Abstract
COVID-19 disease caused by the SARS-CoV-2 virus has had serious adverse effects globally in 2020 which are foreseen to extend in 2021, as well. The most important of these effects was exceeding the capacity of the healthcare infrastructures, and the related inability to meet the need for various medical equipment especially within the first months of the crisis following the emergence and rapid spreading of the virus. Urgent global demand for the previously unavailable personal protective equipment, sterile disposable medical supplies as well as the active molecules including vaccines and drugs fueled the need for the coordinated efforts of the scientific community. Amid all this confusion, the rapid prototyping technology, 3D printing, has demonstrated its competitive advantage by repositioning its capabilities to respond to the urgent need. Individual and corporate, amateur and professional all makers around the world with 3D printing capacity became united in effort to fill the gap in the supply chain until mass production is available especially for personal protective equipment and other medical supplies. Due to the unexpected, ever-changing nature of the COVID-19 pandemic—like all other potential communicable diseases—the need for rapid design and 3D production of parts and pieces as well as sterile disposable medical equipment and consumables is likely to continue to keep its importance in the upcoming years. This review article summarizes how additive manufacturing technology can contribute to such cases with special focus on the recent COVID-19 pandemic.
Keywords: COVID-19, 3D printing, Additive manufacturing, Rapid prototyping, Protective equipment, Diagnosis, Therapeutic devices
Introduction
SARS-CoV-2 virus emerged in Wuhan, China, in December 2019, and spread rapidly to all parts of the country followed by a fast global distribution [1, 2], reaching to over 90 million confirmed cases and ca. 2 million confirmed deaths as of January 2021 [3]. Despite the fact that pandemics have been encountered before in history, it turned out that the world was not prepared for it. One of the main reasons for that is the rapid spread of the threat due to the disappeared borders and ease of travelling to all parts of the world with today’s technology [4–6].
The realization that the virus was spreading rapidly and that it was transmitted between people [4], immediately followed by the realization that its negative effects on human health were more harmful than the commonly encountered viral infections (and even fatal) [7–9], caused a global panic. People all over the world have begun to ask and seek answers to many questions about the nature of this disease [10, 11]. Is there a cure? What are the prevention methods? How fast and what kind of measures should be taken?
Scientific community responded quickly in order to find urgent solutions to meet the needs of the whole world. One of the important factors that put the health services of countries into difficulty is the lack of personal protective equipment, drugs, and vaccines to protect from and to cure the coronavirus disease (COVID-19) [12]. Significant problems have been experienced in procuring many medical materials that are easy to design and manufacture, and bottlenecks have occurred in the supply of sterile disposable consumables needed in health institutions [13, 14]. The importance of three-dimensional (3D) printing technology became evident in these cases with its capacity to produce fast solutions especially in the early days of the pandemic [15]. For example, the COVID-19 outbreak has led to the need to intubate large numbers of patients simultaneously in hospitals, emerging studies to quickly design and fabricate valves for differential multi-ventilation with 3D printing [16]. Several other urgent fabrication requirements for medical devices including face shields and masks [17], powered respirators [18], and surgical helmets [19] were also studied by 3D printing approach. The production of single-use, sterile medical devices, device parts, and accessories has become a great need to eliminate the need for sterilization for re-use, which is possible with the rapid response of 3D printing technology [20, 21]. It can be envisioned that similar rapid 3D design and manufacture approaches with additive manufacturing will be required for other medical equipment, as well, in the near future with the actively changing nature of the pandemic.
What is additive manufacturing?
The third industrial revolution covers the period starting from the first half of the twentieth century to the end of it [22]. The major development of Industry 3.0 was the use of computer numerical control (CNC) machines which enabled processing of materials in many different sizes and numbers. A CNC equipment is basically a computer controlled sculptor, which produces 3D objects by removing parts from a solid block, performing a subtractive manufacturing with top-down approach [23]. During the cutting and shaping of very complex structures with CNC, there may be a loss of detail in the product due to the limited 3D movement of the cutting tip [24]. Additive manufacturing, on the other hand, is a bottom-up approach and is working with the principle of manufacturing 3D objects in a layer-by-layer approach. This technique has been in use since the beginning of 1980s, mostly in the production of small and complex machine parts [25]. The technique was also—more commonly—referred to as rapid prototyping, since the major utility was to create prototypes for the industrial applications rapidly. Medical 3D printing has emerged as a more recent tool, basically following the development of 3D printable biocompatible polymeric materials [26]. Today, it is possible to manufacture any shape with complex 3D geometry by 3D printing technique in the fastest possible manner, compared with traditional manufacturing techniques such as molding.
Creating the 3D model required for 3D printing is the first step of the workflow. 3D model design can be done in three different ways. The first of these is to create a free design. Detailed design of any 3D object can be realized, and it can be converted to the .stl file type required for 3D printing and transferred to 3D printers [27]. Another way to create a 3D model is 3D scanning. High-dimensional precision is obtainable with 3D scanning of existing products, and reverse engineering can be done to prepare the 3D model required for the 3D printing process [28]. A different way to create a 3D model is to segment DICOM files of the radiological images obtained from the patient with computed tomography or MRI and use softwares to reconstruct the cross-sectional images into 3D designs by the process of 3D rendering (surface rendering) [29]. 3D models produced from DICOM images by this way are obtained as the .stl file and are loaded into the 3D printer software and can be used in 3D printing.
After creating a 3D model, production is carried out by 3D printing technique. 3D printing is the general name of additive manufacturing methods that involve the production of any structure in a layer-by-layer form with material accumulation from the bottom to the top. 3D printing can be performed in various ways. Among these, fused deposition modeling (FDM) technology is often preferred. In 3D production with this method, the material leaves a syringe tip to form a filament and is deposited on top of each other in a layer-by-layer manner [30].
Stereolithography (SLA) method is another method of 3D printing. In this method, unlike the FDM method, layered production is not carried out by filament deposition, but by curing the resin with light, thus forming the complex structure with cured resin layers deposited on top of each other [26]. The resolutions of SLA 3D printers are much higher than FDM printers, and layer smoothness can be achieved. It is the preferred production method for more detailed, sensitive, and complex product production. Selective laser sintering (SLS) is another common 3D printing technique where material powder is sintered by laser in a layer-by-layer fashion to produce the final 3D object [26].
Why additive manufacturing is needed in the rapid communicable disease prevention and control
Prototype manufacturing and mass production conditions are different from each other. 3D printing provides a fast production line although with limited capacity and higher manufacturing cost. For example, in the production of a holder for a visor of a face shield which had great importance at the commence of the pandemic when mass production was not available, a piece of such holders can be produced in 25–50 min with a 3D printer, while 2–3 parts per minute can be produced with plastic injection molding technology under mass production conditions. When it comes to single-use products, it is obvious that the need will be at the level of “thousand pieces” and that the design should be made in accordance with mass production in order to keep the production speed to the need. Therefore, 3D printing technology will remain its importance in the fast production of pieces that emerge according to the rapidly changing needs of the healthcare institutions during the pandemic.
Preventive applications of 3D printing during the pandemic
The use of 3D-printed masks and shields are the focus group which underlines the priority selection made according to the rising demands of Personal Protective Equipments (PPE). The summary provided here shows the most general approach for the production of apparatus by dividing into three main design types and gives an idea of how they are being produced and explains the effectiveness of use.
By the help of computer-aided software design, the virtual model obtained and after some desired modifications, the model is saved in a special format called STL. The file is transferred to a different program type called slicer and turns into a “gcode” which is the ready to print format that the 3D printing equipment recognizes to build the part. 3D printing can be done with various approaches as explained earlier. In the case of PPE production, medical safety becomes an important factor. PPE produced by SLA or SLS techniques use resin or petroleum-based plastic powders to fabricate the product. Therefore, products produced by these approaches may necessitate the use of additional layers of protective medical grade coatings to the part to prevent hazards of skin contact for human use. This concern brings the FDM approach as a more useful tool as, in the most practical form, it operates with a biocompatible material (poly(lactic acid), PLA) filament. Frequently used nylon filaments are also options for production of more elastic parts if necessary. Most of the studies show that is a cost-efficient, relatively fast and reliable method chosen for such urgent circumstances [31]. The FDM 3D printers also use commercially available acrylonitrile butadiene styrene (ABS) filament which is a convenient material selection for the production of face shields and snorkel adapters as being very rigid [32].
Face masks
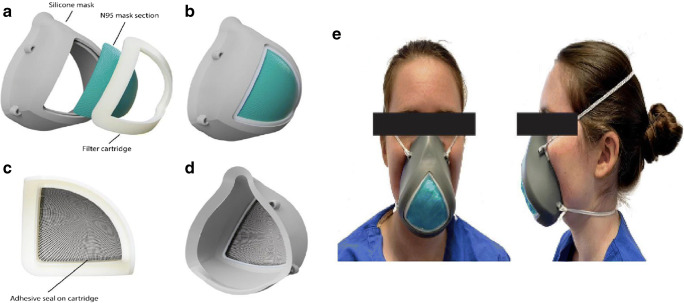
3D-printed face masks consist of two main parts, the strap and the filter membrane support. The particle filter is disposable and it can be replaced after prolonged use in contaminated environments (Fig. 1). The 3D-printed support should fit nicely onto the users’ face, so in most studies, 3D scanning techniques are used like shown below (Fig. 2, left panel) [34]. Another study was conducted in Stanford University, where the production of a 3D printed part to hold a N95 mask filter in place was fitted into a silicone housing (Fig. 2, right panel) [35].
Fig. 1.
a Labeled exploded render of the final mask design with a reusable soft silicone base and a 3D printed filter cartridge, b Front view of the final mask assembly, c The cartridge is assembled separately with one-quarter of a 3 M 1860 N95 mask and adhesive to ensure a seal on the edges of the filter, d Back view of the final mask assembly, e The use on the model [Adapted from 33]
Fig. 2.
Left panel: Custom-made, individualized 3D printed protective face mask. a Reusable 3D printed face mask, b Filter membrane support, c Polypropylene (PP) non-woven melt-blown particle filter, d 3D image of the prototype [Adapted from 34]. Right Panel: Clinical right facial profile views of a sterilization nurse, providing an overview and comparison of the fit of a custom-made 3D printed face mask with commercially available masks. a A disposable surgical face mask (BARRIER Medical face mask; Molnlycke Health Care, Goteborg, Sweden), b A disposable FFP2 face mask (KN95 respirator mask; CTT Co., Ltd, Guangdong, China), c a disposable FFP3 face mask (FFP3 NR D Respiratory Protection Mask; Zekler Safety, Ulricehamn, Sweden), d 3D facial, and e clinical images of the 3D printed face mask, f In combination with protection glasses and a face shield. Note the proper clinical fit of the 3D printed face mask [Adapted from 32].
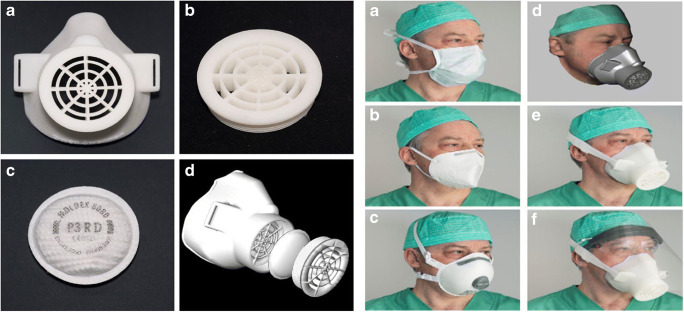
Face shields
While the shields are not providing a full protection, they are good additional options as barriers, especially for the aerosol producing cases to reduce the risk of contamination [36]. A face shield is simple in its construction consisting of three parts: the frame, an elastic band for fastening, and a clear plastic visor. It is needed to fulfill the following parameters: fast production, easy disinfection, and end user comfort. The plastic visor can be any clear plastic sheet. An example for the production and assembly is the use of poly(vinyl chloride) (PVC) film sheets and stiff overhead projector (OHP) sheets [36]. The PVC film was chosen due to its soft and ductile nature which can provide a greater degree of protection during procedures such as wound care, dress change, and traction involving the airway at triage. In Fig. 3, an example is presented in which the frame was 3D printed from PLA. The face shields can be re-used by replacing the clippers and the PVC film. It is advised to discard the paper or binder clips after a cycle of use; however, in situations requiring reuse, they can be disinfected using an EPA-registered hospital disinfectant solution [36].
Fig. 3.
Face shield frame designed as end user feedback and the final assembly [Adapted from 35].
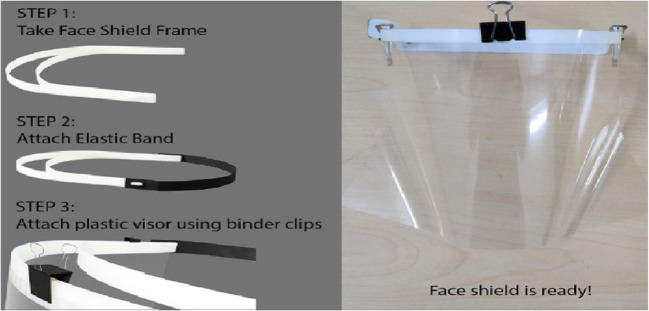
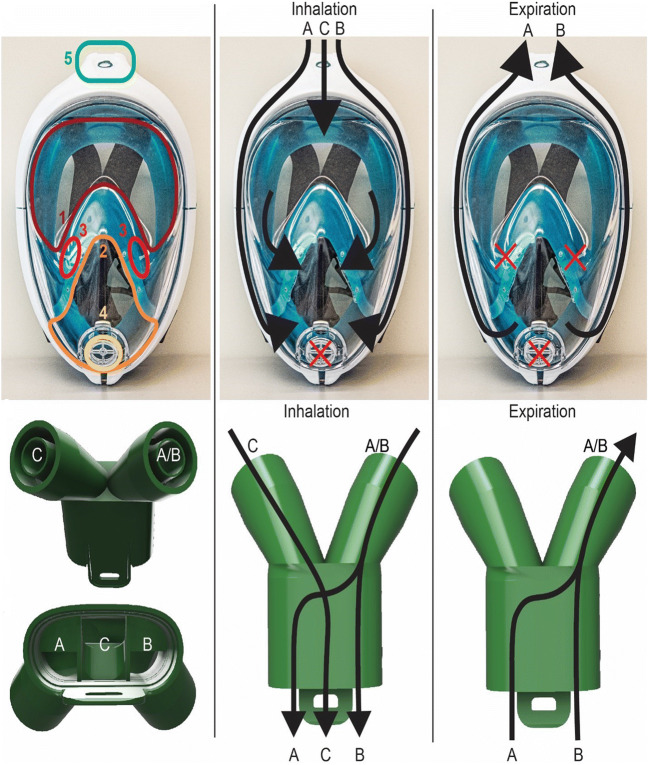
Snorkels as full protection masks
Full mask use is a mandatory case for high contaminated areas, and the level of protection should be high enough to ensure the healthy breathing of the medical staff. The theoretical advantages of using such masks instead of an assembly of oro-nasal protection mask and protective goggles are the ease of use, reusability, and possibly better wearer comfort. Possible disadvantages could be insufficient protection level, increased work of breathing, carbon dioxide accumulation, reduced communication, and fogging of the face shield [37]. The nature of 3D printing has its own limitations so that construction of a full mask out of plastic is not sustainable in terms of printing speed, cost, and effectiveness. Already in use molded silicone sealed diving masks seemed to be the best and most practical alternative. Modification for the special needs of the pandemic was the required additional design. The 3D printers came into play with the adapters fitted on the snorkel part of the mask or the air exiting diaphragms for this adaptation. The adapters have two main uses of oxygen supply and air filtering. PLA or resin materials were chosen for safety precautions. The space margins were filled with an adhesive of the plastic tubes or transition points in between different material types used on the design. With proper adjustment and the utilization of connectors, the mask can be converted into an oxygen supply device and a nebulizer aerosol therapy device as well [38, 39]. Figure 4 presents an example of 3D-printed changing valve design for healthy breathing [40].
Fig. 4.
Inhale and exhale 3D-printed valve design for healthy breathing [Adapted from 39]
3D printing in the diagnosis of COVID-19
During the pandemic, diagnosis of COVID-19 is based on two main elements that include determination of the presence of the virus and describing the signs or symptoms of the disease. Collection of swab samples from nose and throat, laboratory tests, and medical imaging of the affected organs are the main steps in this context. At this point, rapidly produced, cheap, and easy to sterilize—or disposable—medical tools obtained with 3D printers have gained importance. 3D-printed nasopharyngeal swabs [40–42] have been the most frequently produced tools for the diagnosis of COVID-19. In addition, design and 3D printing of testing tubes [43]; rapid diagnostic kits such as PCR, ELISA, and CRISPR components [44–46]; and 3D printable organ models [47] are continuing.
A nasopharyngeal swab is a diagnostic method for collecting a sample of nasal secretions from the back of the nose and throat. These are FDA Class I medical devices [42, 48] constitutes a stick made of a short plastic rod that is covered, at one tip, with adsorbing material such as cotton, polyester, or flocked nylon depending on whether they are fiber or flocked [49]. Since some materials such as wood or cotton inhibit PCR reactions, cotton head swabs are not indicated for COVID-19 [49–51]. Therefore, a large quantity of non-cotton swabs were needed at the beginning of the pandemic to increase the number of scans. 3D printing has emerged as an alternative and effective production technology that can be used in this direction [40, 50]. Nasopharyngeal swabs produced with a 3D printer must be biocompatible, flexible, and easy to sterilize. For validation testing, swabs also need to ensure that it could gather enough viral cells and hold them up and the production material would not interfere with test results [40–42].
One of the most successful initiatives to design and production of nasal swabs by using 3D printing was the model developed in the Division of 3D Clinical Applications at the University of South Florida’s (USF) Department of Radiology in partnership with USF Health and Northwell Health’s 3D Design and Innovation lab. This production was conducted using an SLA printer (Formlabs form 2 or 3B) by using Surgical Guide version I resin and then washed and cured prior to being sent for sterilization with autoclave [40, 50] (Figure 5). Once the bench-lab testing was conducted and completed, the clinical effectiveness of the created final design was performed at Tampa General Hospital and Northwell Health Clinic. In the trials conducted in both clinics, it was observed that there was statistically 94% compatibility between the 3D-printed swab and the synthetic flocked swab. Custom-designed more rigid brush-like head of 3D printed swab likely collected additional epithelial cells which may increase sensitivity in sample collections compared to the standard flocked nasopharyngeal swabs [40, 50]. Both hospitals concluded that the 3D printed swab provides a cost efficient, safety, and fast alternative to synthetic swab and can be used as standard [40, 50].
Fig. 5.
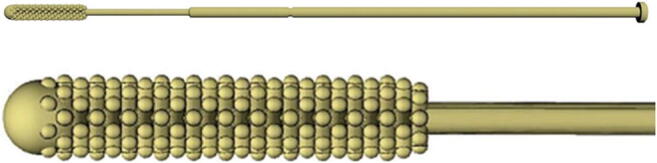
Computer-aided drawing (CAD) of NP swab, consisting roughly of a 150 mm in total length with a 70 mm breakpoint. The tip length is 15 mm long, with a diameter of 3.85 mm. The tip has a rounded nose for patient comfort. The neck is 1.5 mm in diameter and the shaft is 2.45 mm in diameter. The base is 1.75 mm long with a 5-mm diameter [Adapted from 39]
Callahan et al. [51] made a multi-step preclinical evaluation and validation of some prototypes. From this study, a consortium including Carbon, FormLabs, Envisiontec, Origin and Abiogenix companies was created that have a capability for producing FDA-registered test swabs. Cox and Koepsell [52] created a PETG nasopharyngeal swab. Arnold et al. [53] developed a swab with an open lattice design to be produced by DLP process. Resolution Medical and Origin Laboratories also have different types of 3D-printed swab models [54]. All these designs and productions showed a high concurrence in statistics compared with the current standard swabs. Today, some nasopharyngeal swabs designs can also be found at file repositories as free or commercial models [41]. There are millions of 3D-printed nasal swabs around the world that are used for COVID-19 testing and show us that the supply problem of critical needs can be solved with 3D printing when necessary [40].
3D printing in the development of therapeutic devices and their components
3D printing has been used widely for the production of various therapeutic devices developed around the world in the battle against COVID-19. Furthermore, the components of existing devices have been either developed or remanufactured. Different kinds of helpers, consumables, and educative systems have been created with the help of 3D printing where available traditional mass production systems ability to answer the need is lacking.
Therapeutic devices
SARS-CoV-2 virus is more active in highly humidified environments; thus it affects the respiratory system in humans widely. When the SARS-CoV-2 virus enters the human body, it comes into contact with the mucous membranes that line through the nose, mouth, and eyes. As like the rest of viruses, the virus enters a healthy cell and uses the healthy cell to make new virus parts. It multiplies, and the new viruses infect nearby cells. Then the SARS-CoV-2 virus moves through the mucous environment and reaches the lungs where it has the most dramatic effect. While lungs are not functioning properly oxygen saturation starts to decrease. When it goes below 95%, it is recommended to have artificial help for respiration; moreover when it goes below 90%, it is almost mandatory to have artificial help [55]. Nowadays, this help is provided by contemporary devices called mechanical ventilators. These ventilators control important parameters such as respiration rate, tidal volume, airway pressure, and positive end expiratory pressure (PEEP). However, the available stock for these devices to compensate for the necessities of the pandemic of COVID-19 was not possible. For example, the UK has announced that they had 10.000 contemporary and 8.000 old fashioned mechanical ventilators, while the required number was estimated to be 30.000 [56]. Hence, most of the companies around the world focused on the fast production of these contemporary devices. On the other hand, researchers also focused on easy, simple, and cheap versions of artificial respiration devices such as MIT, Oxford, Rice University, and so on. In this review, we will discuss two of those examples published by groups from Brasil-Canada and the UK.
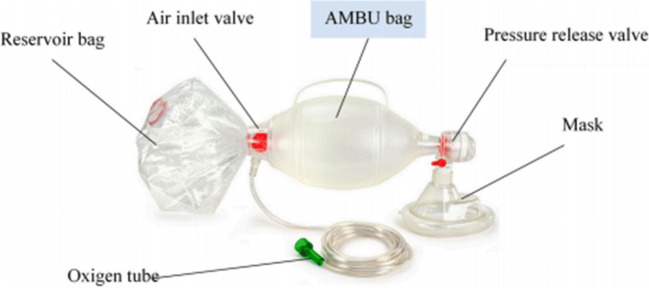
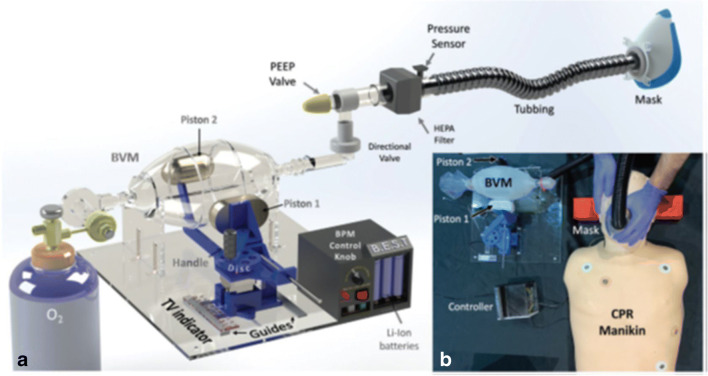
Automated inflating resuscitator (AIR) was developed by Bra-IRL-Can group (Adam Dubrovski et al.) [57] (Fig. 6) in response to the need for contemporary devices mentioned earlier. This group focused on easy, cheap, and fast response to the problem and proposed a device called AIR within a month of developing and manufacturing time. The total manufacturing cost was ca. 80 USD. The design consisted of a bag valve mask (BVM) including an exhalation port, patient valve, self-inflated bag (commonly known as AMBU (Artificial Manual Breathing Unit) (Fig. 7), and an oxygen inlet as the starting point. That oxygen inlet generally connected to a PEEP valve or oxygen tank. They turned the artificial manual breathing unit into an artificial automated breathing unit in a simple word of choice. In AIR, self-inflated bag is squeezed and released back by an automated mechanical system. This function is a substitute for the professional health care person's job in the manual using BVM. However, this device has no automated control in the respiration rate, tidal volume, airway pressure, PEEP, etc. These values can be adjusted at the beginning of the procedure in accordance with the patients’ age and weight. However, the AIR device does not give feedback to the doctors as the other simple ventilation systems created by MIT, Oxford, and RICE University in contrast with contemporary mechanical ventilation devices.
Fig. 6.
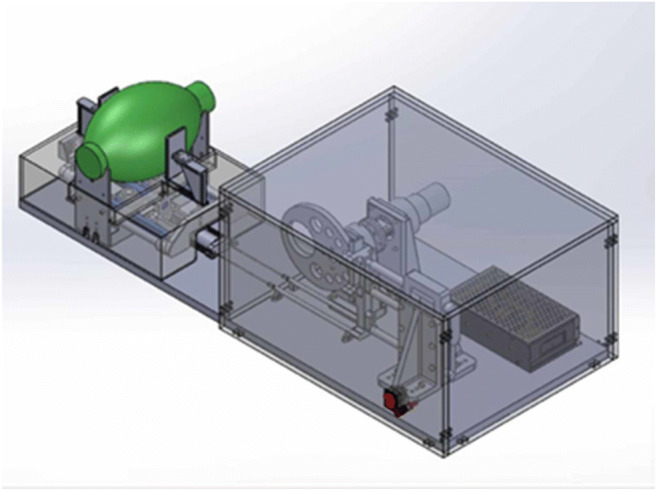
Illustration of AIR model [Adapted from 58]
Fig. 7.
Artificial manual breathing unit (AMBU) bag and main accessories [59]
The most important part about the AIR is it is almost entirely created with 3D printing. It consists of 46 different essential parts as given in [57]. Out of 46 parts, 37 are 3D printed. The AIR device step forward with the use of parts 80% 3D printed. Corresponding to COVID-19 pandemic, the creators manage to adapt the device to not become another contaminant agent with the precautions as follows:
All parts coming into contact with the patient’s breath are disposable or designed to be reusable.
All working components are contained within an impermeable casing. Healthcare workers are able to manually wipe clean all external surfaces.
The AIR can connect to a viral hygroscopic filter [57].
On the other hand, the fast responses given by the various scientists, engineers, and medical doctors for the shortage of mechanical ventilators have lucked the ability of automatic control over important parameters of contemporary mechanical ventilation such as respiration rate, tidal volume, plateau pressure, and PEEP. Remarkably a research done by the scientists of the University of Glasgow managed to automatic control over those parameters by similar design with other artificial automatic breathing units. Ravinder Dahiya et al. [60] proposed a rapidly deployable answer for the inadequacy of mechanical ventilators, a device called GlasVent. Big valve mask (BVM) has been widely used prior to the invention of conventional mechanical ventilators. They have still been used in the poor regions of the world or the emergencies until reaching an available mechanical ventilator. GlasVent differs from the other emergency design of ventilators with the automated control over respiration parameters. The base of the device has the ability to slide its motor away or towards the BVM which creates an ability to regulate the maximum compression of the self-inflated bag which results in control over tidal volume Fig. 8. The design has three-way of gaining power, regular electricity, battery, and manual operations with an additional foot working mechanism. An Arduino controls the GlasVent with inputs coming from potentiometers around the self-inflated bag for respiration rate, inputs coming from pressure sensor for the control of tidal volume and PEEK, and inputs coming from pressure sensor also provides an ability to be aware of critical situations. A LED sensor is placed in the case of such emergencies to warn medical care professionals. All the moving parts of this design and most of the other parts is manufactured from polylactic acid filament using the printing parameters explained by Ravinder Dahiya et al [62].
Fig. 8.
GlasVent System. a CAD model of GlasVent assembly, b System testing on a medical mannequin [Adapted from 61]
Therapeutic device parts
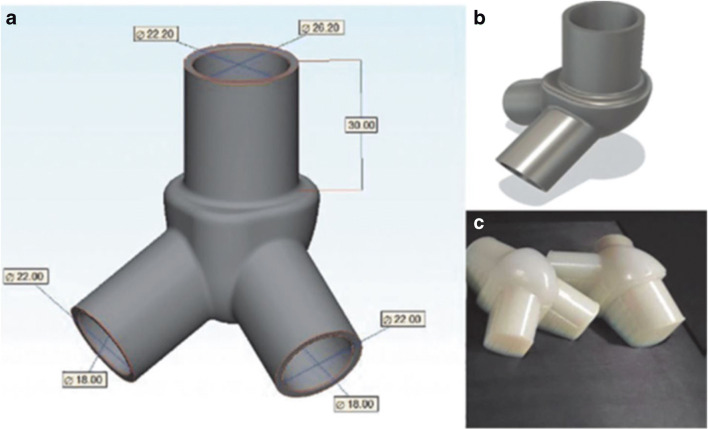
Along with the responses of making fast and easy respirators for the shortage of mechanical ventilators the idea of using one mechanical ventilator for more than one patient has come to light. The idea was put into test by Greg Neyman and Charlene Babcock Irvin 15 years before the COVID-19 pandemic. Commercially available T-tubes were used for the separation of airways. Four lung simulators have been used. Successful ventilation of four lung simulators has been successful, however, this study does not give any clue about adequate oxygenation [63]. Furthermore, the possible application of the 3D printing into the manufacturing of the ventilator airway splitter has been done 5 years earlier than the current pandemic [60]. The design and manufacturing of the airway splitters shows that it is possible to create these airways splitters using 3D printing. It also shows the effectiveness of 3D printing in the manufacturing of therapeutic device components. Another study has been done to analyze the oxygenation after the multi-patient usage of mechanical ventilators. Four sheep around 70 kg are ventilated using one mechanical ventilator and commercial manifolds. The sheep were successfully ventilated for a period of 12 h; however, challenges such as differential lung compliance or the possibility of cross-contamination were not studied [62].
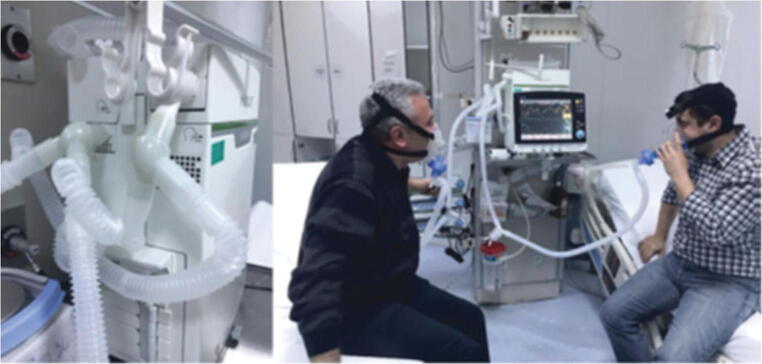
According to the studies discussed so far and the mere idea of “Why not use one ventilator for more patients?”, the need for a field test of this idea was so essential and important in the fight against the COVID-1919 Pandemic. The airway splitters or manifolds have been redesigned from scratch by researchers from the University of Health Sciences, Turkey for the purpose of answering the question. It is manufactured using 3D printing with polyjet technology as shown in Fig. 9. Two intensive care specialists with similar weights shared a mechanical ventilator using 3D manufactured manifolds as presented in Fig. 10. The results of the study showed that in the synchronized ventilation mode the mechanical ventilator did not give any alarms for a period of 15 minutes but in the non-synchronozied inhalation it gives alarms every minute or much frequently. Hence the application to use one ventilator for more than one patient requires synchronization in the patients. Because of the rapid expansion of COVID-19 disease and differentiation of the patient's respiration need and capacity sharing of one ventilator by two patient for a very short period of time doable under very hard conditions but using of one ventilator for more than two patients does not seem possible [63].
Fig. 9.
a Dimensions, b final design, and c manufactured version of the two-port splitter [63]
Fig. 10.
3D printed two-port splitter that adapted both the inspiratory and expiratory outputs of the ventilator and the testing process by two intensive care specialists [63]
Future prospects
Our world is currently facing the greatest challenges at all levels in the century; the novel Coronavirus, as these challenges were not limited to health problems only, but also to social life, the economy, unemployment rates, tourism and many others. Very few countries and places have relatively succeeded in confronting this disease and limiting its spread by taking the necessary measures and the effective use of resources. But, on the other side, the outbreak of this disease began very quickly, which did not allow many other countries to confront its consequences, as the shortage of medical devices and personal protective equipment puts many people, especially doctors and health workers, in inevitable danger. However, compared to the previous pandemics that humankind has undergone, there is no doubt that the development and technology has great impact in containing this disease, such as the use of 3D printing in the manufacture of ventilators and personal protective equipments, in addition to the use of artificial intelligence in the diagnosis and follow-up of patients to treat them, monitor their health and narrow the circle of infection.
Acknowledgments
The authors would like to acknowledge Ankara Development Agency (Ankara Kalkınma Ajansı Project No: TR51/19/FD/0041) for funding.
Declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Footnotes
Orcun Guvener and Abdullah Eyidogan contributed equally to this work.
References
- 1.Lu Y, Huang Z, Wang M, Tang K, Wang S, Gao P, Xie J, Wang T, Zhao J. Clinical characteristics and predictors of mortality in young adults with severe COVID-19: a retrospective observational study. Annals of Clinical Microbiology and Antimicrobials. 2021;20:3. doi: 10.1186/s12941-020-00412-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pettengill, M. A., Mcadam, A. J. (2020). doi:10.1128/JCM.02225-20.
- 3.WHO Weekly epidemiological update - 12 January 2021 https://www.who.int/publications/m/item/weekly-epidemiological-update%2D%2D-12-january-2021
- 4.Wang L, Didelot X, Yang J, Wong G, Shi Y, Liu W, Gao GF, Bi Y. Inference of person-to-person transmission of COVID-19 reveals hidden super-spreading events during the early outbreak phase. Nature Communications. 2020;11:5006. doi: 10.1038/s41467-020-18836-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gössling S, Scott D, Michael Hall C. Pandemics, tourism and global change: a rapid assessment of COVID-19. Journal of Sustainable Tourism. 2021;29(1):1–20. doi: 10.1080/09669582.2020.1758708. [DOI] [Google Scholar]
- 6.Siegenfeld AF, Bar-Yam Y. The impact of travel and timing in eliminating COVID-19. Communications on Physics. 2020;3:204. doi: 10.1038/s42005-020-00470-7. [DOI] [Google Scholar]
- 7.Omori R, Matsuyama R, Nakata Y. The age distribution of mortality from novel coronavirus disease (COVID-19) suggests no large difference of susceptibility by age. Scientific Reports. 2020;10:16642. doi: 10.1038/s41598-020-73777-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323:1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 9.Zhou F, Yu T, Ronghui D, Fan G, Liu Y, Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Serafini G, Parmigiani B, Amerio A, Aguglia A, Sher L, Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM: An International Journal of Medicine. 2020;113(8):531–537. doi: 10.1093/qjmed/hcaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Valeria S, Davide A, Vincenzo A. The Psychological and Social Impact of Covid-19: New Perspectives of Well-Being. Frontiers in Psychology. 2020;11:2550. doi: 10.3389/fpsyg.2020.577684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ranney ML, Griffeth V, Jha AK. Critical Supply Shortages — The Need for Ventilators and Personal Protective Equipment during the Covid-19 Pandemic. The New England Journal of Medicine. 2020;382:e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 13.Boskoski I, Gallo C, Wallace MB, Costamagna G. COVID-19 pandemic and personal protective equipment shortage: protective efficacy comparing masks and scientific methods for respirator reuse. Gastrointestinal Endoscopy. 2020;92(3):519–523. doi: 10.1016/j.gie.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McMahon DE, Peters GA, Ivers LC, Freeman EE. Global resource shortages during COVID-19: Bad news for low-income countries. PLoS Neglected Tropical Diseases. 2020;14(7):e0008412. doi: 10.1371/journal.pntd.0008412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kunovjanek, M. & Wankmüller, C. (2020). "An analysis of the global additive manufacturing response to the COVID-19 pandemic", Journal of Manufacturing Technology Management, Vol. ahead-of-print No. ahead-of-print. 10.1108/JMTM-07-2020-0263.
- 16.Bunting L, Roy S, Pinson H, Greensweig T. A novel inline PEEP valve design for differential multi-ventilation. American Journal of Emergency Medicine. 2020;38(10):2045–2048. doi: 10.1016/j.ajem.2020.06.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wierzbicki J, Nowacki M, Chrzanowska M, et al. Additive manufacturing technologies enabling rapid and interventional production of protective face shields and masks during the COVID-19 pandemic. Advances in Clinical and Experimental Medicine. 2020;29(9):1021–1028. doi: 10.17219/acem/126296. [DOI] [PubMed] [Google Scholar]
- 18.Nazarious MI, Mathanlal T, Zorzano M-P, Martin-Torres J. Pressure Optimized PowEred Respirator (PROPER): A miniaturized wearable cleanroom and biosafety system for aerially transmitted viral infections such as COVID-19. HardwareX. 2020;8:e00144. doi: 10.1016/j.ohx.2020.e00144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah, D., Sahu, D., Kini, A., Bagaria, V. (2020). Improvising the surgical helmet system for aerosol-generating procedures in the OR: Surgeon designed 3D printed mould for augmented filtration system. Journal of Clinical Orthopaedics and Trauma; article in press doi:10.1016/j.jcot.2020.09.030. [DOI] [PMC free article] [PubMed]
- 20.G.A. Longhitano, G.B. Nunes, G. Candido, J.V.L. da Silva, The role of 3D printing during COVID-19 pandemic: a review. Progress in Additive Manufacturing (2020). 10.1007/s40964-020-00159-x [DOI] [PMC free article] [PubMed]
- 21.Nazir, A., Azhar, A., Nazir, U., Liu, Y.-F., Qureshi, W. S., Chen, J.-E., Alanazi, E. (2020). The rise of 3D Printing entangled with smart computer aided design during COVID-19 era. Journal of Manufacturing Systems , article in press, doi:10.1016/j.jmsy.2020.10.009. [DOI] [PMC free article] [PubMed]
- 22.Taalbi J. Origins and pathways of innovation in the third industrial revolution. Industrial and Corporate Change. 2019;28(5):1125–1148. doi: 10.1093/icc/dty053. [DOI] [Google Scholar]
- 23.Akturk MS, Avci S. An integrated process planning approach for CNC machine tools. International Journal of Advanced Manufacturing Technology. 1996;12:221–229. doi: 10.1007/BF01351201. [DOI] [Google Scholar]
- 24.Yau HT, Yang TJ, Lin YK. Comparison of 3-D Printing and 5-axis Milling for the Production of Dental e-models from Intra-oral Scanning. Computer-Aided Design and Applications. 2016;13(1):32–38. doi: 10.1080/16864360.2015.1059186. [DOI] [Google Scholar]
- 25.Horvath, J. (2014) A Brief History of 3D Printing. In: Mastering 3D Printing. Apress, Berkeley, CA. 10.1007/978-1-4842-0025-4_1
- 26.Yan Q, Dong H, Jin S, Han J, Song B, Wei Q, Shi Y. A Review of 3D Printing Technology for Medical Applications. Engineering. 2018;4(5):729–742. doi: 10.1016/j.eng.2018.07.021. [DOI] [Google Scholar]
- 27.https://allaboutcad.com/creating-models-for-3d-printing/ Access date: 15.01.2021
- 28.Hale L, Linley E, Kalaskar DM. A digital workflow for design and fabrication of bespoke orthoses using 3D scanning and 3D printing, a patient-based case study. Scientific Reports. 2020;10(1):7028. doi: 10.1038/s41598-020-63937-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rengier F, Mehndiratta A, von Tengg-Kobligk H, Zechmann CM, Unterhinninghofen R, Kauczor HU, Giesel FL. 3D printing based on imaging data: review of medical applications. The International Journal for Computer Assisted Radiology and Surgery. 2010;5:335–341. doi: 10.1007/s11548-010-0476-x. [DOI] [PubMed] [Google Scholar]
- 30.International Journal of Latest Trends in Engineering and Technology Vol.(8)Issue(4-1), pp.264-272 DOI: 10.21172/1.841.44
- 31.Viera-Artiles J, Valdiande JJ. 3D-printable headlight face shield adapter. Personal protective equipment in the COVID-19 era. American Journal of Otolaryngology. 2020;41:102576. doi: 10.1016/j.amjoto.2020.102576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.M. Meglioli, G.M. Macaluso, A. Toffoli, S. Catros, 3D printing workflows for printing individualized personal protective equipment: an overview. Transactions on Additive Manufacturing Meets Medicine. 2, 1 (2020). 10.18416/AMMM.2020.2009006
- 33.A.M. Imbrie-Moore, M.H. Park, Y. Zhu, M.J. Paulsen, H. Wang, Y.J. Woo, Healthcare (Basel) (2020). 10.3390/healthcare8030225 [DOI] [PMC free article] [PubMed]
- 34.Swennen GRJ, Pottel L, Haers PE. Custom-made 3D-printed face masks in case of pandemic crisis situations with a lack of commercially available FFP2/3 masks. International Journal of Oral and Maxillofacial Surgery. 2020;49:673–677. doi: 10.1016/j.ijom.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.S. Chaturvedi, A. Gupta, S.V. Krishnan, A.K. Bhat, Design, usage and review of a cost effective and innovative face shield in a tertiary care teaching hospital during COVID-19 pandemic. J. Orthop. 21, 331–336 (2020). 10.1016/j.jor.2020.07.003 [DOI] [PMC free article] [PubMed]
- 36.P. Germonpre, D.V. Rompaey, C. Balestra, Evaluation of protection level, respiratory safety, and practical aspects of commercially available snorkel masks as personal protection devices against aerosolized contaminants and SARS-CoV2. International Journal of Environmental Research and Public Health. 17(12), 4347 (2020). 10.3390/ijerph17124347 [DOI] [PMC free article] [PubMed]
- 37.Kao CL, Lin CH, Formos J. A novel mask to prevent aerosol spread during nebulization treatment. Medical Association. 2020;120:769–771. doi: 10.1016/j.jfma.2020.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nicholson, K., Henke-Adams, A., Henke, D. M., Kravitz, A. V., Gay, H. A., Modified full-face snorkel mask as COVID-19 personal protective equipment: quantitative results (Preprints Web, 2020), https://www.preprints.org/manuscript/202004.0293/v1. Accessed 20 Dec 2020 [DOI] [PMC free article] [PubMed]
- 39.Ford, J., Goldstein, T., Trahan, S. et al. (2020). 3D Print Med 10.1186/s41205-020-00076-3 [DOI] [PMC free article] [PubMed]
- 40.Mass-Producing Nasopharyngeal Swabs, (3D Systems Web, 2020). https://www.3dsystems.com/covid-19-response#nasalSwabs. Accessed 24 Dec 2020
- 41.Rybicki F.,3D Printing in Medicine: COVID-19 Testing with 3D Printed Nasopharyngeal Swabs. (Oxford Academic Web, 2020) https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa1437/5908885. Accessed 24 Dec 2020
- 42.C.J. Callahan, R. Lee, K.E. Zulauf, et al., Open development and clinical validation of multiple 3D-printed nasopharyngeal collection swabs: rapid resolution of a critical COVID-19 testing bottleneck. J. Clin. Microbiol. 58(8), e00876-20 (2020). 10.1128/jcm.00876-20 [DOI] [PMC free article] [PubMed]
- 43.Prototyping Rapid Diagnostics for COVID-19 With 3D Printing.(Formlabs Web, 2020) https://formlabs.com/covid-19-response/covid-19-rapid-diagnostics/ Accessed 21 Dec 2020
- 44.Cheriyedath, S., 3D printed nanoparticle biosensing platform detects SARS-CoV-2 antibodies within seconds. (News Medical Web,2020) https://www.news-medical.net/news/20200914/3D-printed-nanoparticle-biosensing-platform-detects-SARS-CoV-2-antibodies-within-seconds.aspx. Accessed 21 Dec 2020
- 45.Beary, B. New Covid Antibody Test Gets Results in 10 Seconds Using 3D Printing., (Medical EXPO Web,2020) http://emag.medicalexpo.com/new-covid-antibody-test-gets-results-in-10-seconds-using-3d-printing/. Accessed 27 December 2020
- 46.Schachner ER, Spieler B. Three-dimensional (3D) lung segmentation for diagnosis of COVID-19 and the communication of disease impact to the public. BML Case Reports. 2020;13:e236943. doi: 10.1136/bcr-2020-236943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sinha MS, Bourgeois FT, Sorger PK. Personal Protective Equipment for COVID-19: Distributed Fabrication and Additive Manufacturing. American Journal of Public Health. 2020;110:1162–1164. doi: 10.2105/AJPH.2020.305753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.G.S. Longhitano, G. Nunes, G. Candido, J.V.L. da Silva, The role of 3D printing during COVID-19 pandemic: a review. Progress in Additive Manufacturing (2020). 10.1007/s40964-020-00159-x [DOI] [PMC free article] [PubMed]
- 49.S. Decker, T. Goldstein, J. Ford, et al., 3-Dimensional Printed Alternative to the Standard Synthetic Flocked Nasopharyngeal Swabs Used for Coronavirus Disease 2019 Testing. Clinical Infectious Diseases (2020). 10.1093/cid/ciaa1366 [DOI] [PMC free article] [PubMed]
- 50.Oladapo BI, Ismail SO, Afolalu TD, Olawade DB, Zahedi M. Review on 3D printing: Fight against COVID-19. Materials Chemistry and Physics. 2021;258:123943. doi: 10.1016/j.matchemphys.2020.123943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cox JL, Koepsell SA. 3D-Printing to Address COVID-19 Testing Supply Shortages. Laboratoriums Medizin. 2020;51:e45–e46. doi: 10.1093/labmed/lmaa031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Arnold, F. W., Grant, G., Bressoud, P.F. et al., A comparison efficacy study of commercial nasopharyngeal Swabs versus a novel 3D printed swab for the detection of SARSCoV-2. The University of Louisville Journal of Respiratory Infections. 4(1), 41 (2020). 10.18297/jri/vol4/iss1/41
- 53.Oland G, Garner O, de St Maurice A. Prospective clinical validation of 3D printed nasopharyngeal swabs for diagnosis of COVID-19. Diagnostic Microbiology and Infectious Disease. 2020;99:115257. doi: 10.1016/j.diagmicrobio.2020.115257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mechanical Ventilator, (London Health Scienses Centre Web,2018) https://www.lhsc.on.ca/critical-care-trauma-centre/mechanical-ventilator. Accessed 21 Dec 2020
- 55.How many ventilators does the UK have - and how many might we need?, (BBC Web, 2020) https://www.bbc.com/news/health-52036948. Accessed 19 Dec 2020
- 56.L. Fiorineschi, F.S. Frillici, F. Rotini, Challenging COVID-19 with Creativity: Supporting Design Space Exploration for Emergency Ventilators. Applied Sciences 10 (2020). 10.3390/app10144955
- 57.Ntagios M, Nassar H, Pullanchiyodan A, Navaraj WT, Dahiya R. Robotic Hands with Intrinsic Tactile Sensing via 3D Printed Soft Pressure Sensors. Advances in Intelligent Systems. 2019;2:1900080. doi: 10.1002/aisy.201900080. [DOI] [Google Scholar]
- 58.B. Gino, Z. Wang, P. d'Entremont, T.S. Renouf, A. Dubrowski, Automated Inflating Resuscitator (AIR): Design and Development of a 3D-Printed Ventilator Prototype and Corresponding Simulation Scenario Based on the Management of a Critical COVID-19 Patient. Cureus (2020). 10.7759/cureus.9134 [DOI] [PMC free article] [PubMed]
- 59.Neyman G, Irvin CB. A Single Ventilator for Multiple Simulated Patients to Meet Disaster Surge. Academic Emergency Medicine. 2006;13:1246–1249. doi: 10.1197/j.aem.2006.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Siderits R, Neyman G. Open J. Emergency Medicine. 2014;02:46–48. doi: 10.4236/ojem.2014.23008. [DOI] [Google Scholar]
- 61.Christou A, Ntagios M, Hart A, Dahiya R. GlasVent—The Rapidly Deployable Emergency Ventilator. Global Challenges. 2020;4:2000046. doi: 10.1002/gch2.202000046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Paladino L, Silverberg M, Charchaflieh JG, Eason JK, Wright BJ, Palamidessi N, Arquilla B, Sinert R, Manoach S. Increasing ventilator surge capacity in disasters: Ventilation of four adult-human-sized sheep on a single ventilator with a modified circuit. Resuscitation. 2008;77:121–126. doi: 10.1016/j.resuscitation.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 63.Ayyıldız, S., Dursun, A.M., Yıldırım, V., Ince, M.E., Gülçelik, M.A., Erdöl, C. 3D-Printed splitter for use of a single ventilator on multiple patients during COVID-19. 3D Printing and Additive Manufacturing. 7(4), 181–185. 10.1089/3dp.2020.0102 [DOI] [PMC free article] [PubMed]