Abstract
Background
Pheochromocytoma is a rare catecholamine-producing tumour that classically displays clinical manifestations related to alpha-adrenergic stimulation, including paroxysmal or sustained hypertension. However, it may occasionally be complicated by life-threatening crisis, leading to refractory acute heart dysfunction in the most severe cases.
Case summary
A 28-year-old woman was admitted to intensive care unit due to hypertensive crisis causing pulmonary oedema, Takotsubo cardiomyopathy, and metabolic acidosis. Due to cardiogenic shock, she required venoarterial extracorporeal membrane oxygenation and IMPELLA implantation. A computed tomography scan revealed a 5 cm tumour of the left adrenal gland compatible with pheochromocytoma The clinical course was complicated by acute kidney injury requiring renal replacement therapy and posterior reversible encephalopathy syndrome (PRES). Pharmacological treatment with alpha lityc agents (including urapidil, dexmedetomidine, and doxazosin at maximum daily dose) and beta blockers, together with left videolaparoscopic adrenalectomy, led to progressive blood pressure control and resolution of the neurological symptoms.
Discussion
Pheochromocytoma crisis turned into a potential catastrophic scenario, characterized by refractory cardiogenic shock requiring circulatory supportive devices and PRES. Alpha-antagonists and beta-blockers were the gold standard pharmacological treatment. A multidisciplinary decision-algorithm was necessary to successfully manage this complex clinical setting.
Keywords: Pheocromocytoma, Cardiogenic shock, Posterior reversible encephalopathy syndrome, Alpha lityc treatment, Case report
Learning points
Pheochromocytoma crisis is a rare but potentially life-threatening condition.
The gold standard pharmacological treatment encompasses the use of alpha-antagonists and beta-blockers.
In cases of cardiogenic shock refractory to medical treatment, the use of venoarterial extracorporeal membrane oxygenation (together with IMPELLA) may be effective.
Introduction
Pheochromocytoma is a rare neuroendocrine tumour that produces and stores adrenaline and noradrenaline.1,2 It usually presents with symptoms related to catecholamines excess, including palpitations, paroxysmal or sustained hypertension, headache, anxiety, fatigue. The severity of these symptoms is extremely variable and depends on the genetics of the tumour itself.3 Pheochromocytoma may occasionally be complicated by acute respiratory distress syndrome, catecholamine-induced cardiomyopathy, and unexplained or intractable cardiogenic shock.4
We report the case of a complex pheochromocytoma requiring a multidisciplinary decision-algorithm to successfully solve a potential catastrophic scenario.
Timeline
| Before admission | Short-lasting episodes of palpitations |
|---|---|
| 27 July 2019 (Day 1) |
Admission to the emergency department (ED): hypertensive crisis (230/110 mmHg) complicated by pulmonary oedema, type II myocardial infarction with low left ventricular ejection fraction (LVEF) and diffuse akinesia, metabolic acidosis Intubation and transfer to a II level ED Implant of venoarterial extracorporeal membrane oxygenation (VA ECMO) and IMPELLA due to cardiogenic shock Diagnosis of Takotsubo cardiomyopathy Admission to the cardiothoracic intensive care unit |
| 28 July 2019 (Day 2) | Acute kidney injury requiring renal replacement therapy (RRT) |
| 29 July 2019 (Day 3) |
Right hemiplegia Total body computed tomography: bilateral parieto-occipital ischaemic areas; hypodense subcortical area in the left frontal lobe; 5 cm tumour of the left adrenal gland (pheochromocytoma) |
| 30 July 2019 (Day 4) |
VA ECMO removal Episodes of hypertensive crisis treated with alpha lityc agents (urapidil) and beta blockers |
| 31 July 2019 (Day 5) | IMPELLA removal |
| 1 August 2019 (Day 6) | Diagnosis of pheochromocytoma confirmed by high levels of plasmatic catecholamines and endomyocardial biopsies suggesting catecholamine-induced cardiomyopathy |
| 2 August 2019 (Day 7) | Magnetic resonance imaging confirming posterior reversible encephalopathy syndrome diagnosis |
| 5 August 2019 (Day 10) |
Transfer to the Department of Shock and Trauma Blood pressure control through alpha lityc agents (including dexmedetomidine and doxazosin at maximum daily dose) and beta blockers |
| 13 August 2019 (Day 18) |
Left videolaparoscopic adrenalectomy Discontinuation of doxazosin treatment and RRT |
| 14 August 2019 (Day 19) | Extubation |
| 22 August 2019 (Day 27) | Discharge from the Department of Shock and Trauma with no residual neurological deficit |
| 25 August 2019 (Day 30) | Discharge from hospital. Complete recovery of LVEF |
Case presentation
An Italian Caucasian 28-year-old woman was transported by ambulance to the emergency room (ER) on 27 July 2019, due to sudden and progressive dyspnoea, epigastric pain, and palpitations occurring while she was at the beach. The patient denied relevant pathological medical history except for short-lasting episodes of palpitations. She was on no regular medication and denied substance abuse.
Early medical examination in the ER revealed paleness, cold sweat, epistaxis, and signs of pulmonary oedema due to a new-onset atrial fibrillation with rapid ventricular response (170 b.p.m.); blood pressure (BP) was 230/110 mmHg and SpO2 was 96%.
Blood tests revealed leucocytosis, hyperglycaemia (309 mg/dL—normal range 70–110 mg/dL) and troponin T elevation (151 ng/L—normal range 0–14 ng/L). Blood gas analysis showed metabolic acidosis. Electrocardiogram revealed ST-segment depression in the lower lateral leads. Transthoracic echocardiogram (TTE) was performed too, showing 33% left ventricular ejection fraction (LVEF) with diffuse akinesia.
The patient was sedated, intubated and mechanically ventilated. Polypharmacological therapy, including amiodarone, bisoprolol, nitroglycerine, furosemide, ticagrelor, acetylsalicylic acid, heparin, ceftriaxone, and pantoprazole was started.
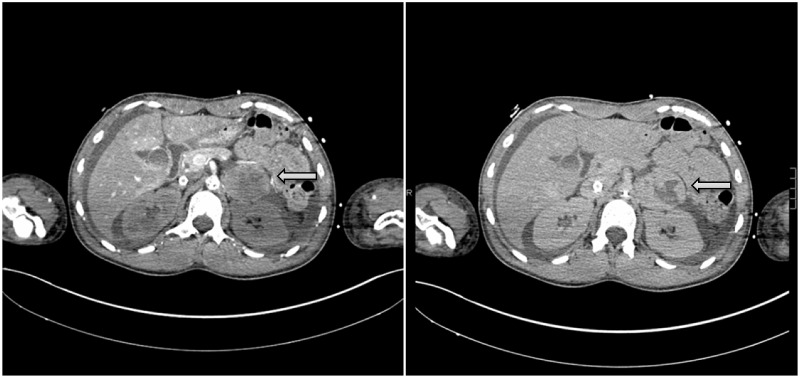
The patient was subsequently transferred to a II level emergency department. At her arrival, she presented with anisocoria, BP was 220/100 mmHg, heart rate was 160, and SpO2 was 74%. Blood gas analysis showed persistent severe metabolic acidosis with elevated lactate levels (5.8 mmol/L—normal value <2 mmol/L). A new TTE was performed, showing 20–30% LVEF. Chest X-ray revealed bilateral symmetrical and diffuse alveolar opacities (Figure 1).
Figure 1.
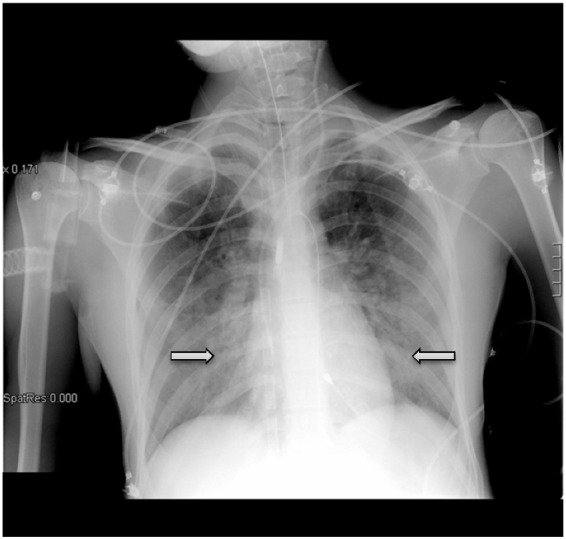
Chest X-ray showing bilateral symmetrical and diffuse alveolar opacities.
Given the sustained hypertension (mean arterial pressure 140 mmHg), despite sedation and maximal pharmacological therapy, resulting in progressive haemodynamic impairment with low ejection fraction, severe pulmonary oedema, and metabolic acidosis, the patient underwent urgent venoarterial extracorporeal membrane oxygenation (VA ECMO) in the cath lab. Coronary angiography did not show any coronary artery stenosis. A percutaneous left ventricular assist device (IMPELLA) was implanted. Three endomyocardial biopsies were obtained, subsequently turning out to be negative for myocarditis but suggestive of catecholamine-induced cardiomyopathy. The patient was then admitted to the cardiothoracic intensive care unit.
In the following day, she developed thrombocytopenia (platelet count of 33000 plt/mm3—normal range 150 000–450 000 plt/mm3) and acute kidney injury requiring renal replacement therapy (RRT).
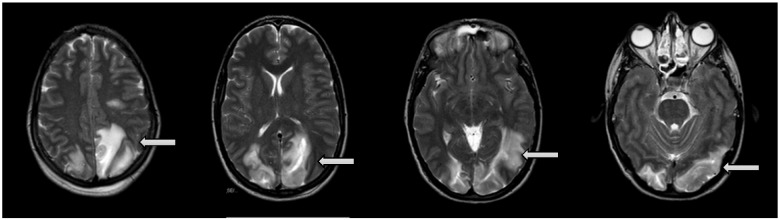
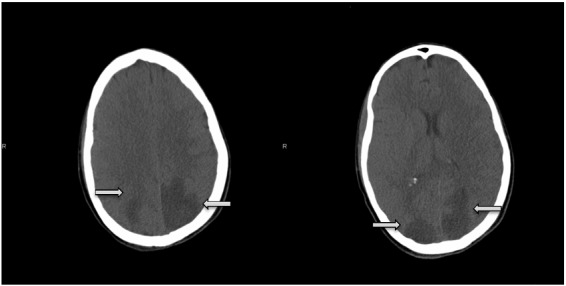
On 29 July, sedation was transiently stopped. Neurological evaluation revealed right hemiplegia. Cerebral computed tomography (CT) scan showed hypodense (ischaemic) bilateral parieto-occipital areas and a hypodense subcortical area in the left frontal lobe (Figure 2). Abdominal CT scan revealed a 5 cm tumour of the left adrenal gland compatible with pheochromocytoma (Figure 3).
Figure 2.
Cerebral computed tomography scan showing hypodense (ischaemic) bilateral parieto-occipital areas and a hypodense subcortical area in the left frontal lobe.
Figure 3.
Abdominal computed tomography scan revealing a 5 cm tumour of the left adrenal gland compatible with pheochromocytoma.
On 30 and 31 July, ECMO and IMPELLA were respectively removed, due to a gradually recovery of the LVEF. Hypertensive crisis and episodes of atrial fibrillation were treated with urapidil, esmolol, and amiodarone. CT scan was repeated confirming the previous findings.
As it was not possible to determine urinary metanephrines due to the ongoing RRT, on 1 August, plasmatic catecholamines were dosed, showing increased adrenaline and noradrenaline levels and therefore confirming pheochromocytoma diagnosis.
On 2 August, magnetic resonance imaging of the brain confirmed the presence of bilateral parieto-occipital ischaemic lesions of recent onset. Ischaemic lesions of the right cerebellum, right centrum semiovale and left frontal subcortical region where also found. Intense vasogenic oedema accompanied these lesions (Figure 4), thus suggesting the diagnosis of posterior reversible encephalopathy syndrome (PRES).
Figure 4.
Magnetic resonance imaging (T1 and T2 sequences; diffusion MR study) showing bilateral parieto-occipital ischaemic lesions of recent onset. Ischaemic lesions of the right cerebellum, right centrum semiovale and left frontal subcortical region can also be observed. Vasogenic oedema accompanies these lesions. These radiological findings, together with a right hemiplegia of new onset, are suggestive of posterior reversible encephalopathy syndrome (PRES).
On 5 August, the patient was transferred from the cardiothoracic intensive care unit to the Department of Shock and Trauma of the same hospital. Neurological evaluation showed persistence of the right hemiplegia. She was still sedated, intubated and mechanically ventilated. Sedation with sufentanil, propofol, and dexmedetomidine improved BP control. Moreover, antihypertensive therapy with doxazosin 16 mg/day and labetalol by continuous intravenous infusion was started, leading to rapid BP and heart rate control. Due to persistent oligo anuria, RRT was continued.
The following days, haemodynamic stability was reached: labetalol infusion was stopped and doxazosin administration was reduced up to 4 mg × 2/day.
On 13 August, left videolaparoscopic adrenalectomy was performed. Histological analysis confirmed the diagnosis of pheochromocytoma. The same day, doxazosin treatment was stopped. On 14 August, the patient was extubated. She was discharged from our department on 22 August. She was conscious; no residual focal deficit could be detected at neurological examination. She was breathing spontaneously. RRT had been stopped due to autonomous diuresis.
On 25 August, she was discharged from hospital. TTE was repeated before discharge, revealing complete recovery of left ventricular systolic function (LVEF 58%). Grade I diastolic dysfunction persisted, as suggested by E/A reversal (ratio < 1.0).
Discussion
Pheochromocytoma crisis is a rare condition but can be potentially life threatening due to cardiovascular complications.
Several mechanisms have been proposed to explain the pathophysiology of cardiovascular failure, including coronary vasospasm caused by alpha-1 stimulation (also known as Takotsubo cardiomyopathy),5 increased myocardial oxygen demand due to tachycardia and high afterload, and direct myocytotoxic effect of increased level of catecholamines.6
Managing pheochromocytoma crisis may be challenging. Alpha-antagonists and beta-blockers are the gold standard pharmacological treatment, but their administration in patients with hemodynamic instability may raise some concerns. Moreover, high endogenous levels of catecholamines may induce sympathetic receptor down-regulation. Vasopressors and inotropes usually used to manage cardiogenic shock (including adrenaline, noradrenaline, and dobutamine) could be less effective, or even exacerbate pheochromocytoma-induced heart dysfunction.7 Since myocardial stunning caused by catecholamines excess is mostly reversible,8 if managed properly, the use of circulatory supportive devices have been shown to be effective in those cases refractory to medical treatment.9
Several studies have reported the successful use of VA ECMO to rescue patients with severe cardiopulmonary failure in a wide spectrum of different aetiologies, including acute myocardial infarction, post-cardiotomy shock, drug intoxication, and acute fulminant myocarditis.10,11 However the use of VA ECMO in pheochromocytoma-induced cardiogenic shock is still a matter of debate and only described in case reports or single-centre studies. Recently, a systematic review investigated the role of VA ECMO in 62 patients with pheochromocytoma-induced cardiogenic shock.12 The authors concluded that VA ECMO may allow cardiac and end-organ recovery also in this specific setting, giving time for accurate diagnosis and specific treatment.
Percutaneous active mechanical circulatory support, including IMPELLA, may also be combined with VA ECMO to decrease left ventricular pressure and improve outcomes.13
In the case, we report, VA ECMO, together with IMPELLA, were used as first-line therapy in the setting of cardiogenic shock. By providing prompt cardiac and circulatory support, they were utilized as a bridge to weaning after cardiac function recovery. Of course, it was of pivotal importance centralizing the patient to a II level emergency department to allow life-saving devices to be implanted.
Pheochromocytoma crisis led to the early occurrence of a PRES too. PRES is a clinical and radiological disease, characterized by subcortical vasogenic brain oedema involving the parieto-occipital region of the brain and causing acute neurological deficits. Although its pathophysiology is not clear, acute cerebral endotheliopathy might be triggered by severe hypertension (exceeding the threshold of cerebral autoregulation), endogenous or exogenous toxins, or neuropeptides (causing severe cerebral vasoconstriction and spasms).14 In order to be reversible, PRES requires early diagnosis and treatment. Anti-hypertensive treatment should aim for BP relative reduction of 20–30% in the first hours after onset according to hypertensive crisis guidelines.15
In the case, we report, alpha lityc agents were the cornerstone of the pharmacological treatment. Hypertensive crisis were treated first with urapidil; subsequently, doxazosin was started at maximum daily dose (16 mg) and then deescalated. Sedation with an alpha lityc agent (dexmedetomidine) contributed to BP control.
Haemodynamic stabilization was mandatory for surgical planning too. The main goal was to minimize the risk of adverse events related to catecholamine-induced haemodynamic fluctuations during anaesthesia and surgical tumour manipulation.16 Left videolaparoscopic adrenalectomy was performed 7–10 days from the beginning of the alpha lityc treatment, in order to ensure the safety of the surgical procedure.
In conclusion, pheochromocytoma is a rare but potentially life-threatening tumour. The complex and challenging case we presented highlights the importance of a multidisciplinary approach, involving intensive care physicians, radiologists, cardiologists, and surgeons, in order to set, handle and solve a clinical scenario burned by a high mortality rate.
Lead author biography

Cristina Dominedò graduated from the University ‘La Sapienza’ of Rome (Italy) in 2013. In 2019, she completed her residency in Anesthesiology and Intensive Care Medicine at the Agostino Gemelli Hospital, Catholic University of the Sacred Heart, Rome (Italy). During her residency, she performed a Clinical Research Fellowship at the Respiratory Intensive Care Unit of the Hospital Clinic of Barcelona (Spain). She is currently working at the Department of Shock and Trauma, San Camillo Forlanini Hospital, Rome (Italy). She has a particular research interest in cardiogenic shock and hemodynamic monitoring.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Funding: none declared.
Supplementary Material
References
- 1. Kopetschke R, Slisko M, Kilisli A, Tuschy U, Wallaschofski H, Fassnacht M. et al. Frequent incidental discovery of phaeochromocytoma: data from a German cohort of 201 phaeochromocytoma. Eur J Endocrinol 2009;161:355–361. [DOI] [PubMed] [Google Scholar]
- 2. Fassnacht M, Arlt W, Bancos I, Dralle H, Newell-Price J, Sahdev A. et al. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol 2016;175:G1–g34. [DOI] [PubMed] [Google Scholar]
- 3. Naranjo J, Dodd S, Martin YN.. Perioperative management of pheochromocytoma. J Cardiothorac Vasc Anesth 2017;31:1427–1439. [DOI] [PubMed] [Google Scholar]
- 4. Cambos S, Tabarin A.. Management of adrenal incidentalomas: working through uncertainty. Best Pract Res Clin Endocrinol Metab 2020;34:101427. [DOI] [PubMed] [Google Scholar]
- 5. Casey RT, Challis BG, Pitfield D, Mahroof RM, Jamieson N, Bhagra CJ. et al. Management of an acute catecholamine-induced cardiomyopathy and circulatory collapse: a multidisciplinary approach. Endocrinol Diabetes Metab Case Rep 2017;2017:17–0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Simons M, Downing SE.. Coronary vasoconstriction and catecholamine cardiomyopathy. Am Heart J 1985;109:297–304. [DOI] [PubMed] [Google Scholar]
- 7. Cohen CD, Dent DM.. Phaeochromocytoma and acute cardiovascular death (with special reference to myocardial infarction). Postgrad Med J 1984;60:111–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wu GY, Doshi AA, Haas GJ.. Pheochromocytoma induced cardiogenic shock with rapid recovery of ventricular function. Eur J Heart Fail 2007;9:212–214. [DOI] [PubMed] [Google Scholar]
- 9. Whitelaw BC, Prague JK, Mustafa OG, Schulte KM, Hopkins PA, Gilbert JA. et al. Phaeochromocytoma [corrected] crisis. Clin Endocrinol 2014;80:13–22. [DOI] [PubMed] [Google Scholar]
- 10. Alba AC, Foroutan F, Buchan TA, Alvarez J, Kinsella A, Clark K. et al. Mortality in patients with cardiogenic shock supported with veno-arterial extracorporeal membrane oxygenation: a systematic review and meta-analysis evaluating the impact of etiology. J Heart Lung Transplant 2020;39:S186. [DOI] [PubMed] [Google Scholar]
- 11. Pineton de Chambrun M, Bréchot N, Combes A.. Venoarterial extracorporeal membrane oxygenation in cardiogenic shock: indications, mode of operation, and current evidence. Curr Opin Crit Care 2019;25:397–402. [DOI] [PubMed] [Google Scholar]
- 12. Matteucci M, Kowalewski M, Fina D, Jiritano F, Meani P, Raffa GM. et al. Extracorporeal life support for phaeochromocytoma-induced cardiogenic shock: a systematic review. Perfusion 2020;35:20–28. [DOI] [PubMed] [Google Scholar]
- 13. Patel SM, Lipinski J, Al-Kindi SG, Patel T, Saric P, Li J. et al. Simultaneous venoarterial extracorporeal membrane oxygenation and percutaneous left ventricular decompression therapy with Impella is associated with improved outcomes in refractory cardiogenic shock. ASAIO J 2019;65:21–28. [DOI] [PubMed] [Google Scholar]
- 14. Liman TG, Siebert E, Endres M.. Posterior reversible encephalopathy syndrome. Curr Opin Neurol 2019;32:25–35. [DOI] [PubMed] [Google Scholar]
- 15. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018;138:e426–e483. [DOI] [PubMed] [Google Scholar]
- 16. Patel D. Surgical approach to patients with pheochromocytoma. Gland Surg 2020;9:32–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.