Abstract
Background
Women represent an increasing proportion of the oncology workforce; however, globally this does not translate into leadership roles, reflecting disparities in career opportunities between men and women. The Spanish Society of Medical Oncology (SEOM) undertook a survey to investigate gender disparity in the Spanish oncology context.
Design
An online survey was made available to SEOM medical oncologists between February and May 2019. It included demographics, professional context and achievements, parenthood and family conciliation issues, workplace gender bias, and approaches to address disparities.
Results
Of the 316 eligible respondents, 71.5% were women, 59.5% were aged 45 or younger, and 66.1% had children. Among women, 12.4% were division or unit heads, compared with 45.5% of men, with most women (74.3%) being attending medical oncologists, compared with 45.5% of men. More males were professors (34.4% versus 14.2% of females), had a PhD (46.7% versus 28.8%), and/or had led clinical research groups (41.1% versus 9.7%). Spending time overseas after completing a residency was also more common for men than women (34.4% versus 20.4%). Professional satisfaction was similar between genders, driven primarily by patient care and intellectual stimulation. More women (40.7%) considered parenthood to have a strong negative impact on their career, compared with men (9.0%). Main perceived barriers to gender equality included a lack of work–life balance (72.6% women, 44.4% men), bias of peers and superiors (50.0% women, 18.9% men), and different career goals (41.2% women, 24.4% men). Preferred solutions included educational programs and scholarships (52.9%), communication and leadership training (35.8%), childcare at conferences (33.2%), and postmaternity return-to-work incentives (32.0%).
Conclusion
There is a clear paucity of equal opportunities for female oncologists in Spain. This can be addressed by encouraging professional development and merit recognition particularly for younger female oncologists, and empowering women to be involved in management and leadership of institutions and professional societies.
Key words: gender, Spain, survey, oncology, women
Highlights
-
•
Under-representation of women in leadership roles in oncology is a widely acknowledged issue receiving global attention.
-
•
This study is a national description of leadership and educational opportunities in terms of gender and family circumstances.
-
•
Perceptions of gender bias in the workplace gender inequality or family conciliation issues and are described.
-
•
Initiatives for equal opportunities in oncology are needed supporting female academic career development and recognition.
Introduction
The subject of the gender gap in the professional context is increasingly the focus of attention worldwide. While there has been notable progress in reducing this gap over the past few decades, many recent studies have highlighted ongoing challenges confronting females in the health and science workplace in terms of equal opportunities in a variety of cultural contexts. Women account for approximately two-thirds of all workers in the health care area,1 and this trend is continuing. In Spain, 2019 membership data of the Spanish Society of Medical Oncology (SEOM) showed a higher proportion of female oncologists (59%). This predominance is increasingly pronounced in younger age brackets. In a survey of female and male oncologists performed by the European Society for Medical Oncology (ESMO) Women for Oncology (W4O) Committee in 2016, 67% of responding females were aged under 45.2 A similar trend is apparent in the SEOM, with female members accounting for nearly three-quarters of medical oncologists aged 35 and younger in 2019.3
While globally women occupy a large proportion of positions within the oncology field, this does not translate into an equivalent presence in senior and leadership roles in academic or clinical settings, in either the public or the private domain. This disparity is both deep seated and multifactorial, and is seen in a variety of settings. Women are underrepresented as presenters at major oncology conferences, a recognized platform for breakthrough clinical research. An analysis covering nearly a decade of annual meetings of the American Society of Clinical Oncology (ASCO) and ESMO showed that only 21% of oral presentations were by women, that women represented 28% of all abstract authors, and that the proportion of female presenters has not changed significantly over this period.4 Similarly, fewer women are recipients of prestigious rewards in the scientific and medical settings.5 Female participation at an educative level in oncology training programs and grand rounds seminars is also weaker, and is particularly pronounced at the leadership level.6,7 With the proportion of female oncologists continuing to increase, it is essential that gender disparities be addressed.
A number of surveys over the last few years have reported on the underrepresentation of women oncologists in leadership roles worldwide, as well as women's perception of the role of gender in their professional environment.2,8, 9, 10, 11 Cultural factors can be strong gender drivers in the professional environment, with women experiencing different challenges and playing different roles in the workplace according to the cultural setting. To better understand the role of gender in professional satisfaction and career development in the oncology field in the Spanish context, the SEOM Working Group of Women in Oncology developed a questionnaire for its members, both male and female, focusing on the perceptions of gender issues in the professional context and what can potentially be done to address any imbalances.
Materials and methods
All SEOM members were invited to complete the questionnaire. To be eligible, participants had to be an SEOM member and a medical oncologist, either qualified or in training. The questionnaire was developed by the SEOM's New Working Group of Women in Oncology, and was adapted from the ESMO survey.2 Responses were anonymous. It consisted of 39 questions in Spanish, addressing demographics, professional context, professional achievements, parenthood, and gender impact in the workplace, and possible approaches to address these (see Supplementary Information, available at https://doi.org/10.1016/j.esmoop.2021.100048). Questions had prespecified multiple-choice answers, and for some questions more than one answer and/or open text was possible.
The survey was available online from February to May 2019. SEOM members were informed via the weekly electronic newsletter and a personalized email sent mid-way during the survey availability period. A link to the survey was also promoted on the SEOM website. The survey was hosted on the SEOM website, and respondents could complete it online at the time and location of their choice. Participants were informed that the survey was voluntary and that data were being collected anonymously. All data were automatically collected and downloaded into MS Excel (2010).
A descriptive analysis of study variables was performed. Categorical variables were expressed as absolute values and percentages. Fisher's exact test was used to compare the percentage of responses across gender. Multivariate analysis was not conducted and no correction for multiple testing was performed due to the exploratory nature of the study. The data analyses were carried out using R statistical software package version 3.6.2 (The R Foundation).
Results
Population demographics
Responses were collected from 318 of the 2151 members contacted, two of whom were ineligible (not medical oncologists). Members from all 17 Spanish autonomous communities responded, with the regions of Madrid, Catalonia, Valencia, and Andalusia being the most highly represented, together accounting for 58.2% of respondents. Other regions each represented between 1.0% and 6.7% of the analyzed population.
Demographics are presented in Table 1. Among the 316 respondents, 226 (71.5%) were women and 90 (28.5%) were men. Respondents were aged between 27 and 70, with 59.5% aged 45 or younger. All professionally active age groups were well represented. In terms of marital status, the majority of respondents (76.9%) were married or living as a couple, and 66.1% of the population had children, with half of the cohort having either one or two children. A higher proportion of female respondents had no children compared with male respondents (38.5% versus 24.4%, P = 0.02).
Table 1.
Demographics, professional, and academic characteristics of survey participants
| Total n (%) (N = 316) |
Females n (%) (N = 226) |
Males n (%) (N = 90) |
|
|---|---|---|---|
| Female | 226 (71.5) | — | — |
| Age (years) | |||
| ≤30 | 35 (11.7) | 29 (12.8) | 6 (6.7) |
| 31-40 | 110 (34.8) | 90 (39.8) | 20 (22.2) |
| 41-50 | 88 (27.8) | 66 (29.2) | 22 (24.4) |
| 51-65 | 76 (24.1) | 38 (16.8) | 38 (42.2) |
| >65 | 7 (2.2) | 3 (1.3) | 4 (4.4) |
| Marital status | |||
| Married/partner | 244 (77.2) | 166 (73.4) | 78 (86.7) |
| Single | 57 (18.0) | 51 (22.6) | 6 (6.7) |
| Separated/divorced/widowed | 15 (4.7) | 9 (4.0) | 6 (6.7) |
| Number of children | |||
| 0 | 109 (34.5) | 87 (38.5) | 22 (24.4) |
| 1 | 47 (14.9) | 36 (15.9) | 11 (12.2) |
| 2 | 113 (35.7) | 74 (32.7) | 39 (43.3) |
| 3-5 | 47 (14.9) | 29 (12.8) | 18 (20.0) |
| Institution position | |||
| Attending medical oncologist | 209 (66.1) | 168 (74.3) | 41 (45.5) |
| Department head | 40 (12.7) | 16 (7.1) | 24 (26.7) |
| Resident/postgraduate | 36 (11.4) | 28 (12.4) | 8 (8.9) |
| Unit head | 29 (9.2) | 12 (5.3) | 17 (18.9) |
| Fellow | 2 (0.6) | 2 (0.9) | 0 |
| Management roles | |||
| PI of a competitively funded research project | 156 (49.4) | 97 (42.92) | 59 (65.5) |
| Leader of a research group | 59 (18.7) | 22 (9.7) | 37 (41.1) |
| Leader of a cooperative group | 29 (9.2) | 12 (5.3) | 17 (18.9) |
| Academic qualifications | |||
| Professorship | 63 (19.9) | 31 (13.7) | 31 (34.4) |
| Medical degree | 107 (33.9) | 65 (28.8) | 42 (46.7) |
| Doctoral thesisa | 90 (28.5) | 70 (31.0) | 20 (22.2) |
PI, principal investigator.
Completed/ongoing.
Professional environment
The large majority of respondents (95%) worked in a public hospital with only 5% in private institutions. Most respondents' institutions (n = 230; 72.8%) had between 5 and 20 attending medical oncologists, with 5.7% (18 respondents) working in large institutions (>30 attending medical oncologists). More than half of the 316 respondents (n = 187; 59.2%) had a permanent contract.
Two-thirds (66.1%) of respondents were attending medical oncologists (Table 1). The remainder mostly held senior positions including 12.7% who were heads of division and 9.2% who were unit heads. The distribution of roles differed between males and females, with the majority of women (74.3%) holding positions as attending medical oncologists versus 45.5% of males in the same position. By contrast, 12.4% of female respondents were division or unit heads, compared with 45.6% of males (P < 0.001). These gender differences were mirrored when respondents were questioned in terms of the overall numbers in their institution, reporting that within their institutions, 60.6% (2031/3349) of attending physicians and 63.7% (1167/1831) of fellows were women, whereas men accounted for 62.1% of the unit heads (231/372) and 78.8% of the division heads (249/316).
Professional satisfaction and achievements
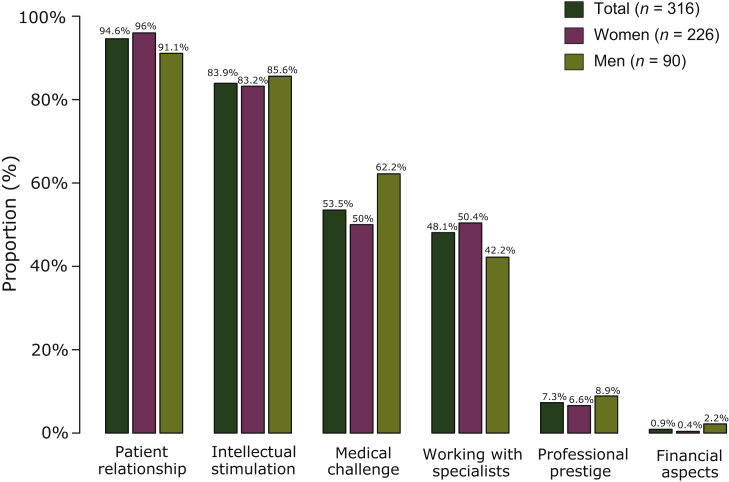
Three-quarters (n = 241; 76.3%) of the respondents reported being satisfied with their professional career, with a slightly but not statistically significant higher proportion of males (n = 73; 81.1%) compared with females (n = 168; 74.3%). When questioned over the aspects they most enjoyed about their jobs from a prespecified list, their relationship with patients was reported by almost all participants (n = 299; 94.6%), as was intellectual stimulus (n = 265; 83.9%; Figure 1). For most respondents (n = 206; 65.2%), patient care accounted for at least three-quarters of their time. Managing financial aspects was the least appreciated part of their job (<1% of respondents). The profiles of sources of potential satisfaction were similar between males and females (P = 0.34).
Figure 1.
Activities contributing to professional satisfaction (choice of 3 from a prespecified list).
In terms of professional projects (Table 1), approximately half of the respondents (49.4%) had led competitively funded research projects, with a lower proportion of females receiving funding (42.9%) than males (65.6%; P < 0.001). Among the 160 remaining respondents, 128 (80.0%) had never applied for a competitive grant, although 112 (70.0%) stated that they would like to lead projects, with equivalent proportions of men and women. A total of 59 respondents (18.7% of the population) had led a clinical research group during the last 5 years, corresponding to 41.1% (n = 37) of males compared with 9.7% (n = 22) of females. Of note, for 42 (71.2%) of them, this role had not been officially recognized. Most respondents (68.5%, 176/257) who had not led a research group had not actively applied for this position, with reasons cited including their patient care burden, lack of interest or of appropriate qualifications, or hospital infrastructure. Only 9.2% (n = 29) had led a cooperative group, and the majority of those who had not (269/287; 93.7%) had not actively applied to.
Overall, 33.9% (n = 107) of respondents had a medical degree, with a higher proportion of the male respondents (46.7%, 42/90) than female respondents (28.8%, 65/226; P < 0.01). Among respondents, 28.5% were working on or had completed a doctoral thesis, corresponding to 22.2% of males and 31.0% of females. In most cases (61.8%), respondents cited a lack of time as the main reason for not completing their thesis.
In terms of academic qualifications, 19.9% (63/316) of participants were university professors, most of whom (88.9%, 56/63) held associate professorships; among male respondents, 34.4% (31/90) were professors compared with 14.2% of female respondents (32/226). Less than half the participants (n = 138, 43.7%) were aware of the Spanish National Agency for Quality Assessment and Accreditation (ANECA), and among them, most (n = 113, 81.9%) had not requested accreditation required for any academic position at university. Seventy-seven respondents (24.4%) had spent time overseas after completing a residency, most (n = 61, 79.2%) of whom stayed for up to 12 months. This was more common among male respondents (31/90, 34.4%) than female respondents (46/226, 20.4%; P = 0.01).
Impact of parenthood and gender in the professional context
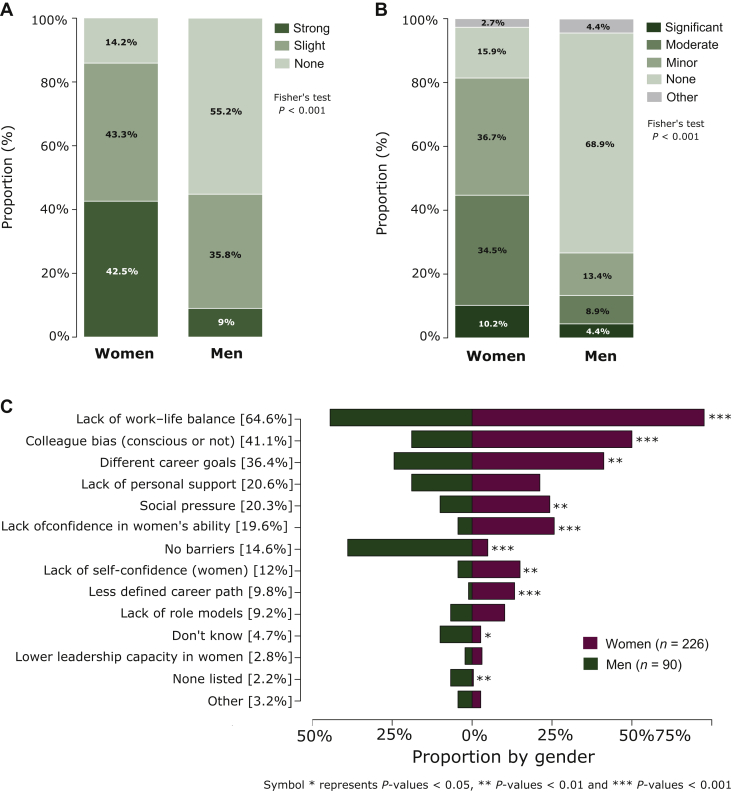
Of the 201 parents who responded to the question whether parenthood had negatively impacted their career, 40.7% (55/135) of women considered that parenthood had a strong negative impact on their professional career, compared with 9.0% (6/66) of men (Figure 2A). Conversely 11.1% (15/135) of women considered there was no negative impact compared with 54.5% (36/66) of men.
Figure 2.
Impact of parenthood and gender. (A) Negative impact of parenthood on respondents' career (N = 66 men; N = 135 women); (B) Impact of gender on respondents' career (N = 90 men; N = 226 women); (C) Three main barriers to gender equality, overall and by gender (N = 90 men; N = 226 women).
In terms of gender impact on their careers, 68.9% (62/90) of men considered it had no impact, compared with 15.9% (36/226) of women. Most women (71.2%, 161/226) reported a minor to moderate impact, compared with 22.2% (20/90) of men (Figure 2B). From a prespecified list of the main barriers to gender equality, lack of work–life balance was the most common reason selected (64.6%, 204/316), notably by women (72.6%, 164/226 versus 44.4%, 40/90; P < 0.001) than men (Figure 2C). Bias of peers and superiors (conscious or unconscious) was reported by 41.1% (130/316) of respondents, chosen by 50.0% (113/226) of women versus 18.9% (17/90) of men. Different career goals were considered a barrier for 36.4% (115/316) of respondents, selected by 41.2% (93/226) of women and 24.4% (22/90) of men. Men were more likely to consider there were no barriers (38.9%, 35/90) compared with women (4.9%, 11/226, P < 0.001). Lack of training was not considered as a contributing reason by any of the respondents. Among women, 41.6% (94/226) reported having suffered sexist or pejorative comments compared with 4.4% (4/90) of men. Inappropriate behavior in terms of gender or sexual orientation was also more frequently experienced by women (28.8%, 65/226) than by men (13.3%, 12/90).
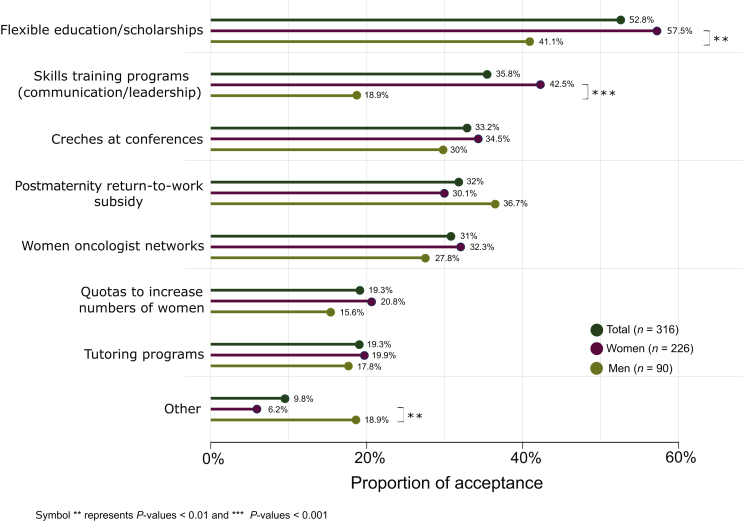
Participants were asked to select from a prespecified list approaches they consider would support professional development for female oncologists (Figure 3). Flexible educational programs and scholarships ranked most highly (52.9%, 167/316), along with skills training such as communication and leadership (35.8%; 113/316), childcare at conferences (33.2%, 101/316), and a financial incentive to return to work after maternity leave (32.0%, 101/316). The profile was similar for men and women, although significantly more women than men saw value in education programs (flexible education and scholarships 57.5% versus 41.1% of men; skills training 42.5% versus 18.9% of men, all P values < 0.01).
Figure 3.
Proposed approaches to addressing barriers to gender equality (men N = 90; women N = 226).
Discussion
This SEOM survey offers insight into gender disparity in the Spanish oncology setting. In our nationally representative population, younger females dominated (2.5:1 female:male ratio and 52.6% of female respondents were aged 40 or younger, compared with 28.9% of male respondents), and almost all respondents worked in public institutions with moderate to large oncology services. In addition, although we received 318 answers, this only represents nearly 15% of the total population and is thus a potential limitation of the study. The survey highlighted gender-based disparities in a number of domains, with leadership and decision-making positions dominated by men. Despite the fact that women represent the majority of the oncology workforce, significantly more male respondents held senior positions compared with females (45.6% versus 12.4%, respectively), and respondents confirmed this reflected the profiles of their institutions. Similar gender disparities were apparent in terms of professional achievements with four times as many men as women having led a research group over the last 5 years. In addition, obtaining competitive research funding, leading cooperative groups, or achieving a professorship were also notably more common among male respondents, although these leadership roles were infrequent in the overall population.
These trends in poor representation of women in leadership positions and academic achievements in this Spanish cohort echo reports from other oncology settings and the broader health care system. Recognition of this vertical segregation is increasing, with calls to break this so-called glass ceiling.12 Implicating women in leadership positions provides a diverse perspective in a male-dominated medical setting. Gender-diverse institutions are more likely to outperform those that are not,13 whereas lower mortality and hospital readmission rates have been reported with female physicians.14
Men were more likely than women to consider that their gender has not had any impact professionally (68.9% versus 15.9% respectively), whereas women primarily cited a mild to moderate impact. The high proportion of younger female participants may conceal the true extent of this impact, with it being too early in younger participants' careers for a true impact to have become apparent. Identifying perceived barriers to gender inequality from both a male and female perspective was revealing. While women were significantly more likely to cite several factors than men, notably a lack of work–life balance, peer bias, and different career goals, men were primarily of the opinion that there were no barriers to achieving gender equality. This is worth highlighting given the higher proportion of men in our cohort who were themselves occupying leadership positions. This lack of recognition of gender inequality by men and of the barriers women face has been reported in the scientific research setting.15
Perceived barriers reported in this Spanish female population, notably the challenges of balancing work and home and unconscious biases (such as men being perceived as natural leaders), echo those reported in other publications addressing gender inequality in a range of populations, including the ESMO survey, primarily reflecting a European perspective (accounting for 72% of respondents),2 as well as in the Middle East, North Africa, and India.10,16 Lack of mentorship, local gender bias, and lack of assertiveness and confidence were also cited as reasons, albeit less frequently, across different geographic regions. A recent global study reporting on barriers found they did not differ by age group.17 Other factors such as difficulties in attending international conferences or training programs, and lower salaries were more prominently cited in surveys of female oncologists in the Middle East, North Africa, and India.10,16
Among the two-thirds of participants who were parents, women were four times as likely as men to report that parenthood had a strong negative impact on their career (40.7% versus 9.0%, respectively). Addressing work–life balance in a social environment where women are commonly expected to put family first highlights a need for support in terms of shared responsibility for care of children and aging parents. In a study investigating women leaving surgical oncology, in addition to absence of interactions with women, another important factor cited was unavailability of or not having a valid reason for leave.18 Sexism and/or gender discrimination in the workplace were reported by up to 40% of our female respondents. Research has linked a harmful workplace environment and gender-based discrimination with adverse effects on women's occupational well-being and health,19 and the unfavorable impact of these behaviors appears greater in male-dominated work contexts.20
In terms of scientific research, the gender gap is a documented phenomenon that has had detrimental consequences, not only for women, but also for the quality of research, suggesting that bias against female medical oncologists might have consequences on research in oncology. In addition, some research findings apply only to men, establishing ‘biased knowledge’. Research into gender bias is less likely to be funded and is published in journals with a lower impact factors than research into equivalent social discrimination such as race.21
The existing merit-based system is biased against gender equality with the responsibilities of women outside of work not taken into consideration such as when accessing funding. The male-dominated professional and social systems perpetuate this situation, penalizing women in the pursuit of leadership positions, and contributing to maintaining the vicious circle. Changes at the level of systems, organizations, and policies have been advocated to address limitations imposed by these networks on opportunities for women to advance in their career path.17,22,23 Increasing transparency of the system is an essential part of addressing this. Steps need to be taken at the highest levels, with active encouragement and integration of diversity and inclusion into the missions of institutions and oncology academic societies, as highlighted by different organizations including SEOM and ESMO.24 Academic societies should be role models demonstrating leadership in advocating for gender equality. This can include statements highlighting the absence of evidence for gender-based differences in science ability, ensuring inclusive conferences in terms of speakers, expert panels, organizing committees, and attendees, and implementing codes of conduct to ensure equal financial support.22 Encouragingly, one study noted that faculties with at least one woman in a leadership position had a higher proportion of women faculty members, supporting a positive knock-on effect from implementing change to reverse the current trends.7 The reported presence of women in senior leadership positions or as invited speakers in national and international oncology societies and conferences is dismally low (ranging from approximately 10% to 25% depending on the position), with similar outcomes in Europe and South America, and slightly lower rates in Asia.25
At an institutional level, accountability and committed resources (financial and infrastructure) are needed, such as officially integrating dedicated time for gender-related training and activities into staff workload, hiring administrative support staff, and formal recognition of contributions.22 In addition to appointing more women to senior roles, other actions include seeking junior women for mentorship and sponsorship, encouraging them to proactively communicate their need for leadership, incentivizing mentorship, and implementing targeted recruitment to improve diversity.17 The current funding system undermines the role of women. It has been reported that in the attribution of health research funding, female principal investigators were evaluated less favorably than male investigators, and this was not due to differences in the quality of their proposals.26 The dominating position of men in obtaining research funding is reproduced in authorship of peer-reviewed publications, with a direct link established between the proportion of female-first authorship and of female faculty positions.27 Although the presence of women in key author positions in oncology publications has increased over time, efforts are required to significantly improve current representation.28
Education about gender inequalities is a critical part of the path forward, including integrating gender stereotypes awareness and the value of diversity in improving outcomes in science and medicine into curriculums at the undergraduate and graduate levels.22 Girod et al. reported a study implementing an educational program about gender bias and strategies for reducing it within a medical faculty, resulting in institutional change and promotion of women to higher ranks.29 For young oncologists, the turning point in their career is the end of residency. The significantly higher proportion of males in our cohort who spent time overseas after completing their residency (34.4% versus 20.4% of women) suggests that men can invest more time at an early stage of their training, increasing their access to senior professional opportunities, whereas for women motherhood is a likely obstacle for traveling.
In our cohort, the high level of professional satisfaction (over 75% of both men and women) was principally driven by patient relationships and intellectual stimulation. However, participants primarily dedicated their time to patient care, and therefore only limited time is available for the development of additional professional skills, such as leadership and management, or obtaining a PhD. Availability of educational programs and scholarships and skills training for communication and leadership were supported by a significantly higher proportion of women in our cohort as means of improving their career opportunities, while both men and women recommended childcare at conferences and financial postmaternity return-to-work incentives. These are all widely reclaimed means of addressing gender equality across geographical regions.2,10,16 In a study by Riaz et al., while women in the United States are clearly underrepresented in senior academic hematology and oncology positions (22% of full professors, 36% of associate professors, and 45% of assistant professors), after adjusting for clinical experience, academic productivity, and workplace ranking, the odds of obtaining professorship were not significantly different for female and male physicians.30 This supports the theory that for women to reach equal leadership representation, differences in length of clinical experience need to be addressed, and publication profiles and workplace visibility must be increased.
Associations dedicated to promoting the role of women in cancer care are an important foundation for the path to changing current attitudes and habits, as well as an excellent conduit for increasing awareness of career opportunities for women. Several global groups have been formed, such as the ESMO W4O Committee, the Women in Oncology Work Group in ASCO, and Women in Cancer Research (WICR) from AACR. National initiatives are being launched, such as the Women's Working Group for Oncology recently introduced by the SEOM,31 and the ASEICA (Asociación Española de Investigación Sobre el Cáncer/The Spanish Association for Cancer Research) Mujer/Women, developed by the Spanish Association for Cancer Research, which focuses on highlighting and fostering the work of female cancer researchers in Spain.32
There are a number of possible biases inherent to this study. Given the voluntary nature of the survey, it is likely that SEOM members who feel more strongly that gender disparity exists participated, potentially skewing the outcome, as suggested by the participating population being more heavily weighted toward younger females. Questions establishing numbers within an institution may have been affected if there was more than one respondent from the same institution. The study was not planned to analyze statistical associations between factors and responses, and robust analyses in a larger sample size may be of interest. The greater participation of younger female respondents likely contributed to the lower proportion of females in senior positions and with career achievements, whereas the older male respondents could be expected to be at a more advanced stage in their career. Nonetheless it is important that such voices are heard, and the survey remains valid, posing both objective and subjective questions.
Gender equality is not only just and fair, but implicit to the value of a new leadership paradigm increasing diversity of thought and of experience. It brings benefit not only to marginalized groups that need to gain representation at the table, but ultimately to the broader population who can also benefit from new approaches toward long-standing, intractable problems. Overall, in Spain, as elsewhere, there is a call to shift the mechanics of addressing gender disparity from individual behavior to comprehensive interventions including education, affirmative action, and accountability, and to take into account cultural specificities. The findings of this survey will be used to support the career development of women in Spain working in the oncology field, and to advocate for societal and cultural changes via public policies facilitating the sharing of care responsibilities, as previously recommended.33 Changing the status quo for female oncologists requires their increased visibility and recognition, and an active focus on appointing women to senior institutional and committee positions, and as conference speakers, along with increased access to funding and travel opportunities. Diversity and inclusion should be integrated into the missions of professional oncology societies and the undergraduate education courses. Changes to the social paradigm are an important part of the foundations of addressing gender inequality, and will support changes made to the professional infrastructure.
Acknowledgements
We thank Sarah MacKenzie, PhD, for writing assistance.
Funding
This study was funded by the Spanish Society of Medical Oncology (SEOM) (no grant number).
Disclosure
The authors declare no potential conflicts of interest.
Supplementary data
References
- 1.Boniol M., McIsaac M., Xu L. World Health Organization; Geneva, Switzerland: 2019. Gender Equity in the Health Workforce: Analysis of 104 Countries.https://apps.who.int/iris/bitstream/handle/10665/311314/WHO-HIS-HWF-Gender-WP1-2019.1-eng.pdf?sequence=1&isAllowed=y Working Paper 1 (WHO/HIS/HWF/Gender/WP1/2019.1) Available at: [Google Scholar]
- 2.Banerjee S., Dafni U., Allen T. Gender-related challenges facing oncologists: the results of the ESMO Women for Oncology Committee survey. ESMO Open. 2018;3(6):e000422. doi: 10.1136/esmoopen-2018-000422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rivera F., Andres R., Felip E. Medical oncology future plan of the Spanish Society of Medical Oncology: challenges and future needs of the Spanish oncologists. Clin Transl Oncol. 2017;19(4):508–518. doi: 10.1007/s12094-016-1595-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dijksterhuis W.P.M., Stroes C.I., Tan W.-L. From presentation to paper: gender disparities in oncological research. Int J Cancer. 2010;146:3011–3021. doi: 10.1002/ijc.32660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Melnikoff D.E., Valian V.V. Gender disparities in awards to neuroscience researchers. Arch Sci Psychol. 2019;7(1):4–11. doi: 10.1037/arc0000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharpe E.E., Moeschler S.M., O'Brien E.K. Representation of women among invited speakers for grand rounds. J Womens Health (Larchmt) 2020;29:1268–1272. doi: 10.1089/jwh.2019.8011. [DOI] [PubMed] [Google Scholar]
- 7.Chowdhary M., Chowdhary A., Royce T.J. Women's representation in leadership positions in academic medical oncology, radiation oncology, and surgical oncology programs. JAMA Netw Open. 2020;3(3):e200708. doi: 10.1001/jamanetworkopen.2020.0708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barry P.N., Miller K.H., Ziegler C. Factors affecting gender-based experiences for residents in radiation oncology. Int J Radiat Oncol Biol Phys. 2016;95(3):1009–1016. doi: 10.1016/j.ijrobp.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 9.Dieci M.V., Massari F., Giusti R. Gender influence on professional satisfaction and gender issue perception among young oncologists. A survey of the Young Oncologists Working Group of the Italian Association of Medical Oncology (AIOM) ESMO Open. 2018;3(6):e000389. doi: 10.1136/esmoopen-2018-000389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salem R., Haibe Y., Dagher C. Female oncologists in the Middle East and North Africa: progress towards gender equality. ESMO Open. 2019;4(3):e000487. doi: 10.1136/esmoopen-2019-000487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Temkin S.M., Rubinsak L., Benoit M.F. Take me to your leader: reporting structures and equity in academic gynecologic oncology. Gynecol Oncol. 2020;157:759–764. doi: 10.1016/j.ygyno.2020.03.031. [DOI] [PubMed] [Google Scholar]
- 12.Jagsi R., Tarbell N.J. Women in radiation oncology: time to break through the glass ceiling. J Am Coll Radiol. 2006;3(12):901–903. doi: 10.1016/j.jacr.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 13.Hunt V., Layton D., Prince S. Why Diversity Matters. 2015. https://www.mckinsey.com/business-functions/organization/our-insights/why-diversity-matters Available at:
- 14.Tsugawa Y., Jena A.B., Figueroa J.F. Comparison of hospital mortality and readmission rates for medicare patients treated by male vs female physicians. JAMA Intern Med. 2017;177(2):206–213. doi: 10.1001/jamainternmed.2016.7875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.García-González J., Forcén P., Jimenez-Sanchez M. Men and women differ in their perception of gender bias in research institutions. PLoS One. 2019;14(12):e0225763. doi: 10.1371/journal.pone.0225763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bajpai J., Mailankody S., Nair R. Gender climate in Indian oncology: national survey report. ESMO Open. 2020;5:e000671. doi: 10.1136/esmoopen-2020-000671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moyer C.A., Abedini N.C., Youngblood J. Advancing women leaders in global health: getting to solutions. Ann Glob Health. 2018;84(4):743–752. doi: 10.29024/aogh.2384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liang R., Dornan T., Nestel D. Why do women leave surgical training? A qualitative and feminist study. Lancet. 2019;393(10171):541–549. doi: 10.1016/S0140-6736(18)32612-6. [DOI] [PubMed] [Google Scholar]
- 19.Sojo V.E., Wood R.E., Genat A.E. Harmful workplace experiences and women's occupational well-being: a meta-analysis. Psychol Women Q. 2016;40(1):10–40. [Google Scholar]
- 20.O'Connell C.E., Korabik K. Sexual harassment: the relationship of personal vulnerability, work context, perpetrator status, and type of harassment to outcomes. J Vocat Behav. 2000;56(3):299–329. [Google Scholar]
- 21.Cislak A., Formanowicz M., Saguy T. Bias against research on gender bias. Scientometrics. 2018;115(1):189–200. doi: 10.1007/s11192-018-2667-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coe I.R., Wiley R., Bekker L.-G. Organisational best practices towards gender equality in science and medicine. Lancet. 2019;393(10171):587–593. doi: 10.1016/S0140-6736(18)33188-X. [DOI] [PubMed] [Google Scholar]
- 23.Knoll M.A., Glucksman E., Tarbell N., Jagsi R. Putting women on the escalator: how to address the ongoing leadership disparity in radiation oncology. Int J Radiat Oncol Biol Phys. 2019;103(1):5–7. doi: 10.1016/j.ijrobp.2018.08.011. [DOI] [PubMed] [Google Scholar]
- 24.Tabernero J. All change: closing the gender gap in oncology. ESMO Open. 2018;3(7):e000448. doi: 10.1136/esmoopen-2018-000448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hofstädter-Thalmann E., Dafni U., Allen T. Report on the status of women occupying leadership roles in oncology. ESMO Open. 2018;3(6):e000423. doi: 10.1136/esmoopen-2018-000423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Witteman H.O., Hendricks M., Straus S., Tannenbaum C. Are gender gaps due to evaluations of the applicant or the science? A natural experiment at a national funding agency. Lancet. 2019;393(10171):531–540. doi: 10.1016/S0140-6736(18)32611-4. [DOI] [PubMed] [Google Scholar]
- 27.O'Connor E.E., Chen P., Weston B. Gender trends in academic radiology publication in the United States revisited. Acad Radiol. 2018;25(8):1062–1069. doi: 10.1016/j.acra.2017.12.030. [DOI] [PubMed] [Google Scholar]
- 28.Salinaro J.R., Puechl A.M., Havrilesky L.J., Davidson B.A. Gender trends in gynecologic oncology authorship: implications for the critical evaluation of gender distribution in academic rank and leadership positions. Gynecol Oncol. 2018;151(3):542–546. doi: 10.1016/j.ygyno.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 29.Girod S., Fassiotto M., Grewal D. Reducing implicit gender leadership bias in academic medicine with an educational intervention. Acad Med. 2016;91(8):1143–1150. doi: 10.1097/ACM.0000000000001099. [DOI] [PubMed] [Google Scholar]
- 30.Riaz I.B., Siddiqi R., Zahid U. Gender differences in faculty rank and leadership positions among hematologists and oncologists in the United States. JCO Oncol Pract. 2020;16(6):e507–e516. doi: 10.1200/OP.19.00255. [DOI] [PubMed] [Google Scholar]
- 31.SEOM Nuevo Grupo de Trabajo de Mujeres por la Oncología [New Working Group of Women in Oncology] https://seom.org/es/noticias/106799-nuevo-grupo-de-trabajo-de-mujeres-por-la-oncologia Available at:
- 32.ASEICA [Asociación Española de Investigación Sobre el Cáncer] The Spanish Association for Cancer Research. https://www.aseica.es/aseica-mujer?lang=en Available at:
- 33.Artazcoz L., Borrell C., Benach J. Gender inequalities in health among workers: the relation with family demands. J Epidemiol Community Health. 2001;55(9):639–647. doi: 10.1136/jech.55.9.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.