Abstract
The Ministry of Health, Labour and Welfare has published the Manual of Antimicrobial Stewardship (1st edition) in June 2017 to improve the prescribing practice of antimicrobials for immunocompetent adult and pediatric (both school-aged and older children) patients. Due to the increasing demand for further promoting outpatient antimicrobial stewardship, we conducted a literature and national guideline review to identify the area of need. The results of our review revealed a high antimicrobial prescription rate in the Japanese pediatric population. Furthermore, although the Japanese clinical guidelines/guidance covered the fields of almost all infectious diseases, no system exists to estimate the incidence and treatment patterns of important infectious diseases such as asymptomatic bacteriuria, skin and soft tissue infections, and dental practices in Japan. Therefore, addressing the issues of both establishing surveillance systems and the implementation of guidelines/guidance can be the next step to promote further outpatient antimicrobial stewardship.
Keywords: antimicrobial resistance, antimicrobial stewardships, infectious disease guideline, public health
Introduction/Rationale of this review
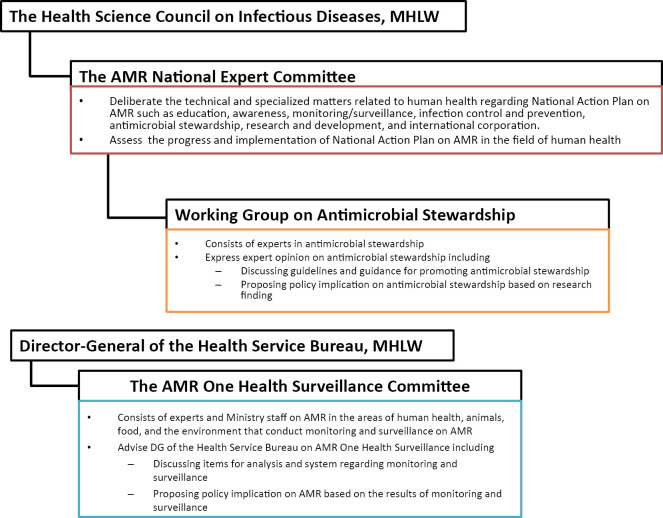
Following the publication of Japan's National Action Plan on Antimicrobial Resistance (AMR) 2016-2020 (1), the Japanese Ministry of Health, Labour and Welfare (MHLW) published the “Manual of Antimicrobial Stewardship (1st edition)” (hereinafter referred to as the Manual) to guide the judicial use of antimicrobials in the primary care setting (2). The Manual was developed by the working group on antimicrobial stewardship and approved by the AMR national expert committee and the national advisory board of infectious disease (Figure).
Figure.
Regulatory Framework for Combating Antimicrobial Resistance (AMR), The Ministry of Health, Labor and Welfare (MHLW).
The impetus for the government to issue such a downstream clinical manual was based on the alarming fact that oral antimicrobials accounted for approximately 90% of the total sales of antimicrobials in Japan and the National Action Plan targets to reduce their total use to two-thirds by 2020 using the One Health approach (1, 3-5). Similarly, of all oral antimicrobials, the third-generation cephalosporins, macrolides, and fluoroquinolones accounted for more than 75% in 2013 and those agents are also targeted to be reduced by half by 2020. Accordingly, the MHLW considered it imperative to reach out to medical providers in the outpatient setting where oral antimicrobials are often prescribed to achieve this goal (6).
The Manual focused on the two commonly experienced infectious disease conditions in the outpatient care: acute respiratory tract infection and acute diarrhea among healthy, immunocompetent adults and pediatric (both school-aged and older children) patients (2). These conditions are often self-limiting and do not require antimicrobial use. Nevertheless, antimicrobial prescription for acute respiratory tract infection is common in Japan as is the case in other developed countries (7). Therefore, the Manual provides a detailed explanation of the rationale behind the necessary and unnecessary antimicrobial prescription and provides practical patients' education materials to facilitate shared decision-making with patients and their parents for busy frontline providers (2, 6). Based on the Manual, a few interventions have been developed in different levels of healthcare system. For instance, to improve the acceptability and utilization of the Manual by providers, the digest version of the Manual was published by the MHLW (8), and a continuing medical education course using the Manual has been launched in local levels with some success in terms of their readiness to reduce their intention to prescribe unnecessary antimicrobials (9). Furthermore, at the regulatory level, antimicrobial stewardship in the outpatient setting adapting the Manual onto their practices is currently one of the requirements for facilities to claim additional fee through the national reimbursement system (10).
With further demand for expanding the fields and the targeted population of the Manual by professional societies and providers, the AMR national expert committee requested the MHLW-funded research team (11) to make a recommendation for them to discuss further direction of the Manual (12). In other words, the recommendation could assist the committee in making evidence-based decision about prioritizing areas of infectious diseases to optimize the use of antimicrobials in the outpatient setting.
Therefore, our research team investigated the infectious disease fields 1) that had not been covered by the existing national guidelines and 2) wherein unnecessary antimicrobial prescribing was often described (12). In this narrative review, we intended to share the process of analysis and its results with key stakeholders, including primary care providers including internal medicine physicians, professional societies, and importantly communities, so that we hope that the process can be more transparent and we can promote further discussion and activities to optimize outpatient antimicrobial prescribing trends in various healthcare systems.
Methods
We often ascertain the problematic antimicrobials use as “unnecessary use” or “inappropriate use” (13). The former refers to the use of antimicrobials when they are prescribed unnecessarily. “Inappropriate use,” on the other hand, implies that the selection, dose, and duration of antimicrobials are deviated from standard practice when the clinical situation compels the use of antimicrobials. As such, unnecessary use can be addressed relatively straightforward from the perspective of antimicrobial stewardship, and hence we opted to discuss the unnecessary use of antimicrobials in the current review.
1.Analysis of Japanese Guidelines
We followed the method that the MHLW-funded research report used to analyze the national infectious disease guidelines and to assess their methods, precision, and transparency (14). We explored whether there was any domestic treatment guideline in selected infectious diseases. We selected infectious diseases by referring to the infectious disease practice guidelines published by Swedish and Belgium government (15, 16). In addition to interviewing the area experts in professional societies, we used the Google Scholar Engine using terms “guideline,” “manual,” and “guidance” and also searched the homepages of Japanese academic societies regarding selected infectious diseases on November 20, 2016 and January 30 and 31, 2019, and additionally on November 28, 2019.
2.Assessment of the impact of unnecessary antimicrobial prescription on health outcomes
We searched the incidence of selected infectious diseases. To assess the impact of unnecessary antimicrobial prescription on health outcomes and the incidence of adverse events (17) derived from antimicrobial prescription, we searched the published literature, conference reports, and white papers to the MHLW in PubMed, Google Scholar, and Ichu-shi (Japan Medical Abstracts Society) (18). We selected acute upper respiratory tract infection, skin and soft tissue infection (SSTI), asymptomatic bacteriuria, and dental infection, and the corresponding Medical Subject Headings terms for English articles and their Japanese translated terms for Japanese articles were used. These infectious diseases were often described as the important clinical areas for antimicrobial stewardship in the outpatient setting (7, 19-21). Similarly, we also searched for the frequency of complications caused by the infectious diseases and the effect of antimicrobials used for preventing such complications. We conducted this search in December 2017 and January 2018 and additionally in November 2019.
Results
1.Analysis of the Japanese Guidelines
We found 21 original guidelines that cover various respiratory tract infections, urogenital tract infections, gastrointestinal tract infections, SSTIs and dental infection, and acute bacterial conjunctivitis (Table). Some guidelines covered more than one area of diseases, and the Japanese Association for Infectious Disease and the Japanese Society of Chemotherapy have published joint guidelines for the management of various infectious diseases extensively (Table); in addition, individual academic societies have developed a guideline. Among all the identified guidelines, eight (38%) required subscription fee or purchase to view the content. Overall, we found such guidelines/guidance covered the areas of major infectious diseases.
Table.
Japanese Infectious Disease Guidelines.
| Diseases | Guidelines | Published by | Published year | Link | Subscription required |
|---|---|---|---|---|---|
| Overview of the management of infectious diseases | JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y |
| Respiratory airway infections | The Japanese Respiratory Society guidelines for the management of respiratory tract infection | The Japanese Respiratory Society | 2003 | http://www.jrs.or.jp/modules/guidelines/index.php?content_id=18 | N |
| JAID/JSC Guidelines for the Treatment of Respiratory Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2014 | http://www.chemotherapy.or.jp/publications/publications.html | Y | |
| The Japanese Respiratory Society guidelines for the management of cough and sputum | The Japanese Respiratory Society | 2019 | https://www.jrs.or.jp/modules/guidelines/index.php?content_id=121 | Y | |
| Otitis media | Clinical practice guidelines for the management of serious otitis media in children | The Oto–Rhino–Laryngological Society of Japan/Japan Society for Pediatric ORL | 2015 | http://www.otology.gr.jp/guideline/img/guideline_otitis2015.pdf | N |
| Clinical practice guidelines for the diagnosis and management of acute otitis media in children in Japan | Japan Otological Society/Japan society for Pediatric ORL/Japan Society for Infection and Aerosol in Otorhinolaryngology | 2018 | https://www.otology.gr.jp/common/pdf/guideline_otitis2018.pdf | N | |
| JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y | |
| Pneumonia | JAID/JSC Guideline for the Treatment of Respiratory Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2014 | http://www.chemotherapy.or.jp/guideline/jaidjsc-kansenshochiryo_kokyuki.pdf | N |
| The Japanese Respiratory Society guidelines for the management of pneumonia in adults | The Japanese Respiratory Society | 2017 | http://www.jrs.or.jp/modules/guidelines/index.php?content_id=94 | Y | |
| Guidelines for the Management of Respiratory Infectious Diseases in Children in Japan | Japanese Society of Pediatric Pulmonology/Japan Society for Pediatric infectious Diseases | 2017 | http://eckyowa.shop16.makeshop.jp/shopdetail/000000000091/ | Y | |
| JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y | |
| COPD exacerbation | JAID/JSC Guideline for the Treatment of Respiratory Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2014 | http://www.chemotherapy.or.jp/guideline/jaidjsc-kansenshochiryo_kokyuki.pdf | N |
| The Japanese Respiratory Society guidelines for the diagnosis and treatment of COPD (5th edition) | The Japanese Respiratory Society | 2018 | https://www.jrs.or.jp/modules/guidelines/index.php?content_id=112 | Y | |
| JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y | |
| Seasonal influenza infection | JAID/JSC Guideline for the Treatment of Respiratory Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2014 | http://www.chemotherapy.or.jp/guideline/jaidjsc-kansenshochiryo_kokyuki.pdf | N |
| Guidance to seasonal influenza infection 2019–2020 season | Japan Pediatric Society | 2019 | http://www.jpeds.or.jp/uploads/files/2019-2020_influenza_all.pdf | N | |
| JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y | |
| Acute cystitis | JAID/JSC Guide to the Clinical Management of Infectious Diseases - Urinary tract infection/male genital infection | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2015 | http://www.chemotherapy.or.jp/guideline/jaidjsc-kansenshochiryo_nyouro.pdf | N |
| Clinical Guideline for the management of Obstetrics and Gynecology - Gynecology clinic setting | Japan Society of Obstetrics and Gynecology | 2017 | http://www.jsog.or.jp/activity/pdf/gl_fujinka_2017.pdf | N | |
| JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y | |
| Acute pyelonephritis; Asymptomatic bacteriuria; and Prostatitis | JAID/JSC Guide to the Clinical Management of Infectious Diseases - Urinary tract infection/male genital infection | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2015 | http://www.chemotherapy.or.jp/guideline/jaidjsc-kansenshochiryo_nyouro.pdf | N |
| JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y | |
| Epididymitis | JAID/JSC Guide to the Clinical Management of Infectious Diseases - Urinary tract infection/male genital infection | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2015 | http://www.chemotherapy.or.jp/guideline/jaidjsc-kansenshochiryo_nyouro.pdf | N |
| Guideline for the diagnosis and treatment of sexually transmitted diseases | Japanese Society for Sexually Transmitted Infections | 2016 | http://jssti.umin.jp/pdf/guideline-2016_v2.pdf | N | |
| JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y | |
| Pelvic inflammatory disease | Guideline for the diagnosis and treatment of sexually transmitted diseases | Japanese Society for Sexually Transmitted Infections | 2016 | http://jssti.umin.jp/pdf/guideline-2016_v2.pdf | N |
| Clinical Guideline for the management of Obstetrics and Gynecology - Gynecology clinic setting | Japan Society of Obstetrics and Gynecology | 2017 | http://www.jsog.or.jp/activity/pdf/gl_fujinka_2017.pdf | N | |
| JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y | |
| Bacterial vaginosis; Candida vulvovaginitis; and Genital herpes simplex virus infection | Guideline for the diagnosis and treatment of sexually transmitted diseases | Japanese Society for Sexually Transmitted Infections | 2016 | http://jssti.umin.jp/pdf/guideline-2016_v2.pdf | N |
| Clinical Guideline for the management of Obstetrics and Gynecology - Gynecology clinic setting | Japan Society of Obstetrics and Gynecology | 2017 | http://www.jsog.or.jp/activity/pdf/gl_fujinka_2017.pdf | N | |
| JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y | |
| Urethritis | Guideline for the diagnosis and treatment of sexually transmitted diseases | Japanese Society for Sexually Transmitted Infections | 2016 | http://jssti.umin.jp/pdf/guideline-2016_v2.pdf | N |
| JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y | |
| Diverticulitis | Guidelines for the management of diverticulosis | Japanese Gastroenterological Association | 2017 | https://minds.jcqhc.or.jp/docs/gl_pdf/G0001033/4/diverticulosis_of_colon.pdf | N |
| Helicobacter pylori infection | Guidelines for the diagnosis and treatment of H. pylori infection | The Japanese Society for Helicobacter Research | 2016 | http://www.sentan.com/products/detail.php?product_id=21 | Y |
| Impetigo; cellulitis; erysipelas; and infected leg ulcer | JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y |
| Diabetic foot ulcer and infection | Guideline for the management of wound, pressure ulcer, burn 3: Diabetic foot ulcer and infection | Japan Dermatological Association | 2017 | https://www.dermatol.or.jp/uploads/uploads/files/3.diabetic_ulcer_GL.pdf | N |
| JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y | |
| Animal bite | JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y |
| Dental infection | Antimicrobial therapy guideline for patients with periodontal disease | Japan Society of Periodontology | 2010 | http://www.perio.jp/publication/upload_file/jsp_guideline_antimicrobial_therapy.pdf | N |
| JSP Clinical Practice Guideline for Periodontal Treatment | Japan Society of Periodontology | 2015 | http://www.perio.jp/publication/upload_file/guideline_perio_plan2015.pdf | N | |
| JAID/JSC Guide to the Clinical Management of Infectious Diseases - Dental Infection | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2016 | http://www.chemotherapy.or.jp/guideline/jaidjsc-kansenshochiryo_shisei.pdf | N | |
| Japanese Clinical Practice Guidelines for antimicrobial prophylaxis in surgery | Japanese Society of Chemotherapy/Japan Society for Surgical Infection | 2016 | http://www.chemotherapy.or.jp/publications/publications.html#jutugo | Y | |
| JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y | |
| Bacterial conjunctivitis | JAID/JSC Guide to the Clinical Management of Infectious Diseases | The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy | 2019 | http://lifescience.co.jp/shop2/index_0190.html | Y |
JAID: Japanese Association of Infectious Disease, JSC: Japanese Society of Chemotherapy, COPD: Chronic obstructive pulmonary disease, JSP: Japan Society of Periodontology, Y: Yes, N: No
2.Assessment of the importance of unnecessary antimicrobial prescription
1.Epidemiology abroad
In the US ambulatory care 2011-2012, among 184,032 sampled visits, 12.6% involved antimicrobial prescription that translated into 506 antimicrobial prescriptions per 1,000 US population annually (7). The annual antimicrobial prescription rate was variable for age categories and geographical locations. For instance, the highest rate was observed among children aged 0 through 2 years at 1,287 prescriptions per 1,000 population, and the lowest rate was observed among adults aged 20-39 years at 397 prescriptions per 1,000 population. The southern region had the highest annual prescription rate at 553 per 1,000 population versus the western region at 423 per 1,000 population. Sinusitis, suppurative otitis media, and pharyngitis were the major indications for the antimicrobial prescription, followed by SSTIs and urinary tract infections.
SSTIs include a wide spectrum of diseases. Localized mild cellulitis and abscess can be treated in the outpatient setting, whereas severe diseases such as necrotizing fasciitis necessitate critical care and surgical debridement (22, 23). In addition, the 2014 Infectious Disease Society of America guidelines did not recommend routine antimicrobial therapy after incision and drainage for a healthy population with mild diseases (20). Alternatively, recent large randomized control studies suggested a potential benefit of adjunctive antimicrobial therapy in this population (24-26).
Asymptomatic bacteriuria refers to the identification of bacteria in an appropriately collected urine specimen from patients without symptomatic urinary tract infection (27). In addition to special clinical scenarios with pregnant patients and patients undergoing urologic procedures, the majority of patients with asymptomatic bacteriuria do not warrant antimicrobial therapy given its scarce adverse consequences. The prevalence of asymptomatic bacteriuria differs according to age, sex, comorbidities, and pregnancy. For instance, 6-7% of the female population in their 50s and 60s and 8-10% of females in their 60s and 70s were reported to have asymptomatic bacteriuria (28). In the young healthy female population, asymptomatic bacteriuria is transient, although in the elderly, it can be continuous and repetitive phenomena (29). Multicenter studies conducted in the US have revealed that 38% of patients with asymptomatic bacteriuria were treated (30). Unnecessary antimicrobial use is a plausible risk in both ambulatory and inpatient practices (31).
In the UK, dental practitioners accounted for 7-9% of community prescriptions of antimicrobials (32, 33). In Canada, from 1996 to 2013, although the overall antibiotic use declined by 13% and the proportion of physicians prescribing antibiotics declined by 18%, dental prescribing increased by 62% and its proportionate contribution increased from 6.7% to 11.3% of antimicrobial prescription (21). This information implicates the importance of understanding the current situations at both regional and national levels and perhaps require intervention for dental practices with antimicrobial stewardship (34).
According to the guidelines from US and Europe (35, 36), antimicrobial prophylaxis for the prevention of endocarditis is warranted when invasive dental procedures such as tooth extractions are involved in high-risk populations (e.g., adults with prosthetic heart valves). Questionnaire surveys conducted on dentists in Canada showed that the degree of following such guidelines was variable; some dentists may prescribe prophylactic antimicrobials to non-high-risk populations, whereas others may not prescribe prophylactic antimicrobials to high-risk populations (37, 38).
2.Epidemiology in Japan
The national claims database (the National Database for Prescription and National Health Check-up) and the sales database are the two major databases that can be used for a retrospective estimation of antimicrobial use in Japan (3, 39, 40). Regarding disease-specific antimicrobial use, we have not developed an on-time surveillance system; therefore, as an alternative, the NDB can be used as a tool to estimate the number of prescribed antimicrobials using the primary and co-diagnosis codes.
In an earlier study, it was observed that among 691 immunocompetent patients aged 15-64 years with acute respiratory tract infection, excluding influenza, who visited 5 clinics between October 2004 and April 2005, nonspecific respiratory tract infections accounted for 80%, acute rhinosinusitis 2%, acute pharyngitis 13%, and bronchitis accounted for 5% (41). When the researchers followed the ACP guideline (42), 5% of all patients required antimicrobials at the initial visit, and an additional 2% of them needed antimicrobials in the subsequent visits (41). Higashi et al. analyzed NDB data recorded between January and March 2005 and found that oral antimicrobials were prescribed to 60% of patients with nonbacterial upper respiratory tract infection (43). Third-generation cephalosporins were the highest at 46%, followed by macrolides at 27% and fluoroquinolones at 16%. More oral antimicrobial prescriptions were found in the clinics rather than inter hospitals without any significant inter-hospital or interregional differences.
The results of the more recent studies that had analyzed the NDB and an equivalent national claims database regarding outpatient antimicrobial prescribing were similar to or extend those of previous studies. Despite an overall reduction in its prescription rate, they found that inappropriate antimicrobial prescribing in nonbacterial acute respiratory tract infection and higher antimicrobial prescribing under the diagnosis of infectious diseases such as acute respiratory tract infection and gastrointestinal tract infection for which antimicrobials were rarely indicated (44, 45). Furthermore, in children (aged <15 years), there was no statistically significant change in antimicrobial prescribing between 2013 and 2016, and the antimicrobial prescription rates were the highest among those aged 1-5 years (46). In line with adults, macrolides and third-generation cephalosporins were the most commonly prescribed antimicrobials.
We found no report describing the current practice for SSTIs, including its management and antimicrobial prescribing pattern. Regarding the urogenital infection, the Japanese Association for Infectious Disease and the Japanese Society of Chemotherapy discussed about asymptomatic bacteriuria and they followed the US guideline recommendations (47). However, we found no surveillance or database addressing the burden of asymptomatic bacteriuria in the community and the use of antimicrobials for this condition in Japan.
Regarding Japanese dental practices, we found no data to describe total antimicrobial use. Nagashima et al. monitored antimicrobial use in the 18 privately funded dental university hospitals between 1983 and 2013 and found that the proportion of antimicrobial use among all prescriptions was increased from 22% to 33%, the use of oral cephalosporins was increased from 53% to 67% and that of oral penicillin declined from 33% to 23%, and oral macrolides were often prescribed in the long-term antimicrobial treatment (>7 days) (48). Amari et al. conducted a questionnaire survey on randomly selected 500 dental practitioners working in 500 Japanese urban dental facilities in 2011 (49). They found that among the 252 responders (50.4%), 46% prescribed prophylactic antimicrobials for any dental procedure, 90% responded that 3-4 days of prescription was appropriate for prophylactic antimicrobial use, 67.1% reported using antimicrobials after dental procedures but only 12% reported prescribing these prior to procedures, and third-generation cephalosporins, despite the lack of indications by guidelines (36, 50), were the most often prescribed antimicrobials for both prophylaxis and treatment (49). In a more recent survey, despite the fact that >80% of responders understood the indications of antimicrobials for infective endocarditis prophylaxis described in the guidelines, several factors, including a fear of liability, misconception, and culture, directed their unnecessary antimicrobial prescribing practices (51).
3.The frequency of complications and the impact of antimicrobial prescription on the prevention of complications
A multicenter prospective study was conducted in two tertiary and one community hospital in Canada, and among 1,529 adults presenting to the emergency department over a period of 12 months, 184 (12%) were diagnosed with adverse drug events, and the antimicrobial use within 1 week was one of the important variables that was associated with the diagnosis of adverse drug events (52). The calculated excess risk of suppurative complications of respiratory tract infections in children who did not receive an antibiotic was estimated at 3.8 per 10,000 (53). In the systematic review, no evidence of benefit from antimicrobial use was found for the common cold or for persisting acute purulent rhinitis in children or adults (54). Antimicrobials appeared to be ineffective in preventing further bacterial complications following upper respiratory tract infections (55).
Apart from specific patient populations such as pregnant patients and patients undergoing urologic procedures, treatment for asymptomatic bacteriuria does not appear to change the outcome. A prospective study conducted in the US, which followed up 358 elderly subjects for 8 years with urine cultures being analyzed every 6 months, showed no effect on mortality between the patients with asymptomatic bacteriuria who were treated and those who were not treated (31, 56). Similarly, in the randomized controlled study including institutionalized elderly subjects with asymptomatic bacteriuria, the incidence of symptomatic urinary tract infection and death was similar between the treatment group and the nontreatment group (31, 57). Rather, there was an increasing tendency of adverse drug events such as rash, diarrhea, and candidiasis in the treatment group.
When healthcare providers offered more patient education, patient satisfaction did not appear to be reduced even when antimicrobials were not prescribed to those with a diagnosis of acute respiratory tract infection (41, 58). In a similar manner, the denial of a request for antimicrobials was not associated with lower satisfaction with clinicians (59).
Discussion
The clinical guidelines and guidance published in Japan have covered the fields of almost all infectious diseases. Research conducted using sales data and NDB were useful for the estimation of total antimicrobial use in Japan, though the estimated quantity of prescribing per diagnosis and its validity may not be reliable due to the nature of the administrative claims database (e.g., lack of validation of diagnostic codes, linkage of other data sets such as microbiology databases, and granularity of clinical data) (45, 60-62). As such, at this stage, the effect of necessary and unnecessary antimicrobial use on the health outcomes can only be estimated through individual-based research.
Outside Japan, acute respiratory tract infection, SSTIs (especially antimicrobial use for localized abscess post drainage), asymptomatic bacteriuria, and dental practice have been the growing areas of focus for optimizing outpatient antimicrobial prescribing (7, 19-21). Similarly, unnecessary antimicrobial use in cases of acute respiratory tract infection and acute gastroenteritis has been well described in Japan over the past decade (41, 43, 63), and the Manual was developed to address this long-standing challenge and to propel outpatient antimicrobial stewardship forward (2). Antimicrobial use in Japan was twice more common in the outpatient setting as in the hospital setting in 2017; and the decline of antimicrobial use between 2016 and 2017 in adults and older children was smaller than that in younger children (64). Therefore, the efforts of implementing antimicrobial stewardship interventions including the Manual should be continued. Of note, the Manual excludes those patients younger than 5 years of age. Among children aged <15 years, the rate of antimicrobial prescribing was the highest among those aged 1-5 years (46). These findings have emphasized the need to address unnecessary antimicrobial use and to develop intervention for providers taking care of children.
There is an ongoing discussion on prescribing antimicrobial post incision and drainage of localized abscess to reduce treatment failure (65). We did not find a study on antimicrobial use for SSTIs in Japan, due to which we were not able to assess the validity and necessity of the prescription. Similarly, we lacked data to assess the incidence of asymptomatic bacteriuria and the frequency of antimicrobial use for this condition. With an aging population in Japan (i.e., those aged ≥65 years accounted for 25% in 2013) (66), a high prevalence of asymptomatic bacteriuria likely exists, leading to excessive unnecessary antimicrobial prescribing. Because unnecessary antimicrobial treatment of asymptomatic bacteriuria is recognized as an important contributor to promote the emergence of AMR and Clostridioides difficile infection (19), it will be increasingly important for healthcare policies to develop a system to assess the current situation in Japan.
We also lack data describing the current antimicrobial prescribing in the Japanese dental practices. According to the questionnaire survey administered to dental providers, indications, choices, and the duration of antimicrobial use for both treatment and prophylaxis for endocarditis appear to be variable (48, 49). The Japanese Society of Chemotherapy and Japan Society for Surgical Infection have published a clinical guideline for the prevention of postsurgical infection in dental practice (Table). However, in reality, the Japanese national insurance does not cover the preventive use of antimicrobials, and the degree of implementation of such guidelines is thus questionable.
In conclusion, our findings suggest that the Manual can extend the guidance to immunocompetent children aged <5 years in conjunction with the ongoing emphasis on the judicial antimicrobial use in acute respiratory tract infection and acute diarrhea in healthy adult population commonly seen by internal medicine providers. Further studies are required to develop a national system to capture the burden of SSTIs and asymptomatic bacteriuria in addition to the current antimicrobial prescribing behaviors. We understood that the heterogeneous antimicrobial prescribing behavior in the Japanese dental practices does not align with the clinical guidelines, and intervention for dental practices, such as promoting the use of penicillin in minor surgery, can be launched by implementing guidelines for dental practitioners. As there are extensive infectious disease guidelines, understanding the facilitators and the obstacles of guidelines roll out is also a crucial step for promoting further judicious and necessary use of antimicrobials.
The authors state that they have no Conflict of Interest (COI).
Financial Support
This work was funded through the Ministry of Health, Labour and Welfare (MHLW) research grant of Japan (H29-shinkougyouseishitei-005).
References
- 1. The Government of Japan. National Action Plan on Antimicrobial Resistance (AMR) 2016-2020 [Internet]. [cited 2020 Jan 10]. Available from: http://www.mhlw.go.jp/file/06-Seisakujouhou-10900000-Kenkoukyoku/0000138942.pdf
- 2. Infectious Diseases Control Division, Health Service Bureau, Ministry of Health, Labour, Welfare. Manual of Antimicrobial Stewardship (1st Edition) [Internet]. [cited 2020 Jan 10]. Available from: https://www.mhlw.go.jp/file/06-Seisakujouhou-10900000-Kenkoukyoku/0000193504.pdf
- 3. Muraki Y, Yagi T, Tsuji Y, et al. . Japanese antimicrobial consumption surveillance: First report on oral and parenteral antimicrobial consumption in Japan (2009-2013). J Glob Antimicrob Resist 7: 19-23, 2016. [DOI] [PubMed] [Google Scholar]
- 4. Infectious Diseases Control Division, Health Service Bureau, Ministry of Health, Labour, Welfare. The AMR One Health Surveillance Committee. Nippon AMR One Health Report (NAOR) [Internet]. [cited 2020 Jan 10]. Available from: https://www.mhlw.go.jp/file/06-Seisakujouhou-10900000-Kenkoukyoku/0000204347.pdf
- 5. Jindai K, McLellan RT, Takakura S, Noda H, Miyake K. Nippon AMR one health report: the first step towards multisectoral collaboration. Lancet Infect Dis 18: 1179-1180, 2018. [DOI] [PubMed] [Google Scholar]
- 6. Saito H, Noda H, Takakura S, Jindai K, Takahashi McLellan R, Asanuma K. First major practical step toward appropriate antimicrobial use by the government of Japan. Jpn J Infect Dis 72: 56-57, 2019. [DOI] [PubMed] [Google Scholar]
- 7. Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. . Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010-2011. JAMA 315: 1864-1873, 2016. [DOI] [PubMed] [Google Scholar]
- 8.Infectious Diseases Control Division, Health Service Bureau, Ministry of Health, Labour, Welfare. Manual of Antimicrobial Stewardship (1st Edition). Digest Version [Internet]. [cited 2020 Jan 10]. Available from: https://www.mhlw.go.jp/file/06-Seisakujouhou-10900000-Kenkoukyoku/tebiki_1.pdf
- 9. Yamamoto S, Gu Y, Fujitomo Y, et al. . Development and efficacy of a clinician-targeted refresher course for treating nonpneumonia respiratory tract infections. J Gen Fam Med 19: 127-132, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ministry of Health, Labour, Welfare. FY 2018 Revision of Medical Fee (Japanese only) [Internet]. [cited 2020 Jan 10]. Available from: https://www.mhlw.go.jp/file/06-Seisakujouhou-12400000-Hokenkyoku/0000198532.pdf
- 11.Ohmagari N, Jindai K, Kusama Y, Gu Y, Honda H, Assessing the field that revised Manual of Antimicrobial Stewardship can cover. Research concerning the implementation of National Action Plan on Antimicrobial Resistance (AMR). Representative Researcher: Norio Ohmagari, Grants for Research from the Ministry of Health, Labour, and Welfare of Japan, Research Project concerning Emerging and Re-emerging Infectious Diseases and Vaccination Policies FY2017 [Internet]. [cited 2020 Jan 10]. Available from: https://mhlw-grants.niph.go.jp/index.html
- 12.Infectious Diseases Control Division, Health Service Bureau, Ministry of Health, Labour, Welfare. The third AMR expert comittee meeting [Internet]. [cited 2020 Jan 10]. Available from: https://www.mhlw.go.jp/file/05-Shingikai-10601000-Daijinkanboukouseikagakuka-Kouseikagakuka/siryo4.pdf
- 13. McDonagh M, Peterson K, Winthrop K, Cantor A, Holzhammer B, Buckley DI. AHRQ Comparative Effectiveness Reviews. In: Improving Antibiotic Prescribing for Uncomplicated Acute Respiratory Tract Infections. Agency for Healthcare Research and Quality, Rockville, 2016: ES-2. [PubMed] [Google Scholar]
- 14. Gu Y. Research concerning the method facilitating appropraite antimicoribial use in the outpatient setting. Representative Researcher: Tetsuya Yagi, Grants for Research from the Ministry of Health, Labour, and Welfare of Japan, Research Project concerning Emerging and Re-emerging Infectious Diseases and Vaccination Policies FY2017 [Internet]. [cited 2020 Jan 10]. Available from: https://mhlw-grants.niph.go.jp/about.html
- 15. The Public Health Agency of Sweden. Behandlingsrekommendationer för vanliga infektioner i öppenvård (in Swedish). [Google Scholar]
- 16. Belgium Federal Public Service (Health, Food Chain Safety and Environment). antibiotiques: guide belge des traitements anti-infectieux en pratique ambulatoire (In Dutch and French) [Internet]. [cited 2020 Jan 10]. Available from: https://www.health.belgium.be/en/node/27104
- 17. World Health Organization. Quality Assurance and Safety of Medicines Team. Safety of medicines: a guide to detecting and reporting adverse drug reactions: why health professionals need to take action [Internet]. [cited 2020 Jan 10]. Available from: https://apps.who.int/iris/handle/10665/67378
- 18. Ichushi (Japan Medical Abstracts Society) [Internet]. [cited 2020 Jan 10]. Available from: https://www.jamas.or.jp/shusaishi/search/
- 19. Nicolle LE, Gupta K, Bradley SF, et al. . Clinical practice guideline for the management of asymptomatic bacteriuria: 2019 Update by the Infectious Diseases Society of America. Clin Infect Dis 68: e83-e110, 2019. [DOI] [PubMed] [Google Scholar]
- 20. Stevens DL, Bisno AL, Chambers HF, et al. . Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis 59: e10-e52, 2014. [DOI] [PubMed] [Google Scholar]
- 21. Marra F, George D, Chong M, et al. . Antibiotic prescribing by dentists has increased: why? antibiotic prescribing practices by dentists: a review. J Am Dent Assoc 147: 320-327, 2016. [DOI] [PubMed] [Google Scholar]
- 22. Miller LG, Eisenberg DF, Liu H, et al. . Incidence of skin and soft tissue infections in ambulatory and inpatient settings, 2005-2010. BMC Infect Dis 15: 362, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ki V, Rotstein C. Bacterial skin and soft tissue infections in adults: a review of their epidemiology, pathogenesis, diagnosis, treatment and site of care. Can J Infect Dis Med Microbiol 19: 173-184, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Talan DA, Mower WR, Krishnadasan A, et al. . Trimethoprim-sulfamethoxazole versus placebo for uncomplicated skin abscess. N Engl J Med 374: 823-832, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Talan DA, Moran GJ, Krishnadasan A, et al. . Subgroup analysis of antibiotic treatment for skin abscesses. Ann Emerg Med 71: 21-30, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Daum RS, Miller LG, Immergluck L, et al. . A Placebo-controlled trial of antibiotics for smaller skin abscesses. N Engl J Med 376: 2545-2555, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis 40: 643-654, 2005. [DOI] [PubMed] [Google Scholar]
- 28. Nicolle LE. Asymptomatic bacteriuria: when to screen and when to treat. Infect Dis Clin North Am 17: 367-394, 2003. [DOI] [PubMed] [Google Scholar]
- 29. Rodhe N, Lofgren S, Matussek A, et al. . Asymptomatic bacteriuria in the elderly: high prevalence and high turnover of strains. Scand J Infect Dis 40: 804-810, 2008. [DOI] [PubMed] [Google Scholar]
- 30. Grein JD, Kahn KL, Eells SJ, et al. . Treatment for positive urine cultures in hospitalized adults: a survey of prevalence and risk factors in 3 medical centers. Infect Control Hosp Epidemiol 37: 319-326, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Daniel M, Keller S, Mozafarihashjin M, Pahwa A, Soong C. An implementation guide to reducing overtreatment of asymptomatic bacteriuria. JAMA Intern Med 2017. [DOI] [PubMed] [Google Scholar]
- 32. Karki AJ, Holyfield G, Thomas D. Dental prescribing in Wales and associated public health issues. Br Dent J 210: E21, 2011. [DOI] [PubMed] [Google Scholar]
- 33. Sweeney LC, Dave J, Chambers PA, Heritage J. Antibiotic resistance in general dental practice--a cause for concern? J Antimicrob Chemother 53: 567-576, 2004. [DOI] [PubMed] [Google Scholar]
- 34. Dar-Odeh NS, Abu-Hammad OA, Al-Omiri MK, Khraisat AS, Shehabi AA. Antibiotic prescribing practices by dentists: a review. Ther Clin Risk Manag 6: 301-306, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Habib G, Hoen B, Tornos P, et al. . Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer. Eur Heart J 30: 2369-2413, 2009. [DOI] [PubMed] [Google Scholar]
- 36. Wilson W, Taubert KA, Gewitz M, et al. . Prevention of Infective Endocarditis. Guidelines from the American Heart Association. A Guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation 116: 1736-1754, 2007. [DOI] [PubMed] [Google Scholar]
- 37. Jain P, Stevenson T, Sheppard A, et al. . Antibiotic prophylaxis for infective endocarditis: knowledge and implementation of American Heart Association Guidelines among dentists and dental hygienists in Alberta, Canada. J Am Dental Assoc (1939) 146: 743-750, 2015. [DOI] [PubMed] [Google Scholar]
- 38. Lodi G, Figini L, Sardella A, Carrassi A, Del Fabbro M, Furness S. Antibiotics to prevent complications following tooth extractions. Cochrane Database Syst Rev 11: Cd003811, 2012. [DOI] [PubMed] [Google Scholar]
- 39. Ministry of Health, Labour, Welfare. Information for National Database for Prescription and National Health Check-up [Internet]. [cited 2020 Jan 10]. Available from: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/iryouhoken/reseputo/index.html
- 40. Yamasaki D, Tanabe M, Muraki Y, Kato G, Ohmagari N, Yagi T. The first report of Japanese antimicrobial use measured by national database based on health insurance claims data (2011-2013): comparison with sales data, and trend analysis stratified by antimicrobial category and age group. Infection 46: 207-214, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Tomii K, Matsumura Y, Maeda K, Kobayashi Y, Takano Y, Tasaka Y. Minimal use of antibiotics for acute respiratory tract infections: validity and patient satisfaction. Intern Med 46: 267-272, 2007. [DOI] [PubMed] [Google Scholar]
- 42. Gonzales R, Bartlett JG, Besser RE, Hickner JM, Hoffman JR, Sande MA. Principles of appropriate antibiotic use for treatment of nonspecific upper respiratory tract infections in adults: background. Ann Intern Med 134: 490-494, 2001. [DOI] [PubMed] [Google Scholar]
- 43. Higashi T, Fukuhara S. Antibiotic prescriptions for upper respiratory tract infection in Japan. Intern Med 48: 1369-1375, 2009. [DOI] [PubMed] [Google Scholar]
- 44. Kimura Y, Fukuda H, Hayakawa K, et al. . Longitudinal trends of and factors associated with inappropriate antibiotic prescribing for non-bacterial acute respiratory tract infection in Japan: a retrospective claims database study, 2012-2017. PLoS One 14: e0223835, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hashimoto H, Saito M, Sato J, et al. . Indications and classes of outpatient antibiotic prescriptions in Japan: a descriptive study using the national database of electronic health insurance claims, 2012-2015. Int J Infect Dis 91: 1-8, 2019. [DOI] [PubMed] [Google Scholar]
- 46. Kinoshita N, Morisaki N, Uda K, Kasai M, Horikoshi Y, Miyairi I. Nationwide study of outpatient oral antimicrobial utilization patterns for children in Japan (2013-2016). J Infect Chemother 25: 22-27, 2019. [DOI] [PubMed] [Google Scholar]
- 47. JAID/JSC Guidelines for the Treatment of Urinary Track Infection/Male Genital Infection: The Japanese Association for Infectious Diseases/Japanese Society of Chemotherapy - The JAID/JSC Guide to Clinical Management of Infectious Disease/Guideline-preparing Committee Urinary Track Infection/Male Genital Infection WG [Internet]. [cited 2020 Jan 10]. Available from: http://www.kansensho.or.jp/uploads/files/guidelines/guideline_JAID-JSC_2015_urinary-tract.pdf
- 48. Nagashima T, Shoji T, Nakamura I, Endo T, Yonezawa Y, Takeno T. Multicenter surveillance study on the use of antibacterial agents at 18 private dental university hospitals in Japan. Shika Yakubutsu Ryoho (Oral Ther Pharmacol) 35: 16-26, 2016. (in Japanese, Abstract in English). [Google Scholar]
- 49. Amari Y, Uehara Y, Watanabe Y, et al. . Status of antimicrobial use among dentists in Japan. J Gen Hosp Med 6: 8-15, 2014. [Google Scholar]
- 50. The Japanese Circulation Society. Guidelines for Prevention and Treatment of Infective Endocarditis (JCS 2017) [Internet]. [cited 2020 Jan 10]. Available from: http://www.j-circ.or.jp/guideline/pdf/JCS2017_nakatani_h.pdf [DOI] [PubMed]
- 51. Kano Y, Tagashira Y, Kobayashi D, Honda H. Dentists' perceptions of antimicrobial use for dental procedures. Infect Control Hosp Epidemiol 40: 1081-1083, 2019. [DOI] [PubMed] [Google Scholar]
- 52. Hohl CM, Badke K, Zhao A, et al. . Prospective validation of clinical criteria to identify emergency department patients at high risk for adverse drug events. Acad Emerg Med 8: 13407, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Keith T, Saxena S, Murray J, Sharland M. Risk-benefit analysis of restricting antimicrobial prescribing in children: what do we really know? Curr Opin Infect Dis 23: 242-248, 2010. [DOI] [PubMed] [Google Scholar]
- 54. Kenealy T, Arroll B. Antibiotics for the common cold and acute purulent rhinitis. Cochrane Database Syst Rev 2013: CD000247, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Cars T, Eriksson I, Granath A, et al. . Antibiotic use and bacterial complications following upper respiratory tract infections: a population-based study. BMJ Open 7: e016221, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Abrutyn E, Mossey J, Berlin JA, et al. . Does asymptomatic bacteriuria predict mortality and does antimicrobial treatment reduce mortality in elderly ambulatory women? Ann Intern Med 120: 827-833, 1994. [DOI] [PubMed] [Google Scholar]
- 57. Nicolle LE, Mayhew WJ, Bryan L. Prospective randomized comparison of therapy and no therapy for asymptomatic bacteriuria in institutionalized elderly women. Am J Med 83: 27-33, 1987. [DOI] [PubMed] [Google Scholar]
- 58. Harris AM, Hicks LA, Qaseem A. Appropriate antibiotic use for acute respiratory tract infection in adults: advice for high-value care from the American College of Physicians and the Centers for Disease Control and Prevention. Ann Intern Med 164: 425-434, 2016. [DOI] [PubMed] [Google Scholar]
- 59. Jerant A, Fenton JJ, Kravitz RL, et al. . Association of clinician denial of patient requests with patient satisfaction. JAMA Intern Med 178: 85-91, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. van Walraven C, Bennett C, Forster AJ. Administrative database research infrequently used validated diagnostic or procedural codes. J Clin Epidemiol 64: 1054-1059, 2011. [DOI] [PubMed] [Google Scholar]
- 61. Yamana H, Moriwaki M, Horiguchi H, Kodan M, Fushimi K, Yasunaga H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol 27: 476-482, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Koram N, Delgado M, Stark JH, Setoguchi S, de Luise C. Validation studies of claims data in the Asia-Pacific region: a comprehensive review. Pharmacoepidemiol Drug Saf 28: 156-170, 2019. [DOI] [PubMed] [Google Scholar]
- 63. Hashimoto H, Matsui H, Sasabuchi Y, et al. . Antibiotic prescription among outpatients in a prefecture of Japan, 2012-2013: a retrospective claims database study. BMJ Open 9: e026251, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. AMR Clinical Reference Center. Surveillance of Antimicrobial Use Based on National Database for Prescription and National Health Check-up [Internet]. [cited 2020 Jan 30]. Available from: http://amrcrc.ncgm.go.jp/surveillance/010/20181128172333.html
- 65. Gottlieb M, DeMott JM, Hallock M, Peksa GD. Systemic antibiotics for the treatment of skin and soft tissue abscesses: a systematic review and meta-analysis. Ann Emerg Med 73: 8-16, 2019. [DOI] [PubMed] [Google Scholar]
- 66. OECD, Elderly Population [Internet]. [cited 2020 Jan 10]. Available from: https://data.oecd.org/pop/elderly-population.htm