Abstract
The developments in hip and knee arthroplasty over recent years have aimed to improve outcomes, reduce complications and improve implant survival. This review describes some of the most interesting trends and developments in this important and fast-moving field. Notable developments have included ceramic hip resurfacing, mini hip stems, cementless knee replacement and the wider adoption of the dual mobility articulation for hip arthroplasty. Advances in additive manufacturing and the surface modification of joint replacements offer increasing options for more challenging arthroplasty cases. Robotic assisted surgery is one of the most interesting developments in hip and knee surgery. The recent growth in the use of this technology is providing data that will help determine whether this approach should become the standard of care for hip and knee arthroplasty in the future.
Keywords: Orthopaedics, hip arthroplasty, total knee arthroplasty, osteoarthritis, robotic care
Introduction
Hip and knee total joint arthroplasty are effective surgical treatments for the management of arthritis. Joint replacement surgery involves the resection of the degenerative joint and replacement with syntenic components which reconstruct the worn joint surface allowing pain free mobilisation. Hip and knee implant design and development over the past century has predominantly focussed on reducing mechanical wear and enhancing implant fixation. This approach has been very successful, with modern bearing surfaces and implant coatings providing far more durable solutions than those available at the advent of modern hip and knee arthroplasty in the 1960s. With an increasingly active and longer living population and a trend for joint replacement earlier in life, the work on improving implant survival continues. However, increasingly the latest developments in hip and knee arthroplasty implant technology have concentrated on technologies hoping to improve patient outcomes through strategies to mimic more natural kinematics and optimised implant positioning. This review will highlight several of what we consider are the most significant technological developments with respect to implant design and assistive technology in hip and knee arthroplasty.
Hip resurfacing
Hip resurfacing is perhaps a surprising choice to consider as a new technology given that resurfacing implants have been used in various guises for well over 40 years.1 Hip resurfacing surgery provides an alternative to the more conventional hip replacement for the treatment of hip arthritis. Hip resurfacings (Figure 1) preserves femoral bone stock compared to conventional total hip arthroplasty. The larger size femoral head articulation results in a biomechanically more stable joint.3 The advantages of larger metal on metal articulations, were not without cost, with certain implants demonstrating high revision rates predominantly due to the generation of metal debris leading to adverse reactions in some patients. The increased revision rate has negatively affected the perception of hip resurfacing.1 However, hip resurfacing has been shown to offer lower dislocation rates and superior functional outcomes for younger active patients compared to conventional total hip arthroplasty.4,5 Whilst metal on metal hip resurfacing remains an option for active males with larger hips, it is no longer considered appropriate for men with smaller femoral head sizes and never appropriate in women. Therefore, recent advances have focused on new alternative bearing couples for hip resurfacing. Novel approaches to address this issue include the use of ceramic on ceramic or metal on polyethylene articulations.
Figure 1.
Metal-on-metal Birmingham Hip Resurfacing.2
To date there are at least two ceramic hip resurfacings undergoing early clinical trials. The H1 ceramic non-porous non-cemented hip resurfacing developed by Embody Orthopaedic Limited (London, UK) is presently under evaluation as part of a multicentre observational study which commenced recruiting in September 2017.6 This ten-year follow-up study aims to evaluate the safety and efficacy of the prosthesis. The ceramic on ceramic ReCerf™ developed by MatOrtho (Leatherhead, Surrey UK) is currently awaiting certification in the UK, however the first device was implanted on the 24th September 2018. While early clinical data are not yet available for either implant, cadaveric studies have evaluated the mechanical properties of the ReCerf™ arthroplasty which have reassuringly demonstrated comparable deformation between a standard metal component and the novel ceramic acetabular component.7
Although ceramic on ceramic articulations do have favourable wear characteristics, there is concern regarding the potential for squeaking and the brittleness of ceramic bearings. Furthermore, there is the potential for unwanted reduction in bone density around the implanted ceramic implants, a phenomenon known as stress shielding.8 To address these potential issues the metal on cross-linked polyethylene (MoX) hip resurfacing was developed by Derek McMinn. To date, 88 MoX resurfacings have been implanted.9 This articulation has the potential to minimise metal ion release and with the lower stiffness of polyethylene there is reduced potential for stress shielding seen with stiffer acetabular components, though this is at the possible risk of increased volumetric polyethylene wear.10
Mini stem total hip arthroplasty
One of the advantages of hip resurfacing is the preservation of femoral bone stock in comparison to conventional total hip replacement. Partly as a consequence of the decline of metal on metal hip resurfacing and due to the increased popularity of minimally invasive surgical approaches, there has been a trend for the development of smaller femoral prostheses (Figure 2) that aim to preserve bone stock and load the proximal femur in a more physiological manner.12
Figure 2.

Tri-Lock mini stem.11
Differences between mini-stem philosophies and designs has meant that systematic reviews and meta-analyses of the varying implants has been challenging.13 However, a systemic review by Lidder et al. including 15 studies demonstrated implant survival of 98.6% at a mean follow up of 12 years.14 However, the learning curve for mini stems appears to be greater than for conventional total hip arthroplasty with variation in femoral neck canal diameter and the need for a stable press fit requiring a low tolerance for error in implant positioning and surgical technique.Click or tap here to enter text.15 Evaluation of these stems is ongoing with a recently published randomised trial into stability of mini stem implants at 2 years with radiostereometric analysis demonstrating femoral component migration comparable to standard length stems.16
Dual mobility total hip arthroplasty
The use of dual mobility articulations, whilst not novel having first been developed by Gilles Bousquet in 1974,17 have in recent years been adopted more frequently for use in primary total hip arthroplasty.10 Dual mobility implants (Figure 3) consist of a small metal or ceramic head that is enclosed but mobile within a larger polyethylene head which in turn articulates with the acetabular component of the joint replacement. Many national joint registries have noticed an increasing trend in the use of Dual Mobility articulations, the latest report from the American joint replacement registry reported an increase use of Dual mobility to 6.9% of all total hip arthroplasties.19 There is presently some suggestion that dual mobility articulations should be offered as a mainstream alternative to more traditional articulations.20 Given the advantageous and well-established increase in stability associated with a dual mobility articulation,4,5 the trend for increased utilisation of the technology may be related to increasing recognition of the relevance of unfavourable spinopelvic mobility and its implications in the stability of total hip arthroplasty. There has also been growth of their use in high risk groups such as those with neuromuscular conditions or cognitive impairment.21 However, there are concerns related to volumetric polyethylene wear, intraarticular dislocations and there is limited data on long term survivorship.Click or tap here to enter text.22 Retrieval studies to date have been reassuring with respect to wear rates.23,24
Figure 3.
Dual Mobility Total hip arthroplasty.18
The use of a dual mobility articulation also has a role in revision surgery given their increased stability. They have been used successfully for femoral only revision of large head metal on metal hip arthroplasty25 as well as for alternative revision indications with dual mobility articulations demonstrating superior survivorship compared to fixed-bearing implants.26
Cementless knee total knee arthroplasty
One of the more promising areas in the development of knee arthroplasty implants has been in the development of cementless methods of fixation. Traditionally total knee arthroplasty prostheses have been implanted with polymethyl methacrylate cement as a grout interdigitating with the cancellous bone and the implant surface. Cementless total knee arthroplasty has the advantage of avoiding an extra interface with the hope this could reduce rates of wear and loosening. However, initial pressfit designs were associated with high early failure rates with a series demonstrating 8% aseptic loosening rate at a mean follow-up of 11 years.Click or tap here to enter text.27,28 Recent developments in cementless technology and implant design have led to a new generation of cementless total knee arthroplasty implants. A recent randomised study has reported early follow-up data comparing patients receiving cemented or cementless implants. At two years both showed equivalence in patient reported outcome scores and degree of subsidence. Cementless implants were associated with a shorter operative time. It should be noted that patients aged over 75, those with a body mass index over 40 kg/m2, evidence of grossly osteoporotic bone or bone defects were excluded.29 A meta-analysis of cementless knee arthroplasty encompassing 7 studies with a mean follow-up of 6 years found encouraging results in terms of survivorship, though studies again used highly selective inclusion criteria.30 The relatively selective nature of studies of cementless knee arthroplasty implants makes it difficult to draw conclusions on the appropriateness of this technology in the general population.31
Cementless technology can be successful in the knee. The Oxford® cementless partial knee replacement from Zimmer Biomet (Warsaw, Indiana USA) has demonstrated excellent survivorship with limited concern regarding osseointegration.32,33
While Early cementless knee replacement designs with high failure rates left many younger patients with significant lysis and bone loss.7 Overall the initial results of the newer class of cementless knee replacement are encouraging, though further long-term studies are required before this technology supplants cementation.
Implant surface modification
Advances in the shape of implants is often at the forefront of prosthetic joint development. However, with the growing challenge of prosthetic joint infection and the aim of further improving osseointegration, modification of the implant surface topography and chemistry has provided a new avenue in implant design with promising results.
While several materials are used for the production of joint replacements, Titanium has been the focus for the advances in surface modification. Titanium alloy, commonly Ti-6Al-4V, is frequently used in orthopaedics owing to its favourable biomechanical properties and amenity to surface modification.34 Topographical modifications aim to improve osteointegration by encouraging ongrowth or ingrowth of bone. These techniques have focused on the microscale and use roughening processes such as grit blasting or plasma sprayed surface coatings.35
The recognition of the potential effects of nanoscale surface topography have led to the development of techniques to modify the surface topography on a much smaller scale. These approaches include methods such as electron beam lithography and anodisation creating nanoscale tubes, pits, pores and pillars on the implant surface that can be favourable to osteoconduction and consequently osteointegration.
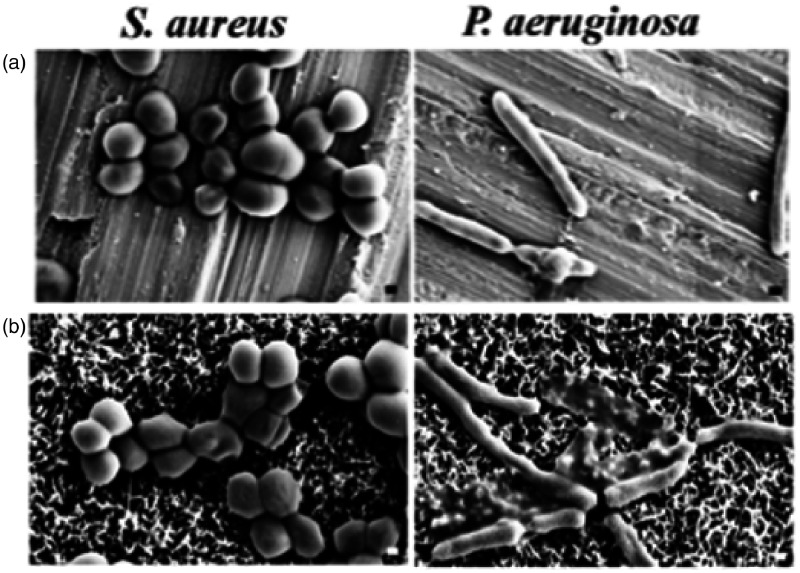
The process of surface modification on the nanoscale level apart from promoting osteointegration, also has the potential to affect the interaction between bacterial pathogens and the implant potentially mitigating the devastating consequences of prosthetic joint infection.36–38 Since the discovery of the adverse role of biofilms associated with bacterial infection,39 alteration of implant surfaces either via nanotopographic patterns or elution of bactericidal ions such as silver have provided an appealing approach. Modulation of a Titanium surface nanostructure has been demonstrated to reduce the adhesion of several bacterial species that are responsible for over 50 percent of prosthetic joint infections.40 Preventing bacterial adhesion helps inhibit early bacterial colonisation, impede evasion of the immune system and maximise the effectiveness of antibiotics given in the perioperative period. The techniques have looked to nature for inspiration and have recognised that through evolution over millennia several natural surfaces have developed ways to reduce bacterial colonisation. Therefore, scientists have recreated on a nanoscale the features of dragonfly wings and shark skin (Figure 4), the dragon fly wing with nanopillars has a self-cleaning surface reducing bacterial adhesion as well as bacteriocidal properties.42
Figure 4.
Effect of S. aureus and P. aeruginosa growth on control titanium surface a) and the nanopatterned surface fabricated via hydrothermal etching to mimic the surface architecture of dragonfly wings. A reduction in attachment and viability of bacteria was seen in the modified surface.41
An alternative to modifying the implant surface topography, is to engineer the implant to elute substances with antimicrobial properties. The most widely studied technique is silver nanoparticles. These antimicrobial nanoparticles leeched from implants have been demonstrated to be effective against Escherichia coli and Staphylococcus aureus for up to 10 days in vitro.43 However, there is some concern regarding elution of nanoparticles and local tissue toxicity. These technologies are in the translational stage but are likely to find their initial justification for use in terms of risk and cost-benefit in megaprosthetic replacements for revision joint replacement or sarcoma surgery.44
Additive manufacturing and custom implants
The majority of joint replacements undertaken utilise ‘off the shelf’ components which provide a satisfactory solution for the majority of patients. The customisation of implants provides the opportunity to provide a personalised solution for hip and knee joint reconstruction. While the majority of arthroplasty cases probably do not require such a tailored approach. More complex revision surgery with substantial bone loss, tumour surgery and surgery following major trauma may benefit from such a strategy. As technology has advanced and individual implant costs are reduced, the customisation of implants is expected to rise.45
Customisation of femoral implants for total hip arthroplasty aims to improve the match between the native anatomy and the implant to reduce stress shielding as well as more accurately restore the joint centre of rotation. The earlier generations of implants were customised from standard radiographs and manufactured using standard Computer Numerical Control (CNC) machining before coating to encourage osteointegration. The series of customised hip replacements published by Muirhead-Allwood et al. in 2010 demonstrated survivorship of 98.2% at 13.2 years for the use of customised hip stems which was felt comparable to the best standard femoral components.46 Dessyn et al. demonstrated similarly good follow-up at 20 years from their series of 232 hip replacements with 96.6% survivorship in a younger cohort of patients published more recently.47
Newer additive manufacturing techniques have made it simpler to produce complex customised implants including porous structures with variable density and stiffness to minimise bone loss and remodelling due to stress shielding.48,49 The majority of experience of custom additive manufactured implants comes from acetabular revision surgery. A recently published review into the use of a custom triflange acetabular components by Martino et al. found in 17 studies that the combined complication rate was 29% with dislocation being the most common (11%) followed by infection (6%).50 The aseptic loosening rate of the 579 hips included with a mean follow-up of 57.4 months was 3.1%. These complex cases demonstrated outcomes that were comparable with other reconstructive options. While these custom solutions often provide an appealing option for challenging cases it should be remembered that due to their individualised nature these implants cannot provide a track record. Since 2002 the Orthopaedic Data Evaluation Panel (ODEP) have evaluated the outcomes for standard joint replacements ensuring that they remain safe and effective as well as providing a benchmark for newer implants. Such ratings are unavailable for custom implants and surgeons should ensure that patients are aware that data on survivorship is unavailable.
Robotic assisted surgery
The decision regarding the intraoperative placement of components for hip and knee replacements has traditionally relied on anatomical landmarks and referencing jigs to guide component orientation. One of the most exciting developments in joint arthroplasty is the use of robotic assisted hip and knee arthroplasty to support the surgeon in these critical decisions. Robotic assisted joint replacement surgery has been around for a while, with systems available in the 1980s.51 Robotic assisted surgery is an evolution of navigated joint replacement surgery where computer assistance helped to guide the positioning of instruments and implants. Robotic surgery takes this a step further with the robot helping to position instruments or controlling the function of tools to ensure that bone resection matches the planned operation. The surgical plan may be based on the patient’s own anatomy derived from a CT scan or increasingly “image-free” systems are used which map a series of anatomical landmarks from the patient peri-operatively to a stored catalogue of joint morphologies that are used to plan the procedure.
There has been significant growth in the use of robotic assistance over the past decade, particularly in the USA. In the New York region between 2008 and 2015 just over 5% of all hip and arthroplasty procedures were either robot or navigation assisted.51 Much of the recent drive for increased use of robotic technology (Figure 5) has come from the engagement of the major hip and knee implant manufacturers. The Mako system by Stryker (Kalamazoo, Michigan USA), the Navio/BlueBelt from Smith & Nephew (Andover, Massachusetts USA) or ROSA from Zimmer Biomet (Warsaw, Indiana USA) are increasingly widely available.
Figure 5.
Stryker Mako Robotic System Chai W, et al. Use of Robotic‐Arm Assisted Technique in Complex Primary Total Hip Arthroplasty.52
There is good evidence that robotic assisted surgery can help to improve implant positioning accuracy compared to manual placement in both hip and knee arthroplasty surgery. Lawson et al.50,53 demonstrated statistically significant improvement in acetabular component positioning placed within 5° of the target alignment with the use of robotic guidance compared to standard techniques in a case series of 100 patients. Illgen et al.51,54 found similar improvement in acetabular component placement for total hip arthroplasty accuracy using robotic assistance compared to manual placement.
Bell et al. demonstrated improved accuracy in implant position with robotic assisted surgery compared to standard techniques in unicompartmental knee replacement in a randomised study of 120 patients.55 Several other studies for unicompartmental knee replacement and total knee replacement have demonstrated that accuracy of implant alignment can be improved with robotic assisted surgery.56–59 In knee arthroplasty, robotic assistance can include tensioning devices to ensure accurate ligament balance when using a gap balancing technique.60
It is clear that robotic assistance can help surgeons achieve a particular plan, though are there other benefits? Bukowski et al. reported lower blood loss and superior functional outcome scores with robotic assistance in their comparison of 100 robotic assisted and 100 manual total hip arthroplasties.61 In total knee arthroplasty, robotic assistance has been shown to protect soft tissues in comparison to manual techniques.62 However, overall there is little data currently to suggest that robotic assisted surgery leads to superior functional outcomes. A meta-analysis by Karunaratne et al. looking at the outcomes of 14 studies of robotic hip and knee arthroplasty did not detect a difference in functional outcomes between robotic assisted and manual surgery.63 None of the included studies, which were noted to all be of low or very low quality, showed any difference in pain, quality of life or satisfaction with surgery. In a meta-analysis of manual and robotic assisted unicompartmental knee replacement Zhang et al. did not show a difference between the groups in terms of functional outcomes, revision rate or range of motion.64
Robotic assisted surgery has additional associated costs including hardware purchase, theatre time and radiology related outlay for image guided systems. Given the absence of clear clinical benefit to date, cost-effectiveness has been a barrier to wider adoption. However, studies have suggested that high volume centres using robotic assisted surgery could be cost effective for unicompartmental knee replacement.51,65 Further studies will be needed to demonstrate if robotic assisted surgery should be considered the gold standard for hip and knee arthroplasty.
Conclusion
This review has focussed on several of the most exciting strategies and developments in hip and knee arthroplasty as well as our evolving understanding of the use of robotics in joint replacement. While these developments focus on separate aspects of joint arthroplasty; they are united in their overarching aim of improving patient outcomes. There isrecognition that innovation, whilst essential, needs to be balanced with the critical role of doctors to protect patients from the potential harmful effects of novel technologies being brought to market without a prior rigorous evaluation. Surgeons should resist the temptations of these technological advances until such evaluation has been undertaken often in the form of well conducted and reviewed clinical trials. The rule of diminishing return and the fact that the majority of joint replacement surgeries provide excellent outcomes means that these advances need to demonstrate convincing long-term data to justify their adoption over established technology.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Martin Marsh https://orcid.org/0000-0003-4172-7890
References
- 1.Amstutz HC, Duff MJL. Hip resurfacing: history, current status, and future. Hip Int J Clin Exp Res Hip Pathology Ther 2015; 25: 330–338. [DOI] [PubMed] [Google Scholar]
- 2.De Smet KA, Pattyn C, Verdonck R. Early results of primary Birmingham hip resurfacing using a hybrid Metal-On-Metal couple. Hip Int 2002; 12: 158–162. [DOI] [PubMed] [Google Scholar]
- 3.Su EP. Hip resurfacing: for the right patient and surgeon. Seminars Arthroplast 2016; 27: 239–243. [Google Scholar]
- 4.Oxblom A, Hedlund H, Nemes S, et al. Patient-reported outcomes in hip resurfacing versus conventional total hip arthroplasty: a register-based matched cohort study of 726 patients. Acta Orthop 2019; 90: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haddad FS, Konan S, Tahmassebi J. A prospective comparative study of cementless total hip arthroplasty and hip resurfacing in patients under the age of 55 years. Bone Joint J 2015; 97-B: 617–622. [DOI] [PubMed] [Google Scholar]
- 6.Cobb JP, Clarke SJ, Jeffers J, et al. Anatomic ceramic hip resurfacing arthroplasty: first in human trials. Orthopaedic Proceedings 2018; 100-B: 29–29. [Google Scholar]
- 7.Farrier AJ, Moore L, Manning W, et al. Comparing the cup deformation following implantation of a novel ceramic-on-ceramic hip resurfacing bearing to a metal standard in a cadaveric model. Proc Inst Mech Eng H 2019; 233: 603–610. [DOI] [PubMed] [Google Scholar]
- 8.Su EP. Ceramic-Ceramic bearing: Too unpredictable to use it regularly. Hss J 2012; 8: 287–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Treacy RBC, Holland JP, Daniel J, et al. Preliminary report of clinical experience with metal-on-highly-crosslinked-polyethylene hip resurfacing. Bone Joint Res 2019; 8: 443–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones CW, De Martino I, D'Apolito R, et al. The use of dual-mobility bearings in patients at high risk of dislocation. Bone Joint J 2019; 101-B: 41–45. [DOI] [PubMed] [Google Scholar]
- 11.Tatani I, Panagopoulos A, Diamantakos I, et al. Comparison of two metaphyseal-fitting (short) femoral stems in primary total hip arthroplasty: study protocol for a prospective randomized clinical trial with additional biomechanical testing and finite element analysis. Trials 2019; 20: 359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stulberg SD, Patel RM. The short stem. Bone Joint J 2013; 95-B: 57–62. [DOI] [PubMed] [Google Scholar]
- 13.Feyen H, Shimmin AJ. Is the length of the femoral component important in primary total hip replacement? Bone Joint J 2014; 96-B: 442–448. [DOI] [PubMed] [Google Scholar]
- 14.Lidder S, Epstein DJ, Scott G. A systematic review of short metaphyseal loading cementless stems in hip arthroplasty. Bone Joint J 2019; 101-B: 502–511. [DOI] [PubMed] [Google Scholar]
- 15.Pairon P, Haddad FS. Stem size in hip arthroplasty. Bone Joint J 2018; 100-B: 1133–1135. [DOI] [PubMed] [Google Scholar]
- 16.Ferguson RJ, Broomfield JA, Malak TT, et al. Primary stability of a short bone-conserving femoral stem. Bone Joint J 2018; 100-B: 1148–1156. [DOI] [PubMed] [Google Scholar]
- 17.Fessy M-H. La double mobilité. Revue De Chir Orthopédique Et Traumatologique 2010; 96: 891–898. [Google Scholar]
- 18.Mertl P, Combes A, Leiber-Wackenheim F, et al. Recurrence of dislocation following total hip arthroplasty revision using dual mobility cups was rare in 180 hips followed over 7 years. Hss J Musculoskelet J 2012; 8: 251–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heckmann N, Weitzman DS, Jaffri H, et al. Trends in the use of dual mobility bearings in hip arthroplasty: an analysis of the american joint replacement registry. Bone Jt J 2020; 102-B: 27–32. [DOI] [PubMed] [Google Scholar]
- 20.Blakeney WG, Epinette J-A, Vendittoli P-A. Dual mobility total hip arthroplasty: should everyone get one? Efort Open Rev 2019; 4: 541–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rivière C, Lazennec J-Y, Straeten CVD, et al. The influence of spine-hip relations on total hip replacement: a systematic review. Orthop Traumatol Surg Res 2017; 103: 559–568. [DOI] [PubMed] [Google Scholar]
- 22.Plummer DR, Haughom BD, Valle CJD. Dual mobility in total hip arthroplasty. Orthop Clin North Am 2014; 45: 1–8. [DOI] [PubMed] [Google Scholar]
- 23.Boyer B, Neri T, Geringer J, et al. Long-term wear of dual mobility total hip replacement cups: explant study. Int Orthop 2018; 42: 41–47. [DOI] [PubMed] [Google Scholar]
- 24.Tarity TD, Koch CN, Burket JC, et al. Fretting and corrosion at the backside of modular cobalt chromium acetabular inserts: a retrieval analysis. J Arthroplasty 2017; 32: 1033–1039. [DOI] [PubMed] [Google Scholar]
- 25.Chan MK, Caudwell M, Suchowersky A, et al. Femoral side‐only revision options for the Birmingham resurfacing arthroplasty. Anz J Surg 2019; 89: 1016–1021. [DOI] [PubMed] [Google Scholar]
- 26.Harwin SF, Sultan AA, Khlopas A, et al. Mid-Term outcomes of dual mobility acetabular cups for revision total hip arthroplasty. J Arthroplasty 2018; 33: 1494–1500. [DOI] [PubMed] [Google Scholar]
- 27.Berger RA, Lyon JH, Jacobs JJ, et al. Problems with cementless total knee arthroplasty at 11 years followup. Clin Orthop Relat R 2001; 392: 196–207. [DOI] [PubMed] [Google Scholar]
- 28.Nafei A, Nielsen S, Kristensen O, et al. The press-fit kinemax knee arthroplasty. High failure rate of non-cemented implants. J Bone Jt Surg Br Volume 1992; 74-B: 243–246. [DOI] [PubMed] [Google Scholar]
- 29.Nam D, Lawrie CM, Salih R, et al. Cemented versus cementless total knee arthroplasty of the same modern design. J Bone Joint Surg Am 2019; 101: 1185–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Newman J, Sodhi N, Dekis J, et al. Survivorship and functional outcomes of cementless versus cemented total knee arthroplasty: a meta-analysis. J Knee Surg 2020; 33: 270–278. DOI: 10.1055/s-009-1678525. [DOI] [PubMed] [Google Scholar]
- 31.Evans JT, Walker RW, Evans JP, et al. How long does a knee replacement last? a systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 2019; 393: 655–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van der List JP, Sheng DL, Kleeblad LJ, et al. Outcomes of cementless unicompartmental and total knee arthroplasty: a systematic review. Knee 2017; 24: 497–507. [DOI] [PubMed] [Google Scholar]
- 33.Mohammad HR, Kennedy JA, Mellon SJ, et al. Ten-year clinical and radiographic results of 1000 cementless Oxford unicompartmental knee replacements. Knee Surg Sports Traumatology Arthrosc 2019; ▪: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guillemot F. Recent advances in the design of titanium alloys for orthopedic applications. Expert Rev Med Devices 2005; 2: 741–748. [DOI] [PubMed] [Google Scholar]
- 35.Ramaswamy Y, Wu C, Zreiqat H. Orthopedic coating materials: considerations and applications. Expert Rev Med Devices 2009; 6: 423–430. [DOI] [PubMed] [Google Scholar]
- 36.Campoccia D, Montanaro L, Arciola CR. A review of the biomaterials technologies for infection-resistant surfaces. Biomaterials 2013; 34: 8533–8554. [DOI] [PubMed] [Google Scholar]
- 37.Gbejuade HO, Lovering AM, Webb JC. The role of microbial biofilms in prosthetic joint infections. Acta Orthop 2015; 86: 147–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chouirfa H, Bouloussa H, Migonney V, et al. Review of titanium surface modification techniques and coatings for antibacterial applications. Acta Biomater 2019; 83: 37–54. [DOI] [PubMed] [Google Scholar]
- 39.Costerton JW. Biofilm theory can guide the treatment of Device-Related orthopaedic infections. Clin Orthop Relat R 2005; 437: 7–11. [DOI] [PubMed] [Google Scholar]
- 40.Puckett SD, Taylor E, Raimondo T, et al. The relationship between the nanostructure of titanium surfaces and bacterial attachment. Biomaterials 2010; 31: 706–713. [DOI] [PubMed] [Google Scholar]
- 41.Bhadra CM, Truong VK, Pham VTH, et al. Antibacterial titanium nano-patterned arrays inspired by dragonfly wings. Sci Rep 2015; 5: 16817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Levack AE, Cyphert EL, Bostrom MP, et al. Current options and emerging biomaterials for periprosthetic joint infection. Curr Rheumatol Rep 2018; 20: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pishbin F, Mouriño V, Gilchrist JB, et al. Single-step electrochemical deposition of antimicrobial orthopaedic coatings based on a bioactive glass/chitosan/nano-silver composite system. Acta Biomater 2013; 9: 7469–7479. [DOI] [PubMed] [Google Scholar]
- 44.Sullivan MP, McHale KJ, Parvizi J, et al. Nanotechnology. Bone Jt J 2014; 96-B: 569–573. [DOI] [PubMed] [Google Scholar]
- 45.Trauner KB. The emerging role of 3D printing in arthroplasty and orthopedics. J Arthroplasty 2018; 33: 2352–2354. [DOI] [PubMed] [Google Scholar]
- 46.Muirhead-Allwood S, Sandiford N, Skinner JA, et al. Uncemented custom computer-assisted design and manufacture of hydroxyapatite-coated femoral components. J Bone Joint Surg Br 2010; 92: 1079–1084. [DOI] [PubMed] [Google Scholar]
- 47.Dessyn E, Flecher X, Parratte S, et al. A 20-year follow-up evaluation of total hip arthroplasty in patients younger than 50 using a custom cementless stem. Hip Int 2018; 29: 112070001880329. [DOI] [PubMed] [Google Scholar]
- 48.Murr LE, Gaytan SM, Martinez E, et al. Next generation orthopaedic implants by additive manufacturing using electron beam melting. Int J Biomater 2012; 2012: 245727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Arabnejad S, Johnston B, Tanzer M, et al. Fully porous 3D printed titanium femoral stem to reduce stress-shielding following total hip arthroplasty. J Orthop Res 2017; 35: 1774–1783. [DOI] [PubMed] [Google Scholar]
- 50.Martino ID, Strigelli V, Cacciola G, et al. Survivorship and clinical outcomes of custom triflange acetabular components in revision total hip arthroplasty: a systematic review. J Arthroplast Epub ahead of print 2019; DOI:DOI: 10.1016/j.arth.2019.05.032. [DOI] [PubMed]
- 51.Clement ND, Deehan DJ, Patton JT. Robot-assisted unicompartmental knee arthroplasty for patients with isolated medial compartment osteoarthritis is cost-effective. Bone Joint J 2019; 101-B: 1063–1070. [DOI] [PubMed] [Google Scholar]
- 52.Chai W, Guo R, Puah KL, et al. Use of robotic‐arm assisted technique in complex primary total hip arthroplasty. Orthop Surg 2020; 12: 686–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lawson JA, Garber AT, Stimac JD, et al. Does robotic-assisted total hip arthroplasty improve accuracy of cup positioning? J Hip Surg 2019; 03: 176–180. [Google Scholar]
- 54.Illgen RL, Bukowski BR, Abiola R, et al. Robotic-Assisted total hip arthroplasty: outcomes at minimum two-year follow-up. Surg Technology Int 2017; 30: 365–372. [PubMed] [Google Scholar]
- 55.Bell SW, Anthony I, Jones B, et al. Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty. J Bone Jt Surg 2016; 98: 627–635. [DOI] [PubMed] [Google Scholar]
- 56.Lonner JH, Fillingham YA. Pros and cons: a balanced view of robotics in knee arthroplasty. J Arthroplasty 2018; 33: 2007–2013. [DOI] [PubMed] [Google Scholar]
- 57.Rahman J, Al-Tawil K, Khan WS. General principles of. Orthopedics and Trauma 2019; ▪: 629–637. [Google Scholar]
- 58.Volpin A, Maden C, Konan S. 23 New advances in robotic surgery in hip and knee replacement. Handb Robotic Image-Guided Surg 2020; ▪: 397–410. [Google Scholar]
- 59.Hampp EL, Chughtai M, Scholl LY, et al. Robotic-Arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques. J Knee Surg 2019; 32: 239–250. [DOI] [PubMed] [Google Scholar]
- 60.Shalhoub S, Lawrence JM, Keggi JM, et al. Imageless, robotic-assisted total knee arthroplasty combined with a robotic tensioning system can help predict and achieve accurate postoperative ligament balance. Arthroplast Today 2019; 5: 334–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bukowski BR, Anderson P, Khlopas A, et al. Improved functional outcomes with robotic compared with manual total hip. Arthroplasty Surg Technology Int : XXIX. [PubMed]
- 62.Sultan AA, Piuzzi N, Khlopas A, et al. Utilization of Robotic-Arm assisted total knee arthroplasty for soft tissue protection. Expert Rev Med Devices 2017; 14: 925–927. [DOI] [PubMed] [Google Scholar]
- 63.Karunaratne S, Duan M, Pappas E, et al. The effectiveness of robotic hip and knee arthroplasty on patient-reported outcomes: a systematic review and Meta-analysis. Int Orthop 2019; 43: 1283–1295. [DOI] [PubMed] [Google Scholar]
- 64.Zhang F, Li H, Ba Z, et al. Robotic arm-assisted vs conventional unicompartmental knee arthroplasty: a Meta-analysis of the effects on clinical outcomes. Medicine 2019; 98: e16968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Moschetti WE, Konopka JF, Rubash HE, et al. Can Robot-Assisted unicompartmental knee arthroplasty be Cost-Effective? a markov decision analysis. J Arthroplast 2016; 31: 759–765. [DOI] [PubMed] [Google Scholar]