Abstract
Background
Traditional teaching of medical microbiology has revolved around an organism centric, didactic lecture approach, lacking clinical relevance and appeal. Studies have shown that case-based learning in comparison to didactic lectures leads to a greater comprehension and understanding of the subject. To conduct a pilot study in our medical. College for the current MBBS batch (2019) (following the old pattern of syllabus), on student perceptions on case based learning (CBL) before the new Competency based undergraduate curriculum is rolled out for 2021 batch coming to second year of MBBS.
Methods
This pilot study was conducted at a medical college. The study was designed as an observational study on educational research and was approved by the institutional ethical committee (IEC). Study participants were second MBBS students willing to participate in the study (n = 60). Four topics were chosen to be taught as casebased scenarios as per the new CBME syllabus. Six weeks after the first CBL session was conducted, a survey questionnaire was given to the students to share their perceptions anonymously. The questionnaire had questions framed to assess the students' perception about CBL. The evaluation was done on a 5-point Likert. The responses collected were compiled in Microsoft excel sheet and the data was analysed statistically. Faculty perspective was also gathered.
Results
Majority of the students perceived CBL positively. There was a shift in the student's perspective towards the subject of microbiology, from being perceived earlier as theoretical and non-clinical to being perceived as appealing and clinically relevant.
Keywords: Case based learning, Medical education, MBBS, Microbiology
Introduction
Traditional teaching in medicine has revolved around a didactic lecture (DL) approach.1 The standard traditional method being followed in all medical colleges is the 1-h lecture format. This method has shown to be effective for knowledge transfer in a large group teaching but has inherent limitations too. Holding student's attention throughout the lecture delivery period is often challenging for the teacher. The current pattern of syllabus being followed for undergraduates in medical colleges in our country emphasizes little on the clinical and applied aspects of medical microbiology.2 Studies have shown that microbiology when taught by the case-based learning (CBL) approach leads to improved understanding and clinical comprehension of the subject.3 There has been a long-standing need for a change in the medical microbiology curriculum for some time now.4 The new competency-based medical education (CBME) being rolled out aims to make the Indian medical graduate (IMG) clinically competent and globally relevant.5,6
Traditional didactic lecture-based microbiology teaching has been generally a 1-h class where the teacher delivers the content within this time, and is often one-sided, with little participation of the students. Cognitive knowledge and theory form the basis of microbiology but an organism centered curriculum based on bacterial identification, growth, and cultural characteristics, lacks clinical connect and relevance to a medical student.7 With automation paving its way into clinical microbiology laboratories, interpreting the lab reports, understanding antibiotic resistance patterns of pathogens an emphasis on the clinical and applied aspects of disease is imperative to bridge the gap between theory and practice.8 Thus, using innovative methods to train medical students in clinical microbiology that promote problem-solving ability, enhance analytical thinking, and evoke interest in learning such as CBL should be adopted as an adjunct to various methods. We implemented CBL to the current batch before the students were sent back to their hometowns as the pandemic caused lockdown throughout the country. To integrate case-based learning (CBL) for the undergraduate medical students in microbiology. To assess the acceptability and analyse feedback of students and faculty perceptions about CBL.
Material and methods
This pilot study was conducted in a medical college setting from 2019 to 20. It was designed as an observational study on educational research and was approved by the institutional ethical committee.
Planning of the CBL sessions: Brainstorming sessions with available 6 core faculty of the department and 3 faculty from department of medicine were carried out to develop the CBL module, including the patient cases/clinical scenarios. The MCI guidelines and listed competencies and topics to be taught as clinical syndromes were followed. The principal investigator also being a medical education faculty sensitized the faculty and students of this innovation.
Defining content of the CBL module- The case content including patient history, relevant physical examination, laboratory findings and questions to be discussed were framed. Clinical case details such as case sheets, lab investigations reports, and nuances such as number of CBL sessions, timing and duration of these sessions, and the competencies to be covered were all referred to the MCI documents.
Discussion with peer faculty, for improvements and regular departmental meetings for revision of the UG CBME brought clarity about CBL sessions. Nonbiased evaluation and informal feedback were taken.
Brainstorming with undergraduate students what CBL is and how it will be conducted was done.
Implementation of the CBL module as part of CBME- Pilot study
In addition to the classroom lectures the CBL sessions were conducted.
Evaluation of performance of CBL as an innovation and adjunct to lectures: The participants were administered survey forms. Feedback from participants was taken by asking them to answer a survey form.
Feedback from Faculty who were facilitating the process was taken by asking them to answer a survey form.
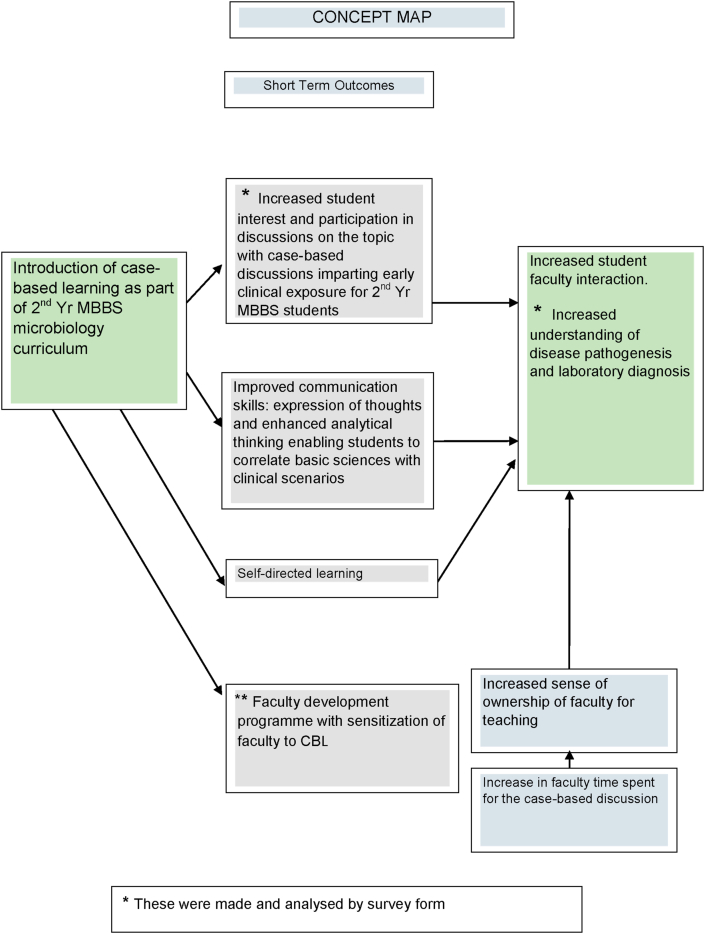
Brainstorming and informal feedback by faculty: This helped in developing the scenarios. Sensitisation of faculty was being done to roll out the new CBME curriculum, which helped in faculty development. A survey was developed to be administered to students. The study intent and likely outcomes developed and are depicted in the concept map (Fig. 1). Study participants were second MBBS students who were willing to participate in the study (n = 60).
Fig. 1.
The concept map for the study showing the short term expected outcomes.
Four topics were chosen for CBL, to be taught first as didactic lectures and then as case-based scenarios. These topics were urinary tract infection (UTI), gastrointestinal infections including cholera, central nervous system infections, and Pyrexia of unknown origin (PUO) including fever in a returned traveller. The topics were taught traditionally as an organism centric approach by a didactic one-way lecture using a power point presentation over a period of 4–5 weeks. These were then taught as syndromes with a case-based approach with student participation a week later.
Students were administered a 10-item, 5-point Likert scale survey form six weeks later, after the initial classes taken. The evaluation and the responses were rated as; 1-strongly disagree, 2-disagree, 3-neutral, 4-agree, and 5-strongly agree. They were asked to give feedback and share their perceptions anonymously. The questions were framed to assess the students' perception of CBL and the traditional way of lecture-based teaching. The responses collected were compiled in a Microsoft excel sheet and the data was analysed statistically. Also, a 10-item survey form for the faculty was developed and given to them. Both survey forms are available as supplementary material.
Results
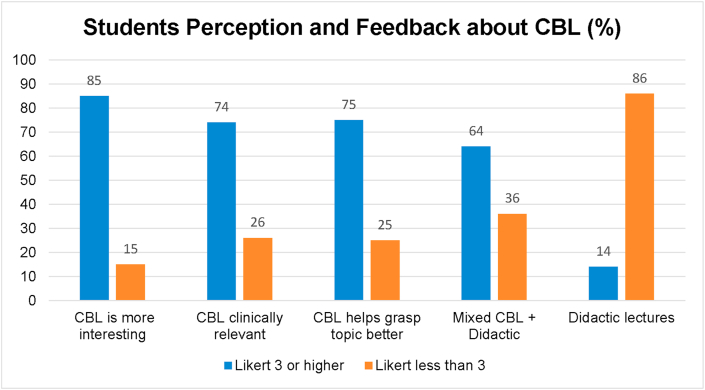
Analysis of the perception of students on CBL by quantitative feedback from 60 students was obtained. Almost 80 percent had responses higher than or equal to 3 points on the Likert Scale. About n = 51 (86%) of students agreed that CBL was an interesting way of learning microbiology than lectures. However, n = 8 (14%) preferred to be taught traditionally by lectures. A combination of traditional lectures and CBL was preferred by n = 39 (64%) and n = 45 (74%) thought that CBL improved their learning skills, n = 6 (11%) gave a neutral response (Fig. 2).
Fig. 2.
Student perceptions and feedback about CBL.
Faculty perceptions were as follows;
Initially seemed difficult, however was doable (n = 5).
It increased faculty interactions (n = 3).
Students interest and communication skills improved (n = 4).
Discussion
This was a pilot study, wherein CBL was introduced and noted to have evoked a mixed reaction from the students. As second MBBS students, their transformation into adult learners is yet to happen. To keep the students interested in the topic and to hold their attention medical teachers must adopt T-L methods which can achieve this.9
Various studies have shown evidence of the effectiveness of CBL as a T-L method in achieving defined learning objectives.10, 11, 12 Our results are similar to other studies wherein students rated CBL over lectures and found it more clinically relevant in understanding microbiology.13 CBL was found to be enjoyable in another study.14 A small percentage of students preferred didactic lectures to CBL. The majority were enthused by this novel method which engaged them, and this has also been seen by another study from United Kingdom.15 A study from India introduced CBL and reported similar results.16
Faculty perceptions and feedback: The faculty though undergoing training by the medical education department of the college was also applying it for the first time and found it time-consuming and requiring greater planning. However, for the coming batches incorporating these T-L methods is to become part of the new curriculum.
As the students had never been exposed to an activity like CBL it was observed that some students participated actively while some remained passive. While appreciating the importance of a novel method, the students in this batch preferred a combination of CBL with traditional lectures.17 Also, with the recently introduced new CBME curriculum which is soon going to be applied to the second MBBS students of 2020–21 batch, the students will get familiar with this technique and shall be motivated to participate actively. However, noting the students' preferences, and to take advantage of both these methods it would be best if a combination model of CBL and traditional lectures are used for learning in clinical microbiology as was seen in another study.18,19
CBL bridges the gap between theoretical knowledge and its clinical application for disease diagnosis.20 Cases designed in CBL provide students the details of patients such as the history of present illness, past history, clinical signs and symptoms, laboratory investigations. Students are actively involved in the discussion; interact with each other in a group and work together on the case. The instructor acts as a facilitator, steering the discussion and monitoring group dynamics, all the while ensuring that the learning objectives are being met. This highlights the clinical application of microbiology to a case and makes the subject relevant in the context of the patient. It is a teaching method that encourages students to be exposed to simulated real life like case scenarios, enhancing their analytical and thinking processes by this student-centered learning approach.21
Other student-centered learning methods include role-play, problem-based learning (PBL),22 and small group discussions to facilitate students' learning.23,24 Innovative projects involving a visit to the hospital and wards have been tried by some authours.25 CBL improves academic performance and learning outcomes however it has challenges and difficulties especially in implementing it.26
Conclusions
To make medical microbiology engaging and interesting for medical students we tried CBL as a pilot study for the students who were following the old curriculum. We conclude that the pilot study revealed CBL is appreciated by the students and in future CBL with horizontal integration may be a good strategy for arming the students with good clinical reasoning for application during their clinical rotations. With CBME curriculum being implemented CBL as an effective teaching learning tool will be of utmost relevance as an adjunct to other teaching methods.
Disclosure of competing interest
The authors have none to declare.
Acknowledgements
This article is the project work in 8th advance course in medical education. I am immensely grateful to the faculty at GSMC KEM, Mumbai for guiding steadfastly towards a greater understanding. I am indebted to all my students who participated in the study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.mjafi.2021.01.005.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Cantillon P. Teaching large groups. BMJ. 2003;326:437–440. doi: 10.1136/bmj.326.7386.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Basheer A. Competency–based medical education in India: are we ready? J Curr Res Sci Med. 2019;5(1):1–3. [Google Scholar]
- 3.Ciraj A.M., Vinod P., Ramnarayan K. Enhancing active learning in microbiology through case based learning: experiences from an Indian medical school. Indian J Pathol Microbiol. 2010;53(4):729–733. doi: 10.4103/0377-4929.72058. [DOI] [PubMed] [Google Scholar]
- 4.Williams Fraser. The place of microbiology teaching in medical curriculum. Br J Med Educ. 1969;3:206–214. doi: 10.1111/j.1365-2923.1969.tb02084.x. [DOI] [PubMed] [Google Scholar]
- 5.Gruppen L.D., Mangrulkar R.S., Kolars J.C. The promise of competency-based education in the health professions for improving global health. Hum Resour Health. 2012;10(43):1–7. doi: 10.1186/1478-4491-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Modi J.N., Gupta P., Singh T. Competency-based medical education, entrustment and assessment. Indian Pediatr. 2015;52(5):413–420. doi: 10.1007/s13312-015-0647-5. [DOI] [PubMed] [Google Scholar]
- 7.Nerurkar A.B., Dhanani J.V. Effectiveness of Project based learning in teaching microbiology to undergraduate medical students. IOSR J Res Method Educ. 2016;6(5):19–22. [Google Scholar]
- 8.Sawant A.P., Patil S.A., Vijapurkar J., Bagban N.N., Gupta D.B. Is the undergraduate microbiology curriculum preparing students for careers in their field?: an assessment of biology majors' conceptions of growth and control of microorganisms. Int J STEM Educ. 2018;5(1) doi: 10.1186/s40594-018-0138-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ronald M., Harden J.M.L. Elsevier; 2017. Essential Skills for a Medical Teacher; pp. 1–305. [Google Scholar]
- 10.Thistlethwaite J.E., Davies D., Ekeocha S. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23. Med Teach. 2012;34(6):421–444. doi: 10.3109/0142159X.2012.680939. [DOI] [PubMed] [Google Scholar]
- 11.Grover S., Garg B.S.N. Introduction of case-based learning aided by WhatsApp messenger in pathology teaching for medical students. J Post Grad Med. 2020;66:17–22. doi: 10.4103/jpgm.JPGM_2_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eissa S., Sallam R.M., Moustafa A.S., Hammouda A.M.A. Large-scale application of case-based learning for teaching medical biochemistry: a challenging experience with positive impacts. Innov Educ. 2020;2(1):1–19. [Google Scholar]
- 13.Chamberlain N.R., Stuart M.K., Singh V.K., Sargentini N.J. Utilization of case presentations in medical microbiology to enhance relevance of basic science for medical students. Med Educ Online. 2012;17(1):1–7. doi: 10.3402/meo.v17i0.15943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tarun George R.A.B.C., Abraham O.C., Tunny Sebastian M.F.F. Trainee doctors in medicine prefer case-based learning compared to didactic teaching. J Fam Med Prim Care. 2020;9:580–584. doi: 10.4103/jfmpc.jfmpc_1093_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blewett E.L., Kisamore J.L. Evaluation of an interactive, case-based review session in teaching medical microbiology. BMC Med Educ. 2009;9(1):1–9. doi: 10.1186/1472-6920-9-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garg R., Singh V. Introduction of case based learning in microbiology at undergraduate level. Natl J Lab Med. 2018;7(3):6–10. [Google Scholar]
- 17.Beylefeld A.A., Struwig M.C. A gaming approach to learning medical microbiology: students' experiences of flow. Med Teach. 2007;29(9–10):933–940. doi: 10.1080/01421590701601550. [DOI] [PubMed] [Google Scholar]
- 18.Sannathimmappa M., Nambiar V., Arvindakshan R. Implementation and evaluation of case-based learning approach in microbiology and immunology. Int J Med Res Health Sci. 2019;8(1):1–5. [Google Scholar]
- 19.Shrivastava S., Shrivastava P. Implementing case-based learning in medical colleges in India. Muller J Med Sci Res. 2018;9(2):98. [Google Scholar]
- 20.Srinivasan M., Wilkes M., Stevenson F., Nguyen T., Slavin S. Comparing problem-based learning with case-based learning: effects of a major curricular shift at two institutions. Acad Med. 2007;82(1):74–82. doi: 10.1097/01.ACM.0000249963.93776.aa. [DOI] [PubMed] [Google Scholar]
- 21.Date K., Nagdeo N., Gade S., Dashputra A. Case based learning- a method of active learning in Microbiology. J Educ Technol Health Sci. 2016;3(1):16–19. [Google Scholar]
- 22.Azer S.A. Challenges facing PBL tutors: 12 tips for successful group facilitation. Med Teach. 2005;27(8):676–681. doi: 10.1080/01421590500313001. [DOI] [PubMed] [Google Scholar]
- 23.Wood D.F. Problem based learning. BMJ. 2003;326(7384):328–330. doi: 10.1136/bmj.326.7384.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Manap A.A., Sardan N.A., Rias R.P.M. Interactive learning application in microbiology: the design, development and usability. Procedia–Soc Behav Sci. 2013;90:31–40. [Google Scholar]
- 25.Singh Suman, singh Tejinder. An innovative approach to teaching microbiology to undergraduates. Med Educ. 2009;43(11):1091–1092. doi: 10.1111/j.1365-2923.2009.03469.x. [DOI] [PubMed] [Google Scholar]
- 26.Ibrahim M., Al-Shahrani A. Implementing of a problem-based learning strategy in a Saudi medical school: requisites and challenges. Int J Med Educ. 2018;9:83–85. doi: 10.5116/ijme.5aae.2db8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.