Abstract
We report an unusual case of acute myocardial infarction in a high school girl. The patient was 17 years of age and had multiple coronary risk factors, including marked obesity with a body mass index (BMI) of 42.7 kg/m2, dyslipidemia and glucose intolerance. She had been an on and off smoker since she was 13 years of age. Due to the recent Westernization of the lifestyle, the prevalence of metabolic syndrome in the young generation has been increasing in Japan. Cardiovascular disease based on lifestyle-related diseases may become more common in young people.
Keywords: obesity, acute myocardial infarction, metabolic syndrome, percutaneous coronary intervention
Introduction
Recent Westernization of the Japanese lifestyle has increased the incidence of lifestyle-related diseases. Hypertension, dyslipidemia, diabetes mellitus and arteriosclerosis are known to be related to obesity. Obesity in adolescence has the potential to exacerbate these cardiovascular risk factors. We herein report a case of acute myocardial infarction (AMI) in a high-school girl with multiple cardiovascular risk factors.
Case Report
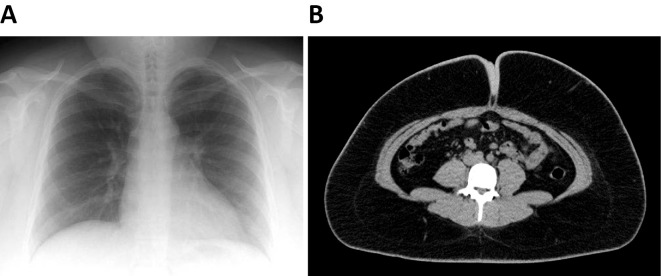
A 17-year-old high-school girl visited the emergency department of our hospital due to chest pain. The first onset of the symptom occurred at 4 P.M. while she was participating in karaoke, and it had shown no improvement when she arrived at the hospital at 8 P.M. She had no previous history of significant illness, but had several coronary risk factors, including obesity, dyslipidemia and glucose intolerance. She had been an on and off smoker since 13 years of age. Her body weight was 112 kg and her BMI was 42.7 kg/m2. A physical examination revealed the following findings: blood pressure (BP), 132/87 mmHg; heart rate, 82 beats/min; oxygen saturation, 98% on room air; respiratory rate, 17 beats/min; and body temperature, 36.9℃. Auscultation revealed no chest murmur or no lung rales. An electrocardiogram showed ST elevation in leads I, aVL, V2-6 (Fig. 1) and an echocardiogram showed akinesis of the anterior wall in the apical area. A chest X-ray showed a 56.7% cardiothoracic ratio without lung congestion or effusion (Fig. 2A). Fast tests for troponin T and human fatty acid binding protein were positive. The laboratory findings included a creatine kinase (CK) level of 532 U/L, and a creatine kinase MB fraction (CKMB) of 30 U/L. Her low-density lipoprotein (LDL) cholesterol level was high at 171.8 mg/dL, and her high-density lipoprotein (HDL) cholesterol level was low at 35.0 mg/dL; her serum triglyceride (TG) level was 158 mg/dL. Her serum uric acid (UA) level was 8.5 mg/dL and her HbA1c value was 6.0%. Indicators of the blood coagulation function were normal. Computed tomography (CT), showed no other specific findings for chest pain; however, serious visceral obesity was present (her subcutaneous fat area was 586.2 cm2 and her V/S ratio was 0.19). The abdominal visceral fat area was 113.6 (≥100) cm2 (Fig. 2B).
Figure 1.
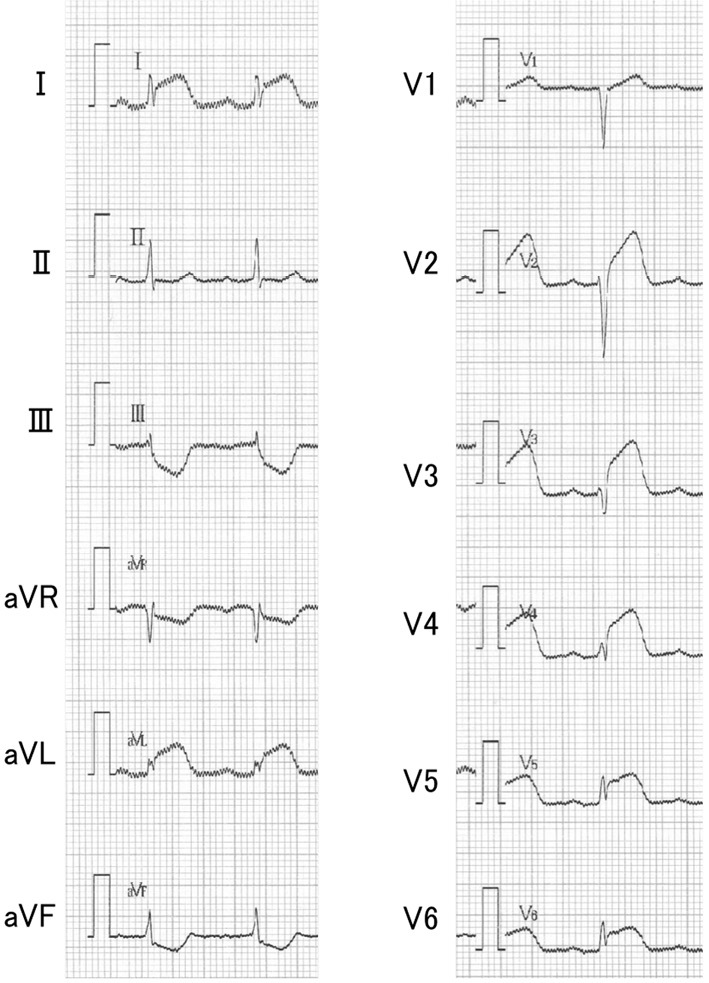
Electrocardiogram in the emergency room. ST elevation was evident in leads I, aVL, and V2-6.
Figure 2.
(A) Chest X-ray: The cardiothoracic ratio was 56.7% without lung congestion or effusion, but with a thick soft tissue shadow in extra-thoracic area. (B) Abdominal computerized tomography (CT): The abdominal visceral fat area was 113.6 cm2 and the subcutaneous fat area was 586.2 cm2.
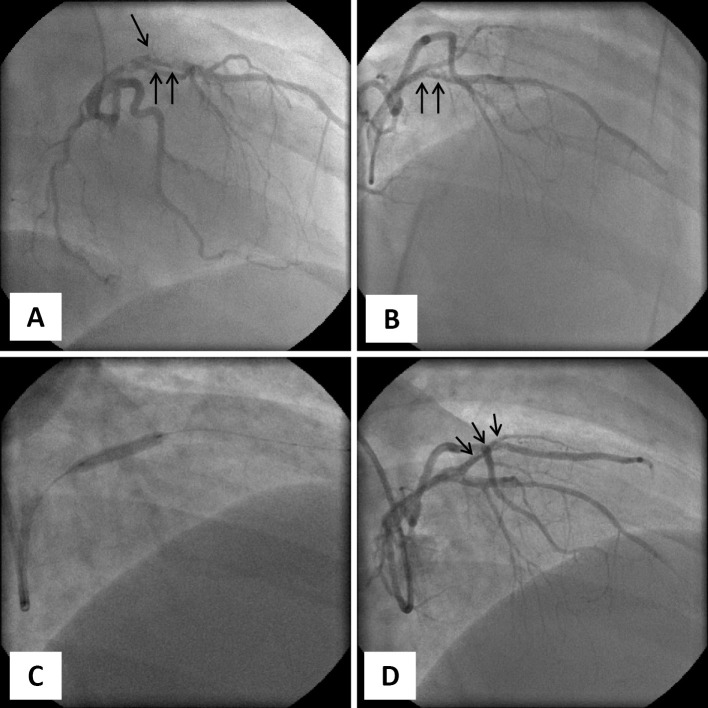
Emergent coronary angiography (CAG) revealed total occlusion at the ostium of the diagonal branch and severe stenosis at the mid-left anterior descending artery (LAD) with a typical filling defect image, suggesting floating thrombi on the left CAG (Fig. 3A, B). Unfortunately, there were no intravascular imaging data in this case. At the onset of AMI in the present case, which was in 2009, intravascular imaging was not routinely available for emergency cases at our hospital.
Figure 3.
(A) (B): CAG of left coronary artery: severe stenosis in the mid-LAD (↑↑) and total occlusion at the diagonal branch (↓) [(A) RAO 30°, (B) RAO 30°, Cranial 30°], (C): PCI at the LAD lesion, (D): The final view of CAG: The LAD lesions were successfully dilated and the stent (↓) was successfully placed. CAG: coronary angiography, RAO: right anterior oblique position, PCI: percutaneous coronary intervention, LAD: left anterior descending coronary artery
Percutaneous coronary intervention (PCI) was performed to treat the lesions (Fig. 3C). Two guidewires were smoothly advanced to the distal LAD and diagonal branch. Next, thrombus aspiration was performed; only small white debris and thrombi were aspirated. An OTTIMO ROSSO balloon catheter 2.5×20 mm (Kaneka Medics) was inflated at the lesions. We found a remaining stenotic lesion, which being a newly formed thrombus disturbed the optimal blood flow. Finally, stenting was reluctantly selected as a bailout measure. We chose a bare-metal stent (BMS) according to the standard consensus for stent selection for AMI in 2009. A Liberte BMS 3.0×16 mm (Boston Scientific) was implanted at the lesion of the diagonal branch. Finally, a Ryujin Plus balloon catheter 3.0×20 mm (TERUMO) was inflated to dilate the LAD lesion and to set the stent. The final angiogram revealed some small debris of thrombi remaining at the LAD lesion; however, the lesion and stent were successfully dilated (Fig. 3D). The peak CK and CKMB levels were 2,929 U/L and 270 U/L, respectively. Following the intervention procedure, aspirin (100 mg), clopidogrel (75 mg) and cilostazol (200 mg) were administered daily and heparin (25,000 U/day) was continued for 5 days. In addition, rosuvastatin (2.5 mg) was administered to treat dyslipidemia and valsartan (40 mg) was administered to prevent cardiac remodeling.
123I-BMIPP on day 11 after percutaneous coronary intervention (PCI) showed a severely low uptake in the anterior to lateral areas of the left ventricle, which was compatible with AMI of the LAD and diagonal branch. On echocardiography, global contraction was relatively preserved, despite hypokinesis of the anterior wall. Polysomnography (PSG) showed an apnea hypopnea index (AHI) of 41.8, indicating a severe grade of obstructive sleep apnea. She was treated with dietary measures for obesity and continuous positive airway pressure (CPAP) for obstructive sleep apnea. Follow up CAG on day 36 revealed no significant stenosis at the PCI site and no new lesions. She was discharged on day 38 following a period of rehabilitation.
Following her discharge, she made huge changes to her lifestyle. The changes included strict dietary restriction. After 8 months, follow-up CAG revealed a stable condition at the PCI sites. She achieved a 40 kg body weight reduction. This was accompanied by normalization of her HbA1c, lipid profile and UA levels. She gave up smoking. She has not experienced any other coronary events and has not developed any major cardiovascular diseases during 10 years of follow-up.
Discussion
The present case, which involved a 17-year-old high-school girl, is unusual, and represents the youngest-ever case of AMI in a patient with multiple atherosclerotic coronary risk factors. This case may reflect the increasing prevalence of metabolic syndrome (MetS) as a cause of cardiovascular disease in young people. There is little data available regarding AMI in young adults, except in relation to immunological or infectious diseases, such as Kawasaki disease.
A previous paper reported that young patients with acute coronary syndrome (ACS) account for 2-10% of all AMI cases (1). Most young ACS cases are men; women account only for approximately 25% of the patient population (2, 3). The prevalence of ischemic heart disease among young women in European countries (≤45 years of age) is <1.1% (4). The most common causes of ACS in young women include congenital or anatomical abnormalities of vessels, the presence of a myocardial bridge, vascular dissection, vascular spasms and inflammatory vegetation (1, 5-7). In pediatric medicine, the most common causes of AMI are reported to anomalous origin of coronary artery and Kawasaki disease (8-10).
Recently, the pathogenesis of coronary artery disease seems to vary. In a total of 363 cases of AMI (mean age, 64.2 years in males and 69.4 years in females) during ten years at our hospital, 13 cases (3.6%) involved patients of ≤40 years of age (Table). Of note, all of these young AMI patients had at least two or more coronary risk factors, with the exception of case No. 3, a 19-year-old woman in whom AMI was caused by injuries sustained in a traumatic traffic accident (11) (Table). As shown in Table, the patient in the present case (No. 6), a 17-year-old high-school girl, had many coronary risk factors, including on and off smoking. Osaki et al. reported on smoking behavior among a total of 106,297 junior-high and high-school students in Japan (12). According to their report, 22.5% of boys and 10.8% of girls had tried smoking at least once. To our surprise, 7.5% of boys and 3.8% of girls continued smoking and were current smokers (12).
Table.
AMI Cases in Young Patients (≤ 40 Years) in Our Hospital during These 10 Years
| No. | Age | Sex | Culprit | BMI | HT | DM | DLP | Smoking | SAS |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 33 | M | RCA | 33.8 | + | - | + | - | + |
| 2 | 37 | M | LCX | 28.1 | - | - | + | + | - |
| 3 | 19 | F | RCA | 20.5 | - | - | - | - | - |
| 4 | 35 | M | LAD | 29.4 | + | + | + | + | - |
| 5 | 40 | M | LAD | 22.4 | + | - | + | + | - |
| 6 | 17 | F | LAD | 41.9 | - | ± | + | + | + |
| 7 | 38 | M | RCA | 27.4 | - | + | + | + | + |
| 8 | 40 | M | RCA | 26.5 | + | + | + | + | + |
| 9 | 40 | M | LCX | 29.0 | + | - | + | + | + |
| 10 | 36 | F | RCA | 26.8 | + | + | + | + | + |
| 11 | 40 | M | LCX | 25.1 | + | + | + | + | - |
| 12 | 38 | M | RCA | 33.2 | + | - | + | + | - |
| 13 | 37 | M | RCA | 26.3 | + | - | + | - | - |
No 3: a case caused by traumatic injury (Ref 11). No 6: the present case. AMI: acute myocardial infarction, Culprit: culprit lesion in coronary arteries, BMI: body mass index, HT: hypertension, DM: diabetes mellitus, DLP: dyslipidemia, SAS: sleep apnea syndrome
Recently, childhood obesity is becoming a worldwide epidemiological problem. The global prevalence of obesity has increased markedly: more than 41 million children under five years of age were classified as overweight in 2016 (WHO website https://www.who.int/dietphysicalactivity/childhood/en/). Concomitantly, with the increasing prevalence of childhood obesity, the prevalence of MetS is increasing among children and adolescents (13, 14). MetS is the disease concept based on visceral fat obesity merging with dyslipidemia, hypertension, and carbohydrate metabolic disorder. The Japanese Ministry of Health, Labor and Welfare announced the diagnostic criteria for childhood MetS in 2010. These criteria were stricter than the International Diabetes Federation criteria.
The Japanese criteria for childhood MetS include an essential component of central obesity, a waist circumference (WC) of ≥75 cm for elementary-school students and WC ≥80 cm for junior-high-school students or a weight-height ratio ≥0.5. The diagnosis of childhood MetS requires two or more of the following three factors, in addition to central obesity. The first one is increased BP (systolic BP ≥125 mmHg and/or diastolic BP ≥75 mmHg). The second is increased TG (≥120 mg/dL) and/or decreased HDL (<40 mg/dL). The third is an increased fasting glucose level (≥100 mg/dL).
The prevalence of MetS has been reported to be 0.2-2% in all children and in 10-35% in overweight children in Japan (15). Iwashima et al. also reported that an increase in WC was related to the cardiovascular risk in Japanese adolescents (16). They concluded that WC was the most sensitive marker for the detection of arterial elasticity, even in school-age children (16). In general, subjects with MetS have a significantly greater probability of experiencing AMI or stroke events in comparison to those without MetS (17, 18). It is essential to overcome MetS in children and adolescents not only for the prevention of future cardiovascular disease, but also to prevent these conditions from arising in childhood and adolescence.
Conclusion
We reported an unusual case of AMI in a 17-year-old high-school girl. Cardiovascular events may become more common with young people in the near future; thus, attempts to prevent MetS are crucial.
The authors state that they have no Conflict of Interest (COI).
Satoshi Kawaguchi and Tomomi Hasebe contributed equally to this work.
References
- 1. Maciej B. Acute coronary syndromes in young women - the scale of the problem and the associated risks. Kardiochir Torakochirurgia Pol 12: 134-138, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Doughty M, Mehta R, Bruckman D, et al. Acute myocardial infarction in the young - The University of Michigan experience. Am Heart J 143: 56-62, 2002. [DOI] [PubMed] [Google Scholar]
- 3. Chua SK, Hung HF, Shyu KG, et al. Acute ST-elevation myocardial infarction in young patients: 15 years of experience in a single center. Clin Cardiol 33: 140-148, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Egred M, Viswanathan G, Davis GK. Myocardila infarction in young adults. Postgrad Med J 81: 741-745, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Stefan M, Waldemar H, Junbo G, Raimund E. Update on myocardial bridging. Circulation 106: 2616-2622, 2002. [DOI] [PubMed] [Google Scholar]
- 6. Vrints CJ. Spontaneous coronary artery dissection. Heart 96: 801-808, 2010. [DOI] [PubMed] [Google Scholar]
- 7. Hung MJ, Hu P, Hung MY. Coronary artery spasm: review and update. Int J Med Sci 11: 1161-1171, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kato H, Sugimura T, Akagi T, et al. Long-term consequences of Kawasaki disease. A 10- to 21-year follow-up study of 594 patients. Circulation 94: 1379-1385, 1996. [DOI] [PubMed] [Google Scholar]
- 9. David SC, Gray FS, Robert HG, John MC. Myocardial infarction in childhood: clinical analysis of 17 cases and medium term follow up of survivors. Br Heart J 65: 332-336, 1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Newburger JW, Takahashi M, Gerber MA, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation 110: 2747-2771, 2004. [DOI] [PubMed] [Google Scholar]
- 11. Ota H, Tashiro N, Nakagawa N, et al. Spontaneous resolution of an accidental total coronary occlusion. Intern Med 49: 2593-2597, 2010. [DOI] [PubMed] [Google Scholar]
- 12. Osaki Y, Tanihata T, Ohhida T, et al. Adolescent smoking behaviour and cigarette brand preference in Japan. Tobacco Control 15: 172-180, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pacifico L, Anania C, Nartino F, et al. Management of metabolic syndrome in children and adolescents. Nutr Metab Cardiovasc Dis 21: 455-459, 2011. [DOI] [PubMed] [Google Scholar]
- 14. Martino F, Pannarele G, Puddu PE, et al. It is possible a new definition of metabolic syndrome in childfood? Eur Rev Med Pharmacol Sci 19: 4324-4331, 2015. [PubMed] [Google Scholar]
- 15. Kubo T. Common approach to childhood obesity in Japan. Pediatar Endocr Met 27: 581-592, 2014. [DOI] [PubMed] [Google Scholar]
- 16. Iwashima S, Nakagawa Y, Ishikawa T, et al. Abdominal obesity is associated with cardiovascular risk in Japanese children and adolescents. J Pediatr Endocr Met 24: 51-54, 2011. [DOI] [PubMed] [Google Scholar]
- 17. Laura K, Jurate B, Antanas N. Metabolic syndrome related to cardiovascular events in a 10-year prospective study. Diabetol Metab Synd 7: 102-108, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Khosravi-Boroujeni H, Ahmed F, Sadeghi M, et al. Does the impact of metabolic syndrome on cardiovascular events vary by using different definitions? BMC Public Health 15: 1313-1340, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]