown positive results in altering lower extremity biomechanics during gait using real-time feedback.24–26 Real-time feedback can be given in different manners. Recently, external focus of attention feedback consisting of the clinician giving feedback to the athletes on errors they make while using an external focus of attention such as sitting back further in a chair instead of stating to increase knee flexion has shown promise to be superior over the typical internal focus of attention feedback.1,27,28 While expert feedback is the gold standard, it requires trained personnel, whereas a paradigm based on a dyad model of feedback may have more widespread application. Dyad training consists of a partner or teammate who corrects a participant on their task using a selected list of external feedback cues.1 Dynamic landing tasks are widely used to assess abnormal lower extremity biomechanics, yet there is limited research on the effects of real-time feedback, particularly expert and dyad feedback on this kind of movement.29
Dyad training has a unique advantage in addition to minimizing the need for expert personnel and reducing clinician burden, the use of a teammate or peer could increase program efficacy and compliance. Working with a peer allows for constant feedback, as athletes are not waiting on a single expert and provides a team-oriented atmosphere that may increase accountability. However, the lack of expert training of the dyad partner may limit effectiveness. If dyads feedback can improve injury risk mechanics to the same degree as experts this may bolster implementation and compliance of injury prevention programs. Thus, the purpose of this study was to determine the immediate effects of dyad versus expert feedback on drop landing kinematics and kinetics in female athletes. The primary hypothesis is the dyad group would have significantly better landing kinematics and kinetics compared to the expert feedback group.
METHODS
Participants
This cohort study enrolled 23 female athletes between the ages of 18-25 (19.30 ± 0.93 years, 1.71 ± 0.09 m, 68.44±9.82 kg; 13 basketball, 10 volleyball) that had completed the informed consent and initial questionnaires to meet inclusion criteria. All participants were given the informed consent and had the opportunity to ask questions before they were enrolled in the study. It was made clear to potential participants that they were free to opt out of the study at any time. Two teams (one female basketball and one female volleyball), from a local college, were team randomized to either dyad feedback (volleyball team) or expert feedback (basketball team) training conditions (13 expert, 19±0.87years, 1.7±0.09 m, 68.04±7.21kg) (10 dyad 19.4±1.07years, 1.73±0.08m, 72.18±11.23kg). Team randomization as dyad feedback is commonly used with a teammate thus, ensuring volleyball athletes provided feedback to volleyball players and avoid cross contamination. Participants were given the Tegner Activity Scale and Marx survey to ensure they were at competitive athlete activity levels. Individuals were only included in the study if they indicated Tegner Activity score of seven (study cohort average: 8.1±0.5) and indicated four times a week for all Marx sub-scales (running, cutting, decelerating, and pivoting). In addition, participants were given the International Knee Documentation Committee to ensure no subjective deficits were present. Individuals were only included in the study if they scored 80 (study cohort average: 97.0±5.4).
Previous medical history and demographic information were documented. Any athlete with a previous history of knee ligament or lower extremity injury in the previous two months that limited activity for more than one day was excluded. In addition, any female athlete that self-reported a current history of lower extremity instability (episodes of ‘giving way’), balance problems not remedied (feelings of instability), any illness that would negatively affect performance or safety during drop landing, or had undergone any previous lower extremity surgery within the previous two years was excluded, as well as athletes who had previously participated formal training in jump landing before participation in this study. No one was excluded based on any of the previously mentioned criteria.
Procedures
Testing Day One:
Initial Baseline
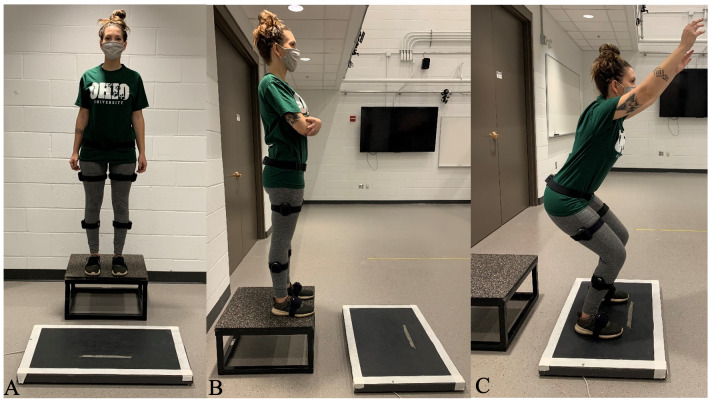
After participants enrolled and met the aforementioned inclusion and exclusion criteria they completed a DVJ pre-test as described by Hewett.30 Participants completed three trials of landing off of a box that was 30.38 cm in height and 38.1 cm in width. Participants dropped off the box, landing just in front of it, and immediately performed a maximum vertical jump. These drop jump tasks were recorded using Noraxon® Inertial Measurement Units (IMU, 100 Hz) (Noraxon Inc., Scottsdale, AZ, USA) system to record ankle, knee and hip joint angles placed on the foot, tibia, femur, and pelvis to provide 3D kinematics of the ankle, knee and hip. Per manufacturer instructions, shank and thigh sensors were placed laterally, halfway between the distal and proximal ends of the segment, and with the x-axis aligned to point superiorly along the long-axis of the bone.31 The pelvis IMU was placed posteriorly over the sacrum with the x-axis pointed towards the head. IMUs for the foot segments were placed on top of the feet over the midfoot region.31 The x-axis of each foot segment sensor pointed toward the toes. A subject-specific neutral-posture calibration was conducted prior to completing trials following manufacturer guidelines.31 Native algorithms integrated the calibration and sensor data to report three-dimensional segment orientations and accelerations and joint angles (myoMOTION Software 3.14.52; Noraxon Inc., Scottsdale, AZ, USA).31 The placement of the IMU units was done by an experienced researcher with over 15 years of clinical experience and nine years of biomechanics research (D.G.). A portable Bertec® force platform (FP4060-05-PT, Bertec Inc., Columbus, OH, USA) was used to collect ground reaction forces (GRFs: 100 Hz using Acquire Software 4.0). Figure 1 includes the set up for the IMUs and force platform.
Figure 1. IMU Placement, Force Platform Set up, and DVJ Landing. A: Frontal View of IMU Placement and Force Platform; B: Lateral View of IMU Placement and Force Platform; C: DVJ Landing.
Testing Day Two
Pre Test-Double Baseline
One week following initial pre-testing all participants were again asked to perform an IMU instrumented DVJ . This secondary assessment served as a double baseline and as a control for both intervention groups (i.e. participants served as their own control). It has been found that subjects will reliably land the same way at the same institution, even when with significant time between the assessments.32 An initial baseline and pre-test measure (double baseline) has been utilized in previous intervention studies.33–37 This study design is typically used when the dependent variables are relatively stable over time as the case for this study, as the kinetic and kinematic parameters have all been shown to be reliable within each site, across sites, and across examiners.32,38 The use of a double baseline design in collegiate athletes is particularly advantageous, as no team or athlete has to be the control group and receive no feedback.
Immediate Feedback
Directly following the second baseline (pre-test), Expert or Dyad feedback occurred. As previously mentioned, the entirety of two teams from one institution was randomly assigned to either dyad feedback or expert feedback. Dyad training consisted of a partner or teammate who corrected their partner on a squat jump landing task by using a checklist so the feedback would be correct with regards to technique (Appendix A). Expert external feedback consisted of the expert trained clinician (the lead author, after 20 hours of movement screening training) who gave feedback to the athlete on errors they made while using an external focus of attention (Appendix B). The external focus of attention feedback provided was based on previous literature.1,39 In the expert group, participants were given feedback one on one by an certified athletic trainer and in the dyad group, participants completed the study in individual pairs. Prior to dyad training each participant was provided with the feedback checklist and underwent a short five-minute tutorial of what to look for by the certified athletic trainer. This was done to simulate how a clinician may do an initial session with a team or coach but then the team or individuals implement the program.
All groups completed five trials of a squat jump landing during their assigned feedback method. The squat jump was elected elected during the feedback, because it is a common exercise during injury prevention programs,40 allows feedback to be provided, requires no equipment to administer, and is a bilateral landing task similar to the DVJ, but different sufficiently to limit participants simply becoming better at the DVJ with no transfer. Five trials were chosen to represent the minimal dose for potential efficacy,41 ensure compliance,42 and to be clinically translatable. Immediately following the feedback, a post-test of the IMU instrumented DVJ was completed with the same procedure as the pre-test and baseline.
Statistical Analysis
The dependent variables were knee flexion displacement, knee abduction displacement, and peak vGRF. Data were only collected during the three DVJ trials and averaged and used for analyses. Three repeated measures ANCOVAs (RMANCOVA) were conducted. Each RMANCOVA had the same within subjects factor time (pre and post) and the same between subject factor group (expert and dyad) with the covariate initial baseline. The first RMANCOVA was conducted for the dependent variable knee flexion displacement (initial contact to maximum knee flexion) with the covariate baseline knee flexion displacement. The second RMANCOVA was conducted for the dependent variable knee abduction displacement (initial contact to maximum knee abduction) with the covariate baseline knee abduction displacement. The last RMANCOVA was conducted for the dependent variable vGRF with the covariate baseline vGRF. If the individual RMANCOVA was significant follow up pairwise comparisons were conducted. Additionally, ƞ2 was calculated for each ANOVA as a measure of the proportion of the total variance in a dependent variable that is associated with the two groups.43 Eta-squared was interpreted as 0.01-0.05 as small, 0.06 as medium, and greater than 0.14 as large.43 Lastly, individual changes in knee kinematics and kinetics were compared to previously established minimal detectable change (MDC) values.44,45 MDC values of 3° for knee kinematics44 and 0.02 N·bw-1 for vGRF45 were used. Based on the frequency of whether an individual met the MDC, frequencies were calculated for each group (yes [met MDC] and no [did not meet MDC]) and a Chi-square test was conducted to evaluate group differences. Alpha level was set at α0.02 for all analyses to adjust for multiple tests using the Bonferroni correction method.46 All analyses were conducted in IBM SPSS Statistics for Windows, version 25 (IBM Corp., Armonk, N.Y., USA).
RESULTS
Kinematics
For the dependent variable knee abduction displacement the RMANCOVA revealed there was a significant difference for time (F(1,20)= 10.14, p=0.01, 1-β=0.77, ƞ2=0.44 [large]), but no significant difference for group (F(1,20)= 0.29, p=0.59, 1-β=0.08, ƞ2=0.02), or time by group (F(1,20)= 0.17 p=0.68, 1-β=0.07, ƞ2=0.01). Following immediate feedback, the mean difference was (-4.65˚, p=0.01), indicating that following feedback there was a 4.65˚ decrease in knee abduction displacement regardless of group. For the dependent variable knee flexion displacement, the RMANCOVA revealed there was no significance for time (F(1,20) =0.03, p=0.87, 1-β=0.05, ƞ2=0.01), group (F(1,20) =0.03, p=0.87, 1-β=0.05, ƞ2=0.01), or time by group (F(1,20) =1.54, p=0.23, 1-β=0.22, ƞ2=0.08). It is important to note that at the pre-test there was no difference between groups for any dependent variable (p0.05) and the values reported for our dependent variables are similar to previously published work.47,48 Descriptive statistics are shown in Table 1. Based on the MDC values for knee flexion displacement, 84.6% (n=11) of the individuals in the expert group and 30% (n=3) of the individuals in the dyad group exceeded the MDC and was statistically significant between groups (Χ2(1)=7.07, p=0.008). For knee abduction displacement, 76.9% (n=10) of the individuals in the expert group and 70% (n=7) of the individuals in the dyad group exceeded the MDC, which was not statistically different between groups (p0.05).
Table 1. Descriptive Statistics for the Dependent Variables.
| Pre | Post | ||
|---|---|---|---|
| Knee Flexion Displacement | Expert | 60.79 ± 15.44 | 67.85 ± 14.20 |
| Dyad | 66.45 ± 17.75 | 68.72 ± 18.21 | |
| Knee Abduction Displacement | Expert | -3.81 ± 7.23 | -4.55 ± 7.52‡ |
| Dyad | -2.37 ± 9.86 | -2.64 ± 9.83‡ | |
| vGRF (N·bw-1) | Expert | 4.21 ± 0.93 | 3.49 ± 0.69‡* |
| Dyad | 3.76 ± 0.69 | 3.94 ± 0.73 |
N = Netwons, bw = bodyweight
‡Significant difference from pre for condition (p0.02)
*Significant difference (p0.02) between groups at respective condition
Kinetics
For the dependent variable vGRF the RMANCOVA revealed a significant difference by time (F(1,20)=5.66, p=0.03, 1-β=0.64, ƞ2=0.21 [large]), a significant difference by group (F(1,20)=7.19, p=0.01, 1-β=0.72, ƞ2=0.27 [large]), and significant time by group difference ( F(1,20)=6.48, p=0.01, 1-β=0.68, ƞ2=0.25 [large]). For vGRF, there was a significant interaction of group by condition (p=0.01) effect with no difference between groups before feedback (p0.05). Between groups there was a decrease of vGRF in the expert group (difference 0.45 N*bw-1, p=0.01) at post feedback relative to dyad. Within the expert group there was a significant difference between pre- and post-feedback (difference 0.72 N*bw-1, p=0.01), while the dyad group did not significantly change from pre- to post-feedback (difference 0.18 N*bw-1, p=0.67). Overall, the expert decreased vGRF from pre to post compared to the dyad group. It is important to note the values reported for our dependent variables are similar to previously published work.45,49 Descriptive statistics are shown in Table 1. For vGRF, 84.6% (n=11) of the individuals in the expert group and 20% (n=2) of the individuals in the dyad group exceeded the MDC, which was statistically different between groups (Χ2(1)=9.61, p=0.002).
DISCUSSION
The primary finding was that the expert group decreased vGRF from pre to post compared to the dyad group. Additionally, the kinematic data revealed a significant difference with abduction displacement decreasing in both groups post, but no significant group effect. However, when investigating the MDCs, a larger percentage of individuals in the expert group exceeded the MDCs for knee flexion displacement compared to the dyad group. The MDC analysis for the other variables supported the inferential statistical analyses; a large percentage in both the expert and dyad group exceeded the MDC for knee abduction displacement and a larger percentage of individuals in the expert group exceeded the MDC for vGRF compared to the dyad group. The expert group improved kinetics relative to the dyad group, not supporting previous reports that dyad training could lead to effects similar to or exceed expert training.1 Kinematic changes were supportive of feedback offered in both groups, as abduction displacement improved at post regardless of group, indicating dyad was at least as good as expert for kinematic adaptations. However, for knee flexion displacement the MDC analysis supports the need for use of an expert to create change.
Prior reports of dyad success have been attributed to combining partner observation and execution of motor skills, and have been shown to be more effective together than either component alone.1,50,51 In addition, dyad training adds social and competitive aspects to training that can increase motivation.52 While the results of the current investigation did not support the primary hypothesis that the dyad group would be superior to the expert group, dyad feedback was able to induce beneficial kinematic adaptions to the expert level feedback indicating a potential alternative to experts for injury prevention training feedback for knee abduction displacement. However, for kinetic and kinematic adaptations and in alignment with prior literature, the use of expert feedback is preferred to decrease jump landing impact forces for immediate effectiveness.2,4,20,53
For vGRF, there was a significant difference between groups with the expert group decreasing vGRF at post while the dyad group did not change. This was also supported by the MDC analysis. A previously reported positive moderate association between increased vGRF and increased anterior tibial acceleration while landing from a jump supports the hypothesis that individuals who land with greater impact loads might have an increased risk of ACL injury suggesting the need for external feedback to alter landing mechanics.54 Previously, decreased vGRF was recorded during jump landing after simple instructions to "land softly."55 For the dyad group the individual providing feedback would have had to notice their partner landing stiffly to provide such feedback. It is likely that noticing more subtle landing stiffness that contributes to high vGRF requires further training as experts were able to identify individuals landing with high impact forces and provided feedback to “land softly”. The findings of the current investigation agree with a systematic review21 which, reported when expert feedback is provided a decrease in vGRF is seen. More recently, Beaulieu and Palmieri-Smith29 reported a decrease in vGRF following an intervention of real-time feedback in which participants were instructed to minimize their knee abduction moment as shown on a real-time graph. Additionally, McNair et al56 used expert feedback to successfully decrease vGRF in an immediate follow-up test, aligning with the current study results regarding outcomes in the expert group. The failure of the dyad group to improve vGRF is possibly due to the emphasis of the feedback to be on keeping knees aligned at neutral and the more novice dyad partners not attending to other cues to identify and thus avoid hard or loud landings
Knee flexion displacement did not change with either method of feedback at post testing based on the ANOVA analysis. However, when investigating the MDCs a larger percentage of the individuals in the expert group exceeded the MDC for knee flexion displacement compared to the dyad group. The results in this study are partially supported by Onate et al.22 who used video feedback and found increases in knee flexion immediately after an intervention. Other investigations such as Etnoyer, et al.57 employed expert feedback only and found knee flexion improvements at post testing. It is possible the current study was underpowered to detect statistically significant differences, but the MDC analysis is not impacted by sample size and thus support the use of expert feedback to alter knee flexion displacement. However, both groups were successful to reduce knee abduction displacement. This is consistent with previous literature, when Myer, et al.58 used a tuck jump and augmented external feedback they found that frontal plane knee angle (FPKA) decreased by an average of 37.9% over the three trials. In contrast, Etnoyer, et al57 found that using a combination of expert feedback and self-feedback did not change knee abduction.
Multiple sessions of feedback are likely needed to realize the full benefits of either expert or dyad approaches.59 Alternatively, providing immediate feedback based on a inertial-based sensor system as opposed to visual observation, may allow the more precise targeting of multiple variables including knee flexion, abduction and trunk lean after a one time intervention.60 It also has been noted that combination of feedback modalities may be most effective at improving jump landing biomechanics.21,57 A combination of videotape feedback and real-time feedback may produce the most effective results in altering jump landing biomechanics and reducing ACL injury risk.
This study had several limitations. It used a small sample size and may have been underpowered to detect statistical differences in knee flexion displacement that the MDC analysis identified. However, this study adds to the limited literature on dyad vs expert feedback to alter kinematics and kinetics in the field. The first landing of the DVJ was only analyzed and while analysis of the second landing may also be useful, it was not feasible in this study. Female basketball and volleyball athletes were only used as participants; thus, the results are not generalizable to all female athletes or male athletes. However, females were selected due to their higher risk factors and risk for ACL injury.8,61,62 Team randomization was used specifically for the dyad feedback and there is the possibility that basketball and volleyball players could respond differently to the different feedback delivery methods. Additionally, because the intervention (squat jumps) was different from our tested task (DVJ) this may explain some of results found in this study. However, the squat jump intervention was selected as it is much easier to implement, requiring no equipment and may better simulate sport demands than the DVJ. The DVJ was selected as the test task for its easy standardization (set drop height) and validity to predict injury risk.63 It is also possible that the dyad feedback could have seen better results with a repeated intervention (more than five trials) as participants learn the movement errors. In the future, studies could be done with a repeated intervention and additional resources, such as increased error training and perhaps video feedback for the dyad intervention group. Additionally, future studies should investigate the second landing of the DVJ to evaluate different landing mechanics between the first and second landing. Lastly, it is possible the dyad group could engage in more extensive training to be able to more easily recognize errors and perhaps improve their results would to be more like that of the expert group.
Conclusion
The results of this study indicate that movement screening experts giving real-time feedback were successful in improving key injury-risk kinematics and kinetics in female athletes, while dyad feedback only improved kinematics. Based on these results there may be a need for movement screening experts (athletic trainers, physical or physio therapists, strength and conditioning professionals etc.) to give feedback in ACL prevention programs to address multiple movement variables. However, dyad feedback, with even minimal training may be effective in order to improve knee abduction displacement, a key kinematic variable that reduces injury risk. Thus, if a movement expert or clinician is not available, improving knee abduction displacement (a key variable in reducing injury risk) is still possible with a dyad approach.
Conflicts of Interest
The authors have no conflicts of interest.
Appendix A.
Appendix B.
References
- Benjaminse A, Gokeler A, Dowling AV, et al. Optimization of the anterior cruciate ligament injury prevention paradigm: novel feedback techniques to enhance motor learning and reduce injury risk. J Orthop Sports Phys Ther. 2015;45(3):170-182. [DOI] [PubMed]
- Grooms D, Appelbaum G, Onate J. Neuroplasticity following anterior cruciate ligament injury: a framework for visual-motor training approaches in rehabilitation. J Orthop Sports Phys Ther. 2015;45(5):381-393. [DOI] [PubMed]
- Spindler KP, Wright RW. Anterior cruciate ligament (ACL) tear. N Engl J Med. 2008;359(20):2135-2142. [DOI] [PMC free article] [PubMed]
- Krosshaug T, Nakamae A, Boden BP. Mechanisms of anterior cruciate ligament injury in basketball. Am J Sports Med. 2007(35):359-367. [DOI] [PubMed]
- Delfico AJ, Garrett Jr WE. Mechanisms of injury of the anterior cruciate ligament in soccer players. Clin Sports Med. 1998;17(4):779-785. [DOI] [PubMed]
- Kobayashi H, Kanamura T, Koshida S, et al. Mechanisms of the anterior cruciate ligament injury in sports activities: a twenty-year clinical research of 1,700 athletes. J Sports Sci Med. 2010;9(4):669-675. [PMC free article] [PubMed]
- Boden BP, Dean GS, Feagin JA, Garrett WE. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000(23):573-578. [DOI] [PubMed]
- Ford KR, Myer GD, Toms HE, Hewett TE. Gender differences in the kinematics of unanticipated cutting in young athletes: Med Sci Spor Exer. 2005;37(1):124-129. [PubMed]
- Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in National Collegiate Athletic Association basketball and soccer a 13-year review. Am J Sports Med. 2005;33(4):524-531. [DOI] [PubMed]
- Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer NCAA data and review of literature. Am J Sport Med. 1995;23(6):694-701. [DOI] [PubMed]
- Ferretti A, Papandrea P, Conteduca F, Mariani PP. Knee ligament injuries in volleyball players. Am J Sport Med. 1992;20(2):203-207. [DOI] [PubMed]
- Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141-150. [DOI] [PubMed]
- Petushek EJ, Sugimoto D, Stoolmiller M, Smith G, Myer GD. Evidence-based best-practice guidelines for preventing anterior cruciate ligament injuries in young female athletes: a systematic review and meta-analysis. Am J Sport Med. 2019;47(7):1744-1753. [DOI] [PMC free article] [PubMed]
- Padua DA, DiStefano LJ, Hewett TE, et al. National Athletic Trainers’ Association position statement: prevention of anterior cruciate ligament injury. J Athl Train. 2018;53(1):5-19. [DOI] [PMC free article] [PubMed]
- Arundale AJ, Bizzini M, Giordano A, et al. Exercise-based knee and anterior cruciate ligament injury prevention: clinical practice guidelines linked to the international classification of functioning, disability and health from the academy of orthopaedic physical therapy and the American Academy of sports physical therapy. J Orthop Sport Phys Ther. 2018;48(9):A1-A42. [DOI] [PubMed]
- Chimera NJ, Swanik KA, Swanik CB, Straub SJ. Effects of plyometric training on muscle-activation strategies and performance in female athletes. J Athl Train. 2004;39(1):24-31. [PMC free article] [PubMed]
- Heidt RS, Sweeterman LM, Carlonas RL, Traub JA, Tekulve FX. Avoidance of soccer injuries with preseason conditioning. Am J Sports Med. 2000;28(5):659-662. [DOI] [PubMed]
- Lephart SM, Abt JP, Ferris CM, et al. Neuromuscular and biomechanical characteristic changes in high school athletes: a plyometric versus basic resistance program. Br J Sports Med. 2005;39(12):932-938. [DOI] [PMC free article] [PubMed]
- Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003-1010. [DOI] [PubMed]
- Myklebust G, Engebretsen L, Braekken IH, Skjølberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;13(2):71-78. [DOI] [PubMed]
- Ericksen HM, Gribble PA, Pfile KR, Pietrosimone BG. Different modes of feedback and peak vertical ground reaction force during jump landing: a systematic review. J Athl Train. 2013;48(5):685-695. [DOI] [PMC free article] [PubMed]
- Onate JA. Instruction of jump-landing technique using videotape feedback: altering lower extremity motion patterns. Am J Sport Med. 2005;33(6):831-842. [DOI] [PubMed]
- Herman DC, Oñate JA, Weinhold PS, et al. The effects of feedback with and without strength training on lower extremity biomechanics. Am J Sports Med. 2009;37(7):1301-1308. [DOI] [PubMed]
- Barrios JA, Crossley KM, Davis IS. Gait retraining to reduce the knee adduction moment through real-time visual feedback of dynamic knee alignment. J Biomech. 2010;43(11):2208-2213. [DOI] [PMC free article] [PubMed]
- Crowell HP, Davis IS. Gait retraining to reduce lower extremity loading in runners. Clin Biomech. 2011;26(1):78-83. [DOI] [PMC free article] [PubMed]
- Willy RW, Scholz JP, Davis IS. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clin Biomech. 2012;27(10):1045-1051. [DOI] [PMC free article] [PubMed]
- Wulf G. Attentional focus and motor learning: a review of 15 years. Int Rev Sport Exerc Psychol. 2013;6(1):77-104.
- Gokeler A, Benjaminse A, Welling W, Alferink M, Eppinga P, Otten B. The effects of attentional focus on jump performance and knee joint kinematics in patients after ACL reconstruction. Phys Ther Sport. 2015;16(2):114-120. [DOI] [PubMed]
- Beaulieu ML, Palmieri-Smith RM. Real-time feedback on knee abduction moment does not improve frontal-plane knee mechanics during jump landings. Scand J Med Sci Sport. 2014;24(4):692-699. [DOI] [PubMed]
- Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes: decreased impact forces and increased hamstring torques. Am J Sport Med. 1996;24(6):765-773. [DOI] [PubMed]
- Noraxon. MyoMotion: 3D Wireless Inertial Motion Measurement System.
- Myer GD, Wordeman SC, Sugimoto D, et al. Consistency of clinical biomechanical measures between three different institutions: implications for multi-center biomechanical and epidemiological research. Int J Sports Phys Ther. 2014;9(3):289-301. [PMC free article] [PubMed]
- Hopkins WG, Marshall SW, Batterham AM, Hanin J. Progressive statistics for studies in sports medicine and exercise science. Med Sci Sports Exerc. 2009;41(1):3-13. [DOI] [PubMed]
- Kinugasa T, Cerin E, Hooper S. Single-subject research designs and data analyses for assessing elite athletes’ conditioning. Sports Med. 2004;34(15):1035-1050. [DOI] [PubMed]
- Roy JS, Moffet H, Hébert LJ, Lirette R. Effect of motor control and strengthening exercises on shoulder function in persons with impingement syndrome: a single-subject study design. Man Ther. 2009;14(2):180-188. [DOI] [PubMed]
- Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007;87(3):337-349. [DOI] [PubMed]
- Ross SE. Noise-enhanced postural stability in subjects with functional ankle instability. Br J Sports Med. 2007;41(10):656-659; discussion 659. [DOI] [PMC free article] [PubMed]
- Ford KR, Myer GD, Hewett TE. Reliability of landing 3D motion analysis: implications for longitudinal analyses. Med Sci Sports Exerc. 2007;39(11):2021-2028. [DOI] [PubMed]
- Myer GD, Brent JL, Ford KR, Hewett TE. Real-time assessment and neuromuscular training feedback techniques to prevent ACL injury in female athletes. Strength Cond J. 2011;33(3):21-35. [DOI] [PMC free article] [PubMed]
- Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med. 1999;27(6):699-706. [DOI] [PubMed]
- Onate JA, Guskiewicz KM, Sullivan RJ. Augmented feedback reduces jump landing forces. J Orthop Sport Phys Ther. 2001;31(9):511-517. [DOI] [PubMed]
- Sugimoto D, Myer GD, Bush HM, Klugman MF, McKeon JMM, Hewett TE. Compliance with neuromuscular training and anterior cruciate ligament injury risk reduction in female athletes: a meta-analysis. J Athl Train. 2012;47(6):714-723. [DOI] [PMC free article] [PubMed]
- Tabachnick B, Fidell L. Using Multivariate Statistics. 5th ed. Pearson; 2007.
- Di Stasi SL, Snyder-Mackler L. The effects of neuromuscular training on the gait patterns of ACL-deficient men and women. Clin Biomech. 2012;27(4):360-365. [DOI] [PMC free article] [PubMed]
- Cordova ML, Armstrong CW. Reliability of ground reaction forces during a vertical jump: implications for functional strength assessment. J Athl Train. 1996;31(4):342-345. [PMC free article] [PubMed]
- Dunn OJ. Multiple comparisons among means. J Amer Stat Assoc. 1961;56(293):52-64.
- Fox AS, Bonacci J, McLean SG, Spittle M, Saunders N. What is normal? Female lower limb kinematic profiles during athletic tasks used to examine anterior cruciate ligament injury risk: a systematic review. Sports Med. 2014;44(6):815-832. [DOI] [PubMed]
- Delahunt E, Sweeney L, Chawke M, et al. Lower limb kinematic alterations during drop vertical jumps in female athletes who have undergone anterior cruciate ligament reconstruction. J Orthop Res. 2012;30(1):72-78. [DOI] [PubMed]
- Bates NA, Ford KR, Myer GD, Hewett TE. Impact differences in ground reaction force and center of mass between the first and second landing phases of a drop vertical jump and their implications for injury risk assessment. J Biomech. 2013;46(7):1237-1241. [DOI] [PMC free article] [PubMed]
- Shea CH, Wright DL, Wulf G, Whitacre C. Physical and observational practice afford unique learning opportunities. J Mot Behav. 2000;32(1):27-36. [DOI] [PubMed]
- Shea CH, Wulf G, Whitacre C. Enhancing training efficiency and effectiveness through the use of dyad training. J Mot Behav. 1999;31(2):119-125. [DOI] [PubMed]
- Gokeler A, Benjaminse A, Hewett TE, et al. Feedback techniques to target functional deficits following anterior cruciate ligament reconstruction: implications for motor control and reduction of second injury risk. Sports Med. 2013;43(11):1065-1074. [DOI] [PMC free article] [PubMed]
- Mather RC, Koenig L, Kocher MS, et al. Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg Am. 2013;95(19):1751-1759. [DOI] [PMC free article] [PubMed]
- McNair PJ, Marshall RN. Landing characteristics in subjects with normal and anterior cruciate ligament deficient knee joints. Arch Phys Med Rehab. 1994;75(5):584-589. [PubMed]
- Milner CE, Fairbrother JT, Srivatsan A, Zhang S. Simple verbal instruction improves knee biomechanics during landing in female athletes. The Knee. 2012;19(4):399-403. [DOI] [PubMed]
- McNair P, Prapavessis H, Callender K. Decreasing landing forces: effect of instruction. Br J Sports Med. 2000;34(4):293-296. [DOI] [PMC free article] [PubMed]
- Etnoyer J, Cortes N, Ringleb SI, Van Lunen BL, Onate JA. Instruction and jump-landing kinematics in college-aged female athletes over time. J Athl Train. 2013;48(2):161-171. [DOI] [PMC free article] [PubMed]
- Myer GD, Stroube BW, DiCesare CA, et al. Augmented feedback supports skill transfer and reduces high-risk injury landing mechanics: a double-blind, randomized controlled laboratory study. Am J Sport Med. 2013;41(3):669-677. [DOI] [PMC free article] [PubMed]
- Padua DA, DiStefano LJ, Marshall SW, Beutler AI, de la Motte SJ, DiStefano MJ. Retention of movement pattern changes after a lower extremity injury prevention program is affected by program duration. Am J Sports Med. 2012;40(2):300-306. [DOI] [PubMed]
- Dowling A, Favre J, Andriacchi T. Inertial sensor-based feedback can reduce key risk metrics for anterior cruciate ligament injury during jump landings. Am J Sports Med. 2012;40(5):1075-1083. [DOI] [PubMed]
- Wulf G, Lewthwaite R. Conceptions of ability affect motor learning. J Mot Behav. 2009;41(5):461-467. [DOI] [PubMed]
- Zachry T, Wulf G, Mercer J, Bezodis N. Increased movement accuracy and reduced EMG activity as the result of adopting an external focus of attention. Brain Res Bull. 2005;67(4):304-309. [DOI] [PubMed]
- Hewett TE. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492-501. [DOI] [PubMed]