Pneumomediastinum is an uncommon complication of acute respiratory distress syndrome (ARDS) from viral infections, including severe acute respiratory syndrome coronavirus 1 (1). Barotrauma from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (i.e., coronavirus disease [COVID-19]) has been increasingly described (2, 3).
We report five patients with pneumomediastinum of 92 critically ill, mechanically ventilated adults with ARDS from COVID-19 at our institution from March 1, 2020, through August 31, 2020 (Figure 1). Unlike other reports (4, 5), no patient had pneumothorax or required tube thoracostomy at diagnosis, suggesting alveolar rupture occurred without disruption of visceral pleura. Pneumomediastinum developed between 24 hours before and 9 days after initiation of mechanical ventilation without evidence of tracheal injury or the use of recruitment maneuvers. Patients received low-Vt ventilation targeting plateau pressures <30 cm H2O to minimize driving pressure, with sedation and/or paralysis used to reduce initial high respiratory effort and limit dyssynchrony. Our cumulative incidence (5.4%) of pneumomediastinum without pneumothorax falls between incidences reported in other series (2, 3). All patients later developed other barotrauma days after initial diagnosis, including two patients who developed pneumopericardium and one who developed pneumoperitoneum with severe subcutaneous emphysema from the neck to the pelvis (Figure 2). Four of the five patients died during hospitalization, with the remaining patient being discharged alive.
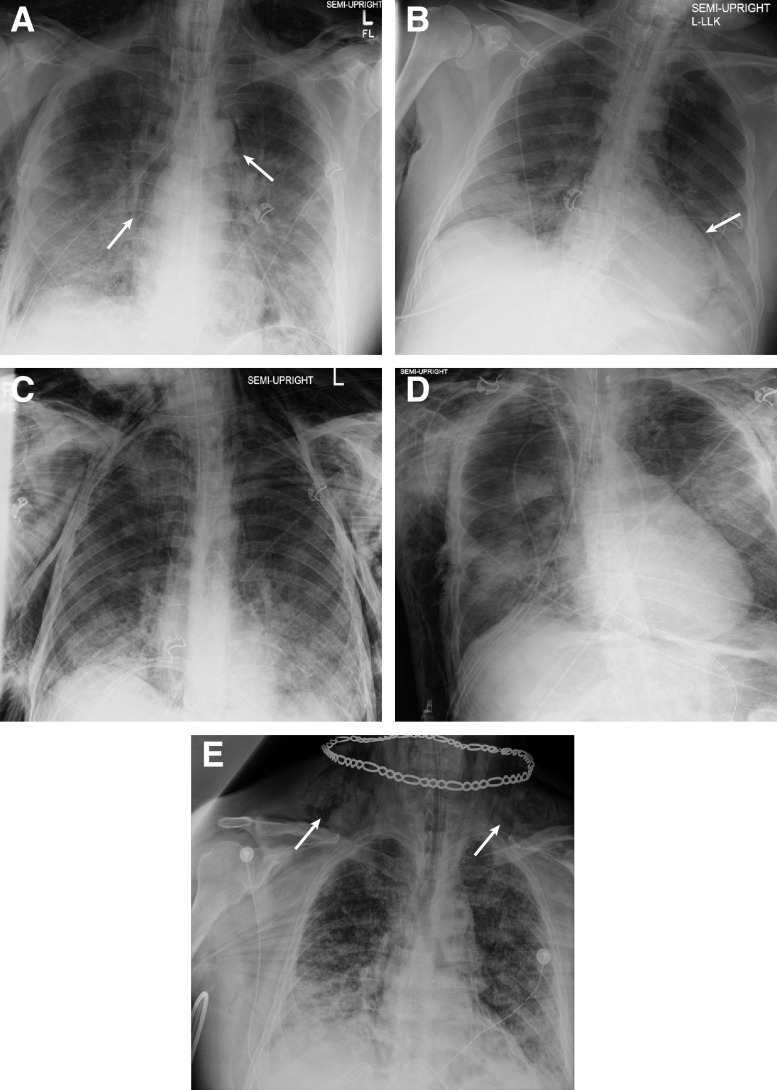
Figure 1.
Chest radiographs from five patients with coronavirus disease (COVID-19) acute respiratory distress syndrome who developed pneumomediastinum. (A) A 55-year-old man with pneumomediastinum (arrows) and pneumopericardium. (B) A 58-year-old man with pneumomediastinum and significant pneumopericardium (arrow). (C) A 43-year-old man with extensive subcutaneous emphysema and pneumomediastinum. (D) A 54-year-old man with pneumomediastinum and extensive subcutaneous emphysema notable in right axilla and across right chest wall. (E) A 61-year-old man with pneumomediastinum and significant supraclavicular subcutaneous emphysema (arrows). This patient had evidence of pneumomediastinum 24 hours before endotracheal intubation. L = left.
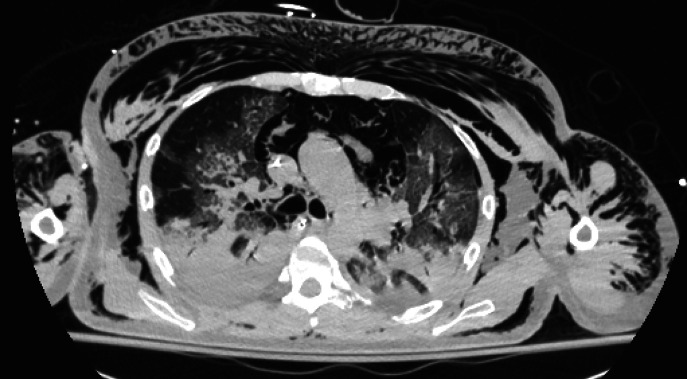
Figure 2.
Noncontrast computed tomographic chest image of a 54-year-old man with coronavirus disease (COVID-19) acute respiratory distress syndrome (ARDS). Extensive bilateral ground glass opacification and consolidation is present, consistent with his known ARDS. Significant pneumomediastinum is demonstrated in addition to extensive subcutaneous emphysema across the chest, arms, and back. Subcutaneous emphysema in this patient extended cephalad into the neck and caudally to the level of the pelvis and scrotum.
Supplementary Material
Footnotes
Author Contributions: M.F.M. and M.J.N. are responsible for the initial draft of this manuscript. All authors provided substantial contributions to the conception of the work as well as critical revision for the initial draft and the revised draft. All authors also provided final approval for this manuscript.
Originally Published in Press as DOI: 10.1164/rccm.202008-3376IM on November 20, 2020
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Chu CM, Leung YY, Hui JY, Hung IF, Chan VL, Leung WS, et al. Spontaneous pneumomediastinum in patients with severe acute respiratory syndrome. Eur Respir J. 2004;23:802–804. doi: 10.1183/09031936.04.00096404. [DOI] [PubMed] [Google Scholar]
- 2.McGuinness G, Zhan C, Rosenberg N, Azour L, Wickstrom M, Mason DM, et al. High incidence of barotrauma in patients with COVID-19 infection on invasive mechanical ventilation. Radiology. doi: 10.1148/radiol.2020202352. [online ahead of print] 2 Jul 2020; DOI: 10.1148/radiol.2020202352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martinelli AW, Ingle T, Newman J, Nadeem I, Jackson K, Lane ND, et al. COVID-19 and pneumothorax: a multicentre retrospective case series. Eur Respir J. 2020;9:2002697. doi: 10.1183/13993003.02697-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wali A, Rizzo V, Bille A, Routledge T, Chambers AJ. Pneumomediastinum following intubation in COVID-19 patients: a case series. Anaesthesia. 2020;75:1076–1081. doi: 10.1111/anae.15113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Udi J, Lang CN, Zotzmann V, Krueger K, Fluegler A, Bamberg F, et al. Incidence of barotrauma in patients with COVID-19 pneumonia during prolonged invasive mechanical ventilation - a case-control study. J Intensive Care Med. doi: 10.1177/0885066620954364. [online ahead of print] 22 Sep 2020; DOI: 10.1177/0885066620954364. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.