Abstract
Background
The lockdown imposed due to novel coronavirus disease 2019 (COVID-19) has resulted in adopting electronic learning (e-learning) as the means of education in various institutions all over India. This study aimed to collect the experiences of faculty and students regarding e-learning in medical colleges during COVID-19 and to analyse the likely perceived benefits and problems to choose blended learning activities after the COVID crisis.
Methods
A survey-based study was conducted among undergraduate students and faculty members in medical colleges of Delhi-NCR.
Result
Two hundred forty-eight medical students and 23 faculty members participated in the study. Two hundred twelve (85.4%) students considered medical education to be severely affected during the lockdown and 219 (88.3%) students found the online classes to be useful. Poor connectivity followed by lack of human interface and poor sound or acoustics were the major hindering factors, whereas convenience and access were reported as important facilitating factors. In the postlockdown phase, 135 (54.4%) students want online classes to be continued in addition to classroom teaching for the cognitive domain, 42 (16.9%) students want it for both cognitive and psychomotor domain and 60 (24.1%) do not want online classes. The majority of the faculty members (65.2%) were in favour of including online teaching modules in routine curriculum and 69.6% suggested a 70%:30% distribution of traditional and online classes after the COVID lockdown.
Conclusion
Implementation of e-learning within the existing curriculum is bound to be challenging; however, it remains the only solution during COVID-19 imposed lockdown for maintaining the chain of learning.
Keywords: COVID-19, Coronavirus, Learning, Medical education, Medical student
Introduction
Novel coronavirus disease 2019 (COVID-19) has caused widespread panic and disease globally and in India.1 In addition to healthcare and economic losses, the lockdown imposed during COVID has adversely affected educational opportunities.2
Traditional educational activities use the live experience of a facilitator with the students. This can be in the form of a large group or small group activity for teaching any of the three domains—cognitive, psychomotor or affective.3 The revised curriculum by Medical Council of India mandates the revision in the traditional teaching-learning methods to include more interactive sessions, small group discussions with use of e-resources.4 E-learning is a newer concept in education, where electronic media or technology (internet- or non-internet–based) are used for learning. Online learning has been less frequently practiced in medical education in developing countries such as India citing lack of infrastructure, expertise and feasibility.5 Traditional teaching including using printed material as resource material are identified as cornerstone for learning by most medical students versus internet-based or non-online computer–based learning.6
However, e-learning has emerged as the only possible mode of education during COVID crisis for school and college students. Medical education is more challenging and stressful as it involves bedside and soft skills training which cannot get adequately represented through e-learning. We therefore planned this study to assess the students' and faculty's perceptions towards e-learning as a mode of education when widely implemented during the COVID pandemic.
Materials and methods
This was a cross-sectional online survey administered to the undergraduate students and faculty members of medical colleges in Delhi-NCR region shared through social group messaging on WhatsApp to known alliances/students who further circulated it to their contacts. The questionnaire was developed by discussion among 4 undergraduate teachers of different specialities and one senior resident. This was then revised and edited by 2 medical education faculty members. A pretesting was carried out among 10 students. The response was then reviewed by the 2 medical education faculty and the 4 undergraduate teachers together, and the questionnaire was finalized. The study was conducted during the second week of April, 2020 (approximately three weeks after enforcement of complete lockdown in the country). Informed consent was taken from the respondents. The study was approved by the institutional ethics committee.
The participants were provided with a questionnaire through an online Google form to assess their perceptions of online learning during COVID-19 lockdown. There were 22 questions (20 closed questions) in the learners' questionnaire and ten questions (nine closed questions) in the faculty's questionnaire. It consisted of questions on the effect of lockdown on medical education, time spent on online and offline learning, and the various modality of didactic learning used by the students during this phase. It also assessed the time spent by students on the online lectures organized by the college and their experiences, whether they found them useful, duration of each lecture they would prefer and if they had sufficient opportunity to interact with educators and resolve their doubts. The various facilitating and hindering factors during online classes faced by the students were analysed too. The answers to questions pertaining to more time being spent online, online learning being preferred over traditional classroom teaching, were graded on a 5-point scale between strongly disagree, disagree, neutral, agree and strongly agree. The options regarding the various modes of learning used during lockdown and frequency of using them were rated on a 5-point Likert scale, with 1 being never and 5 being very frequently. The questions regarding the various facilitating and hindering factors were graded on a scale of 1–5 with 1 being not helpful/not problematic and 5 being most helpful/most problematic, respectively. Regarding the features preferred during online classes, options ranged from 1-not prefer to 5-strongly recommend. In the faculty questionnaire, experience related to the various features of online learning such as timing, connectivity, logistics, lesson preparation, convenience and access, interest and interaction with students were graded from 1-poor to 5-excellent. A 5-point Likert scale was used to rate the overall experience of an online class, where one was unsatisfactory and five was excellent. The form collected all responses in an anonymous manner without personal identification information like college or city.
Sample size
The sample size was calculated assuming 90.6% students who would use an online tool for learning as per a study (Wynter et al, 2019)7 The sample size required with an absolute precision of five percent with design effect of one will be 131 students. A convenient sample of 25 faculties was chosen to record the facilitators’ perceptions.
Statistical analysis
Data were recorded on a MS excel sheet and analysed using SPSS, version 23. Quantitative data were expressed by mean and standard deviation and significance level of differences between the means were tested by Student's t-test (unpaired). Proportions were compared by chi-square test or Fisher's exact-test. A P value of <0.05 was considered statistically significant.
Results
A total of 248 students of medical colleges from Delhi-NCR region participated in the study. The distribution of students from different batches was as follows: 53 students (21.4%) were from first year, 27 students (10.9%) from second year, 120 students (48.4%) from third year and 48 students (19.4%) from the final year. There were 23 responses from the faculty who had an experience of taking online classes, 13 (56.5%) had more than ten years of teaching experience, 5 (21.7%) teachers had <5 years’ experience and 5 had experience between 5 and 10 years. There were 18 (78.3%) teachers from clinical fields, 4 (17.4%) from preclinical and 1 (4.3%) from paraclinical subjects.
Medical education was severely affected during the lockdown according to 212 (85.4%) of the students. A total of 219 (88.3%) students found the online classes to be useful in facilitating education during this period. Table 1 shows the frequency of various modes of learning used by the students during the lockdown period which varied significantly between different batches (P < 0.05). A total of 187 students (75.4%) were spending between one-four hours/day on online learning at home, 31 (12.5%) students spent > 4 h whereas, 30 (12.1%) spent <1 h. However, the tendency to spend more time on online learning than offline was reported by only 72 students (29.0%). The opportunity to interact with the educator was sufficient according to 108 (43.5%) students, 74 (29.8%) were neutral, whereas 69 (27.8%) felt it was inadequate. In response to the question of getting their doubts cleared during the online session, 186 (75.0%) answered in affirmation while 62 (25.0%) students felt it was not carried out.
Table 1.
Sources of study material used by students of different batches during lockdown.
| Sources of study | MBBS-1st year, (n = 53) | MBBS-2nd year (n = 27)< | MBBS-3rd year Part I, (n = 120) | MBBS-3rd year Part II, (n = 48) |
|---|---|---|---|---|
| Printed material – books, notes | 45 (84.9%) | 17 (63.0%) | 86 (71.7%) | 38 (79.2%) |
| Online material – self-study | 27 (50.9%) | 20 (74.1%) | 69 (57.5%) | 27 (56.3%) |
| Online material – coaching centres | 12 (22.6%) | 14 (51.9%) | 86 (71.7%) | 26 (54.2%) |
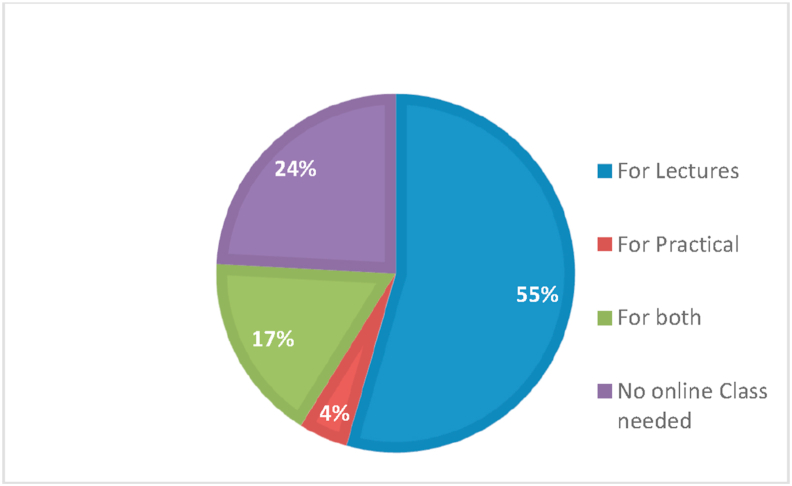
Regarding their own preference on the time that should be invested on online classes per day, 119 students (48.0%) opted for 1–2 h, 88 (35.5%) were willing to spend 2–4 h, 22 (8.9%) preferred < 1hr and only 19 (7.7%) students wanted to give >4 h to online classes. The most preferred duration of each lecture was between thirty minutes and one hour, according to 187 (75.4%), 35 (14.1%) students wanted it to be 1–2 h long and 26 (10.5%) wanted it to be less than 30 min in duration. Online learning was preferable to traditional classroom teaching by 88 (35.4%) students, 107 (43.1%) students did not prefer online teaching over traditional classroom and 53 (21.4%) remained neutral. After the lockdown period, 135 (54.4%) students wanted online classes to be continued in addition to classroom teaching for cognitive domain (lectures), 42 (16.9%) students wanted it for both cognitive (lectures) and psychomotor domain (practical), 11 (4.4%) students suggested using them for only psychomotor domain (practical), whereas 60 (24.1%) students were against having any online classes. Fig. 1 shows the preference of students for the continuation of the online classes after the lockdown.
Fig. 1.
Preference for e-learning platform after lockdown would open.
From the perspective of the faculty members, 15 (65.2%) were interested in including online teaching modules in routine curriculum once classroom teaching restarts, 3 (13%) were against it and 5 (21.7%) remained neutral. Sixteen (69.6%) teachers suggested a 70%:30% distribution of traditional and online classes, 4 (17.4%) wanted it to be equally distributed and 3 (13%) preferred only classroom teaching. Use of online platforms for internal assessments in routine curriculum was recommended by 10 (43.5%) faculty, 4 (17.4%) did not prefer it and the 9 (39.1%) were neutral.
Table 2 shows different features of online sessions which were preferred and recommended by the learners. The option for viewing the content later offline and the inclusion of online videos or live demonstrations in the classes was preferred by most of the students. Poor connectivity was the most commonly recorded hindering factor (94, 35.9%), followed by lack of human interface (78, 29.8%) and poor sound or acoustics (71, 27.1%). One hundred seventy-nine (68.3%) found convenience and access as one of the important facilitating factors followed by improved understanding (108, 41.2%) and good presentations (112, 42.7%). One hundred and ninety-one (75.2%) students could solve their doubts during the online class. Majority identified a lack of clinical skills exposure and the opportunity to collaborate with peers as the biggest disadvantage of online classes.
Table 2.
Features of online sessions preferred by learners.
| Characteristics of online session | Not recommend n(%) | Neutral n(%) | Recommend n(%) |
|---|---|---|---|
| Link for additional teaching-learning material | 35 (14.1%) | 61 (24.6%) | 152 (61.3%) |
| Online videos or live demonstrations | 29 (11.7%) | 36 (14.5%) | 183 (73.8%) |
| Visual interface of the teacher | 39 (15.7%) | 78 (31.5%) | 131 (52.8%) |
| Break between two consecutive lectures | 24 (9.7%) | 45 (18.1%) | 179 (72.2%) |
| Option for questions/doubts during the lecture | 26 (10.5%) | 53 (21.4%) | 169 (68.1%) |
| Interactive quiz during the lecture with mandatory responses | 78 (31.5%) | 64 (25.8%) | 106 (42.7%) |
| Option for feedback about the class after the session | 48 (19.4%) | 77 (31.0%) | 123 (49.6%) |
| Access platform for online classes in college/library | 31 (12.5%) | 62 (25.0%) | 155 (62.5%) |
| Option for offline viewing later | 11 (4.4%) | 32 (12.9%) | 205 (82.7%) |
Assessed on 5-point Likert scale, where 1,2-meant not recommend, 3-neutral and 4,5-recommend/strongly recommend.
For the overall experience of online class/lecture/webinar (rated on a 5-point Likert scale where one was unsatisfactory and five was excellent), 5 faculty members (21.7%) found the experience to be excellent with a score of five, 7 (30.4%) gave a score of four, 9 (39.1%) gave a score of three and 1 (4.3%) each gave a score of two and 1. Amongst the individual features of online learning, timing and scheduling, connectivity, logistics, lesson preparation, convenience and access for teachers, interest and interaction with students were all rated three by the majority, lesson experience was rated three and four by equal number of participants.
The excerpts from student and faculty responses are shown in Box 1. To make these online classes more efficient, many students suggested online classes to be made into a video library with breakdown of lecture contents into smaller lectures. The provision of additional reading material and discussion points before lectures was desired by several students. To make the class more interactive several suggestions were made in the form of using a common chat box, including the visual interface of the teacher, organising separate doubt solving sessions and use of whiteboard, blackboard, tablets for writing and explaining in place of reading from a PowerPoint presentation. Several students wanted illustrations with the help of a stylus, the usage of applications such as 3D anatomy and playing videos of clinical examination and procedures to make the topics more understandable. Technical difficulties faced by the teachers leading to frequent interruptions during the class were disliked by students with suggestions to train the educators with the help of tutorials before the class. The teachers were satisfied with the participation of the students on the online platform. They were overall appreciative of the role of online learning in facilitating medical education during the pandemic associated lockdown. However, most of them were of the opinion that it should act as an adjunct and not a replacement of traditional classroom teaching in future.
Box 1. Comments from students and faculty.
| Student responses | Faculty responses |
|---|---|
|
|
Alt-text: Box 1
Discussion
Online teaching is a pedagogical tool that has the potential to transform medical education and has proved to be very useful during the standstill brought by COVID lockdown. The present study reports the experiences of medical students and faculty of the Delhi-NCR region regarding online education during this phase. The study also highlights the limitations of the methodology in its present state and suggestions for an improved learning experience.
In our study, most of the students preferred traditional classroom teaching however, a significant number of students (35.4%) chose online learning over traditional classroom teaching. The preference was more for the theory topics than practical ones. A similar study was carried out by Singh et al8 who reported traditional classroom being preferred by 106 (50.9%) students and E-classes by only 46 (22.1%) students.
E-learning provides flexibility, convenience to the learner, better platform for sharing information for psychomotor skill, repeatability, improved access of medical information and improved learning experiences. The outlook of medical curriculum may also evolve with digitalisation of medical education using innovative technology. However, there are issues with logistics, supplies, cost, training and validity of information6 as were also reported in the present survey. According to a study from Pakistan involving 382 MBBS and BDS student, 77.4% students showed negative perception about e-learning, of which 86% students felt e-learning has little impact on their learning.9 Both students and teachers reported benefits of features such as video calls and group chat with online platform (Microsoft Teams) in improving the interaction with quick adaptability of the students.10 They however reported poor internet connectivity leading to call dropouts as a limiting factor.10 The use of GoogleHangouts for teaching students in surgery had the limitation of allowing only 10 students to attend at a time.11 A combination of Zoom and Microsoft Teams were recommended for educational activities during the pandemic with prior orientation to the online platform, use of visual interface, proper usage of microphones, availability of a person for troubleshooting during live sessions and the role of a moderator to enhance the teaching-learning experience.12
A web-based training of orthopaedic residents and fellows during the COVID-19 pandemic found the ability to revisit the digitally recorded session, ease of access to both clinical material and key articles, and the ability to connect individuals of different geographic regions as the beneficial factors of online learning over traditional in-person learning.13 Another study from Nepal suggested using interactive sessions, quizzes, brainstorming sessions and students giving presentations as some of the methods to improve student participation and attention during the online sessions while slow internet connections, lack of technical knowledge, issues with etiquette with volume controls and video backgrounds as some of the limitations.14
E-learning helps in improved understanding of the subjects and skills, the ease of accessibility, flexible timing and the chance to interact better with coparticipants.15 It may be associated with dissatisfaction amongst the students due to limited interaction with the educator16 and inadequate chances for solving queries and clarification of concepts for complex topics,17 as were seen in the present study. Students preferred e-learning as a supplement to the conventional didactic methods rather than a replacement,18,19 as experienced by the present study group.
The faculty experiences with e-learning have been variable in the past. In a questionnaire-based study, 500 faculty across 35 medical colleges in Korea reported high usefulness and usability of an e-learning platform. However, only 39% of the faculty had incorporated e-learning into their lessons citing reasons of lack of resources, time, awareness and expertise.20 Another study on 28 medical faculties from Iran reported lacunae in organization, infrastructure, legal-ethical issues such as copyrights and ethical issues as chief barriers to e-learning.4
The participants in the present study belonged to Delhi-NCR region; hence results may not be generalized to medical students all over the country. As the participants belonged to different institutes and used different platforms, hardware and software devices and technological tools for attending the classes, there was a lack of homogeneity in evaluating the teaching-learning methods used. The previous exposure of the medical students and faculty members to e-learning was also not checked which has the potential of affecting the perceptions towards online classes during lockdown. However, the experiences and feedback gained from such studies would help in organising a planned introduction of e-learning tool in the curriculum in the future.
The aforementioned examples highlight the student experiences and the foreseen problems with e-learning. It however, remains as the only feasible solution during the COVID crisis and national lockdown for maintaining the chain of learning. The process of implementation of the same within the existing curriculum is bound to have varied challenges. The pandemic however, has helped schools and colleges to innovate e-learning solutions, which will go a long way in revolutionising medical education.
Disclosure of competing interest
The authors have none to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.mjafi.2020.12.008.
Appendix A. Supplementary data
The following is/are the Supplementary data to this article:
References
- 1.Government of India: India fights Corona-19. [Accessed 2020 Apr 5]. https://www.mygov.in/covid-19/?cbps=1.
- 2.Rose S. Medical student education in the time of COVID-19. J Am Med Assoc. 2020;323(21):2131–2132. doi: 10.1001/jama.2020.5227. [DOI] [PubMed] [Google Scholar]
- 3.MCI booklet. Vision. 2015. https://old.mciindia.org/tools/announcement/MCI_booklet.pdf [Google Scholar]
- 4.Medical Council of India. Undergraduate curriculum. [Accessed 2019 Jun 12]. https://www.mciindia.org/CMS/wp-content/uploads/2019/01/UG-Curriculum-Vol-I.pdf.
- 5.Keshavarzi M.H., SoltaniArabshahi S.K., Gharrahee B., Sohrabi Z., Mardani-Hamooleh M. Exploration of faculty members' perceptions about virtual education challenges in medical sciences: a qualitative study. J Adv Med Educ Prof. 2019;7(1):27–34. doi: 10.30476/JAMP.2019.41042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guarino S., Leopardi E., Sorrenti S., De Antoni E., Catania A., Alagaratnam S. Internet-based versus traditional teaching and learning methods. Clin Teach. 2014;11(6):449–453. doi: 10.1111/tct.12191. [DOI] [PubMed] [Google Scholar]
- 7.Wynter L., Burgess A., Kalman E., Heron J.E., Bleasel J. Medical students: what educational resources are they using? BMC Med Educ. 2019;19(1):36. doi: 10.1186/s12909-019-1462-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh K., Srivastav S., Bhardwaj A., Dixit A., Misra S. Medical education during the COVID-19 pandemic: a single institution experience. Indian Pediatr. 2020;57(7):678–679. doi: 10.1007/s13312-020-1899-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abbasi S., Ayoob T., Malik A., Memon S.I. Perceptions of students regarding E-learning during Covid-19 at a private medical college. Pak J Med Sci. 2020;36 doi: 10.12669/pjms.36.COVID19-S4.2766. (COVID19-S4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hodgson J.C., Hagan P. Medical education adaptationduring a pandemic:transitioning to virtual student support. Med Educ. 2020 April 14 doi: 10.1111/medu.14177. https://onlinelibrary.wiley.com/doi/abs/10.1111/medu.14177 [DOI] [PubMed] [Google Scholar]
- 11.Moszkowicz D., Duboc H., Dubertret C., Roux D., Bretagnol F. Daily medical education for confined students during COVID-19 pandemic: a simple videoconference solution. Clin Anat. 2020 Apr 6 doi: 10.1002/ca.23601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Almarzooq Z., Lopes M., Kochar A. Virtual learning during the COVID-19 pandemic: a disruptive technology in graduate medical education. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kogan M., Klein S.E., Hannon C.P., Nolte M.T. Orthopaedic education during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28(11):e456–e464. doi: 10.5435/JAAOS-D-20-00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Atreya A., Acharya J. Distant virtual medical education during COVID-19: half a loaf of bread. Clin Teach. 2020 doi: 10.1111/tct.13185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Juliani C.M., Corrente J.E., Dell’ Acqua M.C.Q. Comparing the teaching-learning process with and without the use of computerized technological resources. Comput Inform Nurs. 2011;29:212–220. doi: 10.1097/NCN.0b013e3181f9dcb5. [DOI] [PubMed] [Google Scholar]
- 16.Bains M., Reynolds P.A., McDonald F., Sherriff M. Effectiveness and acceptability of face-to-face, blended and e-learning: a randomised trial of orthodontic undergraduates. Eur J Dent Educ. 2011;15:110–117. doi: 10.1111/j.1600-0579.2010.00651.x. [DOI] [PubMed] [Google Scholar]
- 17.Armstrong P., Elliott T., Ronald J., Paterson B. Comparison of traditional and interactive teaching methods in a UK emergency department. Eur J Emerg Med. 2009;16:327–329. doi: 10.1097/MEJ.0b013e32832b6375. [DOI] [PubMed] [Google Scholar]
- 18.Kong J., Li X., Wang Y., Sun W., Zhang J. Effect of digital problem-based learning cases on student learning outcomes in ophthalmology courses. Arch Ophthalmol. 2009;127:1211–1214. doi: 10.1001/archophthalmol.2009.110. [DOI] [PubMed] [Google Scholar]
- 19.Chu L.F., Chan B.K. Evolution of web site design: implications for medical education on the Internet. Comput Biol Med. 1998;28:459–472. doi: 10.1016/s0010-4825(98)00027-4. [DOI] [PubMed] [Google Scholar]
- 20.Kim K.J., Kang Y., Kim G. The gap between medical faculty's perceptions and use of e-learning resources. Med Educ Online. 2017;22(1):1338504. doi: 10.1080/10872981.2017.1338504. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.