Abstract
We report herein a patient with a cloacal malformation and an absent vagina. The patient underwent colostomy on Day 1 of life. At 7 months of age, fistulography of the cloaca showed a common channel >3 cm in length; a vagina was not visible. At the age of 11 months, the patient underwent abdominoperineal anoplasty with the repurposing of her rectal fistula as a substitute vagina. Intraoperative examination revealed a bicornuate uterus and bilateral ovaries. The rectum was resected 7 cm at the confluence of the cloaca. The colonic stump was pulled through a newly created anal canal and an anoplasty was performed. Two months after this procedure, the patient experienced anal prolapse. At the age of 17 months, she underwent partial urogenital mobilization and a modified Delorme operation, and 5 months later the colostomy was closed. At present, this patient is 3 years old and doing well.
INTRODUCTION
In cloacal anomalies, fecal and urinary incontinence is a major problem for patients with anorectal and urogenital malformations. Furthermore, the surgical management of absent vagina with anorectal and urogenital malformations constitutes a significant technical challenge.
CASE REPORT
A female infant was born at 38-week gestational age, weighing 2570 g. After birth, she was diagnosed with a cloacal malformation (Fig. 1a). At 1 day of life, the patient underwent double-barrel colostomy and fistulography of the cloaca (Fig. 1b); the results of the latter were suspicious for a vaginal defect. At the age of 2 months, urethroscopy revealed a urethra and a rectal fistula and an absent vaginal opening (Fig. 1c). Laparoscopy revealed a bicornuate uterus and structures consistent with bilateral ovaries (Fig. 1d and e). At the age of 7 months, fistulography of the cloaca showed a common channel >3 cm in length and was unable to visualize a vagina (Fig. 2). At the age of 11 months, weighing 8 kg, the patient underwent abdominoperineal anoplasty using the rectal fistula as a substitute vagina. Laparotomy confirmed the presence of a bicornuate uterus and bilateral ovaries (Fig. 3a). Next, the position of the anus was decided using neuromuscular stimulation, and an inverted Y incision was performed at the anal dimple (Fig. 3b). After spreading the external anal sphincter muscle and using laparoscopic electrostimulation to identify the center of contraction of the levator ani muscle, the needle pierced the center of the levator ani muscle to create a canal for the colonic pull-through. The colon was resected 7 cm proximal to the confluence of the cloaca, preserving the vessels to the rectal fistula (Fig. 3c). The stump of the colon was pulled through the newly created anal canal (Fig. 3b). Two months after surgery, the patient experienced anal prolapse. When she was 17 months old, she underwent partial urogenital mobilization and a modified Delorme operation for anal prolapse. Preoperative urethroscopy showed that the external urethral sphincter was located on the bladder side of the confluence of the cloaca (Fig. 4a). During partial urogenital mobilization, the initial dissection was made using a posterior omega flap and a posterior midline incision, without an anterior incision of the orifice of the cloaca (Fig. 4b). During dissection of the posterior wall of the persistent common urogenital sinus, the pubovaginalis muscle at the perineal body was detected and preserved using neuromuscular stimulation. The posterior wall of the persistent urogenital sinus was opened ventrally to a point where the perineal flap could reach (Fig. 4c and d). The opened urogenital sinus was then sewn to the perineal flap (Fig. 4e). Both sides of the incised urogenital sinus were then sewn to the skin (Fig. 4f). Finally, the modified Delorme procedure was performed (Fig. 5h). A circumferential mucosal incision, ~1 cm from the skin, was made into the prolapsed neorectum (Fig. 5a and b). The mucosal and submucosal layers were dissected from the muscularis layer (Fig. 5c). After the mucosa was dissected, the exposed circular muscle layer of the colon was pushed back through the anal canal (Fig. 5d and e). We exposed the circular muscular layer up to the vertex of the prolapse. Eventually, the cut ends of the mucosa were sutured together 1 cm from the skin (Fig. 5f and g). Five months after surgery, the patient underwent closure of the colostomy with laparoscopic appendectomy. We were unable to recognize two distinct orifices for the urethra and neovagina (Fig. 6a and b). On laparoscopy, the surgeons were able to recognize the stump of the rectal fistula used as the neovagina and a bicornuate uterus with two ovaries (Fig. 6c).
Figure 1.
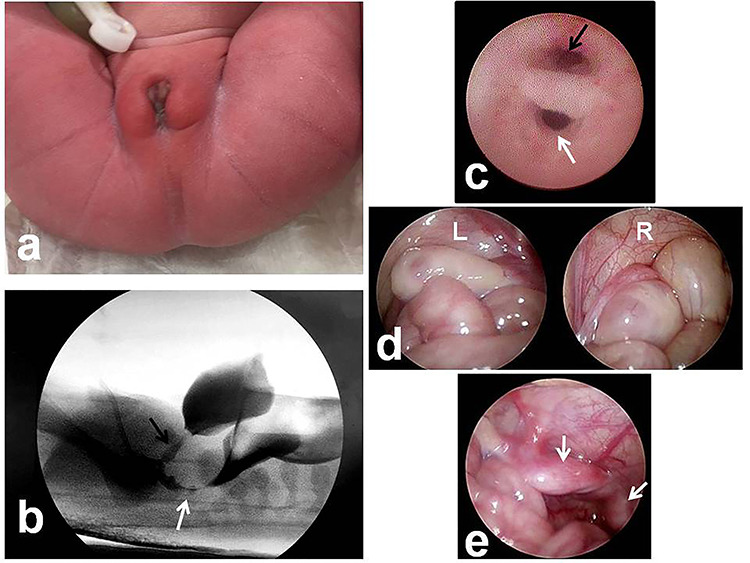
Evaluation of the anorectal and urogenital malformations. (a) External view of the cloacal malformation. (b) Fistulography at 1 day of life shows a cloaca and is suspicious for a vaginal defect (black arrow, urethra; white arrow, rectal fistula). (c) Urethroscopy at 2 months of age reveals two orifices: a urethra and a rectal fistula; there is no vaginal opening (black arrow, urethra; white arrow, rectal fistula). (d, e) Laparoscopy reveals two ovaries and a bicornuate uterus (R, right tube and ovary; L, left tube and ovary; white arrow, bicornuate uterus).
Figure 2.
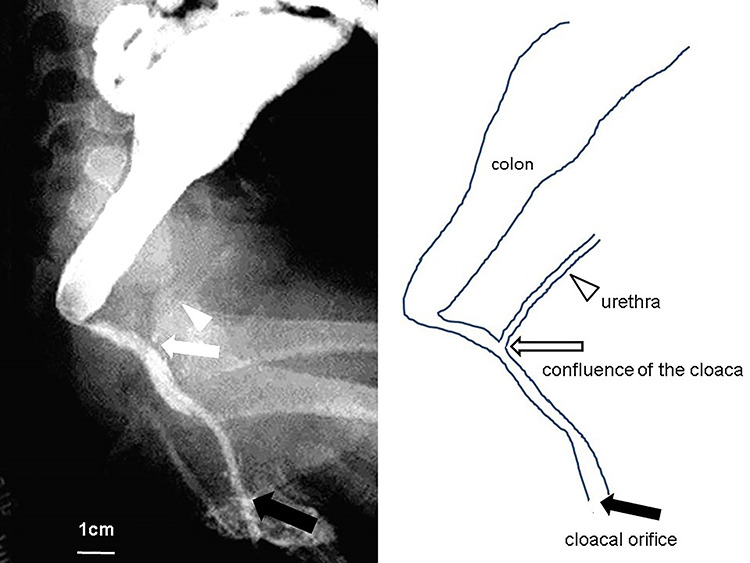
Fistulography and schema of the cloaca, 7 months of age. The common channel is >3 cm in length, and the vagina is defective (black arrow, cloacal orifice; white arrow, confluence of the cloaca; white arrowhead, urethra).
Figure 3.
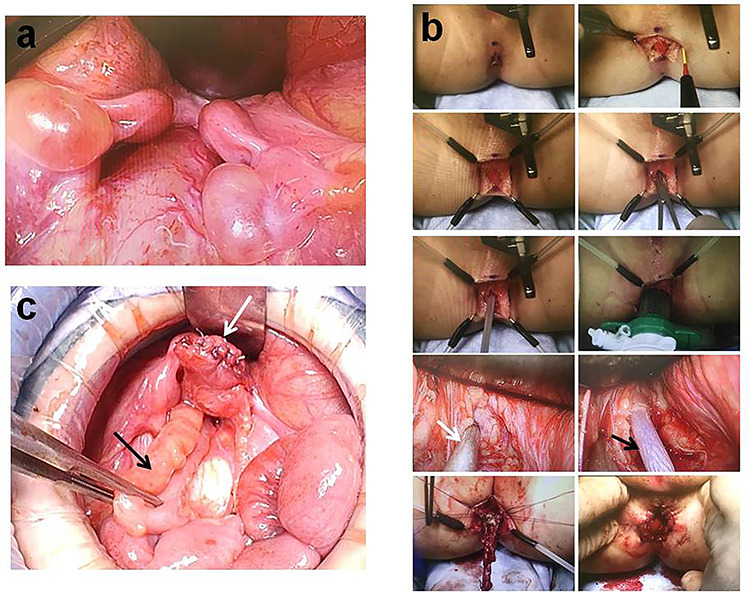
Intraoperative findings during abdominoperineal anoplasty, 11 months of age. (a) Laparotomy confirms the presence of a bicornuate uterus and bilateral ovaries. (b) An inverted Y incision is created at the anal position and the colonic pull-through is performed (white arrow, laparoscopic muscle electrostimulation; black arrow, access needle with radially expandable sleeve). (c) Abdominoperineal anoplasty using the rectal fistula as a neovagina (white arrow, neovagina; black arrow, colonic pull-thorough).
Figure 4.
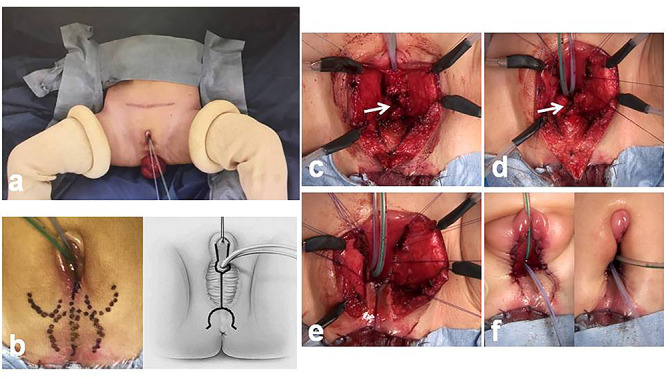
Intraoperative findings during partial urogenital mobilization, 17 months old. (a) Balloon catheters in the bladder and in the rectocutaneous fistula. (b) Surgical planning and initial dissection using a posterior omega flap and a posterior midline incision of the orifice of the cloaca. (c–f) The posterior wall of the persistent urogenital sinus is opened ventrally until the perineal flap is able to reach it. The opened sinus is sewn to the perineal flap. Both sides of the incised sinus are sewn to the skin (white arrow, pubovaginalis muscle at the perineal body).
Figure 5.
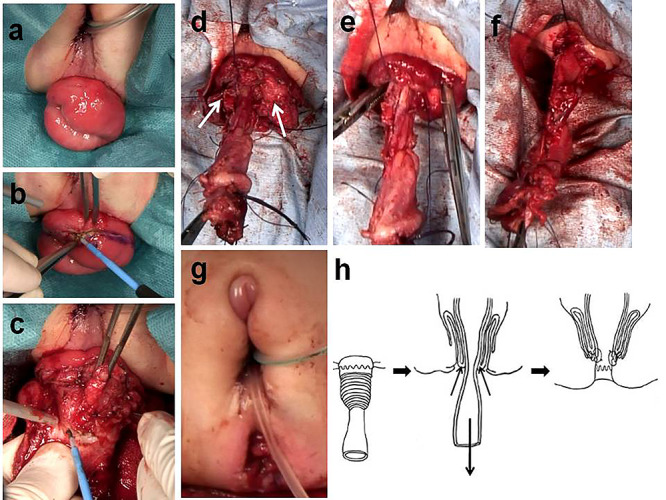
Intraoperative findings during the modified Delorme procedure, 17 months old. (a, b) A circumferential mucosal incision is made ~1 cm from the skin. (c) The mucosal and submucosal layers are dissected from the muscularis layer with the surgeon’s index finger placed in the anal canal. (d) A sleeve of mucosa is dissected, revealing the circular colonic muscular layer up to the vertex of the prolapse (white arrow, circular muscular layer). (e) The exposed circular muscular layer is pushed back through the anal canal. (f) The muscular layer of the colon and the muscle wall of the prolapse are sutured using absorbable material. (g) Completion of partial urogenital mobilization and modified Delorme method. (h) Schematic of the modified Delorme procedure.
Figure 6.
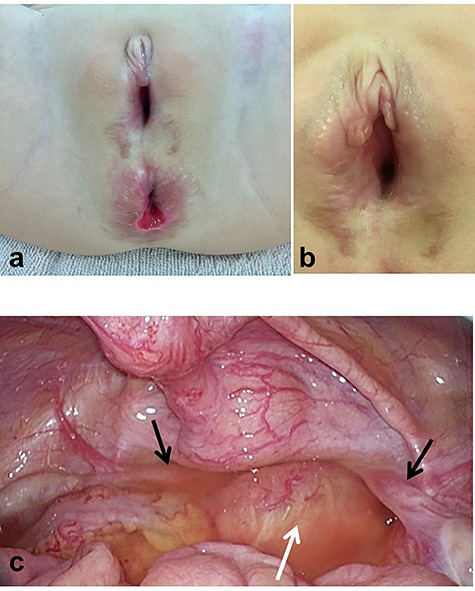
Intraoperative findings during colostomy closure and laparoscopic appendectomy, 22 months old. (a, b) Distinct urethral and vaginal openings are not able to be recognized. (c) The stump of the rectal fistula (now the neovagina), a bicornuate uterus and two ovaries are recognized (black arrows, ovaries; white arrow, neovagina).
The patient is currently 3 years old and has a good cosmetic result at the perineum. She has good urinary function without urinary tract infection or hydronephrosis and is able to defecate without incurring mucosal prolapse.
DISCUSSION
In cloacal anomalies, anoplasty would be achieved by laparoscopy-assisted anorectoplasty or posterior sagittal anorectoplasty. When the vagina is present, total urogenital mobilization or partial urogenital mobilization is often performed for perineal urethroplasty [1–3]. Partial urogenital mobilization with limited proximal dissection of the urogenital sinus is safe and effective at preventing injury to sphincteric function [2]. If, however, there is a vaginal defect, an alternative reconstructive approach is to use a segment of intestine, or the sigmoid colon, to create a neovagina [4]. On the other hand, a rectal fistula was used to create a neovagina in patients with a cloacal malformation, and a rectal flap from the dilated terminal rectum was used to make tubularization and anastomosis cranial to a hypoplastic vagina [5]. If an alternative method of reconstruction is used, long-term follow-up is required because there are reports describing carcinoma developing in the neovagina [6]. The modified Delorme procedure, particularly using the Umegae method, is a procedure for anal prolapse that allows a greater amount of dissected colonic mucosa than does the original Delorme method [7, 8]. The modified Delorme procedure is safe and effective, with a low risk of recurrence.
Our patient will eventually undergo an anastomosis between the uterus and the neovagina in order to allow passage of menses. It is reported that a side-to-side anastomosis of the uterus to the neovagina is a technically easy procedure after the onset of puberty [9]. In vaginal mucosa, lactic acid bacteria such as Doederlein’s bacillus are resident and the vaginal mucosa is always kept acidic. When an alternative reconstructive approach would be to use a segment of intestine, the sigmoid colon or the skin, it is necessary to keep vaginal mucosa acidic to prevent the purulent salpingitis. In a case report about tubo-ovarian abscess after colonic vaginoplasty for high cloacal anomaly, she required a left salpingo-oophorectomy [10]. In this case, vaginal washer with a lactic acid-containing gel, JELLY PLUS MED (JEX Co., Ltd, Yokohama, Japan), is regularly inserted into the neovagina and planned to use until and after vaginoplasty.
Patients with cloacal anomalies experience many problems, including fecal and urinary incontinence, difficulty discharging menstrual blood, issues with sexual function and satisfaction and carcinoma developing in the neovagina.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- 1. Peña A. Total urogenital mobilization--an easier way to repair cloacas. J Pediatr Surg 1997;32:263–7. [DOI] [PubMed] [Google Scholar]
- 2. Rink RC, Metcalfe PD, Kaefer MA, Casale AJ, Meldrum KK, Cain MP. Partial urogenital mobilization: a limited proximal dissection. J Pediatr Urol 2006;2:351–6. [DOI] [PubMed] [Google Scholar]
- 3. Rink RC, Metcalfe PD, Cain MP, Meldrum KK, Kaefer MA, Casale AJ. Use of the mobilized sinus with total urogenital mobilization. J Urol 2006;176:2205–11. [DOI] [PubMed] [Google Scholar]
- 4. Parsons JK, Gearhart SL, Gearhart JP. Vaginal reconstruction utilizing sigmoid colon: complications and long-term results. J Pediatr Surg 2002;37:629–33. [DOI] [PubMed] [Google Scholar]
- 5. Shimada K, Hosokawa S, Matsumoto F, Johnin K, Naitoh Y, Harada Y. Urological management of cloacal anomalies. Int J Urol 2001;8:282–9. [DOI] [PubMed] [Google Scholar]
- 6. Couder F, Golfier F, Traverse-Glehen A, Devouassoux-Shisheboran M, Raudrant D. Mucinous adenocarcinoma of a sigmoid vaginoplasty in a patient with Mayer-Rokitansky-Kuster-Hauser syndrome: a second case report. Gynecol Obstet Case Rep 2016;2:1–3. [Google Scholar]
- 7. De la Torre L, Zornoza-Moreno M, Cogley K, Calisto JL, Wehrli LA, Ruiz-Montañez A, et al. Transanal endorectal approach for the treatment of idiopathic rectal prolapse in children: experience with the modified Delorme's procedure. J Pediatr Surg 2019;54:857–61. [DOI] [PubMed] [Google Scholar]
- 8. Umegae S. Delorme's procedure for rectal prolapse. Nippon Daicho Komonbyo Gakkai Zasshi 2012;65:866–73 (Abstract in English). [Google Scholar]
- 9. Hisamatsu E, Nakagawa Y, Sugita Y. Vaginal reconstruction in female cloacal extrophy. Urology 2014;84:681–4. [DOI] [PubMed] [Google Scholar]
- 10. Fumino S, Iwai N, Tokiwa K, Hibi M, Iwabuchi T. Tubo-ovarian abscess after colonic vaginoplasty for high cloacal anomaly in a 13-year-old girl. Eur J Pediatr Surg 2002;12:345–7. [DOI] [PubMed] [Google Scholar]


