Short abstract
This letter to the editor describes the case of a patient with mediastinal germ cell tumor who developed COVID‐19 at the end of the first cycle of chemotherapy and continues the discussion on whether it is best to continue or delay administration of chemotherapy with an active COVID‐19 infection.
Nappi and colleagues recently reported the viewpoints of 53 highly experienced practitioners regarding the management of patients with germ‐cell tumors (GCTs) during the COVID‐19 pandemic [1]. In this survey, the authors recommend that “chemotherapy should be withheld until an active COVID‐19 infection has resolved or has been ruled out with highly accurate molecular testing.”
Here, we report the case of a young man diagnosed with a metastatic mediastinal GCT who received chemotherapy despite persistent SARS‐CoV‐2 positivity (Fig. 1).
Figure 1.
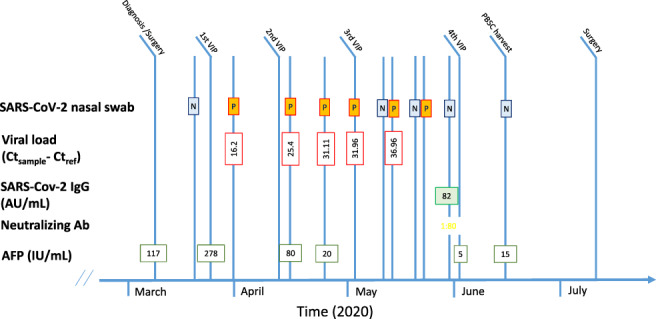
Laboratory parameters at diagnosis and during treatment.Abbreviations: AFP, alpha‐fetoprotein; AU, arbitrary units; Ct, cycle threshold; IgG, immunoglobulin G; N, negative; P, positive; PBSC, peripheral blood stem cells; VIP, etoposide, ifosfamide, cisplatin.
In March 2020, this 29‐year‐old patient underwent magnetic resonance, which revealed a lumbar spinal mass with spinal cord invasion. Following loss of sensibility in both lower limbs, palliative neurosurgery was performed, with histological diagnosis of seminoma (placental alkaline phosphatase, CD117+, CD30−, alpha‐fetoprotein [αFP]−, Ki67: 80%). Serum beta‐human chorionic gonadotropin (βHCG) was undetectable, whereas αFP and lactate dehydrogenase (LDH) were elevated (117 ng/mL; 580 U/L), suggesting nonseminoma. The computed tomography (CT) scan showed a tumor mass of 9.4 × 6.2 × 10 cm in the anterior mediastinum, with superior vena cava compression. The testicles had no evidence of disease and the SARS‐CoV‐2 nasopharyngeal swab was negative.
Given the poor‐risk features [2], chemotherapy with the VIP regimen was commenced (etoposide 75 mg/m2, ifosfamide 1,200 mg/m2, cisplatin 20 mg/m2, days 1–5, every 21 days). VIP was preferred to BEP (bleomycin, etoposide, cisplatin) to limit the contacts with the health care system and to avoid bleomycin pulmonary toxicity. Prophylactic filgrastim was administered for 7 days.
After cycle 1, the patient developed transient high fever, conjunctivitis, dysgeusia, and anosmia and tested positive for SARS‐CoV‐2. Blood tests revealed lymphocytopenia and elevation of C‐reactive protein, transaminases, and LDH. He was hospitalized and treated with hydroxychloroquine, darunavir, and enoxaparin, with complete resolution of symptoms. However, two swabs before cycle 2 were positive for SARS‐CoV‐2.
To ensure optimal treatment delivery, cycle 2 was administered on April 14, and hydroxychloroquine was administered on days 1–7. αFP decreased to 20 ng/mL. The restaging CT scan revealed significant tumor response at the mediastinal and lumbar levels. However, atypical, basal pneumonia was compatible with COVID‐19 (Fig. 2).
Figure 2.
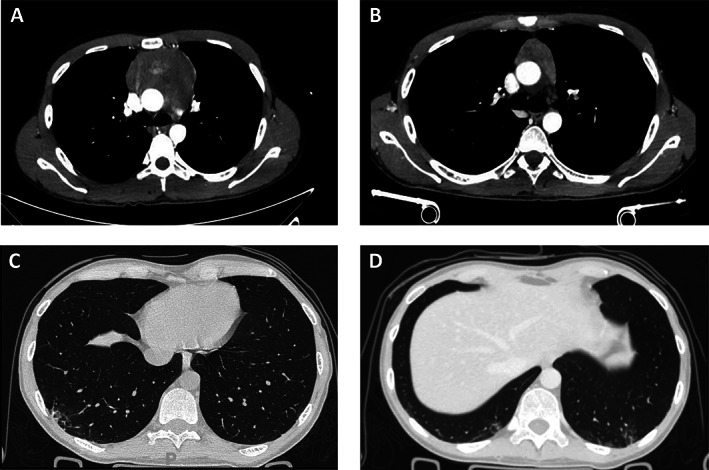
Radiological findings. Computed tomography (CT) scan showing the mediastinal mass at baseline (A) and after two cycles of chemotherapy (B); CT scan performed after two cycles of chemotherapy showing interstitial pneumonia (C, D).
Despite this finding, cycle 3 was administered and hydroxychloroquine was discontinued owing to suggested uselessness. Swabs were performed on May 19 (negative) and May 20 (positive). Finally, two serial swabs tested negative and SARS‐CoV‐2–specific immunoglobulin G (DiaSorin, Saluggia, Italy) were detected.
The additional cycle 4 was administered on June 2. αFP, βHCG, and LDH were normal. A leukapheresis procedure was performed, with the successful collection of CD34+ cells for subsequent high‐dose chemotherapy [3], and the patient underwent another intervention of spinal stabilization.
The SARS‐CoV‐2 viral loads in nasopharyngeal swabs were retrospectively estimated using the cycle threshold (Ct) method (Ctsample‐Ctref). Ct values increased from 16.2 Ct (high viral load) to 36.96 Ct (low viral load) after cycle 3, suggesting that viral clearance may have occurred during cycle 3 and that subsequent positive swabs did not represent active viral replication, but only residual RNA detection. To evaluate the presence of viable SARS‐CoV‐2, swabs collected before cycle 4 were inoculated into cell cultures (Vero‐E6 cells); the cell culture method showed neither virus isolation nor cytopathic effect, further reinforcing the concept of complete viral clearance [4].
In conclusion, this patient with a poor‐risk GCT underwent multimodal curative treatment despite persistent COVID‐19 infection. Our report reinforces the notion that chemotherapy could be safely given in patients who need prompt intervention, without necessarily worsening the course of COVID‐19 [5].
Disclosures
The authors indicated no financial relationships.
Acknowledgments
This research was partially supported by funds from Ricerca Corrente, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy. C.C. is supported by a European Society for Medical Oncology Clinical Research Fellowship (2019–2020).
No part of this article may be reproduced, stored, or transmitted in any form or for any means without the prior permission in writing from the copyright holder. For information on purchasing reprints contact commercialreprints@wiley.com. For permission information contact permissions@wiley.com.
References
- 1. Nappi N, Ovviano M, Rescigno P et al. Management of germ cell tumors during the outbreak of the novel coronavirus disease‐19 pandemic: A survey of international expertise centers. The Oncologist 2020;25:e1509–e1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Honecker F, Aparicio J, Berney D et al. ESMO Consensus Conference on testicular germ cell cancer: Diagnosis, treatment and follow‐up. Ann Oncol 2018;29:1658–1686. [DOI] [PubMed] [Google Scholar]
- 3. Rosti G, Secondino S, Necchi A et al. Primary mediastinal germ cell tumors. Semin Oncol 2019;46:107–111. [DOI] [PubMed] [Google Scholar]
- 4. La Scola B, Le Bideau M, Andreani J et al. Viral RNA load as determined by cell culture as a management tool for discharge of SARS‐CoV‐2 patients from infectious disease wards. Eur J Clin Microbiol Infect Dis 2020;39:1059–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pinato DJ, Zambelli A, Aguilar‐Company J et al. Clinical portrait of the SARS‐CoV‐2 epidemic in European cancer patients. Cancer Discov 2020;10:1465–1474. [DOI] [PMC free article] [PubMed] [Google Scholar]


