Abstract
Introduction
Aortocaval fistulas (ACFs) are a rare complication of abdominal aortic aneurysm (AAA), associated with high morbidity and mortality. It is thought that increased tension in the walls of large aneurysms can cause an inflammatory reaction resulting in adhesion to the adjacent vein and culminating in necrosis of the adherent layers and fistula formation.
Presentation of case
A 70-year-old male was referred from a local state center to the emergency department of our hospital, complaining of weakness and oliguria for two days. The laboratory analysis yielded high urea and creatinine levels, indicating an acute renal failure. Computed tomography images showed an aortocaval fistula complicating infrarenal abdominal aortic aneurysm. The patient was successfully managed with endovascular intervention.
Discussion
Aortocaval fistulas generally affect elderly men with an average age of 65 years. The diagnosis is often delayed because of the variable clinical manifestations, which increases the difficulties in treatment. Conventional surgical intervention has high mortality rates. However, endoleaks and paradoxical pulmonary embolism are the main concerning complications of endovascular treatment.
Conclusion
Spontaneous aortocaval fistulas are a rare, but potentially life-threatening complication of abdominal aortic aneurysm with myriad clinical manifestations. Early diagnosis and management can directly affect the prognosis and outcome. Modern non-invasive diagnostic imaging can help timely diagnosis and provide a road map for the treatment plan. Endovascular repair is the first choice of treatment. However, a high incidence and persistence of endoleak with the endovascular approach requires caution and a close long time follow up.
Keywords: Endovascular management, Aortocaval fistula, Abdominal aortic aneurysm, Case report
Highlights
-
•
Spontaneous aortocaval fistulas are a rare complication of abdominal aortic aneurysm.
-
•
Early diagnosis and management can directly affect the prognosis and outcome.
-
•
Modern non-invasive diagnostic imaging can help timely diagnosis.
-
•
Endovascular repair is the first choice of treatment.
Abbreviations
- ACF
Aortocaval fistula
- AAA
Abdominal aortic aneurysm
- EVAR
Endovascular repair
1. Introduction
Aortocaval fistula (ACF) are a rare complication of abdominal aortic aneurysm (AAA) that often result from erosion or rupture of an abdominal aortic aneurysm into the inferior vena cava [1]. Abdominal pain, abdominal machinery bruit, and a pulsating abdominal mass are the triad of clinical findings. Other findings include pelvic venous hypertension, lower-limb edema with or without arterial insufficiency or venous thrombus, shock, congestive heart failure, and cardiac arrest [2]. Because of the variable clinical manifestations, the diagnosis is often delayed, which increases the difficulties in treatment [3]. Both, conventional open surgery and endovascular repair (EVAR) can be used for the treatment of aortocaval fistula. Conventional surgical intervention has high mortality rates, whereas endoleaks and paradoxical pulmonary embolism are the main concerning complications of endovascular treatment. However, a combination of a bifurcated endograft and a vascular occluder can be a good option for the treatment of aortocaval fistula complicating abdominal aortic aneurysm [1]. The authors present here a case of spontaneous aortocaval fistula presented with an acute renal failure in a 70-year-old male with an abdominal aortic aneurysm, successfully managed with EVAR.
This work has been reported in line with the SCARE 2020 criteria [4].
2. Case presentation
A 70-year-old male was referred from a local state center to the emergency department of our hospital with a complaint of weakness and oliguria for two days. He had a 3-year history of hypertension and long history of smoking and Chronic Obstructive Pulmonary Disease (COPD). On physical examination, he was well conscious and oriented. His vital signs were unremarkable. On auscultation the heart sounds were normal and some rhonchi were audible on the middle zone of the lungs. On palpation, no palpating mass, rebound tenderness, and guarding were detected in abdominal examination. All lower extremity arterial pulses were normally palpable.
The laboratory analysis yielded hemoglobin (Hb): 11.6 g/dl (12–16), white blood cells: 14340/mm3 (4500–11000) with neutrophils 85.7%, Urea: 192 mg/dl, creatinine: 10.49 mg/dl, fibrinogen: 416 mg/dl, and D-dimer was 4088 μg/l. Findings on his chest X-Ray and echocardiography were interpreted as normal. Non- contrast CT images, showed an infra-renal abdominal aortic aneurysm with a transverse diameter of 7.8 cm [Fig. 1a]. However, for more detail a contrast enhanced abdominal CT was advised. As the patient had acute renal failure, so following an urgent hemodialysis a contrast enhanced CT exam was performed. CT findings included early detection of contrast material in the inferior vena cava, suggestive of a fistula between the abdominal aorta and IVC (the abdominal aorta was seen to be open into the proximal part of the left common iliac vein in the right lateral wall just before the iliac bifurcation) [Fig. 1, Fig. 2]. The patient was diagnosed to have an acute renal failure, resulting from spontaneous aortacaval fistula.
Fig. 1.
a. Non- contrast enhanced coronal CT image shows a large abdominal aortic aneurysm (red arrow), compressing the IVC.b. Contrast enhanced MIP coronal CT image shows a large abdominal aortic aneurysm (arrow) distal to the renal arteries, compressing the IVC.
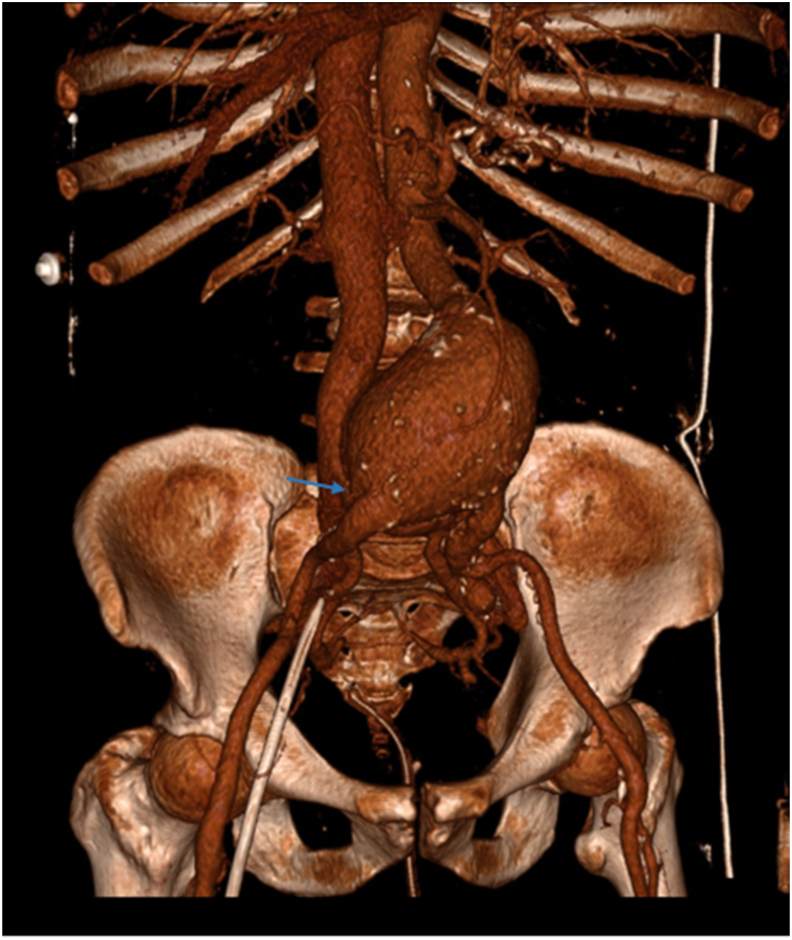
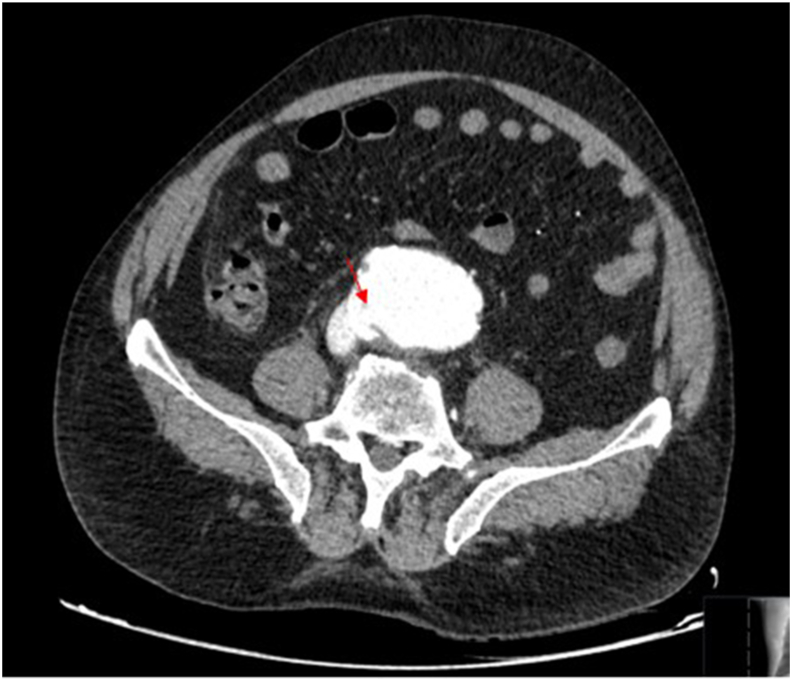
Fig. 2.
a. Volume rending 3D CT image shows a large abdominal aortic aneurysm distal to the renal arteries and the approximate location of the aortocaval fistula (green arrow). b. Contras enhanced axial CT image shows indentation and fistula line in the vena cava (red arrow), disappearance of the fatty planes between vena cava and aorta, and rapid simultaneous contrast passage into the vena cava from the aorta.
He was transferred to the cardiovascular surgery unit and taken up for minimally invasive endovascular intervention by the qualified interventional radiology and vascular surgery teams. The right and left femoral artery, and the left femoral vein were surgically explored. After heparinization, a 7f introducer sheath was inserted through the femoral artery. Pigtail catheter was introduced to pull through the fill femoral artery. The Medtronic Endurant II unibody device was opened at 28x 16 x 145 infrarenal level by sending a rigid carrier wire from the right femoral artery. A stiff attachment wire was sent from the left atrium, over which the contralateral leg was opened with Medtranoic Endurate II 16 x 16 x 93. Afterwards, a Medtranoic Endurate II 16x16x82 with ipselateral extension was opened to the left side. The aortic attachment zone and overlapping segments of the graft were dilated with an aortic balloon. The procedure was terminated by implanting a 24 × 240mm diameter stent graft leg in the location of the aneurysm sac close to the proximal of the left common iliac vein. Leakage into the aneurysmal sac was not detected on control angiography [Fig. 3]. Surgical repair was performed after hemostasis of the right and left femoral arteries and femoral vein. The tissues layers were closed according to the anatomic plan. The patient was transferred to the intensive care unit as extubated postoperatively. His hemodynamics, vital signs, and peripheral pulses remained stable. No significant complications occurred during or after the procedure. The patient was consulted to the nephrology with postoperative renal function test values and the dialysis program was restarted according to that. After improvement of renal functions, normalization of the BUN and serum creatinine levels, the patient, whose urine-outflow was sufficient, vital signs and renal functions were stable during the service follow-up, was discharged with outpatient follow-up recommendations.
Fig. 3.
Post stent graft control angiogram shows no endoleak.
3. Discussion
ACF was first described by Symes in 1831, and Woolley in 1995 reported the first case of aortic exclusion used in the treatment of an intraoperatively diagnosed ACF. Most ACF had been repaired primarily in an open intervention and the literature accounted the surgical mortality to be as high as 16–66% [5]. A primary/spontaneous ACF occurs in 1% of AAA cases and 6% of ruptured AAA cases, being thus responsible for 80% of all ACF cases [6]. It is believed that increased tension in the walls of large aneurysms can cause an inflammatory reaction resulting in adhesion to the adjacent vein and culminating in erosion of the adherent layers and fistula formation [1]. Other causes include penetrating abdominal trauma, iatrogenic trauma at lumbar disc surgery and connective tissue disorders [7].
The disease generally affects elderly men with an average age of 65 years. Smoking appears to be the risk factor most strongly associated with AAA [8,9]. The clinical signs and symptoms are quit variable that include abdominal pain, venous hypertension, lower-limb edema with or without arterial insufficiency or venous thrombus, shock, congestive heart failure, and cardiac arrest. However, abdominal pain, abdominal machinery bruit, and a pulsating abdominal mass are the classical triad of clinical findings [2]. Because of the variable clinical manifestations, the diagnosis is often delayed, which increases the difficulties in treatment [3]. Our patient was presented with an acute renal failure, which is unique for this case and he did not have the characteristic findings of ACF or abdominal aortic aneurysm. His body habitus may probably mad abdominal examination particularly difficult and it was only after CT examination became apparent.
Preoperative diagnosis of an aortocaval fistula is helpful in planning operative strategy, in preparing for the massive blood loss, and for avoiding dislodgement of atheromatous debris that can make an embolization across the fistula causing pulmonary embolism. Contrast CT angiogram and MRA are the non-invasive imaging modalities of choice for the diagnosis of an aortocaval fistula [9]. The pathognomonic imaging findings on CT, include indentation and fistula line in the vena cava, disappearance of the fatty planes between vena cava and aorta, and rapid simultaneous contrast passage into the vena cava from the aorta [10]. The same findings were noted in our case.
Both conventional open surgery and endovascular repair can be used for the treatment of Aortocaval fistula [6]. Conventional surgical intervention has high mortality rates, whereas endoleaks and paradoxical pulmonary embolism are the main concerning complications of endovascular treatment. However, a combination of a bifurcated endograft and a vascular occluder can be a good option for the treatment of aortocaval fistula complicating abdominal aortic aneurysm [1]. The suitable Criteria for stent grafting are; AAA <4 cm, Aneurysmal neck <26 mm diameter and ifrarenal aortic neck length of 1 cm [8].
When considering a high reported mortality rate for open repair of ACF, many surgeons still look to endovascular repair as the first choice of treatment with a mortality rate of about 3.8% if there is not a delayed in diagnosis, comparing to the open surgery that may have a mortality rate of about 12% [5]. Moreover, endovascular repair is beneficial for frail patients and hostile anatomy. On the contrary, open repair is performed when ACF is a coincidental finding during exploratory laparotomy, or when the aortic anatomy is extremely hostile for endovascular treatment. However, open repair can be preferred against EVAR, when comorbidities affecting the cardiovascular and respiratory system are absent. Especially in younger patients, constant follow-up and reintervention, which are often required after endovascular surgery, can be avoided with open repair [6]. On the other hand close attention must be paid to the presence of superficial vein dilation, safe visualization of the renal arteries, and hemodynamic perturbances on stent graft deployment during EVAR [11].Our patient was successfully treated with endovascular stent graft repair and no endoleak into the aneurysmal sac was detected on control angiography.
Although this is one of the documented cases, proved with imaging studies and managed by endovascular stent graft, lack of the long time follow up may be the only limitation for this case.
4. Conclusion
Spontaneous aortocaval fistula are a rare complication of abdominal aortic aneurysm with a high mortality and various clinical manifestations that may present with an acute renal failure. Early diagnosis and management can directly affect the prognosis and outcome. Modern non-invasive diagnostic imaging can help timely diagnosis and provide a road map for the treatment plan. Endovascular repair is the first choice of treatment for frail patients and hostile anatomy. However, a high incidence and persistence of endoleak with the endovascular approach requires caution and a close long time follow up.
Ethical approval
The manuscript has got an ethical review exemption from the Ethical Review Committee (ERC) of our institution, as case reports are exempted from review according to the institutional ethical review committee's policy.
Sources of funding
The authors declare that their work is not funded by any institution, organ, or government and they have no financial support.
Author contribution
Concept - HAE; Design – HAE; Supervision - MWN; Resources and data Collection- HAE; Literature Search - HAE; Writing Manuscript – HAE; Critical Review -.MWN. All authors have read and approved the final manuscript.
Registration of research studies
Not applicable.
Guarantor
The corresponding author is the guarantor for the work and he has the responsibility of access to the data, and controlling the decision to publish.
Consent
Written informed consent was obtained from the patient's next of kin for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
The authors have no potential conflicts of interest to disclose.
Acknowledgments
The authors would like to acknowledge Pro. Dr. Mustafa Harman and Dr. Aydan Ahmadowa for the radiologic diagnosis of this case and Dr. Mustafa Parildar for reporting the interventional procedure, as well as the EGE University Hospital PACS's authorities for providing the patient information.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.01.090.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Almeida Bruno Lorenção de. Endovascular treatment of an abdominal aortic aneurysm with aortocaval fistula using a vascular occluder and a bifurcated endograft in a single intervention: case report. J. vasc. Bras, Porto Alegre. 2017;6(2):68–173. doi: 10.1590/1677-5449.007916. [DOI] [Google Scholar]
- 2.Kim I.H., Min H.K., Kim J.Y., Kim D.K., Kang D.K., Jun H.J., Hwang Y.H. Surgical repair of aortocaval fistula presenting with cardiogenic shock. Kor. J. Thoracic Cardiovasc. Surg. 2018;51(6):406–409. doi: 10.5090/kjtcs.2018.51.6.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang T., Huang B., Zhao J., Yang Y., Yuan D. Aortocaval fistula resulting from rupture of abdominal aortic dissecting aneurysm treated by delayed endovascular repair: a case report. Medicine. 2016;95(18) doi: 10.1097/MD.0000000000003570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Orion K.C., Beaulieu R.J., Black J.H., 3rd Aortocaval fistula: is endovascular repair the preferred solution? Ann. Vasc. Surg. 2016;31:221–228. doi: 10.1016/j.avsg.2015.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patelis N., Giagkos G.C., Maltezos K., Klonaris C. Aortocaval fistula: an unusual complication of ruptured abdominal aortic aneurysm. BMJ Case Rep. 2018 doi: 10.1136/bcr-2018-224998. 2018, bcr2018224998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ravari H., Moini M., Vahedian M., Aliakbarian M. Spontaneous aortocaval fistula: a case report and literature review. Iran. Red Crescent Med. J. 2011;13(4):276–279. [PMC free article] [PubMed] [Google Scholar]
- 8.Woolley D.S., Spence R.K. Aortocaval fistula treated by aortic exclusion. J. Vasc. Surg. 1995;22(5):639–642. doi: 10.1016/s0741-5214(95)70053-6. [DOI] [PubMed] [Google Scholar]
- 9.Ravi R., Peter S.B., Swaminathan T.S., Chandrasekary V. Spontaneous aortocaval fistula due to abdominal aortic aneurysm rupture-a case report. Indian J. Radiol. Imag. 2006;16(4):453–456. https://www.ijri.org/text.asp?2006/16/4/453/32245 [Google Scholar]
- 10.Psathas E.D., Lioudaki S., Doulaptsis M., Charalampoudis P., Klonaris C., Verikokos C. Clinical manifestations of aortocaval fistulas in ruptured abdominal aortic aneurysm: report of two cases. Case Rep. Surg. 2012:123081. doi: 10.1155/2012/123081. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dabbouseh N.M., Mason P.J., Patel P.J., Rossi P.J. Endovascular repair of delayed traumatic aortocaval fistula. J. Vascular Surg. Cases Innov. Tech. 2019;5(4):467–471. doi: 10.1016/j.jvscit.2019.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.