Abstract
Background
COVID-19 has quickly spread throughout the world, necessitating assessment of effective containment methods. The purpose of this study was to examine the impact of government mandated school closures, stay at home orders and mask requirements
Methods
Cumulative incidence rates were calculated at 14-day intervals until the day of the first vaccine administration in the country. Rate ratios were calculated using negative binomial regression while investigating the effects of adjusting for several sociodemographic and medical factors
Results
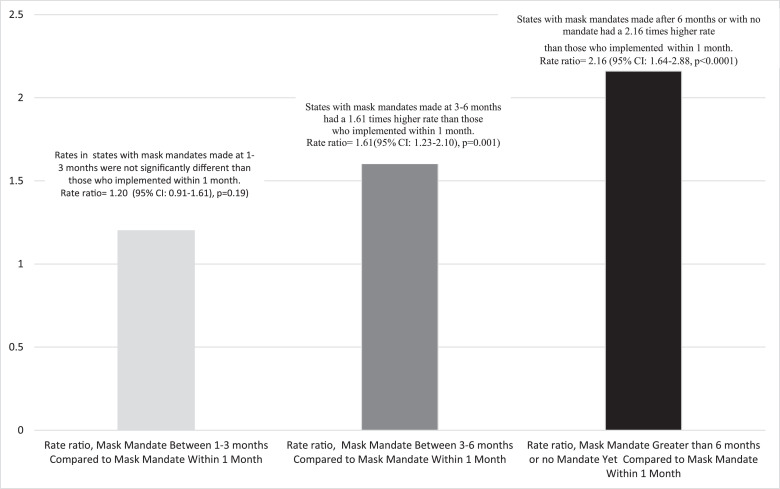
Faster implementation of mask mandates was consistently shown to be protective. States with mask mandates made at three to six months had a 1.61 times higher rate than those who implemented within one month (adjusted rate ratio = 1.61, 95% confidence interval: 1.23-2.10, P = .001). States with mask mandates made after 6 months or with no mandate had a 2.16 times higher rate than those who implemented within 1 month (adjusted rate ratio = 2.16, 95% confidence interval: 1.64-2.88, P < .0001). In contrast, both stay at home orders and school closures had no significant influence on disease trajectory.
Discussion
The benefits of mask mandates are apparent, especially when mandates were issued within a month. The impact of school closing and stay at home orders were less clear.
Conclusions
Our results suggest that of the different physical distancing measures implemented by the government, mask mandates are the most important.
Key Words: COVID-19, Physical distancing
Introduction
The 2019 novel coronavirus (COVID-19), known as the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was recently identified as the causative agent of COVID-19.1 The virus, originating from Wuhan, China, quickly spread throughout the world, leaving countries scrambling to assess the best containment methods.2 Though the virus initially presented in the United States (US) after infected individuals came into the country from international locations, the mode of transmission quickly became domestically person to person.3 Initially, some states, such as Washington, California, and New York were saw extremely high rates4. Throughout the pandemic, the states with the highest rates have changed5. While states with large cities were initially disproportionately affected, with New York City (NYC), emerging as a “hotspot,” rates are now higher in states with larger rural populations.5 , 6
As the world started to learn more about the biology of SARS-CoV-2, proposals for containment measures attempted to address the modes of transmission. Spread of SARS-CoV-2 occurs primarily through respiratory droplets.7 However, the virus can also survive on hard surfaces for hours to days.8 Because the spread of the virus is largely contingent upon proximity to one another, common containment measures included attempts to create physical distance (eg, public health measures such as restrictions on gatherings).9 As the US federal government scrambled to establish containment measures, states and local governments laid out vastly heterogeneous rules on how individuals would prevent close contact.10 , 11 In April of 2020, the Centers for Disease Control and Prevention (CDC) suggested that use of masks in public areas could be useful in addition to other physical distancing measures.12
Analyses that have been reported on existing data show that mitigation efforts may be successful. A report from the CDC examined data from the metropolitan areas of San Francisco, Seattle, New Orleans and NYC in terms of the timing of policy measures, community mobility, and incidence rates. They found that the percentage of residents leaving home declined as the number of policies issued increased, with data trends suggested that physical distancing measures may decrease incidence rates. The analysis was limited by lack of information on confounders (eg, age, gender, and race) and limited data on mobile phone coverage.13 Another study examined the impact of several physical distancing measures on the growth rate of confirmed COVID-19 cases using county level data across the US. They reported that government-imposed physical distancing measures reduced the daily growth rate by 5.4 % after 1-5 days, 6.8 % after six to ten days, 8.2% after 11-15 days, and 9.1% after 16-20 days, and suggested that failure to enact these types of restrictions would fuel exponential spread.14
Most current published studies utilize mathematical modeling to make predictions based on hypothetical situations, yielding a variety of conclusions. One study modeled the effects of physical distancing measures on the progression of the COVID-19 epidemic in Wuhan, which showed that physical distancing measures may be most successful if their relaxation is gradual rather than done as a sudden lifting of interventions. However, they noted that results varied by the duration of infectiousness and the role of school children in the epidemic.15 Another group created a model to study the impact of physical distancing and school closure on viral transmission while accounting for age differences. They reported that physical distancing in China during their outbreak was sufficient to control COVID-19, with a 40%-60% reduction in peak incidence with proactive school closures.16 A mathematical model used to investigate the value of physical distancing interventions in a mid-sized US city (modeled after Seattle) showed that interventions that start earlier in the epidemic delay the epidemic curve while interventions initiated later flatten the epidemic curve.17 A meta-analysis of 172 observational studies across 16 countries found that viral transmission was reduced with physical distancing.18
This same study found that face mask use reduced the odds of infection (adjusted odds ratio = 0•15, 95% confidence interval [CI]: 0.07-0.3).18 The benefits of using masks may work in tandem with physical distancing. It has also been estimated. the number of excess cases per 100,000 residents in states reopening indoor dining rooms without masks was ten times the number in states reopening with masks after 8 weeks (643.1 cases; 95% CI = 406.9, 879.2 and 62.9 cases; CI = 12.6, 113.1, respectively).19 Moreover, an analysis of the impact of policy measures has suggested that nationally mandating face masks for employees early in the pandemic could have reduced the weekly growth rate of cases and deaths by more than 10 percentage points in late April and could have led to as much as 19%-47% less deaths nationally by the end of May. Cases would have been larger by 6-63% without stay-at-home orders and larger by 17%-78% without business closures.20. Hypothetical mask models support these results and one such study suggested that even weak (ineffective) masks could be useful in curbing disease transmission.21 It has also been noted that widespread implementation and enforcement of sustained community mitigation measures helped with mitigation of COVID-19, noting a decline in rates once measures were implemented.22 Similarly, a study looking at daily county-level COVID-19 growth rates in 15 states and Washington, D.C., estimated that more than 200,000 COVID-19 cases could have been averted by May 22, 2020 if utilizing masks in public had been mandatory in all locations.23 While some of the data that has been published show protective outcomes from mask usage, not all studies show this and some have shown that when used improperly, the mask can actually facilitate infection.24
Much of the research that has been published has not been guided by statistics when assessing the influence of physical distancing and other infection mitigation techniques on the COVID-19 infection rates. Reports have largely been based either on charting existing data and making conclusions by visual inspection, or creating models based on simulated data. Additionally, many studies compare rates between states by looking at set dates, rather than adjusting for where a location is in their epidemic cycle. Given that the date of the first COVID-19 case in a state was widely spread around the country, comparison would be more appropriate while placing all states at the same starting point of an epidemic curve. Finally, most studies have not accounted for socio-demographic factors. While many have suggested that population density is a factor in infection rates, this only addresses how many people exist in a given square footage of land and does not account for the structure in which these individuals are spaced throughout the state. On December 11, 2020 the Food and Drug Administration (FDA) issued an Emergency Use Authorization (EUA) for the first COVID-19 vaccine and the first vaccination in the U.S. was given on December 14, 2020, marking the date at which the trajectory of disease rates will be changed by this intervention.25
The purpose of the present study was to examine the impact of school closures, stay at home orders and mask mandates on cumulative incidence rates of COVID-19 in states up until vaccination was introduced, while investigating whether controlling for a variety of socio-demographic variables would affect results. Additionally, the effects of controlling by population density as well as the percent of percent of population represented by an urban population were examined.
Methods
Data were gathered for the 50 states and the District of Columbia. Data for cumulative counts of cases were obtained from the COVID-19 Data Repository by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University.5 Data for dates of social gathering restrictions for each state were acquired from the University of Washington GitHub dataset.26 The physical distancing variables gathered were days to stay home orders, days to school closing and days to issuing a mask mandate.
All sociodemographic variables were acquired through the 2010 Census or 2018 Community Survey.27 , 28 Prevalence of several variables were evaluated for confounding, including population density, percent of population represented by an urban population and percentage in each location of people who are: Black/African American; Hispanic; age 65 and older; female; in poverty; have a college degree; own a computer; have internet access at home; use carpooling for work and use public transit for work.
Data regarding the prevalence of health conditions were obtained from the Centers for Medicare and Medicaid29 or have one of the following medical conditions: diabetes; hypertension; and ischemic heart disease.
Statistical analyses
The first day of the epidemic at any location was defined as the first day at least 50 cases were reported. The days to implementing stay at home orders and days to school closure were calculated as the dates between the date a state issued an emergency order to the date of implementation of the measure. The days to implementing a mask mandate were calculated as the days between CDC guidance on wearing masks (April 3, 2020) to the date of mandate. When no mandate had been made at the time of analysis, the date of analysis was used, as that would represent the maximum number of days that could theoretically exist to mask mandate for those states.
Days to stay home orders and days to school closing mandate were made into categorical variables using the median values as cutoff points. The number of days to stay home orders and to school closing were somewhat homogeneous between states, and thus the states were divided into two groups, rounding to the nearest two week increment. The median values for days to these government mandates were as follows: Stay at home orders had a median of 17 days and days to school closure had a median of six days. For days to stay home orders the categories created were (1) mandate issued in 14 days or less and (2) mandate issued after 14 days. For days to school closing, the categories created were (1) mandate issued in seven days or less and (2) mandate issued after seven days. Mask mandates were implemented quite a while after stay at home orders and school closures, with a wide range in days to making a mandate between the states. Several states had not made a mask mandate as of the date of this analysis. The median days to mask requirements were as follows: the 25th percentile was 28 days, the median was 91 days, and the 75th percentile was 130 days. For days to mask mandates the categories created were (1) mandate issued in one month or less, (2) mandate issued between one and three months, (3) mandate issued between three and six months, and (4) mandate issued after six months or no mandate issued yet.
Cumulative incidence rates were calculated as the total number of reported cases at a given time divided by the population size of that location, multiplied by 100,000. Cumulative incidence rates were calculated for states represented in each of the physical distancing categories. Using negative binomial regression, rate ratios, and 95% confidence intervals were calculated comparing the group that took the longest to implement measures vs those who took the shortest amount of time. Analysis of cumulative incidence was done in 14 day intervals until day 262 of the epidemic curve. This day represents the day in the epidemic cycle for which data was available for all states prior to the date of the first vaccine administration in United States (December 14, 2020).
Goodness-of-fit for including different confounders was assessed using Akaike's Information Criterion (AIC)-based selection criteria to create a final model of predictors. The Akaike Information Criterion is a measure that estimates the relative amount of information lost by a given model, rewarding models that achieve a high goodness-of-fit score and penalizing models that over-fit the data. The score allows for direct comparison of models derived from the same dataset, with a lower score indicating the superior model. Statistical analysis was conducted using SAS 9.4. Statistical significance was set at P-value < .05.
Results
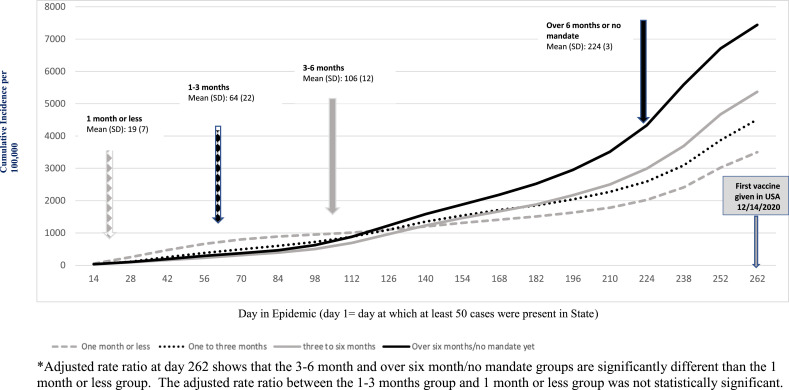
Table 1 shows the mean and standard deviation values for several variables of states in each category of mask mandate implementation. As the categories were created by days to mask implementation, the mean days to mask mandates increased with each group, with the fastest group implementing mandates at 19 days (SD 7), and subsequent groups taking 64 (SD 22), 106 (SD 12) and 224 (SD 3) days for implementation. Eight states had not yet implemented mask mandates at the time this study was concluded. The mean days to school closure were similar for the all groups (between five and seven days), except the fourth group, which took longest to implement mask measures or did not implement mask measures, where the mean was 11 days. This was similar to the pattern for stay at home orders, where three groups took a mean of 17 days. However, the fourth group, which took longest to implement mask measures or did not implement mask measures, took a mean of 26 days
Table 1.
Mask mandates and state characteristics
| U.S. Department of Health & Human Services Region and Associated States | Mean days to mask mandate from date of CDC guidance (SD)* | Mean days to schoolClosure (SD) | Mean days to stay at home orders (SD) | Mean cumulative incidence day 30, cases per 100,000 (SD) | Mean cumulative incidence day 262 cases per 100,000† (SD) | |
|---|---|---|---|---|---|---|
| Mandate in 1 month or less | Region 1: Connecticut, Maine, Vermont Region 2: New Jersey , New York Region 3: Delaware, District of Columbia, Maryland, Pennsylvania Region 5: Illinois, Michigan Region 9: Hawaii Region 10: Alaska |
197 | 74 | 1710 | 260 (201) | 3450 (1595) |
| Between 1 and 3 months | Region 1:Massachusetts, Rhode Island Region 3: Virginia Region 4: North Carolina, Mississippi Region 6: New Mexico Region 8: Colorado, Utah Region 9: California, Nevada Region 10: Oregon, Washington |
621 | 73 | 173 | 122 (100) | 4427 (1796) |
| 3- 6 months- | Region 1: New Hampshire Region 3: West Virginia Region 4: Alabama, Kentucky, South Carolina Region 5: Indiana, Minnesota, Ohio, Wisconsin Region 7: Kansas Region 6: Arkansas, Louisiana, Texas Region 8: Montana |
10612 | 53 | 179 | 94 (104) | 5290 (1507) |
| More than 6 months or no mandate yet | Region 4: Florida, Georgia, Tennessee Region 6: Oklahoma Region 7: Iowa, Missouri, Nebraska Region 8: North Dakota , South Dakota, Wyoming Region 9: Arizona Region 10: Idaho |
2243 in the 4 states that implemented |
1112 | 2615 | 103 (49) | 7362 (2498) |
CDC issued mask recommendations on April 3 2020
Day first vaccine was administered in USA, December 14, 2020. Day 262 represents the day in the epidemic cycle for which data was available for all states.
The mean cumulative incidence at day 30 showed the group fastest to implement mask mandates had the highest cumulative incidence at this time point with 260 cases per 100,000 (SD). However, by day 262, they had the lowest cumulative incidence, at 3450 cases per 100,000. The groups taking longer amounts of time for mandates had progressively higher rates, with 4427, 5290 and 7362 cases per 100,000, respectively.
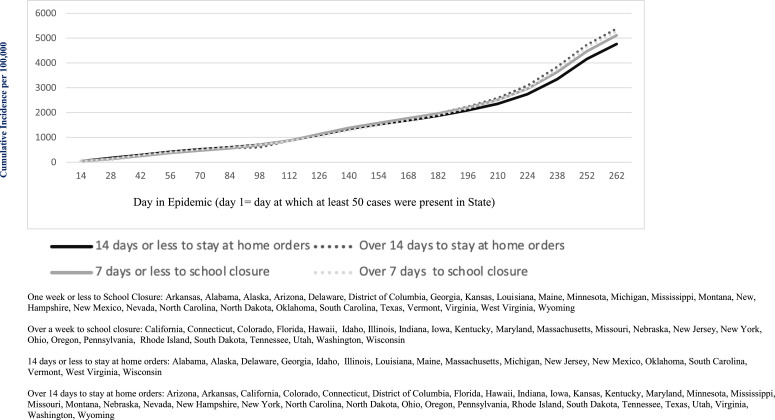
Figure 1 depicts the impact of taking longer to issue mask mandates, with those taking the longest showing the largest cumulative incidence. Figure 2 depicts graphs for school closings and stay at home orders. There was no statistically significant difference between groups for either physical distancing measure.
Fig 1.
Days to Mask Mandate and Cumulative Incidence Rates per 100,000 *Adjusted rate ratio at day 262 shows that the 3-6 month and over 6 month/no mandate groups are significantly different than the 1 month or less group. The adjusted rate ratio between the 1-3 months group and 1 month or less group was not statistically significant.
Fig 2.
Days to school closure and stay at home orders and cumulative incidence rates per 100,000 One week or less to School Closure: Arkansas, Alabama, Alaska, Arizona, Delaware, District of Columbia, Georgia, Kansas, Louisiana, Maine, Minnesota, Michigan, Mississippi, Montana, New, Hampshire, New Mexico, Nevada, North Carolina, North Dakota, Oklahoma, South Carolina, Texas, Vermont, Virginia, West Virginia, Wyoming Over a week to school closure: California, Connecticut, Colorado, Florida, Hawaii, Idaho, Illinois, Indiana, Iowa, Kentucky, Maryland, Massachusetts, Missouri, Nebraska, New Jersey, New York, Ohio, Oregon, Pennsylvania, Rhode Island, South Dakota, Tennessee, Utah, Washington, Wisconsin 14 days or less to stay at home orders: Alabama, Alaska, Delaware, Georgia, Idaho, Illinois, Louisiana, Maine, Massachusetts, Michigan, New Jersey, New Mexico, Oklahoma, South Carolina, Vermont, West Virginia, Wisconsin Over 14 days to stay at home orders: Arizona, Arkansas, California, Colorado, Connecticut, District of Columbia, Florida, Hawaii, Indiana, Iowa, Kansas, Kentucky, Maryland, Minnesota, Mississippi, Missouri, Montana, Nebraska, Nevada, New Hampshire, New York, North Carolina, North Dakota, Ohio, Oregon, Pennsylvania, Rhode Island, South Dakota, Tennessee, Texas, Utah, Virginia, Washington, Wyoming. * Rate ratio shows no statistically significant difference between groups at day 262.
Table 2 shows the beta values, P-values and AIC values when assessing the significance of potential confounders in regression analyses when comparing different lengths of time to mask mandates at day 262, organized by increasing AIC values. Only the variables for percent of the state at age 65 and older as well as male gender showed a statistically significant effect on the regression analyses and also lowered the AIC values. Running a regression analysis with both the age and sex terms did resulted in the sex-term losing statistical significance (data not shown). Thus, the final regression model was adjusted only for percent of population aged 65 or over.
Table 2.
Significance of potential confounders in regression analysis calculating rate ratios comparing COVID-19 rates based on different lengths of time to mask mandates at day 262
| Confounder | Akaike's Information Criterion (AIC)-* | Beta value of variable† | P-value |
|---|---|---|---|
| Unadjusted model | 1289.91 | NA | NA |
| Adjustment for sociodemographic variables | |||
| Percent of population in state who are 65 years or older | 1281.93 | −0.0902 | .001 |
| Percent of population in state who are male | 1287.41 | 0.1391 | .03 |
| Percent of population in state represented by an urban population | 1290.61 | 0.0052 | .25 |
| Percent of population in state who use carpooling to get to work | 1291.27 | −0.0332 | .42 |
| Percent of population in state in state who are black | 1291.79 | 0.0019 | .73 |
| Population density of state | 1291.81 | <0.00001 | .76 |
| Percent of population in state who use public transit for work | 1291.85 | −0.0024 | .81 |
| Percent of population in state who are in poverty | 1291.87 | 0.0040 | .84 |
| Adjustment for medical conditions | |||
| Percent of population in state with chronic obstructive pulmonary disease (COPD) | 1290.55 | −0.0309 | .24 |
| Percent of population in state with asthma | 1290.67 | −0.0885 | .26 |
| Percent of population in state with hypertension | 1291.57 | −0.0044 | .56 |
| Percent of population in state with heart failure | 1291.67 | 0.0150 | .62 |
| Percent of population in state with diabetes | 1291.85 | −0.0039 | .81 |
| Ischemic heart disease | 1291.91 | 0.0143 | 1.00 |
Smaller indicates better model.
Effect of variable when added to the regression model examining different lengths to mask mandates and COVID-19 cumulative incidence rates.
Figure 3 shows the rate ratios adjusted for percent of population aged 65 or older, comparing the cumulative incidence in the groups taking longest to implement mask mandates vs the lowest. An adjusted rate ratio comparing states with mask mandates made at one to three months versus one month or less did not result in a statistically significant result (adjusted rate ratio= 1.20, 95% CI: 0.91-1.61, P = .19). States with mask mandates made at three to six months had a 1.61 times higher rate than those who implemented within one month (adjusted rate ratio = 1.61(95% CI: 1.23-2.10), P = .001). States with mask mandates made after six months or with no mandate had a 2.16 times higher rate than those who implemented within one month (adjusted rate ratio = 2.16 (95% CI: 1.64-2.88, P < .0001).
Fig 3.
Rate Ratios, Adjusted for Percent in State Age 65 or Over, Comparing COVID-19 Rates Based on Different Lengths of Time to Mask Mandates at Day 262. *All rate ratios adjusted for percent in state age 65 or over.
Discussion
The goal of this study was to quantify the impact of physical distancing measures and mask mandates implemented by state governments on COVID-19 infection rates while factoring in the effects of several potential confounders using aggregate data from the US Census Bureau and the Centers for Medicare & Medicaid Services. We found that the majority of sociodemographic and health factors did not significantly change the association between government mandates and COVID-19. The variable for percent of population aged 65 and above did significantly change results. After adjusting for this variable, the benefits of issuing mask mandates quickly were apparent, particularly when mandates were issued within a month. The impact of school closings and stay at home orders were less clear.
At the beginning of the pandemic, there were suggestions that the increased COVID-19 rates in certain states were mostly a result of high population density. As state population density does not address what proportion of a state is urbanized and thus susceptible to crowding, we also attempted adjusting for levels of urbanized population within a state. The US Census Bureau defines “urban” as densely developed territories.27 , 28 The results of this study suggest that mask mandates may be helpful regardless of a state's infrastructure. It is telling that the group of states that implemented mask mandates most quickly initially had the highest COVID-19 rates but were eventually able to lower this rate beneath the rates seen in the states that took longer to implement measures.
The results of this study cannot be taken to mean that school closures and stay at home orders are not beneficial. One possibility is that these physical distancing measures may not have occurred soon enough in many areas to make a significant difference. There was also not very much heterogeneity in how many days states took to close schools – this was one of the earliest interventions adopted. Additionally, a lack of statistically significant results with regards to school closures and its consequences on COVID-19 incidence rates should not be interpreted as children being exempt from the risks of COVID-19. It is important to consider that measures are needed to protect children in addition to adults, since children may be susceptible to a rare but severe COVID-19 manifestations. Several infected children have been described with a multisystem inflammatory syndrome, with some cases resulting in death30 , 31. The potential for severe clinical manifestations in children warrants careful deliberation of the opening and closing schools in areas of high disease transmission.
Other published studies support our findings. For instance, the study by Courtemanche et al may be the most similar published study to our analysis, which found no evidence that school closures or bans on large social gatherings affected growth rate. They found that closing restaurant dining rooms/bars and/or entertainment centers/gyms led to significant reductions in the growth rates. There were several aspects of their study that differed from our study, including analysis at the county level, an outcome of daily growth rate, and use of a combined variable for restaurant closure with other types of business closures. Additionally, they did not adjust for epidemics beginning at different time points in different locations or sociodemographic variables.14 The studies by Kaufman et al., Chernozhukov et al and Gallaway et al all suggest wearing masks in public locations is beneficial.19 , 20 , 22
The challenge in the models used in most of the existing studies assessing physical distancing measures is that there is no adjustment for sociodemographic variables. However, it must be recognized that the United States does have several sub-populations that vary in these variables. There must be an acknowledgment that several other variables influence cumulative incidence, including race, age, and poverty. Many COVID-19 analyses suggest a disproportionate burden of illness and death among racial and ethnic minority groups, particularly the Black/African American community.32
A strength in our study was the attempt to statistically adjust for several pertinent confounding variables as opposed to relying only on visual representations of epidemic curves that do not account for subpopulations. However, this approach is also a potential weakness, as the use of aggregate data from a variety of external sources is not ideal. Rather, these socioeconomic variables should be evaluated by using individual level data. In the process of assessing the success of government mandates, it will be crucial to gather statistical support for observations and account for confounding variables so that solid conclusions can be made to help guide public health measures.
There are several other issues to consider when interpreting the results of our study. In terms of physical distancing laws, it is unclear how each state reported their data, which may lead to a great deal of heterogeneity. The definitions for physical distancing measures were vastly different between locations. Additionally, the results of our study are representative only of the US, which has had one of the highest COVID-19 transmission rates. While some other countries have had similarly high transmission rates, nations such as Australia and New Zealand have not shown this level of transmission. It should also be noted that individual personal behaviors vary substantially between countries, with an emphasis on personal civil liberties over public health measures in some.
Enforcement of physical distancing has been much higher in other countries than in the United States. In countries where physical distancing measures such as lockdowns have been enforced, transmission rates have decreased.33 In the US, other than a CDC recommendation for people to stay six-feet apart, there were no enforcements of these rules, making accurate measurement of physical distancing difficult. The CDC has noted that the recommendation would not have been possible to follow in many cities, where public transit is the key form of transportation. Thus, the mask mandates by the CDC were suggested as that may be the only means by which people could protect themselves.
We omitted analysis of restrictions on gatherings, closing of nonessential business and restaurant closures as the definitions were so vastly different between states. Additionally, even when a state implemented a measure, distinct counties and/or cities may have had additional regulations and mandates that were not accounted for here. Finally, we concluded analysis at the time-point where people started to be vaccinated for COVID-19, as this influences COVID-19 rates. Analysis will need to be conducted after vaccination becomes available in larger quantities of individuals to assess the need for government physical distancing mandates in conjunction with vaccination.
Future studies should investigate other control variables. For example, multi-generational households are at a higher risk for disease transmission.34 Square footage of homes and the structure of the home (apartment complexes vs stand-alone homes) may play a role in disease transmission as well.35 Occupations vary greatly in how much physical distancing is feasible as well as how much commuting using public transportation is required.36 There are numerous other variables that can be taken into account in order to accurately assess how COVID-19 transmission can be reduced. Additionally, there are multiple ways data can be analyzed to show risks, trends and disease burden. Analysis could occur using new cases per day, number of hospitalizations or mortality rates, as these may show different patterns than our analysis. Despite the weaknesses in our study our study provides support to the idea of issuing mask mandates on the government level.
There will likely be multiple waves of COVID-19 epidemics throughout the country. Limited data on wearing masks and behaviors towards gatherings suggest that failure to follow these measures may be the most challenging aspect of infection control in the US. A cross-sectional survey of 1,034 US residents showed that 30% of people reported attending gatherings with more than 50 people and 76% of people did not wear masks outside the home.37 In contrast, a Chinese research study reported that only 3.6% of people reported going to crowded places and 2.0% reported not wearing masks outside the home.38 Ultimately, the success of government mandates will be determined by human behavior. Our analysis did not measure compliance with government mandates in any of the states which is an important factor. The United States has a distinct political profile, which has become a large factor in whether or not individuals choose to comply with mask mandates. Results on a study looking at partisanship and mobility found that partisanship was more important than COVID-19 infection in terms of behavior, and rates in Democrats were 13.1% less likely to be socially mobile as compared to independents, while Republicans were 27.8% more likely to be mobile.39
In conclusion, our findings demonstrate the need for an evidence-based public health response to curbing the COVID-19 pandemic. Given the immense toll the pandemic has taken on human lives in nearly every location in the United States, all locations must take basic infection control precautions as well as physical distancing measures. Areas of high risk must may need to implement localized measures that go beyond broader state measures.
The role of mask mandates, stay at home orders and school closure in curbing the COVID-19 pandemic post wide-scale vaccination is needed along with updating infection control guidance with emerging research and best practices. Additionally, further evaluation of mask mandates, stay at home orders, and school closures should be planned as it is not a matter of if there will be a future pandemic, but when. Practical recommendations are also needed to aid policymakers, public health professionals, and infection control practitioners to prevent and respond to future disease outbreaks beyond routine infection prevention and control practices.
Acknowledgments
The authors recognize Daniela Fratielli, MPH Candidate at Hofstra University, for her assistance with background research.
Footnotes
Conflicts of interest: The authors declare that they have no conflict of interest.
References
- 1.Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fauver JR, Petrone ME, Hodcroft EB, et al. Coast-to-coast spread of SARS-CoV-2 during the early epidemic in the United States. Cell. 2020;181:990–996.e5. doi: 10.1016/j.cell.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haffajee RL, Mello MM. Thinking globally, acting locally - The U.S. response to Covid-19. N Engl J Med. 2020;382:e75. doi: 10.1056/NEJMp2006740. [DOI] [PubMed] [Google Scholar]
- 5.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Inf Dis. 2020;20:533-534. [DOI] [PMC free article] [PubMed]
- 6.Goyal P, Choi JJ, Pinheiro LC, et al. Clinical characteristics of covid-19 in New York city. N Engl J Med. 2020;382:2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gandhi RT, Lynch JB, Del Rio C. Mild or moderate covid-19. N Engl J Med. 2020;383:1757–1766. doi: 10.1056/NEJMcp2009249. [DOI] [PubMed] [Google Scholar]
- 8.Van doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schuchat A. Public health response to the initiation and spread of pandemic COVID-19 in the United States, February 24-April 21, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:551–556. doi: 10.15585/mmwr.mm6918e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haffajee R, Parmet WE, Mello MM. What is a public health "emergency"? N Engl J Med. 2014;371:986–988. doi: 10.1056/NEJMp1406167. [DOI] [PubMed] [Google Scholar]
- 11.Stricker RB, Fesler MC. A novel plan to deal with SARS-CoV-2 and COVID-19 disease. J Med Virol. 2020;92:1394–1395. doi: 10.1002/jmv.25945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Honein MA, Christie A, Rose DA, et al. Summary of guidance for public health strategies to address high levels of community transmission of sars-cov-2 and related deaths, December 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1860–1867. doi: 10.15585/mmwr.mm6949e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lasry A, Kidder D, Hast M, et al. Timing of community mitigation and changes in reported COVID-19 and community mobility - Four U.S. Metropolitan Areas, February 26-April 1, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:451–457. doi: 10.15585/mmwr.mm6915e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong social distancing measures in the United States reduced the covid-19 growth rate. Health Aff (Millwood) 2020;39:1237–1246. doi: 10.1377/hlthaff.2020.00608. [DOI] [PubMed] [Google Scholar]
- 15.Prem K, Liu Y, Russell TW, et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang J, Litvinova M, Liang Y, et al. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science. 2020;368:1481–1486. doi: 10.1126/science.abb8001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Matrajt L, Leung T. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg Infect Dis. 2020;26:1740–1748. doi: 10.3201/eid2608.201093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaufman BG, Whitaker R, Mahendraratnam N, Smith VA, McClellan MB. Comparing associations of state reopening strategies with covid-19 burden. J Gen Intern Med. 2020;35:3627–3634. doi: 10.1007/s11606-020-06277-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chernozhukov V, Kasahara H, Schrimpf P. Causal impact of masks, policies, behavior on early covid-19 pandemic in the U.S. J Econom. 2021;220:23–62. doi: 10.1016/j.jeconom.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eikenberry SE, Mancuso M, Iboi E, et al. To mask or not to mask: modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect Dis Model. 2020;5:293–308. doi: 10.1016/j.idm.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gallaway MS, Rigler J, Robinson S, et al. Trends in covid-19 incidence after implementation of mitigation measures - Arizona, January 22-August 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1460–1463. doi: 10.15585/mmwr.mm6940e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lyu W, Wehby GL. Community use of face masks and covid-19: evidence from a natural experiment of state mandates in the us. Health Aff (Millwood) 2020;39:1419–1425. doi: 10.1377/hlthaff.2020.00818. [DOI] [PubMed] [Google Scholar]
- 24.Isaacs D, Britton P, Howard-Jones A, et al. Do facemasks protect against COVID-19? J Paediatr Child Health. 2020;56:976–977. doi: 10.1111/jpc.14936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oliver SE, Gargano JW, Marin M, et al. The advisory committee on immunization practices’ interim recommendation for use of pfizer-biontech covid-19 vaccine - united states, december 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1922–1924. doi: 10.15585/mmwr.mm6950e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fullman N, Bang-Jensen B, Reinke G, et al. "State-level social distancing policies in response to COVID-19 in the US". Version 1.108, December 17, 2020. Available at: http://www.covid19statepolicy.org. Accessed December 14, 2020.
- 27.U.S. Census Bureau. (2010). U.S. Census Bureau, tables P1, P009, DP03. Available at: https://data.census.gov/cedsci/>. Accessed May 15, 2020.
- 28.U.S. Census Bureau; American Community Survey, 2018 American Community Survey 1-Year Estimates, tables S2801, S0101. Available at: https://data.census.gov/cedsci/>. Accessed May 15, 2020.
- 29.Centers for Medicare & Medicaid Services. Table: Prevalence State/County Level: All Beneficiaries by Age, 2017. Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/CC_Main>. Accessed May 15, 2020.
- 30.Feldstein LR, Rose EB, Horwitz SM, et al. Multisystem inflammatory syndrome in U. S. Children and adolescents. N Engl J Med. 2020;383:334–346. doi: 10.1056/NEJMoa2021680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Viner RM, Whittaker E. Kawasaki-like disease: emerging complication during the COVID-19 pandemic. Lancet. 2020;395:1741–1743. doi: 10.1016/S0140-6736(20)31129-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Millett GA, Jones AT, Benkeser D, et al. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol. 2020;47:37–44. doi: 10.1016/j.annepidem.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alfano V, Ercolano S. The efficacy of lockdown against covid-19: a cross-country panel analysis. Appl Health Econ Health Policy. 2020;18:509–517. doi: 10.1007/s40258-020-00596-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Househ Madewell ZJ, Yang Y, Longini IM, Halloran ME, Dean NE. Household transmission of sars-cov-2: a systematic review and meta-analysis. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.31756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Accorsi EK, Samples J, McCauley LA, Shadbeh N. Sleeping within six feet: challenging oregon's labor housing covid-19 guidelines. J Agromed. 2020;25:413–416. doi: 10.1080/1059924X.2020.1815622. [DOI] [PubMed] [Google Scholar]
- 36.Masotti F, Cattaneo S, Stuknytė M, Pica V, De Noni I. Transmission routes, preventive measures and control strategies of SARS-CoV-2 in the food factory. Crit Rev Food Sci Nutr. 2021;2:1–12. doi: 10.1080/10408398.2021.1879728. [DOI] [PubMed] [Google Scholar]
- 37.Clements JM. Knowledge and behaviors toward COVID-19 among US residents during the early days of the pandemic: cross-sectional online questionnaire. JMIR Public Health Surveill. 2020;6:e19161. doi: 10.2196/19161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhong BL, Luo W, Li HM, et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. 2020;16:1745–1752. doi: 10.7150/ijbs.45221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Clinton J, Cohen J, Lapinski J, Trussler M. Partisan pandemic: how partisanship and public health concerns affect individuals’ social mobility during COVID-19. Sci Adv. 2020;7:eabd7204. doi: 10.1126/sciadv.abd7204. [DOI] [PMC free article] [PubMed] [Google Scholar]