Abstract
Men who inject drugs (MWID) and engage in transactional sex (i.e., receive money or drugs in exchange for sex) are vulnerable to HIV and violence. However, MWID who engage in transactional sex have been less studied than women. We examine factors associated with transactional sex among MWID in Los Angeles and San Francisco and whether transactional sex is associated with violent victimization. MWID were recruited using targeted sampling methods in 2011–2013 and completed surveys that covered demographics, drug use, HIV risk, violence, transactional sex, and other items. Multivariable logistic regression was used to (1) determine factors independently associated with transactional sex and (2) determine if transactional sex was independently associated with violence victimization in the last 6 months among MWID. An interaction term between income source and sexual identity was included in the transactional sex model. Of the 572 male PWID in the sample, 47 (8%) reported transactional sex in the past 6 months. Self-reported HIV infection was 7% for MWID who did not report transactional sex, 17% for MWID who reported transactional sex, and 24% for MWID who reported transactional sex and reported gay or bisexual identity. In multivariable analysis, transactional sex was positively associated with gay or bisexual identity (GB without illegal income adjusted odds ratio [AOR] = 5.16; 95% confidence interval [CI] = 1.86–14.27; GB with illegal income AOR = 13.55, CI = 4.57–40.13), coerced sex in the last 12 months (AOR = 11.66, CI = 1.94–70.12), and violent victimization in the last 12 months (AOR = 2.31, CI = 1.13–4.75). Transactional sex was negatively associated with heroin injection (last 30 days) (AOR = 0.37; 95% CI = 0.18–0.78). Transactional sex was independently associated with violent victimization in the last 12 months (AOR = 2.04; 95% CI = 1.00–4.14) while controlling for confounders. MWID who engaged in transactional sex are at elevated risk for HIV and multiple forms of violent victimization. Interventions focused on this at-risk subpopulation are urgently needed and should include access to substance use disorder treatment, victimization services, and harm reduction services across the HIV care continuum.
Keywords: Persons who inject drugs, Transactional sex, Violence
Introduction
Men who inject drugs (MWID) are at heightened risk for HIV infection via injection and sexual practices [1, 2]. One sexual behavior that could place MWID at increased risk for HIV is transactional sex, defined as exchanging sex for money or drugs [3–6]. Research examining transactional sex has mostly focused on women, including women who inject drug, and has largely neglected to examine MWID. Research focusing on transactional sex among men has often focused on men who have sex with men (MSM), with little or no focus on MWID engaged in transactional sex [7–9]. Therefore, we do not have a clear understanding about transactional sex experiences among MWID [10]. Studying MWID is important for identifying and understanding the specific associations and circumstances that MWID experience, which could differ from the broader MSM population.
One study examining transactional sex among MWID in New York City found gay and bisexual identity, cocaine use, methamphetamine use, and syringe sharing to be associated with transactional sex [11]. Another study among MWID in Vancouver found transactional sex to be associated with HIV-positive status, daily crack smoking, injecting cocaine, syringe sharing, and inconsistent condom use with casual sex partners [12]. These studies suggest that there may be an interplay between drug use behaviors, sexual behaviors, and sexual identity which should be explored further.
Further, research has demonstrated that MWID who have sex with men (MSM-MWID) are more likely to engage in behaviors that place them at risk for HIV and are more likely to be HIV positive, compared to non-MSM MWID [13, 14]. For example, two studies found that MSM-MWID had higher HIV prevalence than MWID who did not have sex with men [15, 16]. This could be because the concurrence of drug use and sex creates a “synergistic effect” in which HIV transmission risk is markedly increased [17]. Stimulants such as cocaine [18] or methamphetamines may create a greater synergy between sex and drugs for MWID [19]. It is also possible that sexual identity, sexual behaviors, and drug use could impact rates of transactional sex. For example, two studies in New York City found MWID who identified as gay or bisexual were more likely to engage in transactional sex [10, 11]. These studies suggest there is a need to better understand the intersections of drug use, sexual behaviors, and sexual identity.
Syndemic theory posits that biological diseases cluster across groups of people, usually among disadvantaged groups, in a synergistic way [20]. Important to syndemic theory is that biological diseases interact with social environments, which can amplify risk for disease [20, 21]. Research has demonstrated that substance abuse, violence, and HIV/AIDS (i.e., SAVA) are a syndemic [22–25]. Research focusing on MSM has shown an association between interpersonal violence (IPV) and alcohol and/or drug use, including injection drug use [26–28]. Further, there is an association between condomless anal sex (including with partners of unknown or discordant status) [29–33] and having multiple anal sex partners [30] with the SAVA syndemic. Other syndemic factors that have been identified, mainly among MSM, are child sexual abuse [29], depression [32], and sexual compulsivity [24].
Informed by syndemics theory, this study focused on associations between violence, sexual identity, and transactional sex among MWID. In a previous study, authors found that coerced sex among persons who inject drugs (PWID) was associated with transactional sex as well as gay and bisexual identity [34]. Similarly, a study in Vancouver found that 70% of MWID experienced physical violence at least once within a 5-year period [35]. Another study in Vancouver reported that 19% of MWID experienced sexual violence within their lifetime. Pointing towards a syndemic, research has shown that MWID who experience sexual violence are more likely to engage in transactional sex and other sexual and injection risk behaviors [36, 37]. Therefore, this study aimed to identify associations with transactional sex among MWID with a special focus on sexual identity and experiences with violence in order to test a possible syndemic.
Methods
Sampling and Recruitment
Targeted sampling and community outreach methods were used to recruit a cross-sectional sample of PWID in Los Angeles and San Francisco, California, between April 2011 and April 2013 [38–41]. Eligible participants were 18 years of age or older and self-reported injection drug use in the last 30 days, which was verified by visual inspection for signs of recent venipuncture or track marks [42]. Following an informed consent process prior to enrollment, trained interviewers administered a computer-assisted personal interview (Questionnaire Development System, NOVA Research, Bethesda, MD). Participants were compensated $20 for completing the survey. This analysis includes data from 572 MWID, of which 298 participants were recruited in Los Angeles and 274 in San Francisco. All study procedures were approved by the Institutional Review Boards at RTI International and the University of Southern California.
Study Measures
Transactional Sex
Transactional sex was measured through the following question: “In the last 6 months did you have any sex partners who paid you in cash or drugs for sex?”
Experiences with Violence
To assess recent experience of unwanted or coercive sex, participants were asked: “In the past 12 months, has somebody used physical force or threats to make you have vaginal, anal, or oral sex with them?” This item was coded as a dichotomous variable. Participants who answered affirmatively were then asked to identify their relationship to the perpetrator. Response options included various relationships such as steady partner, friend, family member, and stranger. Violent victimization was considered anyone that had experienced at least one incident of physical violence in the last 12 months. Types of physical violence measured were being shot; being shot at (not hit); threatened with a knife, gun, club, or weapon; punched, kicked, slapped, or physically hurt; been attacked by a stranger on the streets.
Drug Use
Injection drug use measures included age of first injection, injection frequency, frequency of injecting with others, years of injecting, types of drugs injected, injecting others or being injected by someone else, and injection sharing. We also included whether MWID had been in drug treatment within the last 6 months. Injection frequency was the sum of self-reported injection episodes with the following drugs: cocaine, crack cocaine, methamphetamine, heroin, speedball (admixture of cocaine and heroin), goofball (admixture of heroin and methamphetamine), prescription opiates, stimulants, sedatives, tranquilizers, methadone, and buprenorphine in the last 30 days. We converted injection frequency in last 30 days into a categorical variable with the following classifications: less than daily use (< 30 injections), once or twice a day (30 to 89 injections), and three or more times a day (≥ 90). Any injection of the drugs listed above was also considered. Chronic drug use was measured as using methamphetamines, heroin, and/or cocaine at least twelve times in the last 30 days, an approach that we and other researchers have classified as regular or chronic drug use [43] [44].
Criminal Justice
We measured experiences with the criminal justice system such as currently being on probation, currently being on parole, any arrest in the last 6 months, encounters with security guards in the last 6 months, and encounters with police in the last 6 months.
Health
Participants were asked to report whether they had received a mental health diagnosis, a positive HCV test, and a positive HIV test.
Demographic Characteristics
We collected participant information on demographic, socioeconomic, and health characteristics. Socio-demographic variables included in our analysis were age (< 30, 30, or older), gender, race/ethnicity (white, Latino, Black, Asian/Pacific Islander, Native American, and mixed race), sexual partner types (steady, casual, paid), and sexual identity (heterosexual, bisexual, gay). Socio-economic characteristics include monthly income (< $1401 vs. $1401 or more—the US federal poverty threshold for a 2-person household in 2016), homeless (yes or no), and education (high school graduate or equivalent). We also collected data on source of income by asking how participants received income in the last 6 months. We collected data on childhood sexual abuse by asking the following: “When you were under the age of 16, did you have sex with someone at least 5 years older than you?” Those answering “yes” were classified as having childhood sexual abuse.
Analysis
Descriptive statistics were examined for all variables of interest. Bivariable analyses were conducted using chi-square test for categorical variables and t-test for continuous variables. Variables significant at the p < 0.05 in bivariable analysis were tested in the multivariable models. We first developed a multivariable logistic model with transactional sex as the outcome variable. Since coerced sex and violent victimization were associated with transactional sex and given the logistic regression method, we were unable to determine directionality. Therefore, we developed an additional multivariable model with violent victimization as the outcome to provide additional insight into associations with violent victimization. Given the small number of MWID who reported coerced sex, we were unable to develop a multivariable model using coerced sex as the outcome. We tested for collinearity among bivariable variables using Pearson correlation. Correlated variables were removed from the final analysis based on strength of association with the dependent variable (i.e., the variable with the strongest association was retained). Multiple logistic regression models with transactional sex in the last 6 months as the dependent variable were constructed. Variables found to be significant at the p < 0.05 level were considered to be independently associated with transactional sex in the last 6 months and were retained in the final model, non-significant variables were dropped. The same methods were used for the violent victimization model. We explored syndemics in two ways. The first was by creating a count variable for syndemic conditions [29, 45], including HIV, mental health, violent victimization, and chronic drug use. The second way we explored syndemics was by testing a series of interaction terms to identify the multiplicative nature of syndemics (something a count variable cannot do) [46, 47]. Specifically, interactions with gay or bisexual identity and illegal income and gay or bisexual identity and family income were significant and retained. We looked at these variables to examine the potential magnified disadvantages due to sexuality and income and how this might create constrained circumstances that encourage transactional sex. The count syndemic variable did not yield significant results so we only report the interaction results in our models.
Results
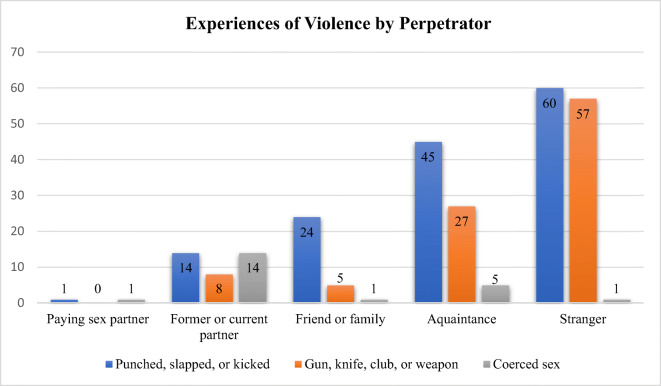
Most MWID reported heterosexual identity (87%) and reported having a high school diploma or higher education level (66%) (Table 1). In terms of race/ethnicity, 34% of MWID were White, 26% Latinx, 31% Black, 2% Native American, 7% mixed race or other, and less than 1% (n = 3) were Asian or Pacific Islander. Over half of MWID reported current homelessness (62%) and living in poverty with a monthly income less than $1400 (78%). MWID ages ranged from 10% aged 18–29 years, 11% aged 30–39 years, 27% aged 40–49, to 53% aged 50 and older. Violent experiences in the last 12 months were reported by 42% of the sample. Figure 1 displays the types of violence experienced by perpetrator. We report the number of participants who encountered each experience.
Table 1.
Selected demographic and behavioral characteristics (n = 572)
| Characteristics | N (%) |
|---|---|
| Demographics | |
| Study site | |
| Los Angeles | 298 (52%) |
| San Francisco | 274 (48%) |
| Sexual orientation | |
| Gay or bisexual | 77 (14%) |
| Heterosexual | 495 (87%) |
| Race/ethnicity | |
| White | 190 (34%) |
| Latino | 149 (26%) |
| Black | 176 (31%) |
| Native American | 12 (2%) |
| Asian/Pacific Islander | 3 (<1%) |
| Mixed race/other | 38 (7%) |
| Education | |
| Less than high school diploma | 196 (34%) |
| High school diploma or more | 376 (66%) |
| Age | |
| 18–29 | 55 (10%) |
| 30–39 | 60 (11%) |
| 40–49 | 153 (27%) |
| 50 and older | 304 (53%) |
| Income, last 30 days | |
| Less than $1400 | 448 (78%) |
| $1400 or more | 124 (22%) |
| Income sources, last 6 months | |
| Job | 81 (14%) |
| Unemployment benefit | 18 (3%) |
| VA benefits | 11 (2%) |
| Welfare benefits | 184 (32%) |
| SSI or SSDI benefit | 205 (36%) |
| Spouse or partner you live with | 36 (6%) |
| Other family or friends | 81 (14%) |
| Recycling | 149 (26%) |
| Panhandling | 144 (25%) |
| Illegal or possibly illegal income | 209 (37%) |
| Homeless (current) | 353 (62%) |
| Sexual behaviors | |
| Any sex partner in the last 6 months | |
| Any steady sex partner (last 6 months) | 273 (48%) |
| Consistent condom use—100% | 41 (15%) |
| Sex partner is a person who injects drugs | 134 (23%) |
| Any casual sex partner (last 6 months) | 193 (34%) |
| Consistent condom use – 100% | (41%) |
| Sex partner is a person who injects drugs | 118 (21%) |
| Any paying sex partners (last 6 months) | 47 (8%) |
| Consistent condom use – 100% | 21 (45%) |
| Sex partner is a person who injects drugs | 37 (7%) |
| Violence | |
| Childhood sexual assault | 59 (10%) |
| Coerced sex | 9 (2%) |
| Violent victimization (last 12 months) | 239 (42%) |
| Witnessed violence (last 12 months) | 134 (24%) |
| Criminal justice | |
| Currently on probation | 128 (23%) |
| Currently on parole | 59 (10%) |
| Any arrest (last 6 months) | 160 (28%) |
| Drug and alcohol | |
| Drug treatment (last 30 days) | 207 (36%) |
| Age at first injection | |
| 17 years or less | 224 (40%) |
| 18–29 years | 267 (47%) |
| 30 or older | 81 (14%) |
| Injection frequency (last 30 days) | |
| Less than 30 | 283 (50%) |
| 30–89 | 153 (27%) |
| 90 or more | 136 (24%) |
| Injected speedball (last 30 days) | 89 (16%) |
| Injected goofball (last 30 days) | 70 (12%) |
| Injected crack cocaine (last 30 days) | 51 (9%) |
| Injected powder cocaine (last 30 days) | 57 (10%) |
| Injected methamphetamine (last 30 days) | 222 (39%) |
| Injected heroin (last 30 days) | 441 (77%) |
| Injected prescription opioid (last 30 days) | 71 (12%) |
| Overdosed (last 6 months) | 41 (7%) |
| Witnessed an overdose (last 6 months) | 131 (23%) |
| Health | |
| Mental health diagnosis (ever) | 243 (43%) |
| Received HIV-positive test result (ever) | 45 (8%) |
| Received HCV-positive test result (ever) | 182 (68%) |
Fig. 1.
Experiences of violence by perpetrator
Overall, 8% of MWID reported transactional sex in the last 6 months, 42% reported violent victimization in the last 12 months, and 2% reported coerced sex in the last 12 months. MWID who engaged in transactional sex reported an average of 4 male sexual partners (median = 0) and 7 female sexual partners (median = 2) in the past 6 months. Self-reported HIV infection was 7% for MWID with no transactional sex (Table 2), 17% for MWID who engage in transactional sex, and 24% for MWID who identified as gay or bisexual and engage in transactional sex (data not shown). A wide range of demographic, health, criminal justice, violence, and drug use measures were different by transactional sex involvement.
Table 2.
Bivariable factors associated with transactional sex among men who inject drugs (n = 572)
| Characteristic | Transactional sex (n = 47) | No transactional sex (n = 525) | p |
|---|---|---|---|
| Socio-demographics | |||
| Sexual identity | 0.000 | ||
| Gay or bisexual | 25 (53%) | 52 (10%) | |
| Heterosexual | 22 (47%) | 473 (90%) | |
| Race/ethnicity | 0.030 | ||
| White | 20 (43%) | 170 (33%) | |
| Latino | 7 (15%) | 142 (27%) | |
| Black | 11 (23%) | 165 (32%) | |
| Native American | 1 (2%) | 11 (2%) | |
| Asian/Pacific Islander | 1 (2%) | 2 (<1%) | |
| Mixed race | 7 (15%) | 31 (6%) | |
| Age | 0.021 | ||
| <3 0 | 9 (19%) | 46 (9%) | |
| 30 and older | 38 (81%) | 479 (91%) | |
| Mental health diagnosis (last 6 months) | 0.001 | ||
| Yes | 31 (66%) | 212 (41%) | |
| No | 16 (34%) | 310 (59%) | |
| Criminal justice | |||
| Contact with police (6 months) | 0.033 | ||
| Yes | 32 (68%) | 272 (52%) | |
| No | 15 (32%) | 252 (48%) | |
| Violence | |||
| Coerced sex (12 months) | 0.000 | ||
| Yes | 7 (15%) | 2 (<1%) | |
| No | 40 (85%) | 521 (>99%) | |
| Violent victimization (12 months) | |||
| Yes | 32 (68%) | 207 (40%) | 0.000 |
| No | 15 (32%) | 313 (60%) | |
| Parental drug and alcohol | |||
| Parent had alcohol problem | 0.004 | ||
| Yes | 35 (75%) | 275 (52%) | |
| No | 12 (26%) | 250 (48%) | |
| Parent had an illegal drug problem | 0.001 | ||
| Yes | 21 (45%) | 116 (22%) | |
| No | 26 (55%) | 409 (78%) | |
| Injectional drug use behavior | |||
| Years of injection | 0.006 | ||
| <1 0 years | 14 (30%) | 67 (13%) | |
| 10–19 years | 5 (11%) | 81 (15%) | |
| 20 years or more | 28 (60%) | 377 (72%) | |
| Frequency of injecting with others | 0.029 | ||
| Never | 105 (20%) | 6 (13%) | |
| Less than 25% of the time | 156 (30%) | 18 (38%) | |
| 25%–74% of the time | 104 (20%) | 3 (6%) | |
| 75%–99% of the time | 78 (15%) | 13 (28%) | |
| Always | 81 (16%) | 7 (15%) | |
| Peer to peer injection (30 days) | 0.017 | ||
| Neither | 19 (40%) | 319 (61%) | |
| Injection provider | 11 (23%) | 97 (19%) | |
| Both | 9 (19%) | 42 (8%) | |
| Injection recipient | 8 (17%) | 67 (13%) | |
| HIV | |||
| Positive HIV test (ever) | 0.019 | ||
| Yes | 8 (17%) | 37 (7%) | |
| No | 38 (83%) | 462 (93%) | |
In multivariable analysis (Table 3), we report the results of an interaction term between sexual identity and illegal source of income. MWID who identified as gay or bisexual (GB) had higher odds of transactional sex (GB without illegal income adjusted odds ratio [AOR] = 5.16; 95% confidence interval [CI] = 1.86–14.27; GB with illegal income AOR = 13.55, CI = 4.57–40.13), as did MWID who experienced coerced sex (AOR = 11.66, CI = 1.94–70.12) and MWID who experienced violent victimization (AOR = 2.31, CI = 1.13–4.75). We also found that MWID who injected heroin in the last 30 days had lower odds of transactional sex (AOR = 0.37; 95% CI = 0.18–0.78) as compared to MWID who did not inject heroin.
Table 3.
Multivariable analysis of factors associated with transactional sex (n = 567)
| OR | CI | aOR | CI | |
|---|---|---|---|---|
| Sexual identity/income | ||||
| Heterosexual/no illegal income | Ref | Ref | ||
| Heterosexual/illegal income | 2.16 | 0.91–5.10 | 1.84 | 0.76–4.48 |
| Gay or bisexual/no illegal income | 7.80*** | 3.05–19.91 | 5.16** | 1.86–14.27 |
| Gay or bisexual/illegal income | 35.08*** | 13.25–92.89 | 13.55*** | 4.57–40.13 |
| Coerced sex (last 12 months) | 45.58*** | 9.17–226.71 | 11.66** | 1.94–70.12 |
| Violent victimization (last 12 months) | 3.23*** | 1.70–6.11 | 2.31* | 1.13–4.75 |
| Heroin injection (last 30 days) | 0.20*** | 0.11–0.37 | 0.37** | 0.18–0.78 |
Log likelihood: − 242. Cox & Snell R-squared: 0.134. Nagelkerke R-squared: 0.307. * indicates p < 0.05, ** indicates p < 0.01, *** indicates p < 0.001
In multivariable analysis examining violent victimization (Table 4), we found that transactional sex in the last 6 months (AOR = 2.04; 95% CI = 1.00–4.14), contact with police in the last 6 months (AOR = 2.34; 95% CI = 1.60–3.41), having an illegal source of income in the last 6 months (AOR = 1.67; 95% CI = 1.14–2.45), relying on a spouse or partner for income in the last 6 months (AOR = 2.70; 95% CI = 1.20–6.07), being homeless (AOR = 1.62; 95% CI = 1.10–2.40), ever having a mental health diagnoses (AOR = 1.74; 95% CI = 1.20–2.54), and chronic methamphetamine use (AOR = 2.02; 95% CI = 1.30–3.18) were positively associated with violent victimization. Residing in Los Angeles, compared to San Francisco, was negatively associated with violent victimization (AOR = 0.53; 95% CI = 0.36–0.77).
Table 4.
Multivariable analysis of factors associated with violent victimization (n = 564)
| OR | CI | aOR | CI | |
|---|---|---|---|---|
| Transactional sex (6 months) | 3.56*** | 1.86–6.82 | 2.04* | 1.00–4.14 |
| Contact with police (6 months) | 2.99*** | 2.11–4.25 | 2.34*** | 1.60–3.41 |
| Illegal source of income (6 months) | 2.39*** | 1.69–3.40 | 1.67** | 1.14–2.45 |
| Spouse/partner source of income (6 months) | 3.34** | 1.61–6.93 | 2.70* | 1.20–6.07 |
| Homeless (last 12 months) | 1.75** | 1.24–2.50 | 1.62* | 1.10–2.40 |
| Mental health diagnosis (ever) | 2.08*** | 1.48–2.93 | 1.74** | 1.20–2.54 |
| Chronic methamphetamine use | 2.89*** | 1.93–4.33 | 2.03** | 1.30–3.18 |
| Study site | ||||
| Los Angeles | 0.47*** | 0.33–0.66 | 0.53*** | 0.36–0.77 |
| San Francisco | Ref. | Ref. | ||
Log likelihood: − 658. Cox & Snell R-squared: 0.179. Nagelkerke R-squared: 0.240. * indicates p < 0.05, ** indicates p < 0.01, *** indicates p < 0.001
Discussion
Of the 47 MWID who reported transactional sex, 53% identified as gay or bisexual. Self-reported HIV infection was highest among the MWID who reported both transactional sex and gay/bisexual sexual identity. In multivariable analysis, we found that sexual identity was highly associated with transactional sex, indicating that MWID who identified as gay or bisexual had greater odds of engaging in transactional sex, compared to heterosexual MWID. This finding is important, as it supports the idea that sexual identity (not just behavior) can impact health [48, 49]. This may be because life circumstances and experiences associated with sexual identity can impact social and economic environments. For example, previous research has highlighted the particular vulnerability of gay and bisexual persons in relation to health [50], and specifically in relation to increased HIV risk [51]. One reason health disparities exist among sexual minority populations may be due to stress, often caused by stigma, that comes with having a minority identity [52]. MWID who identify as gay or bisexual may occupy two stigmatized identities (person using drugs and a sexual minority), which could compound stigmatizing experiences resulting in increased health disparities, including potential increased odds of transactional sex. For this reason, MWID may be at increased risk for negative health outcomes. Research has demonstrated that drug use stigma is prevalent and often more severe than other types of stigma, such as mental health [53] or obesity [54]. Furthermore, experiencing drug use stigma is associated with negative health outcomes [55] and negative healthcare experiences [56, 57]. MWID who are gay or bisexual could potentially be experiencing concurrent sexual minority stigma and drug use stigma, creating a particularly vulnerable environment which could increase rates of transactional sex. Among MWID who identified as gay or bisexual, those who reported illegal source of income had the highest odds (over 13 times increased odds) of transactional sex. This finding points to the intersections between sexual identity and employment/income opportunities. It may be that gay or bisexually identified men face employment discrimination [58] making it difficult to obtain income legally. Sexual identity discrimination coupled with discrimination associated with criminal justice involvement (28% of the sample had been arrested at least once in the last 6 months) [59] may create additional barriers for legal income among MWID. It is important that MWID have viable employment options that allow for a fair wage and healthy working conditions so they do not have to engage in illegal activities (if they do not wish to) or rely on others for income, which place them at risk for violence [60]. If MWID had viable employment options, we may see less transactional sex and fewer experiences with violence.
We also found that both sexual and physical violence (sexual coercion and violent victimization) were significantly and positively associated with transactional sex. MWID who engage in transactional sex might be experiencing elevated rates of violence due to larger systems and structural conditions that create circumstances of oppression. Above, we discussed the role of drug use and sexual minority stigma in increasing health disparities and employment options, which likely applies here as well. In addition, stigma may be more severe for some MWID who engage in transactional sex. For instance, research has shown that bisexual MSM may experience greater stigma because they do not want to disclose their MSM behavior [61, 62]. Experiencing stigma (or anticipating stigma) may contribute to social isolation among MWID, which might heighten experiences with violence. Further, MWID who sell sex may be isolated from larger gay communities, and as a result they may not have access to social supports offered within those communities [63]. In addition, policies (often constructed in stigmatizing ways towards PWID [64]) can impact individual circumstances. For example, the criminalization of drug use [62] could contribute to the choice to engage in transactional sex because transactional sex can generate income. Additionally, the criminalization of drug use along with the criminalization of sex work [65] could be contributing to situations that foster violence when engaging in transactional sex.
In relation to drug use, we found MWID who reported heroin use in the last 30 days had decreased odds of transactional sex. Past research has shown a positive association with sexual risk behaviors and stimulants such as cocaine [66] and amphetamines [67], but not heroin. Given the biological effects of heroin, this finding is not surprising.
Engaging in transactional sex under constrained conditions may place MWID at risk for experiencing violence [36]. In order to gain a better understanding of correlates with violence, and how violence might be associated with transactional sex, we developed an additional model with violence as the outcome. In this model, we found that transactional sex was positively associated with violent victimization. We also found that experiences with police, having an illegal source of income, and relying on a spouse or partner for income were positively associated with violence. It is possible that engaging in illegal activities heightens risk for violence [68]. In regard to relying on a spouse or partner for income, this may suggest MWID who rely on partners for income are experiencing intimate partner violence (IPV). Importantly, high rates of violence have been found among MSM populations [69] and IPV and depression have been associated [70]. In addition, we found that homelessness was associated with violence. Homelessness likely creates structures that allow for greater violence as people do not have the ability to take shelter in their home.
Finally, we found that ever being diagnosed with a mental health condition and chronic methamphetamine use was associated with violent victimization. Research among women sex workers has found that methamphetamine use was associated with mental health and experiences with violence and suggests that there is a bi-directional relationship between the three [71]. Importantly, methamphetamine use has been associated with increased odds of transactional sex [9], HIV risk, and incidence [72–75]. The findings from this study suggest that methamphetamine using MWID, especially those who engage in transactional sex, may be a key population to target HIV prevention efforts at, including pre-exposure prophylaxis (PrEP) [76–78] and increased access to syringe service programs [79, 80]. MWID, specifically men who inject amphetamines, may also benefit from increased efforts towards engagement throughout the HIV care continuum, particularly focusing on treatment as prevention, since HIV-positive stimulant using men who have sex with men have greater odds of a detectable viral load. [81]
Although there is no medication-assisted therapy for methamphetamine use, behavioral interventions have been effective. For example, contingency management, a behavioral therapy that immediately provides an incentive (usually monetary) for not using amphetamines, has been effective in reducing amphetamine use and increasing health promoting behaviors among MSM [82, 83]. Furthermore, integrating positive affect strategies into community-based contingency management interventions may result in lower viral loads among MSM, suggesting the importance of positive messaging to help affirm oneself [84]. Finally, we suggest that interventions consider harm reduction approaches, since integrating harm reduction perspectives into cognitive behavioral interventions can reduce stimulant use and sexual risk behaviors [85].
The results of this study should be considered in light of potential limitations. Given our cross-sectional study design, causality cannot be inferred. Study data are derived from participant self-reports and are subject to recall and social desirability biases. However, the reliability and validity of items used in this study have been established in prior studies [86]. Data were collected in 2011 to 2013, and MWID transactional sex behaviors may have changed since then. However, given the increase of injection drug use nationally, along with increases in injecting-related infectious diseases [87–89], it is possible that MWID are experiencing additional risk than what was reported in 2011–2013. We were unable to describe transactional sex experiences in terms of the number of transactional sex partners (we only know the number of sex partners). We were also unable to describe the context that transactional sex occurred in nor were we able to identify if MWID sought clients on the street or online. Our survey did not collect data on sexual compulsivity and we therefore could not test sexual compulsivity in the models. The variable for coerced sex had small numbers, and as a result, we have wide confidence intervals for this variable, which could reduce the precision of the estimate effects. Given the small cell count for transactional sex, we were unable to test interactions with transactional sex in the violent victimization model (Table 4). Future research should address the contextual factors of sex work, as to fully understand experiences and risk.
Conclusion
The above findings demonstrate the intersections and complexities of transactional sex, violence, poverty, and drug use. We suggest that future research explore how multiple inequalities experienced by MWID may impact health, particularly research focused on how structural inequalities, such as drug policies, poverty, and racism, impact sexual risk behaviors [90].
Future research should also aim to understand the processes of transactional sex (e.g., when, how, and why MWID engage in transactional sex) and how social environments and processes of inequalities impact risk behaviors. Given the results of this study, MWID, especially men who inject amphetamines, may be an important group to target for HIV prevention services, such as pre-exposure prophylaxis (PrEP). Understanding which sub-groups of MWID are most at risk is critical for public health initiatives so that messaging and programs can be tailored to specific communities. Interventions targeting sub-populations of MWID should consider a multi-level approach that targets individual, community, and structural elements [91]. For example, biomedical interventions such as PrEP could be paired with structural interventions aimed at improving the overall quality of life for MWID (e.g., increasing employment opportunities and housing availability) and/or at mitigating stigma.
Transactional sex among MWID was strongly associated with gay and bisexual identity, illegal source of income, coerced sex, violent victimization, and heroin injection (negative association with heroin). Our data suggests that structural factors such as stigma, policies criminalizing drug use and transactional sex impact MWID’s choices to engage in transactional sex and their risk for experiencing violence. Multi-level interventions focused on MWID, which might combine individual, community, and structural elements, are urgently needed. Policies that harm MWID, such as the criminalization of drug use and sex work, should be restructured. In addition, providing easy access to substance use disorder treatment, victimization services, and harm reduction services for MWID would be helpful. Partnering with community organizations, such as syringe service programs (SSPs), may yield the best results as they are likely established non-stigmatizing spaces within communities [16].
Acknowledgements
This work was supported by NIDA grant #R01-DA027689 Program Official: Elizabeth Lambert. We thank the participants who took part in this study. The following research staff and volunteers also contributed to the study and are acknowledged here: Sonya Arreola, Vahak Bairamian, Philippe Bourgois, Soo Kin Byun, Jose Collazo, Jacob Curry, David-Preston Dent, Karina Dominguez-Gonzalez, Jahaira Fajardo, Richard Hamilton, Frank Levels, Luis Maldonado, Askia Muhammad, Brett Mendenhall, Stephanie Dyal-Pitts, and Michelle Thorson.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Neaigus A, Reilly KH, Jenness SM, Hagan H, Wendel T, Gelpi-Acosta C. Dual HIV risk: receptive syringe sharing and unprotected sex among HIV-negative injection drug users in New York City. AIDS Behav. 2013;17(7):2501–2509. doi: 10.1007/s10461-013-0496-y. [DOI] [PubMed] [Google Scholar]
- 2.Strathdee SA, Sherman SG. The role of sexual transmission of HIV infection among injection and non-injection drug users. J Urban Health. 2003;80(3):iii7–iii14. doi: 10.1093/jurban/jtg078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bacon O, Lum P, Hahn J, et al. Commercial sex work and risk of HIV infection among young drug-injecting men who have sex with men in San Francisco. Sex Transm Dis. 2006;33(4):228–234. doi: 10.1097/01.olq.0000204914.91923.ad. [DOI] [PubMed] [Google Scholar]
- 4.Kral AH, Bluthenthal RN, Lorvick J, Gee L, Bacchetti P, Edlin BR. Sexual transmission of HIV-1 among injection drug users in San Francisco, USA: risk-factor analysis. Lancet. 2001;357(9266):1397–1401. doi: 10.1016/S0140-6736(00)04562-1. [DOI] [PubMed] [Google Scholar]
- 5.Rondinelli AJ, Ouellet LJ, Strathdee SA, Latka MH, Hudson SM, Hagan H, Garfein RS. Young adult injection drug users in the United States continue to practice HIV risk behaviors. Drug Alcohol Depend. 2009;104(1–2):167–174. doi: 10.1016/j.drugalcdep.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 6.Javanbakht M, Ragsdale A, Shoptaw S, Gorbach PM. Transactional sex among men who have sex with men: differences by substance use and HIV status. J Urban Health. 2018:1–13. [DOI] [PMC free article] [PubMed]
- 7.Nerlander LM, Hess KL, Sionean C, et al. Exchange sex and HIV infection among men who have sex with men: 20 US cities. AIDS Behav. 2011;2016:1–12. doi: 10.1007/s10461-016-1450-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newman PA, Rhodes F, Weiss RE. Correlates of sex trading among drug-using men who have sex with men. Am J Public Health. 2004;94(11):1998–2003. doi: 10.2105/ajph.94.11.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walters SM, Braksmajer A, Coston B, et al. A ayndemic model of exchange sex among HIV-positive men who have sex with men. Arch Sex Behav. 2020;49:1965. doi: 10.1007/s10508-020-01628-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Walters SM, Rivera AV, Reilly KH, et al. Exchange sex among persons who inject drugs in the New York metropolitan area: the importance of local context, gender and sexual identity. AIDS Behav. 2018:1–15. [DOI] [PubMed]
- 11.Reilly KH, Neaigus A, Wendel T, Marshall DM, IV, Hagan H. Correlates of selling sex among male injection drug users in New York City. Drug Alcohol Depend. 2014;144:78–86. doi: 10.1016/j.drugalcdep.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 12.Kuyper LM, Lampinen TM, Li K, et al. Factors associated with sex trade involvement among male participants in a prospective study of injection drug users. Sex Transm Infect. 2004;80(6):531–535. doi: 10.1136/sti.2004.011106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maslow CB, Friedman SR, Perlis TE, Rockwell R, Des Jarlais DC. Changes in HIV seroprevalence and related behaviors among male injection drug users who do and do not have sex with men: New York City, 1990-1999. Am J Public Health. 2002;92(3):382–384. doi: 10.2105/ajph.92.3.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mirzazadeh A, Evans JL, Hahn JA, et al. Continued transmission of HIV among young adults who inject drugs in San Francisco: still room for improvement. AIDS Behav. 2017:1–12. [DOI] [PMC free article] [PubMed]
- 15.Kral AH. HIV prevalence and risk behaviors among men who have sex with men and inject drugs in San Francisco. J Urban Health. 2005;82(suppl_1):i43–i50. doi: 10.1093/jurban/jti023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bluthenthal RN, Kral AH, Gee L, Lorvick J, Moore L, Seal K, Edlin BR. Trends in HIV seroprevalence and risk among gay and bisexual men who inject drugs in San Francisco, 1988 to 2000. JAIDS J Acquir Immune Defic Syndr. 2001;28(3):264–269. doi: 10.1097/00042560-200111010-00010. [DOI] [PubMed] [Google Scholar]
- 17.Bull SS, Piper P, Rietmeijer C. Men who have sex with men and also inject drugs-profiles of risk related to the synergy of sex and drug injection behaviors. J Homosex. 2002;42(3):31–51. doi: 10.1300/J082v42n03_03. [DOI] [PubMed] [Google Scholar]
- 18.Scheim AI, Nosova E, Knight R, Hayashi K, Kerr T. HIV incidence among men who have sex with men and inject drugs in a Canadian setting. AIDS Behav. 2018;22(12):3957–3961. doi: 10.1007/s10461-018-2185-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lamb S, Kral AH, Dominguez-Gonzalez K, Wenger LD, Bluthenthal RN. Peer-to-peer injection: demographic, drug use, and injection-related risk factors. Int J Drug Policy. 2018;61:44–51. doi: 10.1016/j.drugpo.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singer M, Bulled N, Ostrach B, Mendenhall E. Syndemics and the biosocial conception of health. Lancet. 2017;389(10072):941–950. doi: 10.1016/S0140-6736(17)30003-X. [DOI] [PubMed] [Google Scholar]
- 21.Wright ER, Carnes N, Colón-Diaz M. Understanding the HIV/AIDS epidemic in the United States—the role of syndemics in shaping the public’s health. Understanding the HIV/AIDS Epidemic in the United States. Springer. 2016:1–17.
- 22.Singer M. A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inq Creat Soc. 1996;24(2):99–110. [Google Scholar]
- 23.Parsons JT, Millar BM, Moody RL, Starks TJ, Rendina HJ, Grov C. Syndemic conditions and HIV transmission risk behavior among HIV-negative gay and bisexual men in a US national sample. Health Psychol. 2017;36(7):695–703. doi: 10.1037/hea0000509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parsons JT, Grov C, Golub SA. Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: further evidence of a syndemic. Am J Public Health. 2012;102(1):156–162. doi: 10.2105/Ajph.2011.300284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parsons JT, Rendina HJ, Moody RL, Ventuneac A, Grov C. Syndemic production and sexual compulsivity/hypersexuality in highly sexually active gay and bisexual men: further evidence for a three group conceptualization. Arch Sex Behav. 2015;44(7):1903–1913. doi: 10.1007/s10508-015-0574-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buller AM, Devries KM, Howard LM, Bacchus LJ. Associations between intimate partner violence and health among men who have sex with men: a systematic review and meta-analysis. PLoS Med. 2014;11(3):e1001609. doi: 10.1371/journal.pmed.1001609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Houston E, McKirnan DJ. Intimate partner abuse among gay and bisexual men: Risk correlates and health outcomes. J Urban Health. 2007;84(5):681–690. doi: 10.1007/s11524-007-9188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stults CB, Javdani S, Greenbaum CA, Kapadia F, Halkitis PN. Intimate partner violence and substance use risk among young men who have sex with men: The P18 cohort study. Drug Alcohol Depend. 2015;154:54–62. doi: 10.1016/j.drugalcdep.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stall R, Mills TC, Williamson J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med. 2007;34(1):37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mustanski B, Phillips G, 2nd, Ryan DT, Swann G, Kuhns L, Garofalo R. Prospective effects of a syndemic on HIV and STI incidence and risk behaviors in a cohort of young men who have sex with men. AIDS Behav. 2017;21(3):845–857. doi: 10.1007/s10461-016-1607-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dyer TP, Shoptaw S, Guadamuz TE, et al. Application of syndemic theory to Black men who have sex with men in the multicenter AIDS Cohort Study. J Urban Health. 03/02 2012. 89(4):697–708. 10.1007/s11524-012-9674-x. [DOI] [PMC free article] [PubMed]
- 33.Biello KB, Colby D, Closson E, Mimiaga MJ. The syndemic condition of psychosocial problems and HIV risk among male sex workers in Ho Chi Minh City, Vietnam. AIDS Behav. 2014;18(7):1264–1271. doi: 10.1007/s10461-013-0632-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Williams JE, Dangerfield DT, Kral AH, Wenger LD, Bluthenthal RN. Correlates of sexual coercion among people who inject drugs (PWID) in Los Angeles and San Francisco, CA. J Urban Health. 2018:1–8. [DOI] [PMC free article] [PubMed]
- 35.Marshall BD, Fairbairn N, Li K, Wood E, Kerr T. Physical violence among a prospective cohort of injection drug users: a gender-focused approach. Drug Alcohol Depend. 2008;97(3):237–246. doi: 10.1016/j.drugalcdep.2008.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Richardson LA, Long C, DeBeck K, Nguyen P, Milloy MJS, Wood E, Kerr TH. Socioeconomic marginalisation in the structural production of vulnerability to violence among people who use illicit drugs. J Epidemiol Community Health. 2015;69(7):686–692. doi: 10.1136/jech-2014-205079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Braitstein P, Li K, Tyndall M, Spittal P, O'Shaughnessy MV, Schilder A, Johnston C, Hogg RS, Schechter MT. Sexual violence among a cohort of injection drug users. Soc Sci Med. 2003;57(3):561–569. doi: 10.1016/s0277-9536(02)00403-3. [DOI] [PubMed] [Google Scholar]
- 38.Watters JK, Biernacki P. Targeted sampling: options for the study of hidden populations. SocProbs. 1989;36:416. [Google Scholar]
- 39.Kral AH, Malekinejad M, Vaudrey J, Martinez AN, Lorvick J, McFarland W, Raymond HF. Comparing respondent-driven sampling and targeted sampling methods of recruiting injection drug users in San Francisco. J Urban Health. 2010;87(5):839–850. doi: 10.1007/s11524-010-9486-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bluthenthal RN, Watters JK. Multimethod research from targeted sampling to HIV risk environments. Qual Methods Drug Abuse HIV Res1995:212. [PubMed]
- 41.Lopez AM, Bourgois P, Wenger LD, Lorvick J, Martinez AN, Kral AH. Interdisciplinary mixed methods research with structurally vulnerable populations: case studies of injection drug users in San Francisco. Int J Drug Policy. 2013;24(2):101–109. doi: 10.1016/j.drugpo.2012.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cagle H, Fisher D, Senter T, Thurmond R, Kastar A. Classifying skin lesions of injection drug users: a method for corroborating disease risk. DHHS Pub. No.(SMA) 02. Rockville, MD; 2002.
- 43.Bluthenthal RN, Simpson K, Ceasar RC, Zhao J, Wenger L, Kral AH. Opioid withdrawal symptoms, frequency, and pain characteristics as correlates of health risk among people who inject drugs. Drug Alcohol Depend. 2020;107932 [DOI] [PMC free article] [PubMed]
- 44.Mateu-Gelabert P, Sandoval M, Meylakhs P, Wendel T, Friedman SR. Strategies to avoid opiate withdrawal: implications for HCV and HIV risks. Int J Drug Policy. 2010;21(3):179–185. doi: 10.1016/j.drugpo.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hirshfield S, Schrimshaw EW, Stall RD, Margolis AD, Downing MJ, Jr, Chiasson MA. Drug use, sexual risk, and syndemic production among men who have sex with men who engage in group sexual encounters. Am J Public Health. 2015;105(9):1849–1858. doi: 10.2105/AJPH.2014.302346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tsai AC, Venkataramani AS. Syndemics and health disparities: a methodological note. AIDS Behav. 2016;20(2):423–430. doi: 10.1007/s10461-015-1260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tsai AC, Burns BF. Syndemics of psychosocial problems and HIV risk: a systematic review of empirical tests of the disease interaction concept. Soc Sci Med. 2015;139:26–35. doi: 10.1016/j.socscimed.2015.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pathela P, Blank S, Sell RL, Schillinger JA. The importance of both sexual behavior and identity. Am J Public Health. 2006;96(5):765. doi: 10.2105/AJPH.2005.079186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wright ER, Perry BL. Sexual identity distress, social support, and the health of gay, lesbian, and bisexual youth. J Homosex. 2006;51(1):81–110. doi: 10.1300/J082v51n01_05. [DOI] [PubMed] [Google Scholar]
- 50.Mayer KH, Bradford JB, Makadon HJ, Stall R, Goldhammer H, Landers S. Sexual and gender minority health: what we know and what needs to be done. Am J Public Health. 2008;98(6):989–995. doi: 10.2105/AJPH.2007.127811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Safren SA, Blashill AJ, O'Cleirigh CM. Promoting the sexual health of MSM in the context of comorbid mental health problems. AIDS Behav. 2011;15(Suppl 1(1)):S30–S34. doi: 10.1007/s10461-011-9898-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hatzenbuehler ML, Bellatorre A, Lee Y, Finch BK, Muennig P, Fiscella K. Structural stigma and all-cause mortality in sexual minority populations. Soc Sci Med. 2014;103:33–41. doi: 10.1016/j.socscimed.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Corrigan PW, Kuwabara SA, O'Shaughnessy J. The public stigma of mental illness and drug addiction: findings from a stratified random sample. J Soc Work. 2009;9(2):139–147. [Google Scholar]
- 54.Phillips LA, Shaw A. Substance use more stigmatized than smoking and obesity. J Subst Abus. 2013;18(4):247–253. [Google Scholar]
- 55.Latkin CA, Gicquelais RE, Clyde C, Dayton L, Davey-Rothwell M, German D, Falade-Nwulia S, Saleem H, Fingerhood M, Tobin K. Stigma and drug use settings as correlates of self-reported, non-fatal overdose among people who use drugs in Baltimore, Maryland. International Journal of Drug Policy. 2019;68:86–92. doi: 10.1016/j.drugpo.2019.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Van Boekel LC, Brouwers EP, Van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1):23–35. doi: 10.1016/j.drugalcdep.2013.02.018. [DOI] [PubMed] [Google Scholar]
- 57.Biancarelli DL, Biello KB, Childs E, Drainoni M, Salhaney P, Edeza A, Mimiaga MJ, Saitz R, Bazzi AR. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend. 2019;198:80–86. doi: 10.1016/j.drugalcdep.2019.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tilcsik A. Pride and prejudice: employment discrimination against openly gay men in the United States. Am J Sociol. 2011;117(2):586–626. doi: 10.1086/661653. [DOI] [PubMed] [Google Scholar]
- 59.Smith SS, Broege NC. Searching for work with a criminal record. UC Berkeley: Institute for Research on Labor and Employment; 2012. [Google Scholar]
- 60.Richardson L, Sherman SG, Kerr T. Employment amongst people who use drugs: a new arena for research and intervention? Int J Drug Policy. 2012;23(1):3–5. doi: 10.1016/j.drugpo.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 61.Friedman MR, Dodge BM. The role of syndemic in explaining health disparities among bisexual men: a blueprint for a theoretically informed perspective. Understanding the HIV/AIDS Epidemic in the United States. Springer. 2016:71–98.
- 62.Taussig JA, Weinstein B, Burris S, Jones TS. Syringe laws and pharmacy regulations are structural constraints on HIV prevention in the US. Aids. 2000;14:S47–S51. doi: 10.1097/00002030-200006001-00007. [DOI] [PubMed] [Google Scholar]
- 63.Rhodes F, Deren S, Wood MM, Shedlin MG, Carlson RG, Lambert EY, Kochems LM, Stark MJ, Falck RS, Wright-Deaguero L, Weir B, Cottler L, Rourke KM, Trotter RT., II Understanding HIV risks of chronic drug-using men who have sex with men. AIDS Care. 1999;11(6):629–648. doi: 10.1080/09540129947550. [DOI] [PubMed] [Google Scholar]
- 64.Friedman SR. Sociopharmacology of drug use: initial thoughts. Int J Drug Policy. 2002;13(5):341–347. [Google Scholar]
- 65.Platt L, Grenfell P, Meiksin R, Elmes J, Sherman SG, Sanders T, Mwangi P, Crago AL. Associations between sex work laws and sex workers’ health: a systematic review and meta-analysis of quantitative and qualitative studies. PLoS Med. 2018;15(12):e1002680. doi: 10.1371/journal.pmed.1002680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lejuez CW, Bornovalova MA, Daughters SB, Curtin JJ. Differences in impulsivity and sexual risk behavior among inner-city crack/cocaine users and heroin users. Drug Alcohol Depend. 2005;77(2):169–175. doi: 10.1016/j.drugalcdep.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 67.Bull SS, Piper P, Rietmeijer C. Men who have sex with men and also inject drugs-profiles of risk related to the synergy of sex and drug injection behaviors. J Homosex. 2002;42(3):31–51. doi: 10.1300/J082v42n03_03. [DOI] [PubMed] [Google Scholar]
- 68.Debeck K, Shannon K, Wood E, Li K, Montaner J, Kerr T. Income generating activities of people who inject drugs. Drug Alcohol Depend. 2007;91(1):50–56. doi: 10.1016/j.drugalcdep.2007.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Braksmajer A, Walters SM, Crean HF, Stephenson R, McMahon JM. Pre-exposure prophylaxis use among men who have sex with men experiencing partner violence. AIDS Behav. 2020:1–8. [DOI] [PMC free article] [PubMed]
- 70.Reid RJ, Bonomi AE, Rivara FP, Anderson ML, Fishman PA, Carrell DS, Thompson RS. Intimate Partner Violence Among Men. Am J Prev Med. 2008;34(6):478–485. doi: 10.1016/j.amepre.2008.01.029. [DOI] [PubMed] [Google Scholar]
- 71.Argento E, Strathdee SA, Goldenberg S, Braschel M, Montaner J, Shannon K. Violence, trauma and living with HIV: longitudinal predictors of initiating crystal methamphetamine injection among sex workers. Drug Alcohol Depend. 2017;175:198–204. doi: 10.1016/j.drugalcdep.2017.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nerlander LM, Hoots BE, Bradley H, Broz D, Thorson A, Paz-Bailey G, NHBS Group HIV infection among MSM who inject methamphetamine in 8 US cities. Drug Alcohol Depend. 2018;190:216–223. doi: 10.1016/j.drugalcdep.2018.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hoenigl M, Chaillon A, Moore DJ, Morris SR, Smith DM, Little SJ. Clear Links between Starting Methamphetamine and Increasing Sexual Risk Behavior. J Aquir Immune Defic Syndr. 2015;1:551–557. doi: 10.1097/qai.0000000000000888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Halkitis PN, Parsons JT, Stirratt MJ. A double epidemic: crystal methamphetamine drug use in relation to HIV transmission. J Homosex. 2001;41(2):17–35. doi: 10.1300/J082v41n02_02. [DOI] [PubMed] [Google Scholar]
- 75.Buchacz K, McFarland W, Kellogg TA, Loeb L, Holmberg SD, Dilley J, Klausner JD. Amphetamine use is associated with increased HIV incidence among men who have sex with men in San Francisco. Aids. 2005;19(13):1423–1424. doi: 10.1097/01.aids.0000180794.27896.fb. [DOI] [PubMed] [Google Scholar]
- 76.Walters SM, Rivera AV, Starbuck L, Reilly KH, Boldon N, Anderson BJ, Braunstein S. Differences in awareness of pre-exposure prophylaxis and post-exposure prophylaxis among groups at-risk for HIV in New York state: New York City and Long Island, NY, 2011–2013. JAIDS J Acquir Immune Defic Syndr. 2017;75:S383–S391. doi: 10.1097/QAI.0000000000001415. [DOI] [PubMed] [Google Scholar]
- 77.Walters SM, Coston B, Neaigus A, Rivera AV, Starbuck L, Ramirez V, Reilly KH, Braunstein SL. The role of syringe exchange programs and sexual identity in awareness of pre-exposure prophylaxis (PrEP) for male persons who inject drugs. Int J Drug Policy. 2020;77:102671. doi: 10.1016/j.drugpo.2020.102671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Walters SM, Kral AH, Simpson KA, Wenger L, Bluthenthal RN. HIV pre-exposure prophylaxis prevention awareness, willingness, and perceived barriers among people who inject drugs in Los Angeles and San Francisco, CA. Subst Use Misuse. 2016;2020:1–11. doi: 10.1080/10826084.2020.1823419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Miller M, Lee J-Y, Fulcher J, et al. Getting to the point: methamphetamine injection is associated with biomarkers relevant to HIV pathogenesis. Drug Alcohol Depend. 2020;108133:108133. doi: 10.1016/j.drugalcdep.2020.108133. [DOI] [PubMed] [Google Scholar]
- 80.Muncan B, Walters SM, Ezell J, Ompad DC. “They look at us like junkies”: influences of drug use stigma on the healthcare engagement of people who inject drugs in New York City. Harm Reduct J. 2020;17(1) 10.1186/s12954-020-00399-8. [DOI] [PMC free article] [PubMed]
- 81.Teran RA, Carrico AW, Horvath KJ, et al. Stimulant use and study protocol completion: assessing the ability of men who have sex with men to collect dried blood spots for laboratory measurement of HIV viral load. Arch Sex Behav. 2019:1–15. [DOI] [PMC free article] [PubMed]
- 82.Reback CJ, Peck JA, Dierst-Davies R, Nuno M, Kamien JB, Amass L. Contingency management among homeless, out-of-treatment men who have sex with men. J Subst Abus Treat. 2010;39(3):255–263. doi: 10.1016/j.jsat.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Shoptaw S, Klausner JD, Reback CJ, et al. A public health response to the methamphetamine epidemic: the implementation of contingency management to treat methamphetamine dependence. BMC Public Health. 2006;6(1) 10.1186/1471-2458-6-214. [DOI] [PMC free article] [PubMed]
- 84.Carrico AW, Neilands TB, Dilworth SE, et al. Randomized controlled trial of a positive affect intervention to reduce HIV viral load among sexual minority men who use methamphetamine. J Int AIDS Soc. 2019;22(12) 10.1002/jia2.25436. [DOI] [PMC free article] [PubMed]
- 85.Carrico AW, Flentje A, Gruber VA, Woods WJ, Discepola MV, Dilworth SE, Neilands TB, Jain J, Siever MD. Community-based harm reduction substance abuse treatment with methamphetamine-using men who have sex with men. J Urban Health. 2014;91(3):555–567. doi: 10.1007/s11524-014-9870-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Dowling-Guyer S, Johnson ME, Fisher DG, Needle R, Watters J, Andersen M, Williams M, Kotranski L, Booth R, Rhodes F, Weatherby N, Estrada AL, Fleming D, Deren S, Tortu S. Reliability of drug users’ self-reported HIV risk behaviors and validity of self-reported recent drug use. Assessment. 1994;1(4):383–392. [Google Scholar]
- 87.Zibbell JE, Asher AK, Patel RC, Kupronis B, Iqbal K, Ward JW, Holtzman D. Increases in acute hepatitis C virus infection related to a growing opioid epidemic and associated injection drug use, United States, 2004 to 2014. Am J Public Health. 2018;108(2):175–181. doi: 10.2105/ajph.2017.304132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Peters PJ, Pontones P, Hoover KW, Patel MR, Galang RR, Shields J, Blosser SJ, Spiller MW, Combs B, Switzer WM, Conrad C, Gentry J, Khudyakov Y, Waterhouse D, Owen SM, Chapman E, Roseberry JC, McCants V, Weidle PJ, Broz D, Samandari T, Mermin J, Walthall J, Brooks JT, Duwve JM, Indiana HIV Outbreak Investigation Team HIV infection linked to injection use of oxymorphone in Indiana, 2014–2015. N Engl J Med. 2016;375(3):229–239. doi: 10.1056/NEJMoa1515195. [DOI] [PubMed] [Google Scholar]
- 89.Zibbell JE, Iqbal K, Patel RC, Suryaprasad A, Sanders KJ, Moore-Moravian L, Serrecchia J, Blankenship S, Ward JW, Holtzman D, Centers for Disease Control and Prevention (CDC) et al. Increases in hepatitis C virus infection related to injection drug use among persons aged≤ 30 years-Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64(17):453–458. [PMC free article] [PubMed] [Google Scholar]
- 90.Pouget ER, Bennett AS. A Syndemic Approach to Understanding HIV/AIDS Among People Who Inject Drugs in the US. In: Wright E., Carnes N. (eds) Understanding the HIV/AIDS Epidemic in the United States. Social Disparities in Health and Health Care. Springer, Cham. 10.1007/978-3-319-34004-3_8.
- 91.Baral SD, Friedman MR, Geibel S, Rebe K, Bozhinov B, Diouf D, Sabin K, Holland CE, Chan R, Cáceres CF. Male sex workers: practices, contexts, and vulnerabilities for HIV acquisition and transmission. Lancet. 2015;385(9964):260–273. doi: 10.1016/S0140-6736(14)60801-1. [DOI] [PMC free article] [PubMed] [Google Scholar]