Graphical abstract
Keywords: COVID-19, Pandemic, Sleep habits, Sleep problems, Cross-cultural, Social jetlag
Abstract
Our study aimed to assess the change in the sleep patterns during the Coronavirus lockdown in five regions (Austria/Germany, Ukraine, Greece, Cuba and Brazil), using online surveys, translated in each language. Part of the cohort (age 25–65, well-educated) was collected directly during lockdown, to which retrospective cross-sectional data from and after lockdown (retrospective) questionnaires were added. We investigated sleep times and sleep quality changes from before to during lockdown and found that, during lockdown, participants had (i) worse perceived sleep quality if worried by COVID-19, (ii) a shift of bedtimes to later hours during workdays, and (iii) a sleep loss on free days (resulting from more overall sleep during workdays in non-system relevant jobs), leading to (iv) a marked reduction of social jetlag across all cultures.
For further analyses we directly compared system relevant and system irrelevant jobs, because it was assumed that the nature of the lockdown’s consequences is dependent upon system relevance. System relevant jobs were found to have earlier wake-up times as well as shorter total sleep times on workdays, leading to higher social jetlag for people in system relevant jobs.
Cultural differences revealed a general effect that participants from Greece and Ukraine had later bedtimes (on both work and free days) and wake-up times (on workdays) than Cuba, Brazil and Austria, irrespective of COVID-19 lockdown restrictions.
1. Introduction
In December 2019 a cluster of pneumonia cases developed in the Wuhan province of China, generated by the subsequently identified SARS-CoV2 (severe acute respiratory syndrome - coronavirus 2) [1]. The high contagiosity of the virus drove to a rapid worldwide spread of the coronavirus-disease (COVID-19), leading to the declaration of a pandemic by the World Health Organization (WHO) on 11th of March 2020 [2].
This prompted countries to impose strict social distancing measures, including the recommendation to stay at home, the ban on group meetings, and the shutdown of schools and non-essential commercial activities [3]. The effects of ‘grounding’ a nation reduced the spread of the virus [4], but also forced people to drastically change their social behaviour and everyday habits, such as fixed waking up and going to work times, having regular mealtimes, having scheduled sports and leisure activities, as well as social events. These timekeepers, which kept one’s habitual activity/rest rhythm, were suddenly disturbed due to the lockdown measures, leading to changes in one’s circadian rhythm [5]. For example, the social pressure to wake up early during workdays was partially removed during the lockdown for people who could work from home and/or on a more flexible time schedule. This was found to reduce the difference between sleep times on workdays and sleep times on free days, commonly referred as social jetlag [6]. In addition, the concern about the disease itself, the worry about personal health and about one’s family’s health, as well as the anxiety about the future of one’s workplace and financial situation had a strong impact upon the psychological state of the general population. Numerous reports show a decline in mental health, quality of life and quality of sleep in populations affected by the pandemic [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], with healthcare workers under the most pressure [17], [18].
The current study aims to investigate how sleep patterns and sleep quality changed during the lockdown, and if this varies from one country to another. First, we hypothesized that sleep quality negatively correlates to the amount of worrying about the ongoing pandemic. Furthermore, based on the study by Blume et al. [6], we hypothesized that, during lockdown, there will be a shift of sleep times to later hours during workdays and consequently an attenuation of the social jetlag, as well as lower sleep quality [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16] given the collateral damage of the lockdown measures.
Importantly, we hypothesized that participants having system relevant jobs (workers in health care and public service, as well as IT workers maintaining the IT systems in offices and institutions) may display different effects, with such jobs showing earlier wake-up times, less overall sleep and less reduction of social jetlag.
We also distributed our survey in various countries including Austria, Cuba, Germany, Greece, Ukraine and Brazil to examine whether cultural effects may alter the observed changes in sleep during the pandemic.
2. Materials and methods
2.1. Data collection
Data was collected in two phases: (i) during and (ii) after lockdown. During lockdown, a cohort was gathered through a set of two questionnaires: an entry questionnaire and a morning protocol. The entry questionnaire was a one-time survey containing questions about demographics and habitual sleep times before the COVID-19 situation, as well as about the quality of sleep, and the changes in work patterns and environment. The morning protocol was a survey that had to be completed daily, for about seven days, containing questions about the previous night’s sleep and about the amount of worry for the ongoing COVID-19 pandemic. An average of 4.94 workdays and 3.46 free days were collected from each participant.
Since the acquired cohort was too small when the lockdowns were lifted for the first time, a second roll-out of the survey followed immediately after lockdown. This was a one-time survey where we pooled the questions of the two above-mentioned questionnaires, asking about sleep habits before and sleep habits during lockdown, on workdays and on free days separately. These cross-sectional data were then added, and averages for each sleep value were computed.
Considering the novelty of the COVID-19 situation, standardized sleep questionnaires did not appear sufficient and were extended by questions concerning working from home, being worried about the epidemic, or changes in sleep behaviour during as compared to before lockdown. All questions were reviewed and approved by the Ethics Committee of the University of Salzburg.
All questionnaires were generated in LimeSurvey and had versions in 6 languages: German, English, Greek, Ukrainian, Spanish and Portuguese. The link to the questionnaires was distributed through social media platforms (e.g., Facebook, Twitter) and with the help of collaboration partners from other universities. The data from the first set of questionnaires (the cohort) was acquired for each country depending on the lockdown dates: Austria: 15.03.2020–29.05.2020, Germany: 22.03.2020–11.05.2020, Ukraine: 12.03.2020–02.06.2020, Greece: 12.03.2020–11.05.2020, and Cuba: 20.03.2020–10.07.2020. Data from Brazil were only collected in the second phase in a cross-sectional, one-time retrospective questionnaire. The start dates were set to the start of nationwide restrictions of mobility and to schools and shops closing, and the end dates correspond to the reopening of schools and shops (and mostly return of the workers to their normal offices). The cross-sectional data, collected with the single questionnaire, were acquired from 23.06.2020 until 16.09.2020 and the questions referred specifically to sleep habits “before lockdown” and “during lockdown”. For most countries (except for Cuba, where the lockdown was still in place until 30.09.2020), this data was retrospective. We are aware that the survey answers might be influenced by a recall bias [19], as we had no other objective measures of sleep in the current study, however, we tried to sample data during or as close as possible to the lockdowns. The median number of days since the end of lockdown until the participants answered the survey was 27.6 days, calculated over all participants, with those participants who answered during lockdown having 0 days recall bias. Out of 370 participants, 162 answered during lockdown and 208 answered after the lockdown.
Since this was an ad hoc study, triggered by the COVID-19 pandemic and the sudden social distancing restrictions, the choice of these five countries was also motivated by pre-existing collaborations that would speed up data collection in this novel situation.
2.2. Participants
Inclusion criteria for the participants were: age 25–65 and living in one of the countries mentioned above. In total, 381 participants fulfilled these criteria. After a preliminary analysis, we found that 11 participants working in the food industry had a very different pattern of sleep/wake hours compared to the other job categories. As the group was too small to be considered separately, we had to exclude them, which left us with 370 participants, from which 71 were living in Austria and Germany, 62 in Greece, 78 in Ukraine, 95 in Cuba and 64 in Brazil. Out of the 370 participants, 12.7% (47) were from the cohort data and the rest of 87.3% (323) were from the cross-sectional, retrospective data. For analysis of each sleep variable, we excluded outliers (3 standard deviations from the group mean) and missing values. The (post-hoc) calculated power of our statistical analyses (including 2-ways mixed ANCOVA with 2- and, respectively, 5-group factors) was above 0.95 for medium size effects, p < .05.
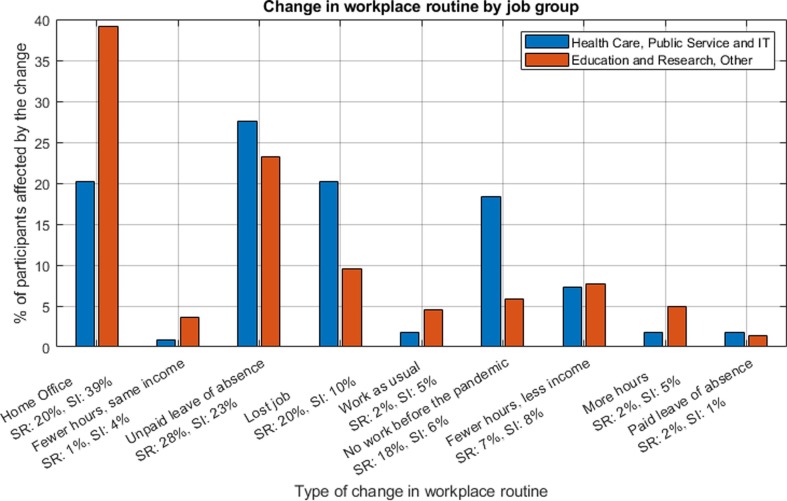
We defined system relevant jobs as activity in areas that could not be shut down but and rather expected increases in the amount of work during lockdown. Because of the expected strain on the healthcare system, health care professionals were included. In addition, we included public service employees such as postal office workers, bus drivers, or workers in administration, as well as people working in IT, because of the increased workload for those managing the IT systems for institutions and companies that moved their activity online. In total, 108 participants had system relevant jobs (health care, public service, IT) and 262 system irrelevant jobs (any other job, retired or unemployed, domestic occupation or no answer). People in system-relevant jobs were less susceptible to be sent on home office, or to work fewer hours under the same income, but were more likely to lose their job or to take unpaid leave of absence (Fig. 1 - How the COVID-19 lockdown affected job routines for participants in different job groups).
Fig. 1.
How the COVID-19 lockdown affected job routines for participants in different job groups. Note that system relevant (SR) jobs are less likely to do home office or to work fewer hours with a constant income, but are more likely to take unpaid leave of absence, or to lose their job. (SR = System Relevant jobs, N = 109, SI = System Irrelevant jobs, N = 220; participants who reported to have no job or who did not provide an answer about their job were excluded here for better illustration, N = 59).
This suggests that the classification in system relevant and irrelevant by the job category (public service, health care) is still imperfect, as, for example, a dermatologist or a dentist, though they are health care workers, might see much fewer elective patients during lockdown than before.
The mean age of our sample was 39.2 years (SD = 11.2). See Table 1 for an overview of sociodemographic data.
Table 1.
Overview of sociodemographic data.
| Total |
Austria |
Ukraine |
Greece |
Cuba |
Brazil |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | ||
| Total | 370 | 100 | 71 | 19 | 78 | 21 | 62 | 17 | 95 | 26 | 64 | 17 | |
| Age | 25–35 | 167 | 45 | 35 | 9 | 47 | 13 | 23 | 6 | 31 | 8 | 31 | 8 |
| 35–45 | 92 | 25 | 23 | 6 | 16 | 4 | 12 | 3 | 21 | 6 | 20 | 5 | |
| 45–55 | 73 | 20 | 8 | 2 | 10 | 3 | 22 | 6 | 23 | 6 | 10 | 3 | |
| 55–65 | 38 | 10 | 5 | 1 | 5 | 1 | 5 | 5 | 20 | 5 | 3 | 1 | |
| Education | Secondary or less | 7 | 2 | 2 | 3 | 3 | 4 | 2 | 3 | 0 | 0 | 0 | 0 |
| Higher education | 132 | 36 | 16 | 22 | 14 | 18 | 27 | 44 | 49 | 52 | 26 | 41 | |
| University degree | 231 | 62 | 53 | 75 | 61 | 78 | 33 | 53 | 46 | 48 | 38 | 59 | |
| Job | System- Relevant | 108 | 30 | 25 | 6 | 9 | 2 | 22 | 5 | 37 | 10 | 15 | 13 |
| System-Irrelevant | 262 | 70 | 46 | 12 | 69 | 18 | 40 | 10 | 58 | 15 | 49 | 4 | |
2.3. Measurement
For each participant, the data was collected separately for workdays and free days. Sleep values collected included bedtime, wake-up-time and subjective total-sleep-time. From this data we derived time-in-bed and social jetlag, with time-in-bed, a more objective measure of sleep duration (and validation of the subjective total-sleep-time), calculated as the simple difference between wake-up-time and bedtime (e.g. 07:15(02Apr) to 23:45(01Apr) = 07:30). Social jetlag was computed as mid-sleep point(free days) – mid-sleep point(workdays). The mid-sleep point was thereby calculated as bedtime + (wake-up-time – bedtime)/2 (e.g. 23:45(01Apr) + (07:15(02Apr) – 23:45(01Apr))/2 = 23:45(01Apr) + 07:30/2 = 23:45(01Apr) + 03:45 = 03:30(02Apr)).
2.4. Data processing
Data analysis was performed in Matlab version 2019b [20]. Averages for each sleep value described above were computed for each country and for each job. The total number of participants was too low to be able to divide them further by job within each country, so in this pilot study we only ran statistical analyses on job groups and on countries separately.
2.5. Statistical analysis
Statistical analysis was performed in R, version 3.6 [21]. Due to a significant country effect on age (F(4, 365) = 5.88, p < .001, η2 = 0.06), as well as job effect on age (F(1, 368) = 14.52, p < .001, η2 = 0.04), main effects and interactions were analysed while controlling for age. Thus, a two way mixed ANCOVA with within-subjects factor “COVID-19” (before vs. after), between-subjects factor “country” (Greece vs. Ukraine vs. Cuba vs. Austria vs. Brazil) and “age” as a covariate was performed to examine country and COVID-19 lockdown effects separately for free and workdays, while controlling for age. Similarly, a two way mixed ANCOVA with within-subjects factor “COVID-19” (before vs. during), between-subjects factor “job” (system relevant vs. system irrelevant), and “age” as covariate, was performed in order to explore job × COVID-19 effects, separately for free and workdays. Post-hoc analysis of significant main effects was performed using Bonferroni-corrected pairwise marginal mean comparisons, using the “rstatix” package [22]; more specifically we performed the Bonferroni correction for multiple testing with 5 countries, on work days as well as on free days, reporting only the effects that reached a significance threshold of p < .005. Similar analysis was used on social jetlag scores. The “age × COVID-19” interaction on social jetlag scores was explored by statistically comparing Fisher-transformed correlation coefficients using a paired t-test. The effects of COVID-19-related worry on sleep quality was examined using both a chi-square and Spearman's correlation. Note that for the chi-square analysis the “I don't worry at all” and “I barely worry” responses were merged to achieve a comparable number of observations.
3. Results
3.1. Effects of COVID-19 pandemic on sleep time variables
3.1.1. Total sleep time
Analysis of total sleep time on free days revealed a significant COVID-19 effect (F(1, 317) = 5.155, p = .024, η2 = 0.016), suggesting that participants slept more before (mean (M) = 08:23, SD = 01:07) than during COVID-19 lockdown on free days (M = 08:13, SD = 01:13) as they seemed to make up for their sleep already during workdays (cf. Table 2 ; Mbefore = 07:19, SD = 01:07; Mduring = 07:30, SD = 01:11). The latter effect however, was only significant for system-irrelevant jobs (F(1, 221) = 11.301, p < .001), but not for system-relevant subjects (F(1, 95) = 0.00, p = .984). There was no main effect of gender on total sleep time. Likewise, the GENDER × COVID-19 interaction (F(1, 316) = 0.738, p = 0.391) was not significant, showing that the lockdown did not differently affect total sleep time between sexes.
Table 2.
Sleep values before and during lockdown, on workdays (A) and on free days (B).
| Total Sleep |
Time in Bed |
Going to Bed |
Wake Up |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| |||||||||
| Country | |||||||||
| Austria * | Before | 07:03 | 00:59 | 07:32 | 01:08 | 23:02 | 00:55 | 06:30 | 00:55 |
| During | 07:05 | 01:04 | 07:40 | 01:08 | 23:29 | 00:52 | 07:04 | 01:09 | |
| Greece | Before | 07:01 | 01:07 | 07:06 | 01:01 | 24:01 | 01:03 | 07:01 | 01:12 |
| During | 07:20 | 01:08 | 07:25 | 01:11 | 24:32 | 01:28 | 07:53 | 01:41 | |
| Ukraine | Before | 07:33 | 01:08 | 07:50 | 00:58 | 23:35 | 01:10 | 07:23 | 01:20 |
| During | 07:52 | 01:15 | 08:06 | 01:17 | 23:51 | 01:29 | 07:54 | 01:33 | |
| Cuba | Before | 07:33 | 01:03 | 07:36 | 00:56 | 22:56 | 00:50 | 06:30 | 00:48 |
| During | 07:34 | 01:04 | 07:43 | 01:02 | 23:15 | 00:59 | 06:54 | 01:04 | |
| Brazil | Before | 07:08 | 01:09 | 07:21 | 00:57 | 23:17 | 01:12 | 06:35 | 01:10 |
| During | 07:21 | 01:18 | 07:33 | 01:17 | 23:43 | 01:41 | 07:15 | 01:45 | |
| Job | |||||||||
| System Relevant | Before | 07:09 | 01:02 | 07:16 | 00:58 | 23:09 | 00:56 | 06:27 | 00:52 |
| During | 07:10 | 01:07 | 07:20 | 01:05 | 23:32 | 01:10 | 06:53 | 01:18 | |
| System Irrelevant | Before | 07:23 | 01:08 | 07:36 | 01:01 | 23:26 | 01:09 | 06:57 | 01:13 |
| During | 07:38 | 01:11 | 07:52 | 01:13 | 23:49 | 01:28 | 07:36 | 01:32 | |
| Total Sleep |
Time in Bed |
Going to Bed |
Wake Up |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| |||||||||
| Country | |||||||||
| Austria * |
Before | 08:21 | 00:55 | 08:41 | 00:57 | 23:55 | 01:11 | 08:31 | 01:17 |
| During | 07:58 | 01:02 | 08:29 | 01:01 | 24:00 | 01:08 | 08:19 | 01:18 | |
| Greece | Before | 08:07 | 01:02 | 08:07 | 00:58 | 24:59 | 01:16 | 09:04 | 01:38 |
| During | 07:59 | 01:18 | 08:01 | 01:15 | 25:12 | 01:29 | 09:12 | 01:42 | |
| Ukraine | Before | 08:27 | 01:18 | 08:38 | 01:05 | 24:03 | 01:08 | 08:42 | 01:34 |
| During | 08:20 | 01:20 | 08:30 | 01:12 | 24:15 | 01:25 | 08:46 | 01:42 | |
| Cuba | Before | 08:38 | 01:00 | 08:41 | 00:59 | 23:58 | 01:14 | 08:37 | 01:08 |
| During | 08:29 | 01:02 | 08:34 | 01:01 | 24:03 | 01:05 | 08:32 | 01:09 | |
| Brazil | Before | 08:15 | 01:12 | 08:28 | 00:55 | 24:02 | 01:17 | 08:22 | 01:26 |
| During | 08:04 | 01:21 | 08:14 | 01:19 | 24:22 | 00:15 | 08:31 | 01:55 | |
| Job | |||||||||
| System Relevant | Before | 08:27 | 00:58 | 08:28 | 01:03 | 23:59 | 01:10 | 08:30 | 01:09 |
| During | 08:10 | 01:09 | 08:20 | 01:07 | 24:16 | 01:22 | 08:34 | 01:25 | |
| System Irrelevant | Before | 08:22 | 01:10 | 08:33 | 00:59 | 24:15 | 01:19 | 08:43 | 01:47 |
| During | 08:15 | 01:15 | 08:24 | 01:12 | 24:23 | 01:30 | 08:43 | 01:51 | |
All values are in HH:MM format and represent the average from all participants in that group (job or country). *Includes values from Austria (55 participants) and Germany (16 participants).
In addition, there was a general and significant country effect on both free (F(4, 314) = 3.72, p = .006, η2 < 0.045) and workdays (F(4, 314) = 5.01, p < .001, η2 < 0.06). On free days, Cuba (M = 08:33, SD = 01:01) slept significantly more than Greece (M = 08:03, SD = 01:10; p < 0.0001), Austria (M = 08:09, SD = 00:59; p = 0.0008, and Brazil (M = 08:09, SD = 01:16; p = 0.0002). On workdays, Cuba (M = 07:34, SD = 01:03) and Ukraine (M = 07:43, SD = 01:12) slept significantly more than Greece (M = 07:11, SD = 01:08; p = 0.0027 for Cuba vs. Greece and p = 0.0008 for Ukraine vs. Greece), Austria (M = 07:04, SD = 01:01; p = 0.0002 and p < 0.0001, respectively), and Brazil (M = 07:14, SD = 01:14, p = .0042 and 0.001, respectively).
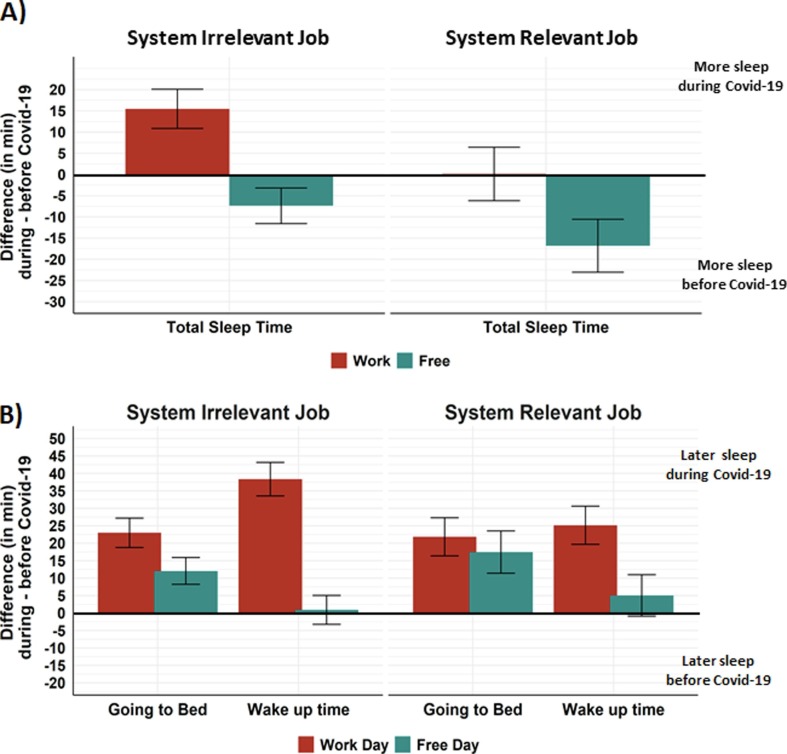
In addition, there was a significant effect of job on workdays (F(1, 317) = 6.74, p = .01, η2 = 0.021) revealing that participants with system relevant jobs slept significantly less (M = 07:09, SD = 01:04) than participants with system irrelevant jobs (M = 07:31, SD = 01:10). This was not the case on free days (F(1, 317) = 0.269, p = .604, η2 < 0.01; cf. Fig. 2 A).
Fig. 2.
(A) Differences in total-sleep-times during minus before COVID-19 lockdown, for system relevant and system irrelevant jobs. On workdays (red) participants with system irrelevant jobs sleep more during lockdown than before, but participants with system relevant jobs do not. On free days (green), all participants sleep less during the lockdown than before. (B) Differences in bedtimes and wake up times during minus before COVID-19 lockdown, for system relevant and system irrelevant jobs. On workdays (red), both job groups go to bed and wake up later during lockdown than before. On free days (green), participants from both job groups go to bed a little later during than before the lockdown, but wake up at almost the same time as before the lockdown. Negative values describe a loss of sleep during lockdown; positive values describe a gain in sleep during lockdown.
3.1.2. Time-in-bed
Time-in-bed data confirm the total sleep time results. We found a marginally significant effect of COVID-19 lockdown for free days (F(1, 312) = 3.382; p = .067; η2 = 0.011; Mbefore = 08:32, SD = 01:00; Mduring = 08:23, SD = 01:10), but not for workdays (F(1, 312) = 0.399; p = .528; η2 = 0.001), similar to the results reported above.
In addition, there was a significant job effect on workdays (F(1, 312) = 10.508; p = .001; η2 = 0.033), suggesting that participants with system relevant jobs spent less time in bed (M = 07:18, SD = 01:01) than participants with system irrelevant jobs (M = 07:44, SD = 01:08). This was not the case on free days (F(1, 312) = 0.004, p = .952, η2 < 0.01), further confirming the results for total-sleep-time, reported above.
3.1.3. Bedtimes
Analysis of bedtimes revealed a significant COVID-19 effect on workdays (F(1, 318 = 17.019, p < .001, η2 = 0.051), with earlier bedtimes before COVID-19 lockdown (M = 23:21, SD = 01:06) than during lockdown (M = 23:44, SD = 01:23), but this was not the case for free days (F(1,318) = 2.081, p = .15, η2 = 0.007).
Furthermore, there was a significant country effect for both work (F(4, 315) = 11.25, p < .001, η2 = 0.125) and free days (F(4,315) = 10.10, p < .001, η2 = 0.114). On free days Greece had later bedtimes (M = 01:06, SD = 01:17) than every other country: Brazil (M = 00:12, SD = 01:37, p = 0.0001), Cuba (M = 00:01, SD = 01:10, p < 0.0001), Austria (M = 23:58, SD = 01:09, p < 0.0001), Ukraine (M = 00:09, SD = 01:17, p < 0.0001). On workdays, Ukraine (M = 23:43, SD = 01:20) had significantly later bedtimes than Cuba (M = 23:06, SD = 00:55, p = 0.0008), while Greece had later bedtimes (M = 00:17, SD = 01:17) than every other country: Brazil (M = 23:00, SD = 01:28, p = 0.0007), Cuba (p < 0.001), Austria (M = 23:16, SD = 00:55, p < 0.0001), and Ukraine (p < 0.0001). The effect of job as well as the job × COVID-19 interactions did not reach statistical significance.
3.1.4. Wake-up-time
Analysis of the wake-up-times on workdays revealed a significant COVID-19 effect (F(1, 312) = 26.75, p < .001, η2 = 0.079) with later wake-up-times during COVID-19 lockdown (M = 07:23, SD = 01:30) as compared to before lockdown (M = 06:48, SD = 1:09). But this was not the case for free days (F(4, 312) = 2.284, p = .132, η2 = 0.004).
In addition, there was a country effect for both free (F(4, 312) = 4.723, p = .001, η2 = 0.057) and workdays (F(4,312) = 7.902, p < .001, η2 = 0.092). On free days, Greece (M = 09:08, SD = 01:39) had later wake-up-times than Brazil (M = 08:27, SD = 01:41, p < 0.0001), Austria (M = 08:25, SD = 01:41, p < 0.0001) and Ukraine (M = 08:44, SD = 01:38, p = 0.0001), while Cuba (M = 0:35, SD = 01:09) had significantly later bedtimes compared to Austria (p = 0.004). On workdays, Greece (M = 07:27, SD = 01:31) and Ukraine (M = 07:39, SD = 01:28) had later wake-up-times than Cuba (M = 06:42, SD = 00:58, p < 0.0001 for Cuba vs. both Greece and Ukraine), Austria (M = 06:47, SD = 01:04, p < 0.0001 for Austria vs. both Greece and Ukraine), and Brazil (M = 06:55, SD = 01:31, p = 0.0001 and < 0.0001, respectively). See Table 2 for more details per country.
Analysis of wake-up-times showed also a significant difference between system relevant and system irrelevant jobs on workdays (F(1, 315) = 27.32, p < .001, η2 = 0.037), with participants in system relevant jobs waking up earlier (M = 06:40, SD = 01:08) as compared to participants in system irrelevant jobs (M = 07:17, SD = 01:25). However, this was not the case for free days (F(1,315) = 0.007, p = .933, η2 < 0.001; cf. Fig. 2B).
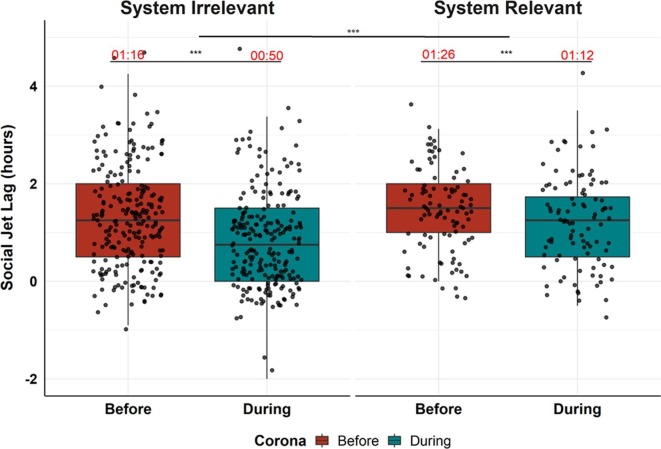
3.2. Effects of COVID-19 pandemic on social jetlag
Analysis of social jetlag revealed a robust COVID-19 effect (F(1, 325) = 22.24, p = <0.001, η2 = 0.064) with higher social jetlag scores before COVID-19 lockdown (M = 01:20, SD = 00:59) than during lockdown (M = 00:57, SD = 00:56). In addition, there was a significant job effect (F(1, 325) = 10.294, p < .001, η2 = 0.031) with participants in system relevant jobs showing higher social jetlag scores (M = 01:20, SD = 00:52) compared to participants in system irrelevant jobs (M = 01:04, SD = 01:01; cf. Fig. 3 ). There was a main effect of gender on social jetlag (F(1, 320) = 4.880, p = 0.028), with females (M = 01:03, SD = 00:52) having less social jetlag than males (M = 01:15, SD = 01:01), irrespective of the lockdown. However, the interaction GENDER × COVID-19 was not significant (F(1, 320) = 0.041, p = 0.84), showing that both sexes were equally affected by the pandemic with respect to social jetlag.
Fig. 3.
Social jetlag in hours (difference of sleep midpoint of workdays minus sleep midpoint of free days) for system relevant (n = 108) and system irrelevant (n = 262) jobs before and during COVID-19. Note that during COVID-19 there is reduced social jetlag for both groups. Participants with system relevant jobs reported higher social jetlag than participants with system irrelevant jobs, independent of the COVID-19 situation. (*p < .05, **p < .001).
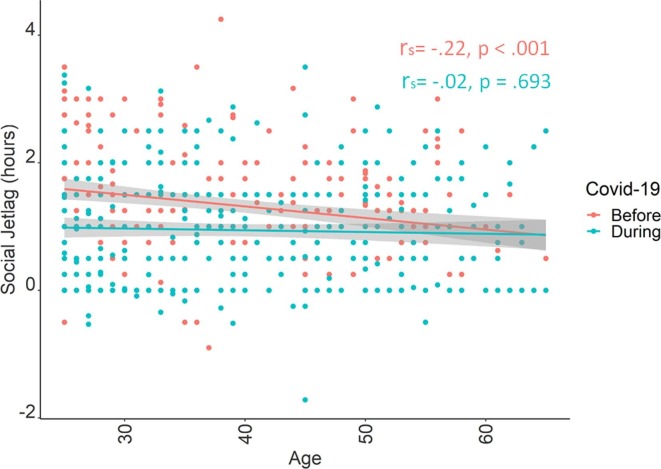
In addition, there was a significant age × COVID-19 interaction (F(1,325) = 9.46, p = .002, η2 = 0.028) indicating less social jetlag with increasing age (rS = −0.21, p < .001), but no such relation during COVID-19 lockdown (rS = -0.01, p = .72) (cf. Fig. 4 ).
Fig. 4.
Correlation between age and social jetlag before (red) and during (blue) COVID-19 lockdown. Note that the negative relationship between age and social jetlag before lockdown (red) disappears during (blue) COVID-19 lockdown.
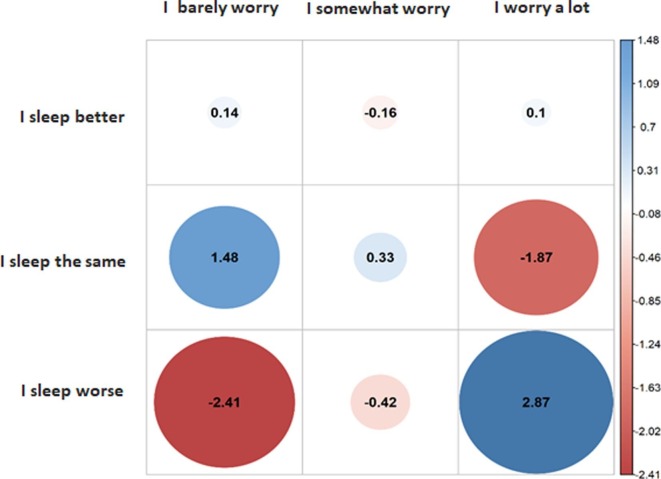
3.3. Effects of worrying about the COVID-19 pandemic on subjective sleep quality
The majority of the participants (53%, N = 174) reported that they were somewhat worried, while 22% (N = 71) barely worried and 25% (N = 81) worried a lot. Sleep quality did not change during lockdown for most 65% of the participants (N = 207), while 26% (N = 84) reported a deterioration and only 12% (N = 35) an improvement. Analysis of the relationship between sleep quality and worry about COVID-19 pandemic revealed a significant association (χ2(4) = 20, p < .001), indicating that participants who do not (or barely) worry are less likely to sleep worse, whereas participants who worry a lot about the pandemic are overrepresented in the group, indicating that they are much more likely to sleep worse during lockdown (cf. Fig. 5 ). Follow-up correlational analysis between sleep quality change and worry about COVID-19 showed that sleep quality change and worry about COVID-19 were negatively correlated (rS = -0.19, p < .001). This negative correlation indicates that sleep quality worsens as worry about COVID-19 increases.
Fig. 5.
Effects of worry about the COVID-19 pandemic on subjective sleep quality visualised as χ2 residuals. Note that people who do not (or barely) worry are less likely (than expected) to sleep worse (in red), whereas the participants who worry a lot about the pandemic are more likely to sleep worse (in blue).
4. Discussion
4.1. COVID-19 lockdown effects
Results reveal that the lockdown had strong effects on all of the measured sleep variables.
On workdays, participants started to go to bed and wake up later during lockdown than before (by an average of 23 min and, respectively, 35 min), meaning that participants on average gained 12 min of sleep every day over the work days. This effect was driven by people in system irrelevant jobs, with those in system relevant jobs not sleeping longer on workdays during lockdown. On free days, participants went to bed and woke up at similar times to those before COVID-19, and even slept 10 min less than before lockdown, likely due to the prolonged sleeping times during the work week. Interestingly this increase of sleep on work days and reduction of sleep on free days during lockdown has also just recently been reported by Korman and colleagues [23] for a big sample and across age groups. An earlier report by Wright et al. [24] on university students, however, shows an increase in sleep timing during both weekdays and weekends during lockdown. However, the age range and employment status (in our case 25–65 years across various jobs) are very different in that study compared to our sample. Another study [25] on an Italian sample report an increase in sleep duration, with more participants now sleeping over 7 h a night during lockdown.
The shift of sleep to later wake-up-times on workdays confirms our hypothesis and is reflected in the reduction of the social jetlag, which reduced for all participants with an average of 23 min. Similar effects are reported by Korman and colleagues [23] and Blume et al. [6] who show a median social jetlag decrease of ~30 and 13 min, respectively, as well as by Wright et al. [24], with 18 min decrease of social jetlag in students. This suggests that without the workweek constraint, sleep during workdays shifts towards participants’ more natural rhythm, with later bedtimes and especially awakening times, thereby resembling sleep patterns during free days. The loss of sleep on free days was unexpected, but given the data, it is most likely related to the decrease of sleep debt during the workweek in lockdown. Alternatively, one could speculate that worrying about COVID-19 could have a negative impact on falling asleep and staying asleep on free days, as worry and rumination are known to increase sleep disturbances [26], [27].
4.2. Cultural effects
The cultural differences we see for total-sleep-time and time-in-bed indicate that, on workdays, participants from Cuba and Ukraine sleep more than the other countries, independently of the lockdown. The country effects for bedtimes and wake-up-times point out Greece and Ukraine as those who go to bed and wake up the latest on workdays, irrespective of the lockdown. These results confirm our hypothesis that sleeping habits differ from country to country.
Two aspects may explain these differences: sociocultural factors and the geographical location, which determines the amount of daily sunlight at time of data sampling. During spring and summer (the time when the data was collected), in Ukraine, Germany and Austria the sun rises earlier and sets later than in Greece and Cuba, while Brazil is in between [28]. This gives the former countries more hours of daylight than the latter. However, in our analyses, Ukraine and Greece had the latest bedtimes and wake-up-times from all the countries analysed, even though they got very different amounts of sunlight during the day. This leaves sociocultural factors (i.e. customs, lifestyle) as the main influence on the intercultural sleep differences. Interestingly, the results indicate that COVID-19 affected sleep in all countries in the same way with no specific cross-cultural effects. This is in agreement with a study on larger samples from Italy and Belgium [29], which reports that the COVID-19 lockdown has similar effects on sleep timing in the two countries. In that study, however, the countries differ in how each job category is affected, unemployed participants being the most affected in Italy and the least affected in Belgium, which may reflect the different welfare systems in the two countries with the Italian population suffering from higher insecurity and psychological stress associated with the pandemic. Another international study [30] comparing sleep in the same month in 2019 and 2020 in five cities around the world (Stockholm, Seoul, London, New York City and Los Angeles) also reports increases in sleep duration during the pandemic. All of their samples show an increase starting with March 2020, ranging between 12 and 24 min, but whether the cities are differently affected by COVID-19 in a statistically significant manner is not reported. However, differences in baseline sleep duration are reported to be significant before COVID-19, with Seoul having the shortest times and Stockholm the longest. Further intercultural differences in baseline sleep, but also in the way COVID-19 changed the sleep quality and duration, was reported in another international study on students [31] from seven countries (China, Ireland, Malaysia, South Korea, Taiwan, the Netherlands and the United States), in the sense that students in Asian countries reported less negative effects during the pandemic than students in Europe and in the United States.
4.3. Job effects
Participants with system relevant jobs woke up, on average, 37 min earlier and slept 22 min less on workdays than participants with system irrelevant jobs, while no differences were found on free days. This also results in a bigger social jetlag for individuals with system relevant jobs than for those with system irrelevant jobs irrespective of the lockdown.
Data show a trend that social jetlag decreased during lockdown more strongly for participants with system irrelevant jobs (on average 26 min) than for those with system relevant jobs (on average 14 min). These results support our hypothesis that participants with system relevant jobs would have earlier wake-up-times and less overall sleep, whereas participants with system irrelevant jobs managed to catch up on sleep with later wake-up-times on workdays (cf. Fig. 2B). In this respect, the current study is an important extension of existing literature [6], endorsing the theory that system relevant and system irrelevant jobs have very different situations and environmental constraints when it comes to sleeping times.
Related to that, two Chinese studies [17], [32] reported poorer sleep quality in healthcare workers, with Zheng et al. [32] showing that about one third of the healthcare workers report sleep problems. In another study on a Dutch sample, van Roeckel et al. [33] narrow down the most affected group to those healthcare workers who are in direct contact with COVID-19 patients, showing that they suffer more from sleep problems and physical (but not mental) exhaustion than their peers who don’t have direct contact with COVID-19 patients. Another report on healthcare workers from Sweden, from a sample from the International COVID-19 Sleep Study [34] revealed that, during the first wave of the COVID-19 pandemic, female healthcare workers were more at risk to suffer from excessive daytime sleepiness and low sleep satisfaction, compared to females not working in healthcare, with these differences not being observed before the pandemic. All of these studies show that health care workers, especially if in contact with COVID-19 patients, are particularly affected by the pandemic in terms of sleep and mental health. Importantly all of the above discussed studies do not include “essential” workers besides healthcare. In our study, “system relevant” includes a wider range of jobs indicating that changes in sleep timing as well as social jetlag due to the COVID-19 pandemic affect more social groups than just medical workers directly involved in managing the patients.
4.4. Age effects
We refrain from formulating hypotheses regarding the influence of age, but one age effect attracted our attention: there was a negative correlation between age and social jetlag before, but not during lockdown (cf. Fig. 4). That is, under normal social circumstances, young people have a higher social jetlag than older people, but during lockdown, this effect disappears. This suggests that the permission to work from home and the ban on social events during the COVID-19 lockdown reduced this work/free difference for young people more than it did for the older ones. As an implication of these results, young people may feel the pressure of the lockdown more strongly than older people, which might make them less inclined to comply with the distancing measures, especially since they are at a lower risk for serious complications of the disease. On the other hand, a reduction in social jetlag may indicate that younger people returned, during lockdown, to their inherent activity/rest rhythm, which may also have positive effects on their overall health during lockdown.
4.5. Subjective sleep quality
Almost two thirds of our participants reported no change in sleep quality during lockdown, which contradicts our hypothesis and is also in disagreement with observed (yet mild) overall decrease in sleep quality in the study of Blume and colleagues [6]. However, in our study, subjective sleep quality is highly correlated with the individual subjective concern regarding COVID-19, and gets worse the more concern is reported (cf. Fig. 5). The reduction in subjective sleep quality for this segment of the population has major implications, since low sleep quality is associated with higher risk for depression, suicide [25], immune system dysfunctions [35], and even a more severe course of COVID-19 infection [36], and can therefore aggravate the risk of serious long-term costs on health and well-being. Poor sleep quality and high psychological distress during the COVID-19 pandemic were also reported in a Turkish sample [37], while a study on an Indian sample [38] indicates that people with previous sleep problems are the most vulnerable to the pandemic measures. For an Italian sample, Costi et al. [39] also report a worsening of sleep quality, associated with less physical activity and a less healthy diet. Lim et al. [40] used online and in-person mindfulness training as an intervention to improve sleep quality and stress levels in a small Singapore sample. They found that either training was effective in reducing stress levels during the COVID-19 pandemic, but none of them helped for improving sleep quality during the pandemic. A French study [41] investigating the change in sleep patterns after the end of the lockdown reports an improvement in sleep quality, especially if they were less exposed to media coverage of the pandemic. This is generally in line with our finding that exclusively people worried by the pandemic show a worsening of sleep quality in our study sample. Together these studies suggest that worsening of self-reported subjective sleep quality during the COVID-19 pandemic is a widely perceived phenomenon, and more interventional studies focusing on improvement of sleep are welcome.
Altogether, the results indicate (i) worse perceived sleep quality in participants worrying about COVID-19, (ii) a shift of bedtimes to later hours on workdays, and (iii) a marked reduction of the social jetlag during the COVID-19 lockdown due to a normalization or harmonization of sleeping times between workdays and free days.
Although the study sample is not huge, we would like to point to the fact that we actually find very coherent effects across 5 different countries when it comes to changes due to the COVID-19 lockdown measures.
When it comes to cross-cultural sleep habits, we see that these vary substantially between culture, and we do find the expected variation [42], [43] in bedtimes and wake-up times with later times for the Greek and Ukrainian samples as compared to Austrian, Brazilian and Cuban samples. Upcoming studies such as the “International COVID-19 Sleep Study (ICOSS)”, initiated by Prof. Markku Partinen from Helsinki, will be covering 15 countries from Europe, Asia and North America, and will substantially contribute to our current knowledge on intercultural differences in sleep during COVID-19 [44]. We are looking forward to seeing how such results will extend recent findings and especially how confinement, anxiety, and other psychosocial factors associated to COVID-19 effect sleep quality and insomnia across cultures and age groups.
Ethics approval and informed consent
The study received approval from the Ethics Committee of the Paris Lodron University of Salzburg, Austria. Informed consent was obtained from each participant. The study was conducted according to the guidelines of the Declaration of Helsinki.
CRediT authorship contribution statement
Cristina Florea: Conceptualization, Software, Writing - original draft, Data curation. Pavlos Topalidis: Investigation, Software, Visualization, Writing - original draft, Formal analysis. Theresa Hauser: Conceptualization, Investigation, Methodology. Monika Angerer: Conceptualization, Writing - review & editing. Anton Kurapov: Investigation, Resources. Carlos Alberto Beltran Leon: Investigation, Resources. Daniel Soares Brandão: Investigation, Resources. Manuel Schabus: Conceptualization, Writing - review & editing, Supervision, Funding acquisition.
Acknowledgments
Acknowledgements
We would like to thank our cooperation partners in (1) Ukraine, principal investigator Anton Kurapov, Department of Experimental and Applied Psychology, Faculty of Psychology, Taras Shevchenko National University of Kiev, (2) Cuba, principal investigator Carlos Alberto Beltran Leon, Institute of Neurology and Neurosurgery, Department of Clinical Neurophysiology, Havana, (3) Greece, Anastasia Chandolia and Vasiliki Chandolia as well as in (4) Brasil, principal investigator Sidarta Ribeiro, Daniel Soares Brandão and Patrick Coquerel for their help in data collection.
We would also like to thank Marina Meier for helping us with data curation, and to Malgorzata Wislowska for supporting us with the graphical abstract.
References
- 1.Team TNCPERE. The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) — China. CCDC Weekly. 2(x) (2020). [PMC free article] [PubMed]
- 2.Organisation WH. WHO Timeline on COVID-19. https://www.who.int/news-room/detail/27-04-2020-who-timeline---COVID-19. Published 2020. Accessed 21.07.2020.
- 3.Lau H., Khosrawipour V., Kocbach P., et al. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med. 2020;27(3) doi: 10.1093/jtm/taaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flaxman S., Mishra S., Gandy A., et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- 5.Morin C.M., Carrier J., Bastien C., Godbout R., Canadian S., Circadian N. Sleep and circadian rhythm in response to the COVID-19 pandemic. Can. J. Public Health. 2020;111(5):654–657. doi: 10.17269/s41997-020-00382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blume C., Schmidt M.H., Cajochen C. Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms. Curr. Biol. 2020;30(14):R795–R797. doi: 10.1016/j.cub.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.F. Beck, D. Léger, L. Fressard, P. Peretti-Watel, P. Verger, G. Coconel, Covid-19 health crisis and lockdown associated with high level of sleep complaints and hypnotic uptake at the population level. J. Sleep Res. (2020) e13119-e13119. [DOI] [PMC free article] [PubMed]
- 8.Broche-Pérez Y., Fernández-Fleites Z., Jiménez-Puig E., Fernández-Castillo E., Rodríguez-Martin B.C. Gender and fear of COVID-19 in a cuban population sample. Int. J. Ment. Health Addict. 2020:1–9. doi: 10.1007/s11469-020-00343-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.N. Cellini, N. Canale, G. Mioni, S. Costa, Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. (2020) e13074–e13074. [DOI] [PMC free article] [PubMed]
- 10.Gualano M.R., Lo Moro G., Voglino G., Bert F., Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int. J. Environ. Res. Public Health. 2020;17(13):4779. doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.C.K. Kaparounaki, M.E. Patsali, D.-P.V. Mousa, E.V.K. Papadopoulou, K.K.K. Papadopoulou, K.N. Fountoulakis, University students' mental health amidst the COVID-19 quarantine in Greece, Psychiatry Res. 290 (2020) 113111-113111. [DOI] [PMC free article] [PubMed]
- 12.C.K. Kokou-Kpolou, O. Megalakaki, D. Laimou, M. Kousouri, Insomnia during COVID-19 pandemic and lockdown: Prevalence, severity, and associated risk factors in French population, Psychiatry Res. 290 (2020) 113128-113128. [DOI] [PMC free article] [PubMed]
- 13.Leone M.J., Sigman M., Golombek D.A. Effects of lockdown on human sleep and chronotype during the COVID-19 pandemic. Curr. Biol. 2020;30(16):R930–R931. doi: 10.1016/j.cub.2020.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Llibre-Guerra J.J., Jiménez-Velázquez I.Z., Llibre-Rodriguez J.J., Acosta D. The impact of COVID-19 on mental health in the Hispanic Caribbean region. Int Psychogeriatr. 2020;1–4 doi: 10.1017/S1041610220000848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marelli S., Castelnuovo A., Somma A., et al. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J Neurol. 2020;1–8 doi: 10.1007/s00415-020-10056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.P. Voitsidis, I. Gliatas, V. Bairachtari, et al., Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 289 (2020) 113076-113076. [DOI] [PMC free article] [PubMed]
- 17.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiao H., Zhang Y., Kong D., Li S., Yang N. The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26 doi: 10.12659/MSM.923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gao C., Scullin M.K. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med. 2020;73:1–10. doi: 10.1016/j.sleep.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MATLAB. 9.7.0.1190202 (R2019b). Natick, Massachusetts: The MathWorks Inc., 2019.
- 21.K. Noguchi, Y.R. Gel, E. Brunner, F. Konietschke, nparLD: An R Software Package for the Nonparametric Analysis of Longitudinal Data in Factorial Experiments, 50(12) (2012) 23.
- 22.rstatix: Pipe-Friendly Framework for Basic Statistical Tests. R package version 0.6.0 [computer program]. 2020-06-18.
- 23.Korman M., Tkachev V., Reis C., et al. COVID-19-mandated social restrictions unveil the impact of social time pressure on sleep and body clock. Sci. Rep. 2020;10(1):22225. doi: 10.1038/s41598-020-79299-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wright K.P., Linton S.K., Withrow D., et al. Sleep in university students prior to and during COVID-19 Stay-at-Home orders. Curr. Biol. 2020;30(14):R797–R798. doi: 10.1016/j.cub.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Di Renzo L., Gualtieri P., Pivari F., et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J. Transl. Med. 2020;18(1):229. doi: 10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McGowan S.K., Behar E., Luhmann M. Examining the relationship between worry and sleep: a daily process approach. Behav. Ther. 2016;47(4):460–473. doi: 10.1016/j.beth.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 27.Palagini L., Mauri M., Banfi T., et al. Daytime rumination as a feature of Insomnia Disorder: sleep related cognition is not merely a problem of the night. Arch. Ital. Biol. 2015;153(2–3):239–247. doi: 10.12871/0003982920152349. [DOI] [PubMed] [Google Scholar]
- 28.Thorsen S. Time and Date AS 1995-2020. https://www.timeanddate.com/. Accessed 21.09.2020, 2020.
- 29.Cellini N., Conte F., De Rosa O., et al. Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors. Sleep Med. 2020;77:112–119. doi: 10.1016/j.sleep.2020.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Robbins R., Affouf M., Weaver M.D., et al. Smartphone application-estimated sleep duration before and during COVID-19 in five major metropolitan areas on three different continents. J. Med. Internet Res. 2021 doi: 10.2196/20546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Du C., Zan M.C.H., Cho M.J., et al. Health behaviors of higher education students from 7 countries: poorer sleep quality during the COVID-19 pandemic predicts higher dietary risk. Clocks Sleep. 2021;3(1):12–30. doi: 10.3390/clockssleep3010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Y. Zheng, L. Wang, L. Feng, L. Ye, A. Zhang, R. Fan, Sleep quality and mental health of medical workers during the coronavirus disease 2019 pandemic. Sleep Biol. Rhythms (2021) 1-8. [DOI] [PMC free article] [PubMed]
- 33.van Roekel H., van der Fels I.M.J., Bakker A.B., Tummers L.G. Healthcare workers who work with COVID-19 patients are more physically exhausted and have more sleep problems. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.625626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Benedict C., Partinen M., Bjorvatn B., Cedernaes J. Sleep in female healthcare workers during COVID-19: a cross-sectional survey study in sweden during the flattening of the first wave of the pandemic. Ann. Am. Thorac. Soc. 2021 doi: 10.1513/AnnalsATS.202101-019RL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Besedovsky L., Lange T., Haack M. The sleep-immune crosstalk in health and disease. Physiol. Rev. 2019;99(3):1325–1380. doi: 10.1152/physrev.00010.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rowlands A.V., Kloecker D.E., Chudasama Y., et al. Association of timing and balance of physical activity and rest/sleep with risk of COVID-19: A UK biobank study. Mayo Clin. Proc. 2021;96(1):156–164. doi: 10.1016/j.mayocp.2020.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Duran S., Geyiktepe Ö.E. Psychologic distress and sleep quality among adults in Turkey during the COVID-19 pandemic. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2021;107 doi: 10.1016/j.pnpbp.2021.110254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Radhakrishnan A., Govindaraj R., Sasidharan A., Ravindra P.N., Yadav R., Kutty B.M. People with dyssomnia showed increased vulnerability to CoVID-19 pandemic: a questionnaire-based study exploring the patterns and predictors of sleep quality using the latent class analysis technique in Indian population. Sleep Med. 2021;79:29–39. doi: 10.1016/j.sleep.2020.12.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Costi S., Paltrinieri S., Bressi B., Fugazzaro S., Giorgi Rossi P., Mazzini E. Poor sleep during the first peak of the SARS-CoV-2 pandemic: a cross-sectional study. Int. J. Environ. Res. Public Health. 2021;18(1) doi: 10.3390/ijerph18010306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lim J., Leow Z., Ong J., Pang L.S., Lim E. The effects of online group mindfulness training on stress and sleep quality during the COVID-19 pandemic in Singapore: a retrospective equivalence analysis. JMIR Ment. Health. 2021 doi: 10.2196/21757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beck F., Leger D., Cortaredona S., Verger P., Peretti-Watel P. Would we recover better sleep at the end of Covid-19? A relative improvement observed at the population level with the end of the lockdown in France. Sleep Med. 2020;78:115–119. doi: 10.1016/j.sleep.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bliwise D.L. Invited commentary: cross-cultural influences on sleep—broadening the environmental landscape. Am. J. Epidemiol. 2008;168(12):1365–1366. doi: 10.1093/aje/kwn336. [DOI] [PubMed] [Google Scholar]
- 43.Randler C., Prokop P., Sahu S., Haldar P. Cross-cultural comparison of seven morningness and sleep-wake measures from Germany, India and Slovakia. Int. J. Psychol. 2015;50(4):279–287. doi: 10.1002/ijop.12098. [DOI] [PubMed] [Google Scholar]
- 44.B.B. Markku Partinen, Brigitte Holzinger, Frances Chung, Thomas Penzel, Colin A. Espie, Charles M. Morin, ICOSS- International Covid Sleep Study. Sleep and Circadian Problems during the COVID-19 Pandemic, An International Collaborative project with harmonized datasets, J. Sleep Res. (2020), under submission. [DOI] [PubMed]