Abstract
Intimate partner violence (IPV) remains a public health issue plaguing families and communities in the USA. Despite considerable research devoted to individual-level factors affecting IPV and a smaller body of ecological IPV research, few studies explore the interaction between individual-level protective factors and neighborhood- or community-level factors in predicting the incidents of IPV among women. Moreover, most IPV studies utilize a unidimensional approach for social capital, despite strong empirical and theoretical support for a multi-dimensional conceptualization. In a sample of heterosexual women in the USA (N = 1884), we found that concentrated disadvantage, social and physical disorder, and community violence together significantly predicted increased rates of IPV victimization. Concentrated disadvantage and higher scores on the social capital index independently predicted a lower probability of victimization. Moderating effects were found for social capital: the protective effects of social capital on the probability of IPV were attenuated for those reporting community violence compared with women who did not report it. These findings enhance the field’s understanding of the synergistic relationship between individual- and neighborhood-level factors, providing important implications for community-based IPV interventions.
Keywords: Intimate partner violence, Social capital, Community violence, Neighborhood
Physical or sexual violence or psychological harm between current or previous romantic partners constitutes intimate partner violence (IPV) [1], which is one common form of gender-based violence and a significant public health issue. In the USA, an estimated 15.8% of women experienced sexual violence by an intimate partner, and 22.3% of women experienced severe physical violence during their lifetimes [2]. Approximately 14% of all homicides in the USA are committed by intimate partners, with women accounting for 70% of IPV homicide victims [3]. Aside from death, there are serious physical health and psychosocial consequences associated with IPV among women, including poor health status [4], depression [5, 6], post-traumatic stress [3], low quality of life [7], and high utilization of health care services [3, 4]. Though IPV reaches all aspects of society, young people (i.e., ages 18 to 24) [3] and individuals experiencing food and housing insecurity at greater risk of IPV victimization [2].
One potential determinant of IPV victimization is neighborhood environment. A wide array of studies report a significant relation between neighborhood-level characteristics and IPV victimization [8, 9], including sexual IPV victimization [10] and intimate partner femicide [11] (i.e., lethal IPV). Specifically, IPV is associated with women living in neighborhoods with high unemployment and low income [12], communities with low levels of collective efficacy and social cohesion [13, 14], and increased levels of perceived violence and exposure to community violence [15, 16]. In addition to community violence, studies indicate that the level of IPV incidence within one’s community network is also related to the likelihood of IPV victimization among the residents [17]. Methodological advances, namely spatial analysis techniques, have shown how the unequal spatial distribution of immigrant concentration and concentrated disadvantage are linked with the unequal spatial distribution of IPV risk [18]. Most ecological IPV research does not, however, examine the synergy of these neighborhood-level factors with individual-level risk or protective factors [9].
Given the extensive evidence on the relationship between neighborhood and community characteristics and IPV among women, a need to explore protective factors that buffer the unhealthy effects of neighborhood factors on intimate relationships is warranted. Previous researchers have suggested that female victims of IPV may rely on their social networks for financial and emotional support when abuse occurs and that these supports may aid in the woman’s ability to exit the relationship or to locate necessary resources [6]. Additionally, social ties in one’s neighborhood may increase communication, which may help women cope with or disclose their victimization [19, 20], and encourage intervening behaviors between residents and the victim, perpetrator, community, or formal systems [21]. General support has been found for the influence of social ties on the likelihood and incidence of IPV among women [22–24], though it should be noted that simply having social ties or support is not always positive and can also be unhealthy or dangerous if friends are in violent relationships [23]. Moreover, one’s perception of their neighborhood characteristics and attitudes towards intimate partner violence has shown to influence an individual’s bystander intervention efforts, distinguishing it from general crime [25]. Overall, neighborhoods with a greater sense of cohesion and connection may reduce residents’ feelings of isolation and victims’ sense of powerlessness, suggesting that social support and social ties may mitigate the negative impacts of neighborhood environment among individuals. Despite considerable research devoted to individual-level social support and IPV, few studies explore the interaction between individual-level protective factors (e.g., social support) and neighborhood- or community-level factors (e.g., concentrated disadvantage and social/physical disorder) in predicting the incidents of IPV among women. For example, it is still unclear whether the effects of neighborhood disorder on IPV victimization are buffered by family and community support.
Theoretical Frameworks
Social Disorganization Theory
Social disorganization theory (SDT) asserts that concentrated disadvantage, residential instability, and ethnic heterogeneity threaten the social fabric of a neighborhood and can increase crime because residents are less likely to assert control via socially agreed-upon informal mechanisms. Re-articulation of this theory has included social processes that may influence the relation between neighborhood structural factors and crime, namely collective efficacy, social ties, and cultural norms [26]. Though SDT was originally applied to “street” or public crimes such as burglary, robbery, and stranger assaults, it has since been applied to “private” crimes, including IPV. Researchers have noted that concentrated disadvantage and perceptions of neighborhood physical and social conditions may exacerbate stress within households and among couples, intensifying the likelihood of violence between intimate partners [27, 28]. Furthermore, researchers have found an association between exposure to or witness of community violence and IPV in women [23]. Researchers hypothesize that community violence may hinder residents’ response to IPV because they either prioritize attention to community violence as a more urgent issue to address in the community, or simply come to tolerate violence in the neighborhood, referred to as “banalization” or “legitimization” of IPV [23, 29]. Additionally, neighborhood physical and social conditions, and community violence, may socially isolate community members [30, 31] and could ultimately diminish the opportunity for building and maintaining social capital that could otherwise provide outlets for stress relief, resources for help-seeking victims, and opportunities to leave violent relationships.
Social Capital Theory
Social capital has been conceptualized to have several dimensions, including social cohesion and cooperation among community members; access to resources through social networks; belonging to and participating in community organizations; and resources that community members could invoke for collective action [26, 32, 33]. Social capital is multi-dimensional and exists at multiple ecological levels. Study results generally indicate that it may serve as an important protective factor for victims of IPV; however, the majority of research on social capital and IPV has focused on individual dimensions of social support (e.g., support from friends and family), with a smaller body of research examining aspects of social capital at higher ecological dimensions (e.g., social ties, social cohesion, collective efficacy), which may indirectly serve as protective factors against IPV. Moreover, few studies have examined the synergistic effects of social capital on IPV despite strong empirical and theoretical support for this approach [34, 35]. Studying the protective effects of social capital as multi-dimensional on IPV victimization will enhance the field’s understanding of how social capital buffers against IPV at various levels of ecology and will expand the scope of malleable protective factors for individuals vulnerable to IPV.
Research Objectives
Previous studies examining social capital and IPV victimization have primarily utilized a single-dimension measure of social capital (e.g., social network or support), whereas other forms of social capital (e.g., collective efficacy) remain understudied, and these different dimensions of social capital are rarely modeled together [9]. Furthermore, few studies examine the synergistic effects evident between neighborhoods, community, and individual-level protective factors relative to IPV. We aim to examine the effects of neighborhood characteristics on IPV victimization among women and test the moderating role of social capital modeled at multiple ecological dimensions, using data from the Fragile Families and Child Wellbeing Study. Our research questions are as follows: (1) Does neighborhood environment predict women’s IPV victimization, when controlling for key demographics? (2) Does social capital moderate the relationship between neighborhood environment and women’s IPV victimization, when controlling for key demographics?
Method
The Fragile Families and Child Wellbeing Study employed a stratified random sampling design in three stages: 16 US cities with at least 200,000 people, hospitals within cities, and births within hospitals, resulting in nearly 5000 families who were followed over 15 years [36, 37]. Surveys consist of interviews with both mothers and fathers at the focal child’s birth (baseline) and again in five later waves (i.e., when the child was aged 1, 3, 5, 9, and 15). The parent interviews collect information on attitudes, relationships, parenting behavior, demographic characteristics, health (mental and physical), economic and employment status, neighborhood characteristics, and program participation. This study focuses on wave 3 (child age three, spanning years 2001 to 2003) due to the inclusion of key data collected through the parent/caregiver surveys and interviewer observations.
Sample
Of the original sample (N = 4898), a total of 4269 cases were retained for wave 3. For the purposes of this study, women in the sample were mothers who had complete data on all relevant variables (N = 1825) and reported on either (1) their intact relationship with the father of the child, (2) their past partnership with the father of the child (with whom they are not currently in a relationship), or (3) their current partner with someone other than the father of the child.
Measures
The variable properties and descriptive statistics are summarized in Table 1.
Table 1.
Variable properties and descriptive statistics (response frequencies for categorical variables; means and standard deviations otherwise) for the study sample
| Variable | Total items | Cronbach’s α or Cohen’s kappa | Scale/range | Frequency or M (SD) |
|---|---|---|---|---|
| Outcome variable | ||||
| Intimate partner violence | 7 | α = 0.60–.83 | 1 = “sometimes” or “often” for any item | 870 |
| 0 = “never” for all items | 958 | |||
| Independent variables | ||||
| Social and physical environment | 13 | α = 0.92 | 0–1.0 (higher number reflects more disorder) | 0.41 (0.16) |
| Community violence | 7 | α = 0.71 | 1 = endorsement of at least one item | 790 |
| 0 = never witnessed or directly victimized | 1038 | |||
| Concentrated disadvantage | 5 | α = 0.75 | − 1.43–5.37 (higher number reflects more disadvantage) | 0.09 (1.01) |
| Moderator variable | ||||
| Social capital index | 20 | 0–1.0 (higher number reflects greater social capital) | 0.50 (0.19) | |
| Social support | 4 | k = 0.74 | ||
| Social participation | 6 | k = 0.59 | ||
| Collective efficacy | 10 | α = 0.86 | ||
| Control variables | ||||
| Age | 1 | 16–50 | 27.93 (5.93) | |
| Race | 1 | 1 = Black | 963 | |
| 0 = White, Hispanic, and “Other” | 862 | |||
Outcome Variable
Intimate partner violence was measured using seven items drawn from Susan Lloyd’s scale of domestic violence [38] and the Conflict Tactics Scale [39]. The survey included three questions about how often the person experienced physical or sexual violence (e.g., [partner] slaps or kicks you, makes you have sex or do sexual things) and four items about non-physical violence (e.g., [partner] keeps you from seeing friends or family). Response options included “never,” “sometimes”, and “often.” There was no time frame prescribed (e.g., in the last month) for mothers reporting on intact partnerships; however, mothers now broken up and not in a new relationship reported on the last month of their relationship with the fathers of their children. Very low reporting of IPV resulted in a sparse distribution across the non-zero categories (skew = 3.07, kurtosis = 11.76), which is common to community samples. Thus, these items were dichotomized such that endorsement of “sometimes” or “often” for any item was coded 1 and “never” was coded as 0 following precedent in other studies utilizing this dataset [40]. Published reports of reliability and validity for Lloyd’s domestic violence scale [38] are scarce; however, the Conflict Tactics Scale has been well validated in the literature [39]. Cronbach’s alpha ranged from 0.60 to 0.83, with better reliability for single mothers reporting on the last month of their last relationship.
Independent Variables
Social and Physical Environment
Social and physical environments were measured based on study interviewers’ personal observations of the neighborhood environment and the primary caregiver/youth interactions at the time of the visit [41] using two well-validated scales [42, 43] totaling 13 items (α = 0.92). Five items, assessing the physical environment (for example, if there was “garbage, litter, broken glass in street, sidewalks, or yards” or “vacant/abandoned buildings”), used response options ranging from 1 (almost none) to 4 (yes almost everywhere). Eight items, assessing social environment (for example, how often “drunks,” or “drug dealers” hang around), used response options ranging from 1 (almost never) to 4 (frequently). Raw scores for each scale were summed and divided by 52 (the total number of items, 13, multiplied by the number of response options, 4), with higher numbers representing more social and physical disorder. Only those cases that had data on at least 10 of the 13 items were included (α = 0.915).
Community Violence
Community violence was measured using seven items probing for direct victimization (e.g., get beat up, attacked with a weapon) and witnessing (e.g., see someone killed) with response options ranging from 0 = zero to 4 = more than 10 times (α = 0.71). Given the sparse distribution across the non-zero categories (skew = 4.128, kurtosis = 28.448), this variable was dichotomized such that endorsement of at least one item resulted in a value of 1, else 0.
Concentrated Disadvantage
The concentrated disadvantage was conceptualized using social disorganization theory and precedent in previous literature [26]. Specifically, census tract data (by zip codes) regarding the percentages of the population who are unemployed (age 16+), on public assistance, below the poverty level, and female head of household with children under 18 years old, was reduced to a single factor score using a principle component analysis. Notably, %black, a common indicator historically included when measuring “concentrated disadvantage,” was not included because it can misattribute cause to race, rather than the racist policies and practices in the housing and labor markets that contribute to concentrated disadvantage. Higher scores indicate greater concentrated disadvantage (α = 0.75).
Moderator Variable: Social Capital Index
Aligning with social capital theory [35], the moderator was operationalized using three dimensions of social capital, creating a combined index of social capital representative of instrumental social support, social participation, and collective efficacy. Instrumental social support was assessed by four items (e.g., if the participant knew someone who could loan them money, provide a place to live, provide child care) with dichotomous (1 = yes, 0 = no) response options (r = .74). Social participation was assessed using six items asking if the respondent participated in community activities (e.g., group affiliated with church, working with children/youth) in the last 12 months (r = .59) with dichotomous response options (1 = yes, 0 = no). Collective efficacy was measured using a widely validated scale made up of 10 items (α = 0.84) [26] with five response options ranging from 1 = very likely to 5 = very unlikely. To mirror response options of the other two scales, response options were dichotomized with 1 = very or somewhat likely and 0 = very or somewhat unlikely or neutral. Finally, the responses (0/1) were summed across the 20 total items (from all three scales of social support, social participation, and collective efficacy) and divided by 20, with higher scores representing higher social capital.
Control Variables
Control variables included age (in years) and race. Due to the disproportionate rates of physical IPV against non-Hispanic black women [44], the majority of the sample identifying as non-Hispanic black, and to preserve degrees of freedom, race was modeled as 1 = non-Hispanic black and 0 = all other races (i.e., white, non-Hispanic, Hispanic, and other).
Analysis Plan
Due to the nested structure of the data, we examined the intra-class correlation (ICC) to assess the need to apply hierarchical linear modeling. Results indicated an ICC of nearly zero; thus, it was determined that the nested structure of the data had no effect on the data and analysis. Therefore, we fit a series of logistic regression models to predict IPV (1 = yes, 0 = no) from the 3 independent variables of concentrated disadvantage (CD), social/physical disorder (CPD), and community violence (CV), after controlling for age and race. To that model we then added the moderator, a combined index of social capital measures and its interaction with each of the independent variables to determine whether the effect of each independent variable on IPV were moderated by social capital. Model assumptions were tested and met; particularly, multicollinearity was tested and tolerance levels were well above the threshold of 0.1, indicating acceptable levels of correlation among predictor variables.
Results
After excluding cases with missing observations on any model variables, the analyses consisted of 1825 women. Descriptive statistics are presented in Table 1. The results for the models are presented below and in Table 2.
Table 2.
Parameter estimates, standard errors, Wald chi-square, and odds ratios for model 1 (control and independent variables) and model 2 (moderation model) (N = 1825).
| Parameter | Model 1 | Model 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| β | S.E. | Wald χ2 | Exp (β) | β | S.E. | Wald χ2 | Exp (β) | |
| Intercept | − 0.52 | 0.32 | 2.55 | 0.60 | − 0.45 | 0.47 | 0.93 | 0.64 |
| Age | 0.02 | 0.01 | 8.29** | 1.02 | 0.03 | 0.01 | 8.72** | 1.03 |
| Race (Black) | − 0.25 | 0.10 | 5.81* | 0.78 | − 0.26 | 0.10 | 6.11* | 0.77 |
| Concentrated disadvantage | − 0.14 | 0.06 | 5.53* | 0.87 | − 0.14 | 0.15 | 0.79 | 0.87 |
| Social/physical environment | 0.59 | 0.38 | 2.46 | 1.80 | 1.02 | 0.97 | 1.12 | 2.78 |
| Community violence (yes) | 0.19 | 0.11 | 3.03 | 1.21 | − 0.40 | 0.31 | 1.60 | 0.67 |
| Social capital index | − 0.86 | 0.28 | 9.82** | 0.42 | − 1.04 | 0.83 | 1.58 | 0.35 |
| Concentrated disadvantage * social capital index | − 0.02 | 0.31 | 0.004 | 0.98 | ||||
| Social/physical environment* social capital index | − 0.82 | 2.02 | 0.17 | 0.44 | ||||
| Community violence (yes) * social capital index | 1.19 | 0.60 | 3.98* | 3.30 | ||||
**p < 0.01 =
*p < 0.05 =
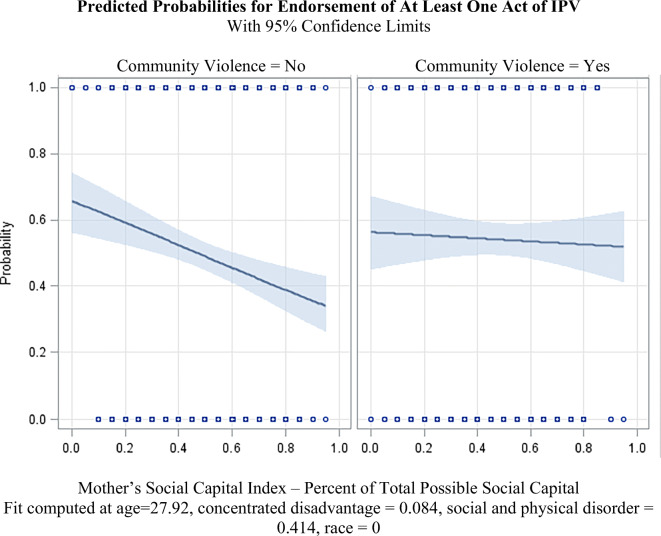
After controlling for age and race, the IVs of concentrated disadvantage, social/physical disorder, community violence, and social capital index together contributed significantly to predicting the likelihood of women reporting any IPV victimization (G2 = 22.25, df = 4, p = 0.0002). Statistically significant effects of two IVs were found, such that after controlling for age and race, higher concentrated disadvantage was associated with lower odds of victimization (β = − 0.14, exp.(− 0.14) = 0.87, 𝜒2 = 5.53, p = 0.019) and higher social capital index was associated with lower odds of reporting victimization (β = − 0.86, exp.(− 0.86) = 0.42, 𝜒2 = 9.82, p = 0.002). The social capital index variable was statistically significant as a moderator of the relationship between community violence and IPV for women (𝜒2 = 3.98, p = 0.046), but not of the other IVs. Specifically, the (generally inverse) relationship between social capital and the probability of reporting IPV was stronger for those not reporting community violence than for those reporting it. Figure 1 shows this at the means of the remaining variables: the negative relationship between social capital and the probability of reporting IPV is much more prominent for those reporting no community violence (and much weaker for those reporting it).
Fig. 1.
The relationship between social capital index and the probability of IPV, at the mean levels (and race-level “all others”) of the remaining variables, for women reporting no community violence (left) and those reporting community violence (right)
Discussion
Results indicated that more concentrated disadvantage was associated with lower rates of IPV. Though most studies report that higher levels of concentrated disadvantage are associated with higher levels of victimization [9, 45], some previous research has reported a non-significant relationship between concentrated disadvantage and IPV after controlling for other individual-level covariates when examining physical and non-physical forms of IPV [19], and, though non-significant, has reported decreased odds of victimization [46] in areas of concentrated disadvantage (similar to the current study). Frye and colleagues [10] reported no relationship between neighborhood income and sexual intimate partner violence, though noted the potential for negative confounding by way of unmeasured neighborhood-level factors. Few studies include other neighborhood characteristics such as social and physical disorder or community violence, so perhaps the effect associated with concentrated disadvantage differs here as a result of controlling for those variables [9]. The results also indicate that higher levels of social capital, measured using a multi-dimensional scale, had a buffering or protective effect on women’s likelihood of reporting IPV. This finding aligns with previous studies reporting protective effects of dimensions of social capital, such as social support [47], and adds to the limited body of research highlighting the protective effects of community-based dimensions of social capital [34].
This study also adds to the small body of studies examining the effects of community violence. In a previous study, Raghavan et al. [23] found that women who lived in areas characterized by social disorder were more likely to witness or experience community violence, which, in turn, put them at greater risk of IPV. Raghavan et al. [23] also found that women’s social networks put them at greater risk of IPV if they were made up of individuals who also experienced IPV. In the current study, we did not find a main effect for community violence like other studies examining this construct [23, 48]; however, we did find that social capital moderated the relationship between community violence and IPV. That is, a higher social capital index decreased the odds of victimization for women who did not report experiencing community violence, while women who did witness or experience community violence did not benefit as much from the protective effects of social capital. These findings suggest that community violence may be an important factor in women’s experience of IPV and that the buffering or protective effects stemming from one’s social capital were negated for women who witnessed or experienced community violence.
Strengths and Limitations
Study strengths and limitations must be considered to contextualize the findings. The overall design with a sample drawn from 16 US cities enhanced the generalizability of study findings, though study findings are limited to heterosexual women with children. Modeling social capital as multi-dimensional advances measurement by building upon theory and previous research [34]. The use of more objective sources such as census data and researcher/observer report for two environmental factors (i.e., concentrated disadvantage and social/physical disorder) strengthened measurement; however, the use of secondary data and survey instrumentation presents bias, such as with the constructs of community violence and social capital. Nevertheless, the use of a subjective measure for community violence may be more relevant to individual-level reporting of IPV compared with more “objective” measures of area-level crime rates [49, 50]. Also, IPV was dichotomized due to the low base reporting, which is common in community samples of criminal behavior. Though dichotomizing the outcome does not necessarily decrease the strength of associations between key explanatory variables [51], it may have obscured potentially important nuances in the types and frequency of IPV [52]. Finally, our analysis was strengthened by modeling all independent variables and their interactions simultaneously, controlling for all other variables when examining each effect.
Future Research
To further advance measurement, researchers should apply qualitative and quantitative methods to develop and validate the measurement of social capital resources at multiple ecological dimensions and levels that are relevant for IPV or relationship stress among women and men and within same- and opposite-sexual couples. Though men were not included in this study due to limitations in the variables collected with fathers, special attention to men’s perspective of social capital resources and potential gender differences related to IPV victimization is warranted. Finally, more studies need to investigate both risk and resources at multiple ecological dimensions and levels in order to tease apart the risk and protective factors of family violence.
Implications
Neighborhoods where women feel there are threats to one’s safety may impact women’s willingness or ability to build and benefit from a supportive social network. Businesses or non-profits may also be deterred from investing in the community, further detracting from opportunities to build social capital necessary for safety. Thus, IPV advocates may consider partnering with public health workers, activists, and organizers to engage residents of marginalized communities in improving physical conditions, such as through creating parks, urban farms, community gardens, or playgrounds, in order to foster a sense of safety and attachment to the neighborhood [53]. Public health campaigns designed to modify social and cultural norms that support violence should also be adopted to improve aspects of the social environment related to violent behavior (e.g., harmful use of alcohol, attitudes condoning violence) [54]. Systematic engagement of stakeholders, evidence-informed knowledge dissemination, and proactive media strategies are necessary for the success of these campaigns [55].
The intersection of community violence and IPV underscores the interconnection of different forms of violence, the increased risk of revictimization once exposed to violence, and the opportunity to effectively address violence using a cross-cutting approach [56]. It is recommended that emergency workers (e.g., police, emergency medical technician) responding to incidents of community violence deliver trauma-informed IPV education, screening, and referral to enhance the resources available to women who may have witnessed or experienced the violent incident, bolstering social capital and potentially preventing future relationship violence. Resources in any neighborhood, especially impoverished neighborhoods, are critical to identify and bolster to enhance the success of community engagement and mobilization. Women proved to be resourceful in building up their social capital that conferred benefits to their safety in relationships; however, barriers to this were evident for women who witnessed or experienced community violence. Social workers and public health workers should engage women in high-violence areas to identify barriers and facilitators to social safety nets and social networks [57]. Community agencies embedded in these neighborhoods should also focus on connecting community members to enhance a sense of trust and cohesion among residents.
Acknowledgements
This study received no grant funding.
Funding
This resaerch was conducted with no funding support.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Violence against women. New York, NY: SAGE Publications; 2013.
- 2.Breiding M, Chen J, Black M. Intimate partner violence in the United States - 2010. Boston, MA: NISVS; 2014.
- 3.Sugg N. Intimate partner violence: prevalence, health consequences, and intervention. Med Clin. 2015;99(3):629–649. doi: 10.1016/j.mcna.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 4.Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359(9314):1331–1336. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- 5.Devries KM, Mak JY, Bacchus LJ, Child JC, Falder G, Petzold M, Astbury J, Watts CH. Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. PLoS Med. 2013;10(5):e1001439. doi: 10.1371/journal.pmed.1001439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wright EM, Pinchevsky GM, Benson ML, Radatz DL. Intimate partner violence and subsequent depression: examining the roles of neighborhood supportive mechanisms. Am J Community Psychol. 2015;56(3):342–356. doi: 10.1007/s10464-015-9753-8. [DOI] [PubMed] [Google Scholar]
- 7.Wathen CN, MacGregor JCD, MacQuarrie BJ. Relationships among intimate partner violence, work, and health. J Interpers Violence. 2016;33(14):2268–2290. doi: 10.1177/0886260515624236. [DOI] [PubMed] [Google Scholar]
- 8.Beyer K, Wallis AB, Hamberger LK. Neighborhood environment and intimate partner violence: a systematic review. Trauma Violence Abuse. 2013;16(1):16–47. doi: 10.1177/1524838013515758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Voith LA. Understanding the relation between neighborhoods and intimate partner violence: an integrative review. Trauma Violence Abuse. 2017;20(3):385–397. doi: 10.1177/1524838017717744. [DOI] [PubMed] [Google Scholar]
- 10.Frye V, Blaney S, Cerdá M, Vlahov D, Galea S, Ompad DC. Neighborhood characteristics and sexual intimate partner violence against women among low-income, drug-involved New York City residents: results from the IMPACT studies. Violence Against Women. 2014;20(7):799–824. doi: 10.1177/1077801214543501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beyer KMM, Layde PM, Hamberger LK, Laud PW. Does neighborhood environment differentiate intimate partner femicides from other femicides? Violence Against Women. 2014;21(1):49–64. doi: 10.1177/1077801214564075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mears D, Carlson M, Holden G, Harris S. Reducing domestic violence revictimization: the effects of individual and contextual factors and type of legal intervention. J Interpers Violence. 2001;16(12):1260–1283. doi: 10.1177/088626001016012003. [DOI] [Google Scholar]
- 13.Dekeseredy WS, Schwartz MD, Alvi S, Tomaszewski EA. Perceived collective efficacy and women’s victimization in. Crime Justice. 2003;3(1):5–27. doi: 10.1177/1466802503003001001. [DOI] [Google Scholar]
- 14.Cunradi CB. Intimate partner violence among Hispanic men and women: the role of drinking, neighborhood disorder, and acculturation-related factors. Violence Vict. 2009;24(1):83–97. doi: 10.1891/0886-6708.24.1.83. [DOI] [PubMed] [Google Scholar]
- 15.Naved RT, Persson LÅ. Factors associated with physical spousal abuse of women during pregnancy in Bangladesh. Int Fam Plan Perspect. 2008;34(2):71–78. doi: 10.1363/3407108. [DOI] [PubMed] [Google Scholar]
- 16.Reed E, Silverman JG, Welles SL, Santana MC, Missmer SA, Raj A. Associations between perceptions and involvement in neighborhood violence and intimate partner violence perpetration among urban, African American Men. J Community Health. 2009;34(4):328–335. doi: 10.1007/s10900-009-9161-9. [DOI] [PubMed] [Google Scholar]
- 17.Uthman OA, Moradi T, Lawoko S. Are individual and community acceptance and witnessing of intimate partner violence related to its occurrence? Multilevel Structural Equation. PLoS One. 2011;6(12):e27738. doi: 10.1371/journal.pone.0027738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gracia E, López-Quílez A, Marco M, Lladosa S, Lila M. The spatial epidemiology of intimate partner violence: do neighborhoods matter? Am J Epidemiol. 2015;182(1):58–66. doi: 10.1093/aje/kwv016. [DOI] [PubMed] [Google Scholar]
- 19.Browning CR, Cagney KA. Neighborhood structural disadvantage, collective efficacy, and self-rated physical health in an urban setting. J Health Soc Behav. 2002;43(4):383–399. doi: 10.2307/3090233. [DOI] [PubMed] [Google Scholar]
- 20.Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, Smith PH. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. 2002;23(4):260–268. doi: 10.1016/S0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- 21.Frye V, Paul MM, Todd M-J, Lewis V, Cupid and Jane Coleman M, Salmon C, O’Campo P. Informal social control of intimate partner violence against women: results from a concept mapping study of urban neighborhoods. J Community Psychol. 2012;40(7):828–844. doi: 10.1002/jcop.21493. [DOI] [Google Scholar]
- 22.Raghavan C, Rajah V, Gentile K, Collado L, Kavanagh AM. Community violence, social support networks, ethnic group differences, and male perpetration of intimate partner violence. J Interpers Violence. 2009;24(10):1615–1632. doi: 10.1177/0886260509331489. [DOI] [PubMed] [Google Scholar]
- 23.Raghavan C, Mennerich A, Sexton E, James SE. Community violence and its direct, indirect, and mediating effects on intimate partner violence. Violence Against Women. 2006;12(12):1132–1149. doi: 10.1177/1077801206294115. [DOI] [PubMed] [Google Scholar]
- 24.Van Wyk JA, Benson ML, Fox GL, DeMaris A. Detangling individual-, partner-, and community-level correlates of partner violence. Crime Delinq. 2003;49(3):412–438. doi: 10.1177/0011128703049003004. [DOI] [Google Scholar]
- 25.Frye V. The informal social control of intimate partner violence against women: exploring personal attitudes and perceived neighborhood social cohesion. J Community Psychol. 2007;35(8):1001–1018. doi: 10.1002/jcop.20209. [DOI] [Google Scholar]
- 26.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science (80- ) 1997;277(5328):918 LP–918924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 27.Ross CE, Mirowsky J. Neighborhood disorder, subjective alienation, and distress. J Health Soc Behav. 2009;50(1):49–64. doi: 10.1177/002214650905000104. [DOI] [PubMed] [Google Scholar]
- 28.Wright EM, Benson ML. Clarifying the effects of neighborhood context on violence “behind closed doors.”. Justice Q. 2011;28(5):775–798. doi: 10.1080/07418825.2010.533687. [DOI] [Google Scholar]
- 29.Browning CR. The span of collective efficacy: extending social disorganization theory to partner violence. J Marriage Fam. 2002;64(4):833–850. doi: 10.1111/j.1741-3737.2002.00833.x. [DOI] [Google Scholar]
- 30.Anderson E. Code of the street: decency, violence, and the moral life of the inner city. New York, NY: W.W. Norton; 1999.
- 31.Tung EL, Johnson TA, O’Neal Y, Steenes AM, Caraballo G, Peek ME. Experiences of community violence among adults with chronic conditions: qualitative findings from Chicago. J Gen Intern Med. 2018;33(11):1913–1920. doi: 10.1007/s11606-018-4607-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bourdieu P. The forms of capital. In: Handbook of theory and research for the sociology of education. Westport, CT: Greenwood; 1986. p. 241–58.
- 33.Coleman JS. Social capital in the creation of human capital. Am J Sociol. 1988;94:S95–S120. doi: 10.1086/228943. [DOI] [Google Scholar]
- 34.Kirst M, Lazgare LP, Zhang YJ, O’Campo P. The effects of social capital and neighborhood characteristics on intimate partner violence: a consideration of social resources and risks. Am J Community Psychol. 2015;55(3):314–325. doi: 10.1007/s10464-015-9716-0. [DOI] [PubMed] [Google Scholar]
- 35.Woolcock M, Narayan D. Social capital: implications for development theory, research, and policy. World Bank Res Obs. 2000;15(2):225–249. doi: 10.1093/wbro/15.2.225. [DOI] [Google Scholar]
- 36.McLanahan S, Garfinkel I. The fragile families and child well-being study: questions, design, and a few preliminary results.; 2000. https://fragilefamilies.princeton.edu/sites/fragilefamilies/files/wp00-07-ff-mclanahan.pdf. Accessed 14 Dec 2018.
- 37.Reichman NE, Teitler JO, Garfinkel I, McLanahan SS. Fragile families: sample and design. Child Youth Serv Rev. 2001;23(4):303–326. doi: 10.1016/S0190-7409(01)00141-4. [DOI] [Google Scholar]
- 38.Lloyd S. The effects of domestic violence on women’s employment. Law Policy. 1997;19(2):139–167. doi: 10.1111/1467-9930.00025. [DOI] [Google Scholar]
- 39.Straus M. Chapter 3 Measuring intrafamily conflict and violence: the conflict tactics (CT) scales. In: Physical Violence in American Families. New York, NY: Routledge; 2017.
- 40.Voith LA, Brondino MJ. Neighborhood predictors of intimate partner violence: a theory-informed analysis using hierarchical linear modeling. Am J Community Psychol. 2017;60(1–2):187–198. doi: 10.1002/ajcp.12163. [DOI] [PubMed] [Google Scholar]
- 41.Center for Research on Child Wellbeing, Columbia Population Research Center. The fragile families and child wellbeing study (survey of parents) fifteen-year follow-up in-home observations. https://fragilefamilies.princeton.edu/sites/fragilefamilies/files/ff_hv_q15.pdf. Accessed 8 July 2020.
- 42.Bradley RH, Caldwell BM. The HOME inventory and family demographics. Dev Psychol. 1984;20(2):315–320. doi: 10.1037/0012-1649.20.2.315. [DOI] [Google Scholar]
- 43.Coulton CJ, Korbin JE, Su M. Measuring neighborhood context for young children in an urban area. Am J Community Psychol. 1996;24(1):5–32. doi: 10.1007/BF02511881. [DOI] [Google Scholar]
- 44.Breiding MJ. Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization—National Intimate Partner and Sexual Violence Survey, United States, 2011. Morb Mortal Wkly report Surveill Summ (Washington, DC 2002) 2014;63(8):1. [PMC free article] [PubMed] [Google Scholar]
- 45.VanderEnde KE, Yount KM, Dynes MM, Sibley LM. Community-level correlates of intimate partner violence against women globally: a systematic review. Soc Sci Med. 2012;75(7):1143–1155. doi: 10.1016/j.socscimed.2012.05.027. [DOI] [PubMed] [Google Scholar]
- 46.Jain S, Buka SL, Subramanian SV, Molnar BE. Neighborhood predictors of dating violence victimization and perpetration in young adulthood: a multilevel study. Am J Public Health. 2010;100(9):1737–1744. doi: 10.2105/AJPH.2009.169730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wright EM. The relationship between social support and intimate partner violence in neighborhood context. Crime Delinq. 2012;61(10):1333–1359. doi: 10.1177/0011128712466890. [DOI] [Google Scholar]
- 48.Stueve A, O’Donnell L. Urban young women’s experiences of discrimination and community violence and intimate partner violence. J Urban Health. 2008;85(3):386–401. doi: 10.1007/s11524-008-9265-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kiss L, Schraiber LB, Hossain M, Watts C, Zimmerman C. The link between community-based violence and intimate partner violence: the effect of crime and male aggression on intimate partner violence against women. Prev Sci. 2015;16(6):881–889. doi: 10.1007/s11121-015-0567-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li Q, Kirby RS, Sigler RT, Hwang S-S, LaGory ME, Goldenberg RL. A multilevel analysis of individual, household, and neighborhood correlates of intimate partner violence among low-income pregnant women in Jefferson County, Alabama. Am J Public Health. 2010;100(3):531–539. doi: 10.2105/AJPH.2008.151159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Farrington DP, Loeber R. Some benefits of dichotomization in psychiatric and criminological research. Crim Behav Ment Health. 2000;10(2):100–122. doi: 10.1002/cbm.349. [DOI] [Google Scholar]
- 52.Grych J, Hamby S. Advancing the measurement of violence: challenges and opportunities. Psychol Violence. 2014;4(4):363–368. doi: 10.1037/a0037886. [DOI] [Google Scholar]
- 53.Anguelovski I. From environmental trauma to safe haven: place attachment and place remaking in three marginalized neighborhoods of Barcelona, Boston, and Havana. City Community. 2013;12(3):211–237. doi: 10.1111/cico.12026. [DOI] [Google Scholar]
- 54.Flood M. Involving men in efforts to end violence against women. Men Masculinities. 2011;14(3):358–377. doi: 10.1177/1097184X10363995. [DOI] [Google Scholar]
- 55.Boyko JA, Wathen CN, Kothari A. Effectively engaging stakeholders and the public in developing violence prevention messages. BMC Womens Health. 2017;17(1):35. doi: 10.1186/s12905-017-0390-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wilkins N, Myers L, Kuehl T, Bauman A, Hertz M. Connecting the dots: state health department approaches to addressing shared risk and protective factors across multiple forms of violence. J Public Heal Manag Pract. 2018;24 https://journals.lww.com/jphmp/Fulltext/2018/01001/Connecting_the_Dots__State_Health_Department.6.aspx. Accessed 18 Oct 2019. [DOI] [PMC free article] [PubMed]
- 57.Goodman LA, Banyard V, Woulfe J, Ash S, Mattern G. Bringing a network-oriented approach to domestic violence services: a focus group exploration of promising practices. Violence Against Women. 2015;22(1):64–89. doi: 10.1177/1077801215599080. [DOI] [PubMed] [Google Scholar]