Abstract
Background
Coronavirus disease 2019 (COVID-19) has spread rapidly across the world. Tunisia reacted early to COVID-19, resulting in a low number of infections during the first wave of the pandemic. This study was performed to model the effects of different interventions on the evolution of cases and to compare these with the Tunisian experience.
Methods
A stochastic transmission model was used to quantify the reduction in number of cases of COVID-19 with the interventions of contact tracing, compliance with isolation, and a general lockdown.
Results
In the model, increasing contact tracing from 20% to 80% after the first 100 cases reduced the cumulative number of infections (CNI) by 52% in 1 month. Similarly, increased compliance with isolation from 20% to 80% after the first 100 cases reduced the CNI by 45%. These reductions were smaller if the interventions were implemented after 1000 cases. A general lockdown reduced the CNI by 97% after the first 100 cases. Tunisia implemented its general lockdown after 75 cases were confirmed, which reduced the cumulative number of infected cases by 86% among the general population.
Conclusions
This study shows that the early application of critical interventions contributes significantly to reducing infections and the evolution of COVID-19 in a country. Tunisia’s early success with the control of COVID-19 is explained by its quick response.
Keyword: COVID-19, Modelling, Contact tracing, Isolation, General lockdown, Tunisia
Introduction
Since first being recognized in late December 2019, coronavirus disease 2019 (COVID-19) has spread rapidly across the world (WHO, 2020a, WHO, 2020b). It has caused huge mortality and morbidity in numerous countries, and as of August 10, 2020, a total of 19 718 030 cases of infection and 728 013 deaths had been reported (WHO, 2020c). Almost all countries and territories across the world have had COVID-19 cases. However, there have been significant differences in the trends and experience of different countries: as of August 10, 2020, a total of 10 590 929 cases of infection had been reported in the Americas, 3 582 911 in Europe, 1 644 359 in the Eastern Mediterranean region, 370 621 in the Western Pacific region, 2 632 773 in South Asia, and 895 696 in Africa (WHO, 2020c). Similarly, there have been variations in the case fatality rate, with rates of 2.6% in the Eastern Mediterranean, 1.9% in Africa regions, and 6.0% in Europe. At the global level, the rate is 3.7% (WHO, 2020c).
In addition to clinical interventions, non-pharmaceutical interventions (NPIs) that aim to interrupt or reduce transmission are essential to combat COVID-19 (Guidelines for non-pharmaceutical interventions, 2020, Calibrating long-term non-pharmaceutical interventions, 2020, COVID19 strategy update, 2020). Major NPIs recommended at the international level to control COVID-19 have been to give priority to active and exhaustive case detection, immediate isolation of COVID-19 patients, carefully monitoring of contacts, and mandatory quarantine for all inbound travelers from countries with significant transmission of COVID-19 (Report of the WHO-China Joint Mission on Coronavirus Disease, 2019). Many countries have also imposed general lockdowns to limit the increases in cases during critical phases, especially in relation to health system capacity.
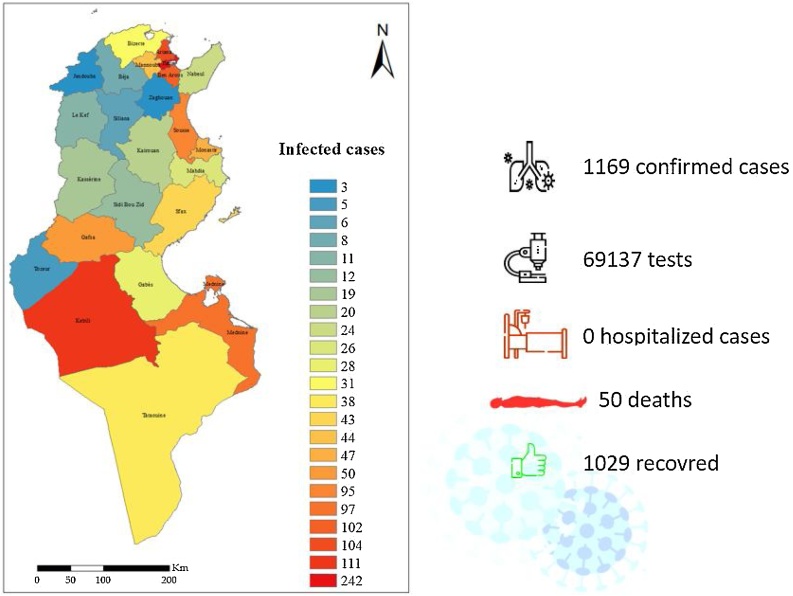
Tunisia stands out as an interesting example as a result of its relatively small burden from COVID-19 in the first few months of the global pandemic. Indeed, despite its close connections to Europe, Tunisia was relatively well protected from COVID-19, since the first case was imported from Italy on March 2, 2020. The number of cases increased slowly for a while, and a few clusters of infections eventually emerged (Observatoire national des maladies nouvelles et émergentes, 2020a). However, large-scale community transmission was avoided, and up until June 27, 2020, the date on which the borders were opened, only 1169 cases had been confirmed. There were 50 deaths due to COVID-19 during this period (Observatoire national des maladies nouvelles et émergentes, 2020b).
This study was performed to examine the impact of specific NPIs, i.e. contact tracing, isolation, and lockdown, in reducing the number of COVID-19 cases through applying an existing model. This model was then adapted to take into account the specificities of the Tunisian population, as well as its epidemiological status. The findings from this study will help assess different possible control interventions and mathematical models in relation to real-world experience.
Methods
Drawing on the methodology proposed by researchers at the Centre for Mathematical Modelling of Infectious Diseases, London School of Hygiene and Tropical Medicine, UK, a stochastic transmission model based on a branching process or Bienaymé–Galton–Watson process was used to quantify the impact of contact tracing, compliance with isolation, and lockdown in reducing the number of cases infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of COVID-19 (Hellewell et al., 2020a). Under ideal circumstances, due to effective isolation after the appearance of symptoms and full contact tracing, there would be no secondary infections.
In this model, the number of potential secondary cases produced by each individual is drawn from a negative binomial distribution branching process. In this study, the level of overdispersion in COVID-19 transmission was estimated by using a mathematical model that is characterized by the basic reproduction number R0 and the overdispersion parameter k of a negative binomial branching process, as described by Hellewell et al. (2020a).
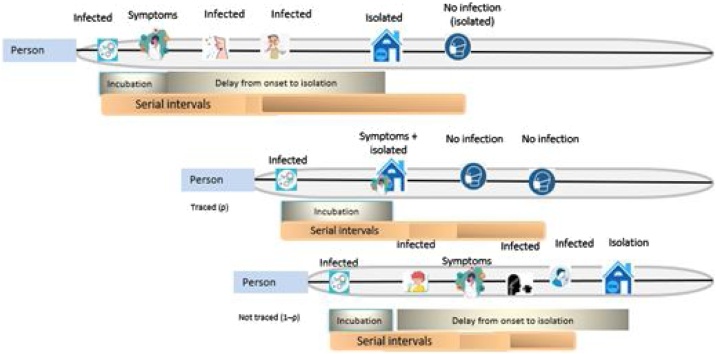
The simulated process begins with an infected person. After an incubation period, the person shows symptoms and is isolated at time t. A person infected with the virus could potentially produce secondary infections, with some transmissions occurring before the case is isolated, either due to contact tracing or due to the appearance of symptoms. Thus, in the model, a reduced delay between onset and isolation would reduce the average number of secondary cases. The model also takes into account the possibility of asymptomatic transmission (Figure 1).
Figure 1.
Structure of the model.
The possible delays between the onset of symptoms and isolation were based on the later stages of the 2003 severe acute respiratory syndrome (SARS) epidemic in Singapore and the first phase of the COVID-19 epidemic in Wuhan (Donnelly et al., 2003, Li et al., 2020). The incubation period for each case was taken from a Weibull distribution. A corresponding serial interval for each case was then drawn from an asymmetric normal distribution. The other main modelling parameters were a dispersion parameter of 0.16, as used in the original model, and a 15% probability of transmission before the onset of symptoms, due to emerging evidence in this area (Yu et al., 2020, Lloyd-Smith et al., 2005).
Using this model, varying scenarios were assumed according to several parameters, namely the initial number of cases, the reproduction rate (Rt), the percentage of contacts traced, and the efficacy of isolation. According to the literature, the Rt is 4 for scenario 0 without interventions and 0.5 after the application of NPIs (Funk et al., 2020). Other assumptions about NPIs were made as specified in the paper. Regarding the Rt after isolation, it was assumed that this was proportional to the percentage of people respecting the NPIs and of the effectiveness of isolation. Rt in the community was further modified to assess the effect of general lockdown, and was assumed to be 0.5 (Talmoudi et al., 2020). One thousand simulations were run under each scenario (Table 1).
Table 1.
Parameters of the overall models.
| Initial number of cases | Rt community | Efficacy of isolation | Rt after isolation | % of contacts tracing | |
|---|---|---|---|---|---|
| Model I | (i) 100 | 4 | 100% | 0 | 20% to 100% |
| Impact of the contact tracing | (ii) 1000 | ||||
| Model II | (i) 100 | 4 | 0% | 4 | 60% |
| Impact of compliance with isolation | (ii) 1000 | 25% | 3 | ||
| 50% | 2 | ||||
| 75% | 1 | ||||
| 100% | 0 | ||||
| Model III | (i) 100 | Rt before lockdown = 4 | 100% | 0 | 60% |
| Impact of the lockdown | (ii) 1000 | Rt after lockdown = 0.5 | |||
| (iii) 10 000 |
Rt, reproduction rate.
The model was then adapted to take into account individual characteristics of the population linked to the severity of infection. The following characteristics relevant to COVID-19 were included: age, hypertension, diabetes, dyslipidemia, chronic obstructive pulmonary disease, and smoking. The inclusion of the distribution of the population by age and the prevalence of having at least one chronic disease or being a smoker in the model was based on the proportion of each group in the general population and the probability of being infected in the observed serial in Tunisia (Institut National de la Statistique, 2018, Saidi et al., 2019).
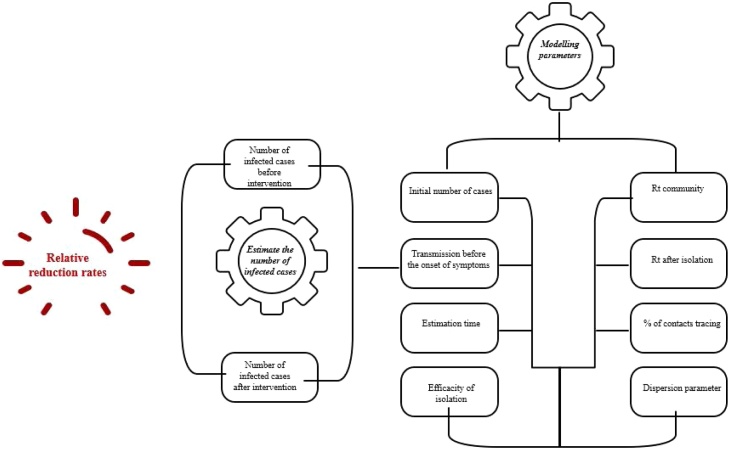
The model was then re-run with Tunisian population data and using the country’s actual number of cases before lockdown and the reproduction rate (Figure 2). Once again, 1000 simulations were run with these parameters (Table 2).
Figure 2.
Modeling parameters and outputs.
Table 2.
Parameters of the Tunisian case study.
| Initial number of cases | R0 community | Efficacy of isolation | R0 after isolation | % of contacts tracing | |
|---|---|---|---|---|---|
| Tunisian case study | 75 cases reported to date general containment March 22, 2020 | The Rt before and after lockdown (Talmoudi et al., 2020) | 100% | 0 | Assumed: 80% |
R0, basic reproduction number.
The results are presented in terms of relative reduction rates, expressed as a percentage with the 95% confidence interval (CI). For the Tunisian case study, results were calculated for the entire population, by age group, and among those with chronic illnesses and smokers. All of the data analysis was performed using R software.
Results
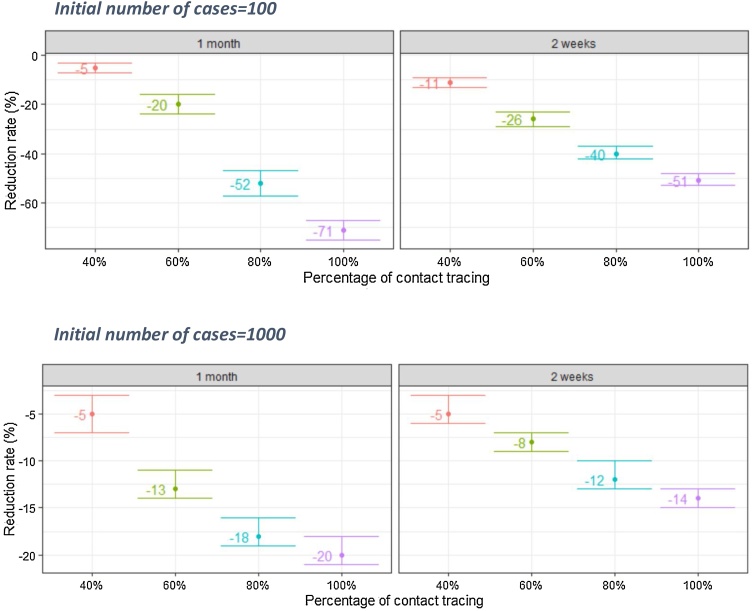
Model I: Impact of increasing the percentage of contact tracing
The results of Model I showed that at a baseline reproduction rate of 4, increasing the identification of contacts from 20% to 80% after the first 100 cases would reduce the number of infections by 40% (95% CI 37–42%) after 2 weeks and 52% (95% CI 47–57%) after 1 month. If 100% of contacts were identified, there would be a 71% (95% CI 67–75%) reduction in infections after 1 month.
However, if the intervention aimed at increasing the percentage of identified contacts was implemented only after the first 1000 reported cases, there would only be a 12% (95% CI 10–13%) reduction in infections after 2 weeks and an 18% (95% CI 16–19%) reduction after 1 month as the percentage of contact tracing increases from 20% to 80% (Figure 3).
Figure 3.
Impact of increasing the percentage of contact tracing.
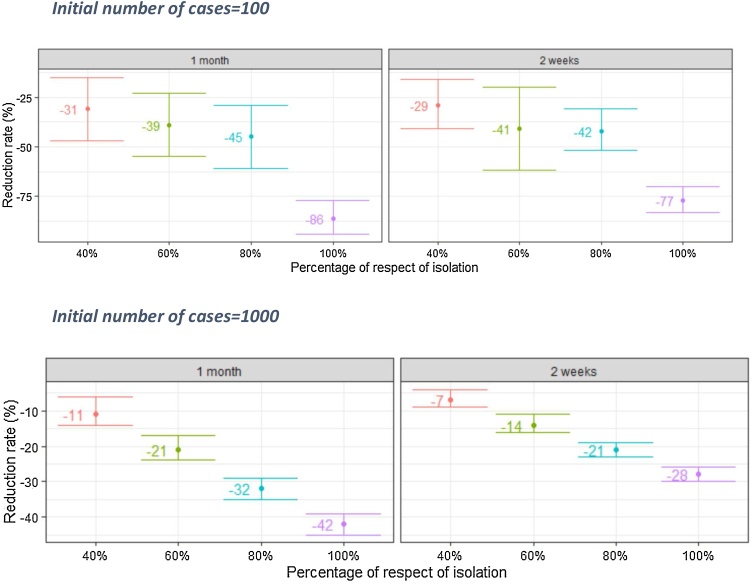
Model II: Impact of increasing the level of compliance with isolation
Compliance with isolation has an important impact in reducing infections. The results showed that at a baseline reproduction rate of 4, increasing the level of compliance to isolation from 20% to 80% from the first 100 cases would reduce the number of infected cases by 42% (95% CI 31–52%) after 2 weeks and 45% (95% CI 29–61%) after 1 month. If isolation was respected fully, there would be an 86% (95% CI 77–94%) reduction in the number of infections.
If an intervention to increase compliance with isolation was only implemented after the first 1000 infected cases, the reduction rate would be around 28% (95% CI 26–30%) after 2 weeks and 42% (95% CI 39–45%) after 1 month (Figure 4).
Figure 4.
Impact of increasing the level of compliance with isolation.
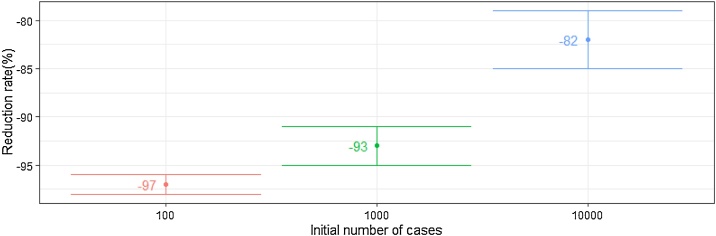
Model III: Impact of lockdown
A general lockdown has a positive impact on the reduction of virus transmission with different degrees depending on the time of implementation and the number of cases recorded at that time. A general lockdown would reduce the number of infections by 97% (95% CI 96–98%) after the first 100 cases, by 93% (95% CI 91–93%) after the first 1000 cases, and by 82% (95% CI 79–85%) after 10 000 cases.
Tunisian case
Demographics, chronic illnesses, and risk factors
Tunisia is a country in the Maghreb region of North Africa. The population was 11 551 447 inhabitants in 2018, with a quarter aged under 15 years and 8% aged 65 years and over. The median age is 32 years. Life expectancy at birth is 75.9 years. There were 68 846 registered deaths in 2018 (Institut National de la Statistique, 2018).
In terms of chronic illnesses, 28.7% (95% CI 27.6–29.8%) of the population suffers from hypertension, 15.5% (95% CI 14.6–16.3%) from diabetes, 40.9% (95% CI 39.6–42.2%) from dyslipidemia, and 2.1% (95% CI 1.8–2.5%) from chronic obstructive pulmonary disease. There is also strong comorbidity among many of these situations. The prevalence of smoking is 25.1% (95% CI 23.9–26.3%). Among people aged 65 years and over, 7.7% (95% CI 6.3–9.1%) suffer from at least one of the diseases listed above and 17.9% (95% CI 15.8–20.0%) are smokers. In addition, the elderly are particularly vulnerable to COVID-19, especially those with chronic illnesses (Saidi et al., 2019).
The COVID-19 situation in Tunisia—March to June 2020
Early after to the onset of the epidemic, the Tunisian government was committed to complying with World Health Organization (WHO) recommendations and to its own strategic response and resilience plan for epidemic diseases elaborated in 2018. The Tunisian strategy was based on the 2P2R strategy developed by the National Observatory for New and Emerging Diseases (NONED) and adapted to COVID-19. A COVID-19 Coordination National Committee was appointed and chaired by the Minister of Health. Five early measures were implemented: early case detection, tracing their contacts, treating those infected at the earliest possible stage, case isolation, and treatment. At the same time, the authorities were actively engaging the public to participate in social-distancing and other preventive measures. This committee has met regularly since late January 2020. The Tunisian Government also effectively managed the risk associated with cross-border traffic with continuous adaptation and fine-tuning of the measures designed to control inbound travelers. These have been phased in, broadly corresponding to the changing locations of virus outbreaks, with travelers arriving from at-risk countries being checked for symptoms upon arrival. In addition, strong contact tracing mechanisms were put in place through the trained regional team in the 24 governorates in February 2020. In early March 2020, the first measures were the suspension of maritime travel between Tunisia and Italy and the closure of schools. A curfew was decreed on March 17, 2020, and a general lockdown was applied on March 22, initially intended to last until April 4, but extended afterwards until May 4 (Présidence du gouvernement, 2020) (Figure 5).
Figure 5.
Impact of lockdown.
As of June 27, 2020, the date on which the borders were opened, the cumulative number of confirmed COVID-19 cases in Tunisia was 1169. Among these cases, 90 (7.7%) were still active, with 92.3% of cases having recovered. The case fatality rate was 4.2%, with 50 deaths. A total of 69 137 RT PCR tests had been conducted. The highest number of infected cases was recorded in the region of Greater Tunis and in the southern governorates of Kebelli and Medenine (Figure 6) (Observatoire national des maladies nouvelles et émergentes, 2020b).
Figure 6.
Tunisian situation in figures (June 27, 2020).
Modelling results: Impact of lockdown in Tunisia between March 22 and May 4, 2020
To understand the epidemiological results in Tunisia, the model was adapted as described earlier to take into account the demographics, chronic illnesses, and smoking behavior of the Tunisian population. In addition, the actual number of cases and Rt from Tunisia were applied.
The results of the impact modelling of the general lockdown were found to be consistent with the numbers of infections reported in the country. Indeed, Tunisia implemented its general lockdown after 75 cases had been confirmed, on March 22, 2020. In the model, the implementation of lockdown at this early stage reduced the number of infected cases by 86% (95% CI 83–89%) among the general population, 98% (95% CI 97–99%) among people aged less than 24 years, 88% (95% CI 86–90%) among people aged 65 years and more, and 92% (95% CI 90–94%) among people aged 65 years and more suffering from chronic illnesses (Table 3). These latter figures are also strongly supported by the low number of COVID-19 deaths in Tunisia.
Table 3.
Impact of the lockdown in the Tunisian population.
| Reduction rate % (95% CI) |
|||
|---|---|---|---|
| Male | Female | Both | |
| General population | 85% (95% CI 83–87%) | 87% (95% CI 83–91%) | 86% (95% CI 83–89%) |
| Age groups | |||
| 0–24 | 98% (95% CI 97–99%) | 98% (95% CI 97–99%) | 98% (95% CI 97–99%) |
| 25–34 | 97% (95% CI 96–98%) | 86% (95% CI 84–88%) | 92% (95% CI 90–94%) |
| 34–44 | 70% (95% CI 67–73%) | 80% (95% CI 79–81%) | 75% (95% CI 72–78%) |
| 45–54 | 79% (95% CI 77–81%) | 73% (95% CI 69–77%) | 76% (95% CI 72–80%) |
| 55–64 | 78% (95% CI 75–81%) | 86% (95% CI 84–88%) | 82% (95% CI 78–86%) |
| Age 65 years and older | 85% (95% CI 83–87%) | 87% (95% CI 83–91%) | 88% (95% CI 86–90%) |
| People aged 65 years and older with chronic illnesses | 91% (95% CI 89–93%) | 93% (95% CI 89–97%) | 92% (95% CI 90–94%) |
CI, confidence interval.
Discussion
The international community is facing an unprecedented global crisis with the fast spread of the COVID-19 pandemic to an ever-growing number of countries and peoples. The epidemic is all the more worrying as there is no vaccine or treatment yet. In order to inform decision-making, it is important to compare strategies to control the epidemic, reduce mortality, and limit pressure on the health system. A major challenge during outbreaks is the design of appropriate control interventions.
Mathematical models are increasingly used to guide decision-making and to evaluate interventions. The results of our mathematical modeling have been very informative. They allowed us to conclude that rigorous contact tracing, screening of suspected cases, effective early isolation, and a general lockdown have been essential in reducing the number of infections and to control the epidemic.
The results of this modelling clearly show that the earlier effective contact tracing is implemented, the higher the reduction of new infections. The impact of an increase in percentage of contacts identified from 20% to 80% was found to be around three times higher when the intervention was initiated immediately following the first 100 reported cases than with a later intervention immediately following the first 1000 reported cases. Similarly, higher compliance with isolation after the first 100 reported cases was found to be two times more efficient in terms of reducing infections than if this intervention was implemented after the first 1000 reported cases.
These results are supported by evidence from other countries. Indeed, the impact of contact tracing on COVID-19 has been proven in previous studies (Sun and Viboud, 2020, Ferretti et al., 2020). Similarly, international evidence has shown that the isolation of cases and precautionary self-isolation of contacts are key measures to bend the epidemic curve downwards (Hellewell et al., 2020b). They are key WHO recommendations, along with early diagnosis. This combination of interventions has been applied by most countries to control the COVID-19 epidemic and prevent a large fraction of possible transmission chains (Marcela et al., 2021).
Furthermore, our model showed that the lockdown in Tunisia had a critical impact on the transmission of the virus. Notably the number of infections among elderly people with chronic diseases was reduced by over 90% due to lockdown, inducing a limited number of deaths.
This is also supported by the evidence from other countries. Analysis of mortality data in the Chinese province of Hubei suggested that lockdown prevented the deaths of thousands of people (Medeiros de Figueiredo et al., 2020). Furthermore, a more stringent confinement of people in high-risk areas seems to have the potential to slow down the spread of COVID-19 (Hien Lau et al., 2020). Similarly, France has been heavily affected by the COVID-19 epidemic and went into lockdown on March 17, 2020. The lockdown resulted in a 77% (95% CI 76–78%) reduction in transmission (Salje et al., 2020).
Nonetheless, the timing of interventions, including a general lockdown, is highly critical. The timing of lockdown measures may explain the differences in capacity to contain cases between different countries (Flaxman et al., 2020). For example, Italy implemented a lockdown on March 11 when it had an incidence rate of 11.71 cases per 10 000 inhabitants and a mortality rate of 0.11 deaths per 10 000 inhabitants (Sebastiani et al., 2020, Paterlini, 2020). In contrast, Tunisia implemented its general lockdown after only 75 reported cases were confirmed (0.65/100 000 habitants), on March 22, 2020.
The population’s compliance with measures imposed by the authorities is also critical in determining the impact. In the case of Tunisia, with the exception of some lapses, the population largely adhered to the measures put in place by the authorities during the first wave of the epidemic. This is supported by the Rt remaining low in almost all regions of the country and only a slight increase in the cumulative number of cases from 1025 until the lifting of the lockdown on May 4 (Talmoudi et al., 2020, Observatoire national des maladies nouvelles et émergentes, 2020c).
A strong limitation of this study is that other effects of lockdown, including the effects on the non-COVID health situation (such as mental health) and domestic violence, were not included in the model. The huge social and economic impacts of lockdown were not studied in this modelling study, but have been documented extensively elsewhere (Nicola et al., 2020). As such, the decision to impose a general lockdown needs to be considered carefully by authorities, and mitigation strategies to reduce the impact on vulnerable groups, including poor women and children, will be critical.
On May 4, 2020, Tunisia embarked on a new phase in the management of the COVID-19 pandemic: progressive and targeted lifting of the general lockdown. Borders were reopened to travelers on June 27, 2020, bringing an increase in the number of new cases. Initially new infections were mostly imported; however after July 30, 2020, local infections started exceeding imported infections, although transmission chains were still identifiable, with clusters emerging from events like weddings or in some businesses (Observatoire national des maladies nouvelles et émergentes, 2020d). Unfortunately, the situation has since deteriorated further, and with more than 30 000 new infections in the last 4 weeks (November 2020) and 227 infections per 10 0000 inhabitants in the last 2 weeks, Tunisia is currently facing an extremely challenging situation regarding COVID-19, with an imminent risk of saturating the capacity of the health system. Authorities have imposed NPIs in this second phase too; however, the strict measures were applied much later than in the first phase when considering the numbers of cases. Additionally, compliance of the population with the measures has been much lower this time around, partially due to the relatively good outcomes in Tunisia during the first phase, which has lowered people’s perception of the risk of COVID-19. As in other countries, another national lockdown is considered untenable due to the huge social and economic impacts. As such, Tunisia faces a precarious situation that will hopefully be contained through continuous strengthening of the health system response, as well as stricter measures such as localized nighttime curfews, which have now been imposed in some parts of the country (COVID-19 - Communiqué de la présidence du Gouvernement tunisien, 2021).
Despite this turnaround in the situation, the Tunisian experience with the first phase of COVID-19 can be very informative for other countries. While the Tunisian response to the first phase of COVID-19 could surely have been improved in different areas, the results of this study confirm that the interventions implemented in Tunisia, notably the general lockdown, likely played an important role in controlling the transmission of COVID-19 and avoiding saturation of the health system. Perhaps the most relevant aspect of the experience from Tunisia’s first wave is the very early application of measures. Indeed, Tunisia rapidly implemented key interventions such as the identification of suspected cases, isolation of positive cases, and contact tracing, with mandatory quarantine of close contacts, as well as a strict general lockdown to contain the first phase of the epidemic [16]. While some of these interventions, particularly early lockdown, may be difficult to replicate, their effects on controlling infections and deaths were very notable. As such, Tunisia’s experience with the first phase of the COVID-19 pandemic presents useful lessons both academically and from a policy perspective.
The reopening has led to a decline in vigilance, even a certain skepticism among Tunisians about the potential seriousness of the epidemic. Barrier measures have not been respected. It seems we are far from realizing the real level of the epidemic. However, this virus is dangerous; it causes different pathologies in the different age groups and can result in very significant consequences, even in the young populations.
Funding
There was no source of funding for this research.
Ethical approval
Anonymized data were used for the Tunisian case study. Neither ethical approval nor individual consent was applicable.
Conflict of interest
The authors declare that they have no competing interests.
Acknowledgements
We acknowledge all of the health professionals and public health decision-makers who are facing the COVID-19 pandemic.
Contributor Information
Olfa Saidi, Email: saidio@who.int.
on behalf of the NONED Working Group:
Mouna Safer, Hejer Letaief, Sonia Dhaouadi, Sondes Derouiche, Ilhem Bouaziz, Donia Gharbi, Molka Osman, Leila Bouabid, and Souha Bougatef
References
- WHO Situation report - 1 Novel Coronavirus (2019-nCoV) 21 January 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_4.
- WHO Situation report - 57 Coronavirus disease 2019 (COVID-19) 17 March 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200317-sitrep-57-covid-19.pdf?sfvrsn=a26922f2_4.
- WHO Coronavirus disease (COVID-19). Situation Report – 203. 10 August 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200810-covid-19-sitrep-203.pdf?sfvrsn=aa050308_4.
- Guidelines for non-pharmaceutical interventions to reduce the impact of COVID-19 in the EU/EEA and the UK. 24 September 2020. ECDC: Stockholm; 2020. https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-guidelines-non-pharmaceutical-interventions-september-2020.pdf.
- Calibrating long-term non-pharmaceutical interventions for COVID-19 Principles and facilitation tools. World Health Organization. 15 May 2020. https://apps.who.int/iris/bitstream/handle/10665/332099/WPR-DSE-2020-018-eng.pdf?sequence=1&isAllowed=y.
- COVID-19 strategy update World Health Organization. 14 April 2020. https://www.who.int/docs/default-source/coronaviruse/covid-strategy-update-14april2020.pdf?sfvrsn=29da3ba0_19.
- Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
- Observatoire national des maladies nouvelles et émergentes. Point de situation sur l’épidémie d’infections au Nouveau Coronavirus « COVID-19 » A la date du 17 Mars 2020, 16H30.
- COVID-19 en Tunisie point situation à la date du 27 Juin 2020.
- Hellewell Joel, et al. Lancet. 2020. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts.www.thelancet.com/lancetgh Published online February 28, 2020 https://doi.org/10.1016/S2214-109X(20)30074-30077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly C.A., Ghani A.C., Leung G.M., et al. Epidemiological determinants of spread of causal agent of severe acute respiratory syndrome in Hong Kong. Lancet. 2003;361:1761–1766. doi: 10.1016/S0140-6736(03)13410-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001316. published online Jan 29. DOI:10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu P., Zhu J., Zhang Z., Han Y., Huang L. A familial cluster of infection associated with the 2019 novel coronavirus indicating potential person-to-person transmission during the incubation period. J Infect Dis. 2020 doi: 10.1093/infdis/jiaa077. published online Feb 18. DOI:10.1093/ infdis/jiaa077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd-Smith J.O., Schreiber S.J., Kopp P.E., Getz W.M. Superspreading and the effect of individual variation on disease emergence. Nature. 2005;438:355–359. doi: 10.1038/nature04153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sebastian Funk et al. Temporal variation in transmission during the COVID-19 outbreak. https://epiforecasts.io/covid/posts/global/ (Accessed 22 May 2020).
- Talmoudi K., Safer M., Hchaichi A. et al. Estimating transmission dynamics and serial interval of the first wave of COVID-19 infections under different control measures: A statistical analysis in Tunisia from February 29 to May 5, 2020. DOI: 10.21203/rs.3.rs-31349/v1. BMC infectious diseases (29 May 2020). [DOI] [PMC free article] [PubMed]
- Institut National de la Statistique. Statistiques Tunisie: flash état civil (2018). http://www.ins.tn/sites/default/files/publication/pdf/Flash-etat%20civil-2018-v4%20%283%29.pdf.
- Saidi O., et al. Publication de l’Institut National de la Santé; Février: 2019. La santé des Tunisiens: Résultats de l’enquête “Tunisian Health Examination Survey-2016”.http://www.santetunisie.rns.tn/fr/toutes-les-actualites/912-rapport-de-l%E2%80%99enqu%C3%AAte-national-thes-2016 [Google Scholar]
- Présidence du gouvernement. Mesures officielles au 20 mars 2020. https://covid-19.tn/fr/mesures-preventives/ (Accessed 19 May 2020).
- Sun K., Viboud C. Impact of contact tracing on SARS-CoV-2 transmission. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30357-1. Published Online April 27, 2020 https://doi.org/10.1016/ S1473-3099(20)30357-1 SeeOnline/Articles https://doi.org/10.1016/ S1473-3099(20)30287-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferretti L., Wymant C., Kendall M. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science. 2020 doi: 10.1126/science.abb6936. published online March 31. DOI:10.1126/science. abb6936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellewell J., Abbott S., Gimma A., Bosse N.I., Jarvis C.I., Russell T.W., et al. Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020;8(4) doi: 10.1016/S2214-109X(20)30074-7. E488–96. doi: https://doi.org/10.1016/ S2214-109X(20)30074-30077. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salathé Marcela et al. COVID-19 epidemic in Switzerland: on the importance of testing, contact tracing and isolation. Swiss Medical Weekly https://smw.ch/article/doi/smw.2020.20225. [DOI] [PubMed]
- Medeiros de Figueiredo A, Daponte Codina A, Moreira Marculino Figueiredo DC, Saez M & Cabrera León A. Impact of lockdown on COVID-19 incidence and mortality in China: an interrupted time series study. Bull World Health Organ. E-pub: 6 April 2020. doi: 10.2471/BLT.20.256701. [DOI]
- Hien Lau B.S., et al. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med. 2020 doi: 10.1093/jtm/taaa037. Mar 17: taaa037. Published online 2020 Mar 17. doi: 10.1093/jtm/taaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- H. Salje et al. Estimating the burden of SARS-CoV-2 in France, Science 10.1126/science.abc3517. [DOI] [PMC free article] [PubMed]
- Flaxman S., Mishra S., Gandy A., et al. (Imperial College COVID-19 Response Team) Estimating the number of infections and the impact of non-pharmaceutical interventions on COVID-19 in 11 European countries. Report 13. Imperial College London, 30 2020. March Available from: http://www.imperial.ac.uk/mrc-globalinfectious-disease-analysis/covid-19/report-13-europe-npi-impact/).
- Sebastiani Giovanni, Massa Marco, Riboli Elio. Covid-19 epidemic in Italy: evolution, projections and impact of government measures. Eur J Epidemiol. 2020;35:341–345. doi: 10.1007/s10654-020-00631-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paterlini Marta. On the front lines of coronavirus: the Italian response to covid-19 Italy has rapidly become the country hit second hardest in the world by the coronavirus pandemic. BMJ. 2020;368:m1065. doi: 10.1136/bmj.m1065. (Published 16 March 2020) [DOI] [PubMed] [Google Scholar]
- Observatoire national des maladies nouvelles et émergentes. COVID-19 en Tunisie point situation à la date du 04 Mai 2020.
- Nicola Maria, et al. The socio-economic implications of the coronavirus and COVID-19 pandemic: a review. Int J Surg. 2020 doi: 10.1016/j.ijsu.2020.04.018. Apr 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Observatoire national des maladies nouvelles et émergentes. COVID-19 en Tunisie. http://www.onmne.tn/bulletin-de-veille-mensuel-covid-aout-2020. Bulletin de veille hebdomadaire. 31 Aout 2020.
- COVID-19 - Communiqué de la présidence du Gouvernement tunisien 29/10/2020 http://www.pm.gov.tn/pm/actualites/actualite.php?lang=ar&id=12764.