Abstract
Objectives
To evaluate if a values clarification workshop conducted at Catholic hospital training programs influenced obstetrics and gynecology residents' abortion attitudes.
Study design
Between 2018 and 2019, we provided a values clarification workshop focused on abortion care to 47 obstetrics and gynecology residents at five Catholic programs that do not provide abortion training. Participants received a pre-survey eliciting participant characteristics, and training experiences. On pre- and post-surveys, we asked participants to respond to abortion scenarios using a five-point Likert scales (1 = strongly disagree, 2 = somewhat disagree 3 = neither agree nor disagree, 4 = somewhat agree, 5 = strongly agree). We calculated descriptive frequencies, report the proportions agreeing with the statements (Likert ≥ 4) before and after the workshop, and compared median Likert responses using Wilcoxon matched pair test.
Results
Forty-one participants (87%) completed both surveys. Twelve (29%) reported Catholic religion, six (15%) reported their personal reproductive care views were in line with their institution, and five (12%) selected their program based on its religious affiliation. Three (9%) had experience with first-trimester abortion for nonmedical reasons, and 20 (49%) planned to provide such care after graduation. Both before and after the workshop, all participants could think of a justification why a patient with an undesired pregnancy would choose abortion. After the workshop, more residents were able to think of a justifiable reason for the following abortion-related scenarios: (1) patients declining post-abortal contraception (51% vs. 78%, p < 0.001), (2) patients presenting for subsequent abortion (93% vs 95%, p = 0.01), and (3) patients presenting for second-trimester abortion (93% vs. 100%, p = 0.001). Many participants increased their Likert score when asked about acceptability of patients declining post-abortal contraception (n = 24, 59%), patients seeking a subsequent abortion (n = 15, 37%), and patients obtaining a second trimester abortion contraception (n = 11, 27%). Emotional and professional reactions to these scenarios were unchanged. After the workshop, residents were more likely to consider either financial inability (73% vs. 83%, p < 0.01) or disruption to career or education (71% vs 80%, p < 0.01) as morally acceptable reasons for requesting an abortion. For abortion for a patient who is financially unable to support their child, 12 (29%) increased their Likert score, 1 (2%) had a lower score and the remaining 28 (68%) had no change. For abortion for a patient whose career or education would be disrupted 13 (32%) increased their Likert score, one (2%) had a lower score and the remaining 27 (66%) had no change.
Conclusion
Our values clarification workshop resulted in more residents at Catholic training programs endorsing accepting attitudes toward abortion patient scenarios. Values clarification exercises can be a useful tool for residents to discuss abortion care, especially when training is insufficient.
Implications
Most obstetrics and gynecology residents at Catholic hospitals experience limited training in abortion care. A values clarification workshop conducted at such programs may result in increasing resident acceptance of abortion-related patient care scenarios and may help reduce abortion stigma.
Keywords: Abortion training, Catholic; Faith-based; Obstetrics and gynecology residency; Values clarification
Highlights
-
•
Most ob-gyn residents at Catholic site are accepting of patients choosing abortion.
-
•
Values Clarification workshops result in increasing acceptance of abortion scenarios.
-
•
Workshops may help reduce abortion stigma when residents lack abortion training.
1. Introduction
The Accreditation Council of Graduate Medical Education (ACGME) requires routine abortion training at all obstetrics and gynecology (ob-gyn) programs, regardless of religious affiliation [1]. Ob-gyn residents training at Catholic hospital programs, however, face barriers to abortion training based on institutional guidelines that restrict abortion services in Catholic health care facilities [2,3]. Between 2018 and 2019 approximately 8% of ACGME accredited ob-gyn residency programs primarily trained residents (> 70% of resident clinical time) in Catholic hospitals [2]. When program directors at these Catholic programs were given the option to rate their residents' experience, 47% rated abortion training as poor, 42% as adequate, and 11% as strong [2]. As a result of abortion training gaps, residents and graduates from Catholic training programs have reported concerns over their ability to counsel and provide family planning services to their patients in both Catholic and secular settings [4,5].
If ob-gyn residents do not gain adequate exposure to abortion services, they may not fully understand the situations in which patients present for abortion care. Recent attention has been drawn to the concept of abortion stigma defined as “a negative attribute ascribed to women who seek to terminate a pregnancy that marks them, internally or externally, as inferior to the ideals of womanhood.” [6] Part of enacted abortion stigma includes actual experiences of discrimination or negative treatment by others that are related to a woman's abortion experience [7]. Given that Catholic healthcare settings exclude abortion care as part of women's health care, and in part discriminate against such care, it is possible that these training experiences perpetuate or reinforce abortion stigma amongst these physicians. Further, such physicians may already be predisposed to abortion stigma based on other factors such as personal affiliation with Catholicism [7].
Values clarification workshops are exercises in articulating how personal values influence the way in which providers interact with patients seeking abortion [8]. Prior studies have highlighted the impacts of values clarification workshops on abortion providers and others involved in the provision of abortion services [8,9]. Less is known about the impact on physicians who are not exposed to abortion services, especially those who work in settings that prohibit abortion care. In this study, we set out to understand whether a values clarification workshop influences abortion attitudes of ob-gyn residents at U.S. training programs that are based in Catholic hospitals and lack abortion training.
2. Materials and methods
Between 2018 and 2019, we provided a values clarification workshop to 47 residents at five obstetrics and gynecology residency training programs that did not have routine abortion training and were primarily associated with Catholic hospitals; three were located in the Midwest, one in the Southeast, and one in the West regions of the U.S. One session was a combination of two nearby programs. We recruited interested programs at the 2019 APGO-CREOG annual meeting and also surveyed interest with a prior survey of educational leaders at ob-gyn residency programs affiliated with Catholic hospitals [2]. We arranged sessions during protected educational time and the Kenneth J. Ryan Residency Program funded sessions so that programs did not incur any costs. Some sessions included medical students and faculty members.
At each site, one moderator (MG) led a 2-hour values clarification workshop that included five components directly taken or modified from Ipas's values clarification guide called: “Abortion Attitude Transformation: A Values Clarification Toolkit for Global Audiences.” [11] Ipas is an international organization focused on expanding access to safe abortion and contraceptive care [12]. Ipas provides Values Clarification activities as a resource to help facilitators in the field of sexual and reproductive health discuss conflicting attitudes about abortion care [11]. Prior to conducting this study, the moderator had experience conducting values clarification exercises at a secular obstetrics and gynecology residency training site and also at a Catholic residency training site not included in this study. Based on her experiences and feedback from trainees, she selected the exercises that appeared most effective at the Catholic site. She also revised the specific exercises to address current and relevant abortion controversies.
Participants were first introduced to the session by reading aloud the ACGME abortion training requirement and discussing ground rules including respect for differing opinions. Next, the participants partook in “Cross the Line.” In this exercise, an imaginary line was designated in the middle of the space and participants were instructed to cross the line if they agreed with statements read by the moderator. Representative statements included “I was raised to believe abortion is wrong,” and “At some point in my life, I believed abortion is wrong.” The moderator asked residents to comment on their experiences and facilitated reflections about abortion stigma. In the third exercise, “Reasons Why,” participants were asked to list the reasons why women have sex, become pregnant, have unintended pregnancies, continue unintended pregnancies, terminate pregnancies, and make decisions about their unintended pregnancies that they really do not want to make. In the fourth exercise, “Continuum,” participants were instructed to move anywhere from one side of the space designated as “strongly agree” to the other side designated as “strongly disagree” in response to statements made by the moderator. Representative statements included “Women having more than one abortion are irresponsible,” “Parental consent should be required for minors seeking abortion,” and “A woman should be able to terminate a pregnancy if she is raped.” Participants were then provided opportunities to reflect on their views and values about abortion care. In the fifth exercise, “The Last Abortion,” participants were placed in small groups and given six pregnancy scenarios to read. They were instructed to reach small group consensus by assigning continuing the pregnancy to two patients, adopting out to two patients, and abortion provision to two patients. Subsequently, the larger group reconvened and reviewed selections as a way of stimulating discussion related to their professional obligations. Finally, residents completed a closing reflections exercise.10
In order to evaluate the workshop, we used and modified pre- and post-workshop surveys from existing surveys created by the Kenneth J. Ryan Residency Training program for their Professionalism in Reproductive Health Workshop. All surveys were voluntary and anonymous. Participants were asked to record the last four digits of their pager number for identification purposes. The University of California San Francisco Institutional Review Board deemed this survey exempt from review given the educational nature and since no identifiers were collected.
Our pre-survey included queries about abortion training experiences, plans for abortion provision after graduation, and relevant participant characteristics including religiosity measures. We focused our queries on four abortion-related scenarios: (1) A woman who has an undesired pregnancy and chooses to have an abortion (woman choosing abortion); (2) A woman who just underwent an abortion and is not interested in starting a birth control method (post-abortal contraception); (3) A woman who has had an abortion in the past and now presents with an undesired pregnancy and wants another abortion (subsequent abortion); (4) A woman who has an undesired pregnancy and presents for care for the first time at 19 weeks' gestation (second-trimester abortion).
To assess how accepting they were of these scenarios we used the statement “I can think of justifiable reasons that would explain why the patient is in this circumstance and makes this decision” and asked them to report using a five-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree). To assess their emotional reactions, we asked them to respond with the same Likert scale to “This case makes me feel frustrated.” To assess their professional reactions to these scenarios, we asked them to respond to “My reaction to this case would make it hard for me to care for this patient.” Using the same Likert scale, we also assessed the extent to which they found the following reasons for abortion to be morally acceptable: (1) patient is financially unable to support the child; (2) patient's career/education would be disrupted; (3) the pregnancy is a result of rape or incest; and (4) the pregnancy is a threat to her physical health.
For data analyses, we only included surveys completed by obstetrics and gynecology residents both before and after the session. We performed data analyses using SPSS 26 (IBM, Armonk) and calculated descriptive frequencies. To compare queries related to abortion scenarios we compared median Likert responses using Wilcoxon paired tests (also known as Wilcoxon signed-rank test) given that the data were not normally distributed. We considered p-values < 0.05 as significant.
3. Results
Amongst the 47 participating residents, 41 (87%) completed both the pre- and post-workshop surveys and were included in analyses. There were relatively equal proportions of participating residents across each postgraduate year (PGY): 34% PGY 1 (n = 14), 26% PGY2 (n = 11), 23% PGY 3 (n = 9), 17% PGY 4 (n = 7). The most common self-reported religious affiliated was Catholic (n = 12, 29%). Other religious affiliations commonly reported included None/Agnostic/Atheist (n = 11, 27%), Christian (n = 8, 20%), and Protestant (n = 4%). With respect to religiosity, 51% (n = 21) reported that religion is either “important” or “very important” in their life. Fifteen percent (n = 6) reported that their personal reproductive care views were in line with their institution and 12% (n = 5) reported they selected their residency training program based on its religious affiliation.
Table 1 demonstrates prior uterine-evacuation experiences with respect to different indications and resident plans to provide abortion services after graduation. Overall, the proportion of residents with exposure to uterine-evacuation methods for nonmedical reasons was low and increased for indications of pregnancy complications and miscarriage management. Abortion experiences contrasted with their plans to provide such services after graduation, which were overall higher proportions.
Table 1.
Resident report on pre-workshop survey of prior experiences with uterine-evacuation-related services according to indications and corresponding plans to provide such services after graduation for nonmedical indications.
| Uterine evacuation- related services | Prior experience with according to indication |
Desire to provide service for nonmedical reason after graduation | ||
|---|---|---|---|---|
| Non-medical indication | Pregnancy complication⁎ | Miscarriage management | ||
| Comprehensive pregnancy options counseling | 26 (74.3) | n/a | n/a | 41 (100) |
| First-trimester medication abortion | 2 (5.7) | 13 (37.1) | 32 (91.4) | 23 (56.1) |
| First-trimester uterine aspiration | 3 (8.6) | 12 (34.3) | 28 (80.0) | 20 (48.8) |
| Second-trimester D&E | 3 (8.6) | 6 (17.1) | 14 (40.0) | 13 (31.7) |
| Second-trimester induction | 1 (2.8) | 13 (37.1) | 27 (77.1) | 11 (26.8) |
| Referral for abortion care | 15 (42.9) | n/a | n/a | 34 (82.9) |
N = 41.
Data are n (%).
Survey specified “pregnancy complication” in addition to “miscarriage management” to reflect scenarios in Catholic hospitals that may warrant approvals including incomplete abortions with ongoing fetal heart tones.
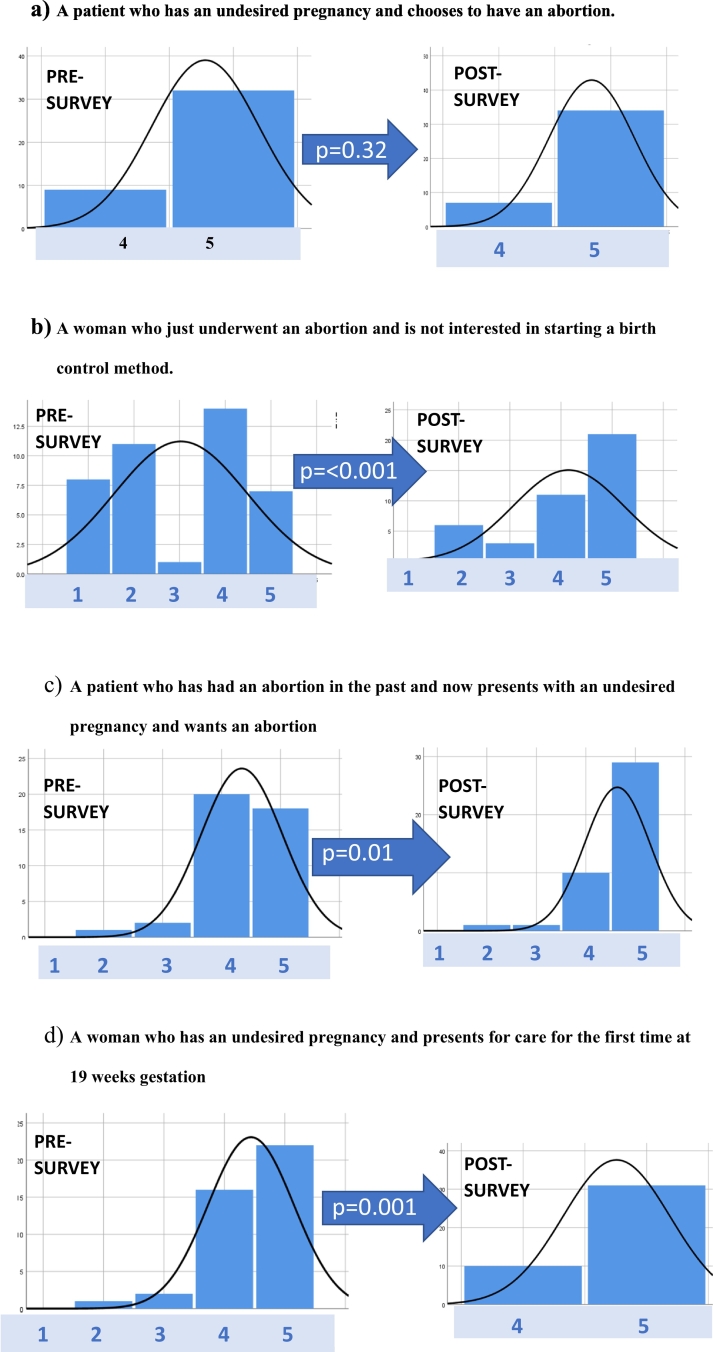
Table 2 demonstrates matched pre- and post-survey responses to the varying statements related to abortion scenarios. Acceptability of a woman choosing an abortion did not change significantly before and after the session and were high to begin with (all were accepting before and after). After the session, there were higher levels of acceptability for patients who decline post-abortal contraception (p < 0.001), those seeking a subsequent abortion (p = 0.01), and those obtaining second-trimester abortion (p = 0.001). Higher proportions of participants agreed that patients were justified in making these decisions in the post-survey (Table 2). Table 3 demonstrates how Likert scores in response to scenarios changed amongst participants. Fig. 1 visually depicts findings with respect to acceptability of abortion scenarios and highlights how pre-survey reactions shifted to more positive ones in the postsurvey assessments.
Table 2.
Comparison of resident responses regarding whether abortion-related scenarios are justifiable, measured at baseline and following the Values Clarification Workshop.
| Abortion-related scenario | Pre-survey Median (range) |
Agreed with scenario on pre-survey⁎ n (%) |
Post-Survey Median (range) |
Agreed with scenario on post-survey⁎ n (%) |
P^ |
|---|---|---|---|---|---|
| “I can think of justifiable reasons that would explain why the patient is in this circumstance and makes this decision” | |||||
| Patient with undesired pregnancy has abortion | 5 (4–5) | 41 (100) | 5 (4–5) | 41 (100) | 0.32 |
| Patient declines post-abortal contraception | 4 (1–5) | 21 (51) | 5 (2–5) | 32 (78) | < 0.001 |
| Patient presenting for subsequent abortion | 4 (2–5) | 38 (93) | 5 (2–5) | 39 (95) | 0.01 |
| Patient presenting for second-trimester abortion | 5 (2–5) | 38 (93) | 5 (4–5) | 41 (100) | 0.001 |
| “This case makes me feel frustrated” | |||||
| Patient with undesired pregnancy has abortion | 1 (1–5) | 7 (17) | 1(1–5) | 5 (12) | 0.60 |
| Patient declines post-abortal contraception | 4 (1–5) | 30 (73) | 4 (1–5) | 23 (56) | 0.04 |
| Patient presenting for subsequent abortion | 4 (1–5) | 22 (54) | 4 (1–5) | 23 (56) | 0.49 |
| Patient presenting for second-trimester abortion | 3 (1–4) | 15 (37) | 2 (1–5) | 14 (34) | 0.22 |
| “My reaction to this case would make it hard for me to care for this patient” | |||||
| Patient with undesired pregnancy has abortion | 1 (1–3) | 0 (0) | 1 (1–5) | 5 (12) | 0.53 |
| Patient declines post-abortal contraception | 1 (1–4) | 6 (15) | 1 (1–5) | 6 (15) | 0.75 |
| Patient presenting for subsequent abortion | 1 (1–5) | 3 (7) | 1 (1–5) | 4 (10) | 0.28 |
| Patient presenting for second-trimester abortion | 1 (1–5) | 2 (5) | 1 (1–5) | 1 (2) | 0.13 |
N = 41.
Likert scale: 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree.
^P is Wilcoxon matched test.
Based on a Likert scale response of 4 or 5.
Table 3.
Change in Participants' Likert Score following the Values Clarification Workshop ( = 41).
| Abortion-related scenario | Higher Likert score after workshop | Likert Score remained the same after workshop | Lower Likert Score after workshop |
|---|---|---|---|
| “I can think of justifiable reasons that would explain why the patient is in this circumstance and makes this decision” | |||
| Patient declines post-abortal contraception | 24 (59) | 17 (41) | 0 (0) |
| Patient presenting for subsequent abortion | 15 (37) | 25 (61%) | 1 (2%) |
| Patient presenting for second-trimester abortion | 11 (27) | 30 (73) | 0 (0) |
| Abortion-scenario is morally acceptable | |||
| Patient is financially unable to support child | 12 (29) | 28 (68) | 1 (2) |
| Patient's career/education would be disrupted | 13 (32) | 27 (66) | 1 2) |
| The pregnancy is a result of rape or incest | 5 (12) | 35 (85) | 1 (2) |
| The pregnancy is a threat to her physical health | 4 (10) | 17 (41) |
Data is n(%).
Fig. 1.
Pre and post Likert scale responses related to the statement “I can think of justifiable reasons that would explain why the patient is in this circumstance and makes this decision.”
Likert scale: 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree
P is Wilcoxon matched test.
Overall emotional and professional reactions did not change after the workshop (Table 2). Although many participants agreed that the scenarios make them feel frustrated, most disagreed with the statement “My reaction to this case would make it hard for me to care for this patient.” When asked about when abortion is morally acceptable, most had favorable views (“agree” or “strongly agree”) at baseline (Table 4). Participants became even more accepting after the workshop (Table 3), especially of patients presenting with financial inability (p < 0.01) and/or for disruption to career or education (p < 0.01).
Table 4.
Comparison of resident responses regarding whether abortion scenarios are morally acceptable, measured at baseline and following the Values Clarification Workshop.
| Abortion scenario | Pre-survey Median (range) |
Agree on pre-survey⁎ n (%) |
Post-Survey Median (range) |
Agree on post-survey⁎ n (%) |
P^ |
|---|---|---|---|---|---|
| Patient is financially unable to support child | 5 (2–5) | 30 (73) | 5 (1–5) | 34 (83) | < 0.01 |
| Patient's career/education would be disrupted | 4 (2–5) | 29 (71) | 5 (1–5) | 33 (80) | < 0.01 |
| The pregnancy is a result of rape or incest | 5 (2–5) | 38 (93) | 5 (3–5) | 40 (98) | 0.08 |
| The pregnancy is a threat to her physical health | 5 (2–5) | 39 (95) | 5 (3–5) | 40 (98) | 0.06 |
N = 41.
Likert scale: 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree.
^P is Wilcoxon matched test.
Based on a Likert scale response of 4 or 5.
4. Discussion
Our study highlights the impact of a values clarification workshop on ob-gyn physicians who work in settings that restrict abortion care, but nonetheless interact with patients who may request or need such services. We found that after our values clarification workshop more residents were accepting of abortion-related scenarios including declining post-abortal contraception, presenting for a subsequent abortion and presenting for second trimester abortion. This was especially true for those who had less-supportive pre-workshop views about abortion. Such reactions are consistent with those of abortion care providers participating in similar workshops [10]. For many participants, the workshop provided a forum for open discussion related to different abortion scenarios and concerns. Participants heard from their peers and colleagues about different abortion scenarios experienced by their patients, friends, family members, and sometimes even themselves, which likely provided greater insights on the scenarios in which abortion patients may be in. As our workshop influenced attitudes related to acceptability and morality of abortion scenarios, it may contribute to unmeasured reductions in abortion stigma they consciously or unconsciously have that negatively impact their interactions with patients. This education intervention is especially valuables as graduates of such programs who go on to work in secular settings have reported that they often feel ill equipped to care for patients in need of abortion care services [5].
Our survey also provides insights regarding obstetrics and gynecology residents who train at Catholic hospital programs that do not provide abortion training. We found that most of these residents do not have reproductive views in line with their institutions' policies, most did not choose their residency program based on its religious affiliation, and most have overall accepting views of abortion scenarios. Such findings are consistent with a prior survey of residents at faith-based programs that demonstrated relatively high proportions that plan to provide family planning services [4]. These findings speak against the presumption that such residents self-select into the programs based on limitations on family planning service provision. As many of the residents plan to provide services after graduation, our findings emphasize the ongoing need to support ob-gyn training programs at Catholic hospitals in order to prepare trainees to take the best possible care of their patients.
There are limitations to this study. Notably, our survey only accounted for short-term changes and we cannot comment on long-term influences. All sessions were conducted by one moderator who is an abortion provider, which may impact respondent bias. We recruited approximately 22% of the U.S. ob-gyn programs that primarily train at Catholic hospitals. The impact of values clarification exercises on residents at other Catholic institutions may be less pronounced, especially at programs that provide abortion training. It is also possible that residents who did not complete the surveys purposely did so based on the nature of the session and because they had fewer accepting views, despite the anonymous nature. Further, responses were based on self-report and it is possible that residents may inaccurately interpret their own biases including professional reactions. While there may be concerns for our small sample size, we were able to detect significant differences. Strengths of our study include that we were able to provide insights about this population of residents, that our workshop can be replicated, and that by having one moderator conduct the workshop at each of the participating sites it improved our ability to examine the impact of the workshop when using pooled analyses.
A recent survey of program directors at U.S. obstetrics and gynecology residency programs found that 73% of programs faced at least some institutional or governmental restriction on abortion provision and training, with hospital policy being the most common barrier [13]. While our findings are limited to residents in Catholic training settings, it is likely that values clarification workshops similarly impact trainees in other settings, especially those that have inadequate exposure to abortion care. As such program wrestle with ongoing barriers to the provision of abortion training, implementing innovative educational strategies like this one are needed to prepare all ob-gyns in providing nonjudgmental and professional care to their patients, regardless of the reproductive care circumstances in which they present.
Footnotes
Declarations of interest: The findings and conclusions in this article are those of the authors and do not necessarily reflect the views of Planned Parenthood Federation of America, Inc.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding Source
Dr. Guiahi received faculty support, honoraria, and travel support from the Kenneth J. Ryan Residency Training Program to conduct workshops. Otherwise, this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The Kenneth J. Ryan Residency Training Program had no role in the study design, collection, analysis, interpretation of the data, writing of the report or decision to submit the article for publication.
References
- 1.Accreditation Council for Graduate Medical Education Review Committee for Obstetrics and Gynecology Clarifications of Program Requirements. http://www.acgme.org/portals/0/pfassets/programresources/220_obgyn_abortion_training_clarification.pdf Retrieved April 27, 2020.
- 2.Guiahi M., Teal S., Kenton K., DeCesare J., Steinauer J. Family planning training at Catholic and other religious hospitals: a national survey. Am J Obstet Gynecol. 2020;222(3):273 e271–273 e279. doi: 10.1016/j.ajog.2019.09.012. [DOI] [PubMed] [Google Scholar]
- 3.Smith J.F., Jr. Should Catholic academic health centers sponsor residency training in obstetrics and gynecology? J Grad Med Educ. 2019;11(6):629–631. doi: 10.4300/JGME-D-19-00355.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guiahi M., Westhoff C.L., Summers S., Kenton K. Training at a faith-based institution matters for obstetrics and gynecology residents: results from a regional survey. J Grad Med Educ. 2013;5(2):244–251. doi: 10.4300/JGME-D-12-00109.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guiahi M., Hoover J., Swartz M., Teal S. Impact of Catholic Hospital affiliation during obstetrics and gynecology residency on the provision of family planning. J Grad Med Educ. 2017;9(4):440–446. doi: 10.4300/JGME-D-16-00496.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar A., Hessini L., Mitchell E.M.H. Conceptualizing abortion stigma, Culture, Health & Sexuality. 2009;11(6):625–639. doi: 10.1080/13691050902842741. [DOI] [PubMed] [Google Scholar]
- 7.Hanschmidt F., Linde K., Hilbert A., Riedel-Heller S.G., Kersting A. Abortion stigma: a systematic review. Perspect Sex Reprod Health. 2016;48(4):169–177. doi: 10.1363/48e8516. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization (WHO) WHO; 2. Geneva: 2012. Safe abortion: technical and policy guidance for health systems. [PubMed] [Google Scholar]
- 9.Harris L.H., Debbink M., Martin L., Hassinger J. Dynamics of stigma in abortion work: findings from a pilot study of the providers share workshop. Soc Sci Med. 2011;73(7):1062–1070. doi: 10.1016/j.socscimed.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 10.Turner K.L., Pearson E., George A., Andersen K.L. Values clarification workshops to improve abortion knowledge, attitudes and intentions: a pre-post assessment in 12 countries. Reprod Health. 2018 Mar 5;15(1):40. doi: 10.1186/s12978-018-0480-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Turner K.L., Chapman Page K. 2014. Abortion attitude transformation: A values clarification toolkit for global audiences. Ipas. [Google Scholar]
- 12.Ipas 1998–2020. https://www.ipas.org/;
- 13.Turk J.K., Landy U., Chien J., Steinauer J.E. Sources of support for and resistance to abortion training in obstetrics and gynecology residency programs. Am J Obstet Gynecol. 2019;221(2):156 e151–156 e156. doi: 10.1016/j.ajog.2019.04.026. [DOI] [PubMed] [Google Scholar]