Abstract
Clinical Trial Registration:
Objective:
To evaluate economic costs from the health system perspective of an electronic health record-based clinical decision support (CDS) tool, TeenBP, designed to assist in the recognition and management of hypertension in youth.
Methods:
Twenty primary care clinics within an integrated health system were randomized to the TeenBP CDS or usual care (UC), with patient enrollment from 4/15/14–4/14/16. The 12-month change in standardized medical care costs for insured patients aged 10–17 years without prior hypertension were calculated for each study arm. The primary analysis compared patients with ≥1 visit with blood pressure (BP) ≥95th percentile (isolated hypertensive BP), and secondary analyses compared patients with ≥3 visits within one year with BP ≥95th percentile (incident hypertension). Generalized estimating equation models estimated the difference-in-differences in costs between groups over time.
Results:
Among 925 insured patients with an isolated hypertensive BP, the pre-to-post change in overall costs averaged $22 more for TeenB P CDS versus UC patients over 12 months, but this difference was not statistically significant (p=0.723). Among 159 insured patients with incident hypertension, the pre-to-post change in overall costs over 12 months was higher by $227 per person on average for TeenBP CDS versus UC patients, but this difference also was not statistically significant (p=0.313).
Conclusions:
The TeenBP CDS intervention was previously found to significantly improve identification and management of hypertensive BP in youth, and in this study, we find that this tool did not significantly increase care costs in its first 12 months of clinical use.
Keywords: decision support, hypertension, costs, economic analysis
Introduction
Based on reviews and recommendations from expert panels sponsored by the National Institutes of Health and the American Academy of Pediatrics,1,2 blood pressure (BP) is routinely measured in children and adolescents during primary care visits.3,4 However, competing examination priorities—and sometimes, difficulty in evaluating BP levels—have tended to interfere with clinical recognition of hypertension during routine pediatric visits.5–7 Elevated BP in childhood has been shown to track into adulthood,8–11 suggesting that early identification and intervention could reduce lifetime risk of subsequent cardiovascular complications. As a result, there remains a need to assist primary care clinicians in diagnosing hypertension in youth. Although much has been written about the prevalence and natural history of hypertension in childhood,12–15 little has been written about the potential cost related to methods for improving diagnosis and management.
The TeenBP study was a primary care clinic-randomized controlled trial comparing an electronic health record (EHR) based clinical decision support (CDS) to assist in the recognition and management of elevated BP versus usual clinical care. Previously published findings indicated that the TeenBP CDS improved clinical recognition of incident hypertension in youth (54.9% vs. 21.3%, p<0.001) and increased rates of dietitian referral (17.1% vs. 3.9%, p=0.001) and additional hypertension workup (9.4% vs. 4.2%, p=0.046).16,17
As health systems consider whether to implement TeenBP, or a similar CDS with demonstrated effectiveness in improving hypertension recognition in youth, they will need to understand the corresponding costs and effects on care patterns. Such decision support systems may affect costs by increasing the number of follow-up encounters and tests or the complexity coding levels of certain clinical visits. Conversely, these tools may help clinicians deliver more efficient care by reducing the number of encounters and tests needed to deliver the same result. This study investigates this issue by assessing the costs and patterns of care associated with the TeenBP CDS intervention.
Methods
Study design and subjects
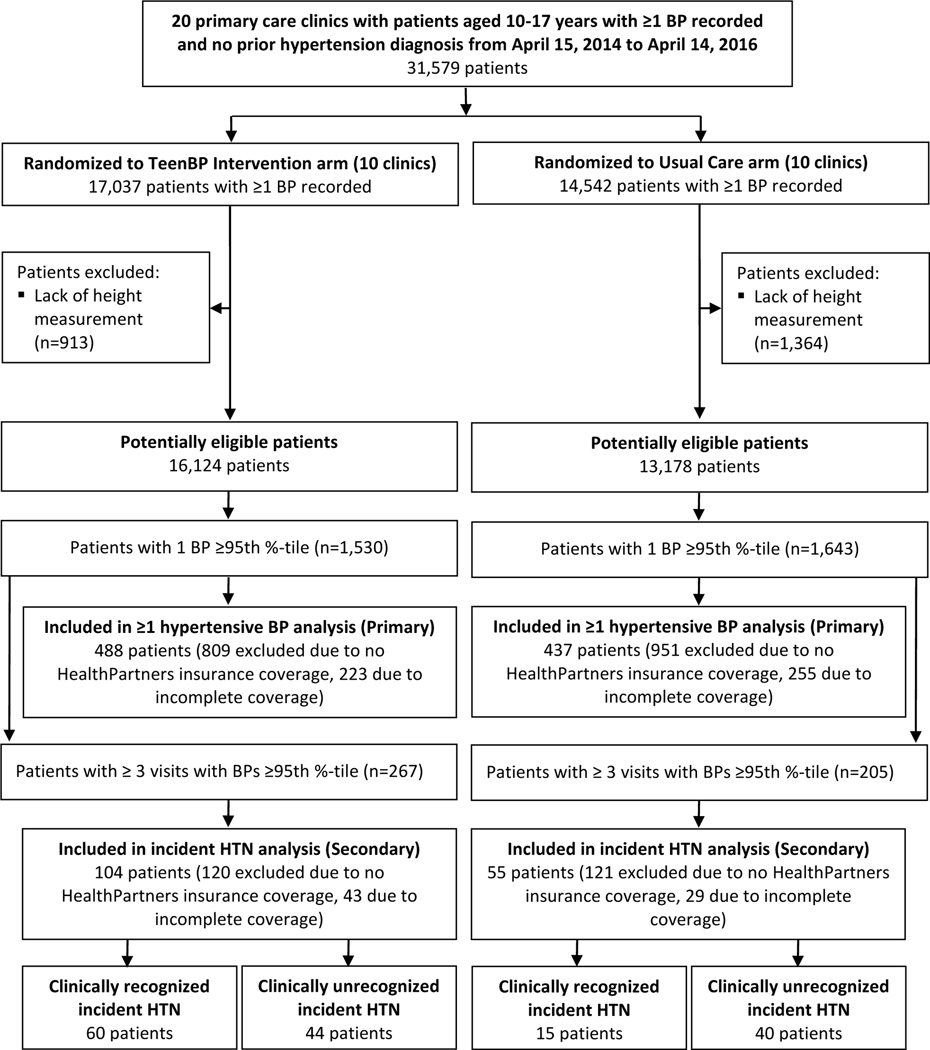
The TeenBP study was a two-arm clinic-randomized controlled trial conducted in primary care clinics at HealthPartners, an integrated health system in the Minneapolis-St. Paul metropolitan area. To be included in the current cost analysis, patients had to meet the following criteria: (a) age at enrollment 10–17 years, (b) no prior hypertension diagnosis, (c) height measurement recorded within the prior year, (d) ≥1 hypertensive BP measured during a primary care visit at a Health Partners study site between April 15, 2014 and April 14, 2016, and (e) continuous Health Partners insurance coverage for the full 12 months pre- and post-enrollment in this study, with coverage gaps no longer than 30 days (Figure 1). Heights, weights, and BP were routinely measured by licensed practical nurses or medical assistants using standardized procedures for rooming patients. Clinical criteria for isolated hypertensive BP (≥1 BP at or above the 95th percentile) and incident hypertension (≥3 visits with BP at or above the 95th percentile) were defined according to national guidelines available during the study, including the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents (Fourth Report).1 Detailed descriptions of the study design and environment have been published elsewhere.16–18 This study was approved by the HealthPartners Institutional Review Board with a waiver of informed consent for the implementation and evaluation of the TeenBP CDS and is registered on ClinicalTrials.gov (NCT01760239).
Figure 1. Summary of Patient Eligibility.
Comparators
Clinics were randomized to TeenBP CDS intervention and usual care control arms. The intervention clinics used TeenBP, a web-based EHR-linked, CDS system designed to support identification and management of hypertensive BP in adolescents aged 10–17 during primary care visits. The TeenBP CDS system is activated when a clinic rooming staff member enters a BP measurement into the EHR, prompting exchange of clinical data from the current and prior visits—including height, weight, problem lists, encounter diagnoses, medications, and laboratory data—for processing by web-based CDS algorithms that generate a display within the EHR showing current and prior BP percentiles (within 2 years) and clinically actionable suggestions for the clinician, as described in Appendix Table 1. Clinicians treating patients in usual care clinics did not have access to the TeenBP CDS. Clinical recognition of hypertension for patients in either arm was ascertained by least 1 of the following: (1) outpatient discharge diagnosis of hypertension (ICD-9 401–405 and ICD-10 110) or elevated BP (ICD-9 796.2 and ICD-10 R03.0), (2) hypertension or elevated BP documented in the clinical note, (3) hypertension or elevated BP documented in the after visit summary, (4) hypertension or elevated BP added to the problem list, (5) a workup for secondary causes of hypertension or end-organ damage, or (6) antihypertensive medication being prescribed.
Time horizon and study perspective
Changes in patient costs in the 12 months following their study index visit relative to their costs in the preceding 12 months are compared from a health system perspective.
Data sources
Utilization of healthcare services was collected using insurance claims data systems. Outpatient care delivered in primary care and specialty care settings was classified using Current Procedural Terminology, Fourth Edition codes (CPT-4), and filled prescriptions for medications were classified using 11-digit General Product Identifier codes. Overall costs were composed of clinic-based (which included utilization related to primary care, urgent care, cardiology and nephrology specialty care, laboratory, and radiology) and pharmacy costs. Appendix Table 2 details the classification codes used to identify each category of utilization. Clinic visits with evaluation and management services for new (CPT −4 99201–99205) and established patients (CPT-4 99211–99215) were also specifically identified with a corresponding coding for complexity—Level 1 (CPT-4 99201/99211) to Level 5 (CPT-4 99205/99215)—assigned. Following standard guidance for economic evaluations,19 we included all claims within each category—without attempt to distinguish attribution of costs specifically affected by the intervention—in primary comparisons; however, we stratified utilization associated with hypertension- or cardiovascular-related specialty care, labs, and medications for contextual and secondary comparison purposes.
To derive healthcare costs, claims were converted to dollar amounts using Total Care Relative Resource Values™ (TCRRVs), which are a nationally standardized set of measures endorsed by the National Quality Forum20 and derived from Centers for Medicare and Medicaid Services (CMS) relative value units (RVUs). TCRRVs extend CMS RVU measures to include utilization categories, such as laboratory services and medications, which do not have CMS RVU weights.21 Specifically, TCRRVs for the year 2015, the midpoint of study enrollment, were used to convert all claims to represent 2015 U.S. dollars.
To quantify the typical costs of deploying the TeenBP CDS, the study team estimated the number of hours needed for a pediatrician (or similar clinician), EHR system application developer, and project manager to implement an existing CDS in an EHR system, conduct training for a care system of 20 clinics, and maintain the CDS implementation over time. Median hourly wages for the closest matching occupation of each role were obtained from National Occupational Employment and Wage Estimates data and benefits for employees in health care were obtained from Employer Costs for Employee Compensation data.23 Compensation costs were converted to 2015 dollars for comparability to reported medical care costs.24
Statistical analysis
All statistical analyses were 2-sided and conducted by “intention-to-treat,” and p-values of less than 0.05 were considered statistically significant. Differences in baseline characteristics between arms were assessed using t-tests for continuous variables and Chi-square tests for categorical variables. Standard health econometric and specification testing methods, described below, were used to assess the incremental differences in healthcare costs between study arm. Specifically, healthcare care costs and utilization were analyzed using a generalized estimating equation model with a time x study arm interaction term that accounted for the correlation in each subjects’ repeated measures over time. The appropriate distribution family was determined using the modified Park test (typically gamma distributed) and the goodness of fit using a log link function was tested using modified Hosmer and Lemeshow and Pregibon link tests. Analyses controlled for covariates statistically imbalanced between comparison groups (e.g., age, race, and insurance status at baseline). Confidence intervals were estimated using a Huber/White heteroscedasticity-robust sandwich estimator. Statistical analyses were conducted using Stata version 11 (StataCorp, College Station, TX).
Results
Among the 3,173 patients meeting study inclusion criteria with at least one BP ≥95th percentile, 488 patients in the TeenBP CDS arm and 437 patients in the usual care (UC) control arm met the additional insurance coverage criteria for inclusion in the primary cost analysis (Figure 1 and Appendix Table 3). Patients in TeenBP CDS clinics were slightly older (13.9 vs. 13.6 years, p<0.05), more likely to be white (69.3% vs. 58.8%, p≤0.01), and less likely to have public insurance (19.3% vs. 26.3%, p≤0.01) compared to their counterparts in the usual care clinics (Table 1). Otherwise, the two arms were statistically balanced in their baseline characteristics.
Table 1.
Baseline Characteristics of Study Patients with Full Insurance Coveragea and ≥1 Hypertensive BP
| All | TeenBP CDS Intervention | Usual Care | |
|---|---|---|---|
| (N=925) | (n=488) | (n=437) | |
| Age, mean (sd) | 13.8 (2.2)b | 13.9 (2.2)b | 13.6 (2.1)b |
| Girls (%) | 489 (52.9) | 265 (54.3) | 224 (51.3) |
| Race (%) | |||
| White | 595 (64.3)c | 338 (69.3)c | 257 (58.8)c |
| Black | 146 (15.8)c | 63 (12.9)c | 83 (19.0)c |
| Asian | 124 (13.4)c | 63 (12.9)c | 61 (14.0)c |
| Other | 60 (6.5)c | 24 (4.9)c | 36 (8.2)c |
| Hispanic (%) | 34 (3.7) | 18 (3.7) | 16 (3.7) |
| Insurance (%) | |||
| Private | 716 (77.4)c | 394 (80.7)c | 322 (73.7)c |
| Public | 209 (22.6)c | 94 (19.3)c | 115 (26.3)c |
| BP percentile (%) | |||
| SBP ≥99th percentile | 150 (16.2) | 84 (17.2) | 66 (15.1) |
| SBP ≥95th and < 99th percentile | 545 (58.9) | 282 (57.8) | 263 (60.2) |
| DBP ≥95th percentile only | 230 (24.9) | 122 (25.0) | 108 (24.7) |
| BMI percentile (%) | |||
| <85th | 406 (43.9) | 214 (43.9) | 192 (43.9) |
| 85–95th | 224 (24.2) | 123 (25.2) | 101 (23.1) |
| ≥95th | 295 (31.9) | 151 (30.9) | 144 (33.0) |
| ADHD diagnosis (%) | 119 (12.9) | 65 (13.3) | 54 (12.4) |
| Anxiety or depression diagnosis (%) | 89 (9.6) | 52 (10.7) | 37 (8.5) |
Notes: sd = standard deviation; BP = blood pressure; sd = standard deviation; BMI = body mass index; SBP = systolic BP; DBP = diastolic BP; ADHD = attention deficit hyperactivity disorder.
Full insurance coverage indicates continuous insurance coverage (gaps no larger than 30 days) in the 12 months pre and post meeting study index criteria with ≥1 hypertensive BP measurement (≥95th percentile, based on age, sex, and height).
p < 0.05.
p ≤ 0.01.
There were no statistically significant pre-to-post differences in 12-month costs between the TeenBP and UC arms for patients with at least one BP ≥95th. Overall medical costs in the TeenBP CDS arm. increased by $357 (95% confidence interval [CI]: $270 to $445, p<0.001) vs. $336 (95% CI: $255 to $417, p<0.001) in the UC arm ($22 difference, 95% CI: -$97 to $140, p=0.723) (Table 2). The largest mean pre-to-post differences in per-person costs were observed in primary care ($17 lower in the TeenBP CDS clinics, p=0.407), cardiology and nephrology specialty care ($26 higher in the TeenBP CDS clinics, p=0.090), and radiology ($24 higher in the TeenBP CDS clinics, p=0.402). The change in urgent care costs differed by about $1 per patient over 12 months (95% CI: -$13 to 14, p=0.942), and the change in laboratory costs—overall and when limited to routine BP- or cardiovascular-related tests—were just slightly lower among TeenBP CDS patients (less than $5 per patient per year, P=0.853), with similarly wide confidence intervals. The average change in pharmacy costs was within $1 per patient per year between arms, whether overall (lower in UC clinics, p=0.967) or only for medications to treat BP (lower in TeenBP clinics, p=0.262). Appendix Table 4 shows that there were no statistically significant differences in clinic visit counts or coding levels between arms, but pre-to-post visit counts were lower with slightly higher coding levels in TeenBP compared to UC clinics
Table 2:
Medical Care Costs for Patients with >1 Hypertensive BP
| TeenBP CDS (n=488) | Usual Care (n=437) | |||||
|---|---|---|---|---|---|---|
| Mean | Change from baseline | Mean | Change from baseline | Study arm differential Change from baseline, Mean (95% CI) | P-Value | |
| Clinic-based Costs | ||||||
| 12 months, pre-index | 472 | 383 | ||||
| 12 months, post-index | 777 | 305 | 662 | 279 | 27 (−78 to 131) | 0.618 |
| Primary Care Visit Costs | ||||||
| 12 months, pre-index | 227 | 201 | ||||
| 12 months, post-index | 402 | 175 | 393 | 192 | −17 (−57 to 23) | 0.407 |
| Urgent Care Visit Costs | ||||||
| 12 months, pre-index | 34 | 35 | ||||
| 12 months, post-index | 37 | 3 | 37 | 2 | 1 (−13 to 14) | 0.942 |
| Cardiology and Nephrology Specialty Care Visit Costs | ||||||
| 12 months, pre-index | 8 | 5 | ||||
| 12 months, post-index | 39 | 31 | 10 | 26 (−4 to 55) | 0.090 | |
| Laboratory Costs | ||||||
| 12 months, pre-index | 105 | 80 | ||||
| 12 months, post-index | 156 | 52 | 136 | 56 | −5 (−55 to 45) | 0.853 |
| Laboratory Costs, BP-related | ||||||
| 12 months, pre-index | 13 | 9 | ||||
| 12 months, post-index | 21 | 8 | 18 | 9 | −1 (−6 to 4) | 0.742 |
| Laboratory Costs, CV-related | ||||||
| 12 months, pre-index | 15 | 10 | ||||
| 12 months, post-index | 26 | 11 | 22 | 12 | −1 (−7 to 5) | 0.704 |
| Radiology Costs | ||||||
| 12 months, pre-index | 97 | 58 | ||||
| 12 months, post-index | 150 | 53 | 87 | 29 | 24 (−32 to 79) | 0.402 |
| Pharmacy Costs | ||||||
| 12 months, pre-index | 247 | 267 | ||||
| 12 months, post-index | 302 | 55 | 321 | 54 | 1 (−47 to 49) | 0.967 |
| Pharmacy Costs, HTN-related | ||||||
| 12 months, pre-index | 3 | 0 | ||||
| 12 months, post-index | 2 | −1 | 1 | 1 | −1 (−3 to 1) | 0.262 |
| Overall Costs | ||||||
| 12 months, pre-index | 712 | 657 | ||||
| 12 months, post-index | 1,069 | 357 | 993 | 336 | 22 (−97 to 140) | 0.723 |
Notes: BP = blood pressure; CI = confidence interval; CV = cardiovascular; HTN = hypertension. Costs presented in this table were measured in the 12 months before and after the first date patients met study criteria with at least one hypertensive BP measurement (≥95th percentile, based on age, sex, and height). Clinic-based costs comprise of the sum of primary care visit, urgent care visit, cardiology and nephrology specialty care visit, laboratory, and radiology costs. Overall costs comprise of the sum of clinic-based and pharmacy costs. Codes for identifying costs in each category are described in Appendix Table 1. Mean and incremental changes in costs were estimated using a generalized estimating equation model with a time x study arm interaction term and covariate adjustment for age, race, and insurance status at baseline. The 95% confidence intervals account for patient random effects and were estimated using a Huber/White robust sandwich estimator. All costs are in 2015 U.S. dollars.
Among the 472 patients meeting criteria for incident hypertension (≥3 visits with BPs ≥95th percentile), 104 in the TeenBP CDS arm and 55 in the UC arm met criteria for inclusion in the secondary cost analysis based on having continuous insu.ance enrollment (Figure 1 and Appendix Table 3). Baseline characteristics for these patients were statistically similar between study arms (Appendix Table 5). Of the patients with incident hypertension, 60 (58%) were recognized in the TeenBP clinics vs only 15 (27%) in the UC clinics.
Table 3 compares patient costs in the TeenBP and UC clinics for the patients with incident hypertension between the two study arms and by whether their hypertension was clinically recognized. The mean pre-to-post change in overall costs over 12 months was higher by $227 (95% CI: -$214 to $667, p=0.313) per person in the TeenBP CDS arm compared to usual care; however, neither the difference in these costs, nor within any subcategory, were statistically significant. Among patients with hypertension that was clinically recognized, regardless the study arm, differences were more pronounced. Most notably, the change in total clinic-based ($505 per person per year, 95% CI: $66 to $943, p=0.024) and cardiovascular-related laboratory costs ($32 per person per year, 95% CI: $10 to $53, p=0.004) were significantly higher in patients with clinically recognized compared to patients with unrecognized hypertension; however, overall costs were not significantly higher for the clinically recognized group ($393 per person per year, 95% CI: $−95 to $881, p=0.114). Appendix Table 6 suggests part of the increased total clinic-based costs may be attributed to more clinic visits associated with hypertension recognition (0.61 per person per year, 95% CI: −0.28 to 1.49, p=0.178), but is less likely due to increased complexity coding levels of visits (−0.01, 95% CI: −0.24 to 0.23, p=0.954). The pre-to-post difference in costs for children and adolescents who had their incident hypertension recognized was higher in the TeenBP CDS $964 (95% $437 to $1,491, p≤0.001) compared to the usual care study arm $429 (95% CI $233 to $625, p≤0.001) ($535 difference, 95% CI: -$27 to $1,097, p=0.062). The pre-to-post difference in overall costs for patients who did not have their incident hypertension re cognized was lower in the TeenBP CDS $405 (95% CI: $120 to $691, p=0.005) compared to the usual care study arm $528 (95% CI: $133 to $923, p=0.009) (-$123 differed, 95% CI: -$610 to $365, p=0.622). Although incident hypertension was associated with significant increases in utilization costs regardless of clinical recognition status, these increases were not significantly different between study arms. Comparing between study arms and clinical recognition status, pre-to-post overall costs were $658 higher for patients with recognized vs. unrecognized hypertension in TeenBP clinics relative to usual > are clinics (95% CI: -$84 to $1,399, p=0.082). This difference was also not statistically significant, nor was the case for any subcategory of costs.
Table 3:
Medical Care Costs for Patients with Incident Hypertension
| TeenBP CDS (n=104) vs. Usual Care (n=55) | Patients with clinically recognized incident HTN vs. patients with unrecognized incident HTN | |||||||
|---|---|---|---|---|---|---|---|---|
| Differential change from baseline, Mean (95% CI) | P-Value | Both study arms: HTN recognized (n=75) vs. unrecognized (n=84) differential change from baseline, Mean (95% CI) | P-Value | [A] Recognized HTN: TeenBP CDS (n=60) vs. usual Care (n=15) differential change from baseline, Mean | [B] Unrecognized HTN: TeenBP CDS (n=44) vs. Usual Care (n=40) differential change from baseline, Mean | [A]-[B] Study arm differential change from baseline, Mean (95% CI) | P-Value | |
| Clinic-based Costs | 221 (−180 to 622) | 0.280 | 505 (66 to 943) | 0.024 | 370 | −96 | 465 (−209 to 1,140) | 0.176 |
| Primary Care Visit Costs | −70 (−205 to 65) | 0.308 | 57 (−67 to 182) | 0.368 | −101 | −93 | −9 (−268 to 251) | 0.949 |
| Urgent Care Visit Costs | 7 (−42 to 55) | 0.787 | −13 (−55 to 30) | 0.564 | −63 | 54 | −117 (−255 to 20) | 0.094 |
| Cardiology and Nephrology Specialty Care Visit Costs | 68 (−33 to 169) | 0.185 | 120 (−19 to 258) | 0.091 | 135 | −23 | 158 (−16 to 332) | 0.074 |
| Laboratory Costs | 117 (−228 to 461) | 0.507 | 208 (−117 to 532) | 0.209 | 268 | −62 | 329 (−195 to 853) | 0.218 |
| Laboratory Costs, BP-related | 14 (−6 to 33) | 0.165 | 24 (5 to 43) | 0.012 | 0 | 11 | −10 (−47 to 27) | 0.591 |
| Laboratory Costs, CV-related | 20 (−1 to 41) | 0.061 | 32 (10 to 53) | 0.004 | 8 | 13 | −5 (−46 to 36) | 0.811 |
| Radiology Costs | 100 (−95 to 295) | 0.315 | 133 (−122 to 387) | 0.307 | 131 | 27 | 104 (−242 to 450) | 0.556 |
| Pharmacy Costs | 6 (−139 to 151) | 0.939 | −112 (−238 to 15) | 0.083 | 164 | −27 | 192 (−43 to 427) | 0.108 |
| Pharmacy Costs, HTN-related | −1 (−8 to 5) | 0.671 | 6 (−1 to 14) | 0.092 | −3 | −4 | 1 (−16 to 18) | 0.926 |
| Overall Costs | 227 (−214 to 667) | 0.313 | 393 (−95 to 881) | 0.114 | 535 | −123 | 658 (−84 to 1,399) | 0.082 |
Notes: BP = blood pressure; CI = confidence interval; CV = cardiovascular; HTN = hypertension. Costs presented in this table were measured in the 12 months before and after the first date patients met study criteria with at least one hypertensive BP measurement (≥95th percentile, based on age, sex, and height). Comparisons labeled as X vs. Y indicate the costs for patients in group X minus the costs for patients in group Y. Clinic-based costs comprise of the sum of primary care visit, urgent care visit, cardiology and nephrology specialty care visit, laboratory, and radiology costs. Overall costs comprise of the sum of clinic-based and pharmacy costs. Codes for identifying costs in each category are described in Appendix Table 1. Mean and incremental changes in costs were estimated using a generalized estimating equation model with a time x study arm interaction term. The 95% confidence intervals account for patient random effects and were estimated using a Huber/White robust sandwich estimator. All costs are in 2015 U.S. dollars.
Table 4 describes the estimated costs of deploying the existing TeenBP CDS to a care system with 20 clinics. Implementing the existing CDS would involve extracting health record data elements (such as BP measurements, height, weight, medications, and lab values) to a web service that runs the CDS algorithm and building components within the health record to deliver the CDS at the point of care (such as via a link or automated pop-up within the EHR). We estimated this would require 160 hours each for a pediatrician and project manager to oversee with 480 hours of an EHR system application developer’s time to do the technical deployment. In addition, we estimated 40 hours for the pediatrician and project manager to develop training materials and 40 hours (2 hours per 20 clinic sites) to present in-person at each site during a designated staff training time. These activities total an estimated $75,673 in upfront costs to deploy the existing CDS. An additional $25,224 annually is estimated for ongoing CDS maintenance, which may include updating data routines and algorithms as EHR data elements or care guidelines change over time.
Table 4:
Estimated Deployment Costs for Existing TeenBP CDS in New Care System with 20 Clinics
| Hours | First Year Cost | Ongoing Annual Cost | |
|---|---|---|---|
| CDS Implementation | |||
| Pediatrician (or similar clinician) | 160 | $17,276 | |
| Programmer | 480 | $33,429 | |
| Project manager | 160 | $10,886 | |
| CDS Training | |||
| Pediatrician (or similar clinician) | 80 | $8,638 | |
| Project manager | 80 | $5,443 | |
| CDS Maintenance | |||
| Pediatrician (or similar clinician) | 80 | $8,638 | |
| Programmer | 160 | $11,143 | |
| Project manager | 80 | $5,443 | |
| Total | $75,673 | $25,224 | |
Notes: CDS = clinical decision support. CDS implementation may include extracting health record data elements (such as blood pressure measurements, height, weight, medication lists, and lab values) to a web service that runs the CDS algorithm and building components within the health record to deliver the CDS at the point of care (such as via a link or automated pop-up within the EHR). CDS training involves developing training materials and delivering in-person training sessions at 20 clinic locations. CDS maintenance may include updating data routines and algorithms as EHR data elements or care guidelines change over time. Hourly wage for a pediatrician is based on U.S. Bureau of Labor Statistics (BLS) code 29–1065 (Pediatricians, General).22 Hourly wage for an EHR system application developer (programmer) is based on BLS code 15–1133 (Software Developers, Systems Software).22 Hourly wage for a project manager is based on BLS code 11–9199 (Managers, All Other).22 Hourly compensation costs include fringe benefits at a rate of 30% of total compensation for employees in the health care sector.23 All costs are in 2015 U.S. dollars.
Discussion
Despite recommendations that BP measurement should be part of the routine examination of children and the relation of childhood elevated BP to development of adult hypertension, BP is measured in only 40 to 70 percent of pediatric clinic visits in the United States.3,4,25 Moreover, elevated or hypertensive BP levels often are missed, with rates of clinical recognition as low as 8–13%.5–7 The association of high BP with cardiovascular disease has been well-established in adults,26 but adverse associations also have been reported in childhood.27 Therefore, methods to ensure office BP measurement and assist in evaluating BP levels would be beneficial, but introducing additional methodology into office practice raises questions about value and cost. We have previously found that use of TeenBP, an electronic health record (EHR) based clinical decision support (CDS) system, significantly improves clinical recognition of incident hypertension in youth and clinical evaluation for hypertension. We now show that use of the TeenBP CDS did not significantly increase clinical care and pharmacy costs per patient per year when compared to patients clinically recognized with hypertension in clinics not using the CDS. We also show that the TeenBP CDS did not significantly affect the frequency of clinical visits or their complexity coding levels, but results suggest some potential offset in costs from modestly fewer clinic visits of slightly higher complexity coding. Thus, we conclude that CDS tools may improve identification and management of hypertension in youth without a significantly increased cost.
Elevated BP has been found to increase annual costs by $20928 and the annual cost of hypertension in children has been estimated to exceed $9,000 per patient per year.29 In comparison, total annual costs for general pediatric care average about $3,000 per patient per year.30 In contrast, we found that clinical recognition of hypertension among youth was associated with a significant increase ($505 per person per year) in clinic-based costs. This finding is not surprising, because children and adolescents diagnosed with hypertension should receive some additional medical attention to rule out secondary causes of hypertension and screen for other evidence of cardiovascular risk factors. Our findings suggest that part of this increase may be attributable to additional follow-up visits, but additional laboratory and diagnostic work-up explains most of this increase. The use of BP medications increased slightly ($6 per person per year) among patients with clinically recognized versus unrecognized hypertension, but this difference was not statistically significant. More broadly, our findings contrast with national data showing an increase in use of antihypertensive medications among adolescents.31
Studies on cost of blood pressure measurement, including using CDS, for identification of hypertension in youth are sparse, and the present study appears to be the first economic analysis of a randomized implementation of an electronic health record system designed to improve identification and management of hypertension in children and adolescents. Prospective studies have evaluated the clinical effectiveness of CDS tools for pediatric populations,32–34 but we are not aware of any that have evaluated their impact on healthcare utilization.
The costs for implementing the TeenBP CDS, once developed, could not be directly measured in this study because we were unable to separate the costs related to research, development, and pilot testing. However, we estimated that the cost for a similar care system to deploy the existing TeenBP CDS would require about $76,000 upfront and $25,000 per year thereafter. For the 29,302 potentially eligible patients reached over two years of accrual and one year of follow-up in this study, this translates to $3.64 per patient (or an average $1.21 per patient per year over three years). This may be a high or low estimate depending on the environment. A previous study estimated that implementation and maintenance of an existing CDS would involve 10 percent of a programmer’s time and 5 percent of a physician’s time over a year, approximated to cost $19,300 annually in 2009 dollars,36 but this may be an optimistic estimate for many environments. Because deployment costs are anticipated to be largely fixed, the per patient per year cost of implementing TeenBP would scale favorably for care systems that serve larger patient populations. In addition, further development and adoption of data standardization and application programming interfaces (APIs) in EHR systems could conceivably lower costs for adoption and maintenance of CDS tools for all care systems to near- negligible levels in the future.37
Several factors constrain the interpretation of these data. Given the high variance and skewness in per patient costs, the study sample was not powered on economic outcomes—meaning statistical non-significance could reflect insufficient sample size—and our findings were limited to patients who had HealthPartners insurance in the 12 months pre- and post-index (which limited eligible individuals to 29% of youth with ≥1 hypertensive BP and 34% with ≥3 hypertensive BPs). No significant differences in baseline characteristics were observed between the included or excluded samples for those with ≥3 hypertensive BPs, but there were significant differences in race, ethnicity, and diagnosis of depression or anxiety in the included sample with ≥1 hypertensive BP. In addition, most of the health benefits—and potential cost offsets—from improved BP recognition and management in youth would be expected to occur over a much longer period due to delayed or prevented cardiovascular complications as adults. A broad base of evidence indicates that high BP during childhood is predictive of hypertension and cardiovascular outcomes in adulthood,8–11 and a consortium of 7 large cohort studies is in the process of combining data to better understand this link.38 Yet little is known about the potential cost savings from early detection of hypertension in children. To address this issue, we plan to conduct a microsimulation model analysis, extending our analysis to include longer-term outcomes, while accounting for the uncertainty in how hypertensive BP during childhood manifests in adulthood. Such an analysis is needed to deepen our understanding of the full long-term value of upfront investments to improve BP care in youth. Comparisons of patients by status of clinical recognition of hypertension may be confounded by uncontrolled for differences in the patients recognized in each study arm. Lastly, this study was a part of a pragmatic trial implemented in an integrated health system, and the outcomes should be replicated in other healthcare settings and populations.
Conclusion
Hypertension in youth presents a unique set of challenges: it usually occurs with an absence of symptoms, calculating and evaluating BP percentiles is a complicated endeavor, and most youth with an isolated hypertensive BP have normal BP at follow-up. Nevertheless, recognition of children with an incident hypertensive BP is relevant to preventive health care because of tracking of childhood elevated BP into adult hypertension. The TeenBP CDS intervention was previously found to significantly improve identification and management of hypertensive BP in youth. In this study, we now report that use of the CDS did not significantly increase costs of care above usual care, affirming the potential practicality of its use as a part of routine care of children and adolescents in large ambulatory primary care practices.
Supplementary Material
Acknowledgements:
This study was supported by the National Heart, Lung, and Blood Institute (grant number R01HL115082; principal investigator E.O.K.). Dr. O’Connor was also supported by grant P30DK092924 from the National Institute of Diabetes and Digestive and Kidney Diseases during the study period.
This study finds that electronic health record-based clinical decision support designed to improve identification and management of hypertensive blood pressure in youth can be implemented without a significant increase in medical care costs.
Funding Source: This sudy was supported by grant R01HL115082 from the National Heart, Lung, and Blood Institute. Dr. O’Connor was also supported by grant P30DK092924 from the National Institute of Diabetes and Digestive and Kidney Diseases during the study period. Funders had no role, in the study design, collection, analysis, and interpretation of data, the writing of the manuscript, or the decision to submit the article for publication.
Footnotes
Conflict of Interest:
The authors have no potential conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.National High Blood Pressure Education Program Working Group on High Blood Pressure in C, Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 Suppl 4th Report):555–576. [PubMed] [Google Scholar]
- 2.Flynn JT, Kaelber DC, Baker-Smith CM, et al. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3). [DOI] [PubMed] [Google Scholar]
- 3.Shapiro DJ, Hersh AL, Cabana MD, Sutherland SM, Patel AI. Hypertension screening during ambulatory pediatric visits in the United States, 2000–2009. Pediatrics. 2012;130(4):604–610. [DOI] [PubMed] [Google Scholar]
- 4.Parker ED, Sinaiko AR, Daley MF, et al. Factors Associated With Adherence to Blood Pressure Measurement Recommendations at Pediatric Primary Care Visits, Minnesota and Colorado, 2007–2010. Prev Chronic Dis. 2015;12:E118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007;298(8):874–879. [DOI] [PubMed] [Google Scholar]
- 6.Brady TM, Solomon BS, Neu AM, Siberry GK, Parekh RS. Patient-, provider-, and clinic-level predictors of unrecognized elevated blood pressure i. children. Pediatrics. 2010;125(6):e1286–1293. [DOI] [PubMed] [Google Scholar]
- 7.Riley M, Dobson M, Sen A, Green L. Recognizing elated BP in children and adolescents: how are we doing? J Fam Pract. 2013;62(6):294–299. [PubMed] [Google Scholar]
- 8.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117(25):3171–3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toschke AM, Kohl L, Mansmanr U, von Kries R. Meta-analysis of blood pressure tracking from childhood to adulthood and implications for the design of intervention trials. Acta Paediatr. 2010;99(1):24–29. [DOI] [PubMed] [Google Scholar]
- 10.Theodore RF, Broadbent J, Nagin D, et al. Childhood to Early-Midlife Systolic Blood Pressure Trajectories: Early-Life Predictors, Effect Modifiers, and Adult Cardiovascular Outcomes. Hypertension. 2015;6 6(6).1108–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oikonen M, Nuotio J, Magnussen CG, et al. Repeated Blood Pressure Measurements in Childhood in Prediction of Hypertension in Adulthood. Hypertension. 2016;67(1):41–47. [DOI] [PubMed] [Google Scholar]
- 12.Lo JC, Sinaiko A, Chandra M, et al. Prehypertension and hypertension in community-based pediatric practice. Pediatrics. 2013;131(2):e415–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rao G Diagnosis, Epidemiology, and Management of Hypertension in Children. Pediatrics. 2016;138( 2). [DOI] [PubMed] [Google Scholar]
- 14.Cheung eL, Bell CS, Samuel JP, Poffenbarger T, Redwine KM, Samuels JA. Race and Obesity in Adolescent Hypertension. Pediatrics. 2017;139(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jackson SL, Zhang Z, Wiltz JL, et al. Hypertension Among Youths - United States, 2001–2016. MMWR Morb Mortal Wkly Rep. 2018;67(27):758–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kharbanda EO, Asche SE, Sinaiko AR, et al. Clinical Decision Support for Recognition and Management of Hypertension: A Randomized Trial. Pediatrics. 2018;141(2):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kharbanda EO, Asche SE, Sinaiko A, et al. Evaluation of an Electronic Clinical Decision Support Tool for Incident Elevated BP in Adolescents. Academic pediatrics. 2018;18(1):43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kharbanda EO, Nordin JD, Sinaiko AR, et al. TeenBP: Development and Piloting of an EHR-Linked Clinical Decision Support System to Improve Recognition of Hypertension in Adolescents. EGEMS (Wash DC). 2015;3(2):1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramsey SD, Willke RJ, Glick H, et al. Cost-effectiveness analysis alongside clinical trials II-An ISPOR Good Research Practices Task Force report. Value Health. 2015;18(2):161–172. [DOI] [PubMed] [Google Scholar]
- 20.National Quality Forum. Press release: NQF Endorses Resource Use Measures. January 31, 2012; http://www.qualityforum.org/News_And_Resources/Press_Releases/2012/NQF_Endorses_Resource_Use_Measures.aspx. Accessed June 12, 2018.
- 21.HealthPartners. Total Care Relative Resource Value (TCRRVTM): A Measurement Approach to Achieve the Triple Aim. HealthPartners White Paper. September 21, 2017; https://www.healthpartners.com/ucm/groups/public/@hp/@public/documents/documents/cntrb_039627.pdf. Accessed June 12, 2018. [Google Scholar]
- 22.U.S. Bureau of Labor Statistics. May 2018 National Occupational Employment and Wage Estimates. 2019; https://www.bls.gov/oes/current/oes_nat.htm. Accessed 1-5-2020.
- 23.U.S. Bureau of Labor Statistics. Employer Costs for Employee Compensation, Supplementary Tables: National Compensation Survey; 2019; https://www.bls.gov/web/ecec/ecsuptc.pdf. Accessed 1-5-2020. [Google Scholar]
- 24.U.S. Bureau of Labor Statistics. Consumer Price Index - All Urban Consumers, Medical care. Series ID: CUSR0000SAM 2019; http://data.bls.gov/cgi-bin/srgate. Accessed 5-19-19.
- 25.Stabouli S, Sideras L, Vareta G, et al. Hypertension screening during healthcare pediatric visits. J Hypertens. 2015;33(5):1064–1068. [DOI] [PubMed] [Google Scholar]
- 26.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/nMa/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High b’oo d Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13–e115. [DOI] [PubMed] [Google Scholar]
- 27.Flynn JT. High blood pressure in the young: why should we care? Acta Paediatr. 2018;107(1):14–19. [DOI] [PubMed] [Google Scholar]
- 28.Gilmer TP, O’Connor PJ, Sinaiko AR, et al. Impact of hypertension on healthcare costs among children. Am J Manag Care. 2014;20(8):622–628. [PMC free article] [PubMed] [Google Scholar]
- 29.Miller GF, Coffield E, Leroy Z, Wallin R. Prevalence and Costs of Five Chronic Conditions in Children. J Sch Nurs. 2016;32(5):357–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.MN Community Measurement. 2017 Cost & Utilization Report Average Cost per Procedure Total Cost of Care Relative Resource Use Utilization. 2017. [Google Scholar]
- 31.Hales CM, Kit BK, Gu Q, Ogden CL. Trends in Prescription Medication Use Among Children and Adolescents-United States, 1999–2014. JAMA. 2018;319(19):2009–2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mayne SL, duRivage NE, Feemster KA, Localio AR, Grundmeier RW, Fiks AG. Effect of decision support on missed opportunities for human papillomavirus vaccination. Am J Prev Med. 2014;47(6):734–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jenssen BP, Bryant-Stephens T, Leone FT, Grundmeier RW, Fiks AG. Clinical Decision Support Tool for Parental Tobacco Treatment in Primary Care. Pediatrics. 2016;137(5). [DOI] [PubMed] [Google Scholar]
- 34.Utidjian LH, Hogan A, Michel J, et al. Clinical Decision Support and Palivizumab: A Means to Protect from Respiratory Syncytial Virus. Appl Clin Inform. 2015;6(4):769–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jacob V, Thota AB, Chattopadhyay SK, et al. Cost and economic benefit of clinical decision support systems for cardiovascular disease prevention: a community guide systematic review. J Am Med Inform Assoc. 2017;24(3):669–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gilmer TP, O’Connor PJ, Sperl-Hillen JM, et al. Cost-effectiveness of an electronic medical record based clinical decision support system. Health Serv Res. 2012;47(6):2137–2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Middleton B, Sittig DF, Wright A. Clinical Decision Support: a 25 Year Retrospective and a 25 Year Vision. Yearb Med Inform. 2016;Suppl 1:S103–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sinaiko AR, Jacobs DR Jr., Woo JG, et al. The International Childhood Cardiovascular Cohort (i3C) consortium outcomes study of childhood cardiovascular risk factors and adult cardiovascular morbidity and mortality: Design and recruitment. Contemp Clin Trials. 2018;69:55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.