Abstract
Amid the current pandemic of coronavirus disease 2019 (COVID-19), orthopaedic surgery was one of the fewer specialties that remained active managing emergent and urgent orthopaedic and trauma cases. On the other hand, with the continued spread of this pandemic and its associated socioeconomic confinement and unpredictability of the pandemic curve; many health care facilities were forced into halting all elective and non-urgent activities including orthopaedic specialties. This in part was to help in reallocation of required resources and focusing on the proper management of COVID-19 patients, and to prevent the transmission of infection among health care workers and patients. In this article we analyzed developments and recommendations of international reports about the current outbreak and its impact on the practice of orthopaedic surgery. Our aim was to provide comprehensive and easy guidelines for the management of urgent and emergent cases in hot zones and for the process of returning to usual orthopaedic work flow in a balanced strategy to assure safe practice and providing quality care without the risk of exhausting institutional resources or the risk of COVID- 19 transmission among health care workers or patients.
Key words: Clinical guidelines, orthopaedics, practice settings
Introduction
In the era of the current outbreak of the novel coronavirus disease (COVID-19) and its link to The Severe Acute Respiratory Distress Syndrome Coronavirus 2 (SARSCoV2), no health care system has been immune from its burden.
On March 11, 2020, the World Health Organization (WHO) declared a global pandemic as the spread of COVID-19 was seen in more than 100 countries around the world.1 Since then, the number of newly diagnosed cases has risen by more than 30 fold with a total number exceeding twenty million patients.2 As a result, several countries had ordered a shutdown of all elective surgeries and outpatient visits.3,4 This, in part was to reallocate possible resources to the management and treatment of the overwhelming increasing numbers of COVID- 19 patients, and to prevent spread of the disease in such facilities.3,5
The modes of spread of the novel corona virus are thought to be through respiratory droplets or secretions of infected individuals as the predominant human to human source.6 A work by Van Doremalen et al. showed that the virus can remain viable and infectious in aerosols for hours and on surfaces up to days.7 This makes the production of aerosols during surgery by surgical incisions, by using electrocautery, drilling/reaming of bone or during wound irrigation, a plausible source of infection.8 Another worrisome issue is the spread of infection from asymptomatic carriers during the incubation period;9,10 in a study by Nishiura et al. they estimated about 41.6% of COVID-19 infected patients to be asymptomatic.10 This makes screening of patients by symptoms somewhat challenging in recognizing potential risks of infection transmission. Of more importance, is the possibility of working healthcare providers to spread the disease unknowingly. The American Academy of Orthopaedic Surgery (AAOS) has adopted the recommendations on delaying elective surgeries and provided a list of updated best practice for variant orthopaedic procedures.11 Orthopaedic surgeons should be fully aware and prepared for dealing with this pandemic as one of the fewer specialties which remained active during this time for the purpose of managing acute and emergency orthopedic cases. Furthermore, several institutions has resumed outpatients clinics and elective surgeries and there is the possibility of others to follow in the near future. We aimed by this article to establish clear guidelines for the practicing orthopaedic surgeons to maximize the proposed outcomes and minimize the potential risk of COVID-19 spread among orthopaedic patients.
General rules
Applying the recommended strategies for prevention of infection spread has become a norm for both public and health care professionals. These strategies include: social distancing, regular and thorough personal and respiratory hygiene, self-isolation and community containment.12 Although these strategies won’t reduce the expected absolute number of COVID 19 infections, with the lack of effective vaccine, it will help the effort of flattening the pandemic curve.5,13,14 Kenyon et al. performed an ecological analysis of the potential effect of pandemic curve flattening for 65 countries and found that these strategies will reduce the probability of hospitals and health care facilities being over-run and decrease the likelihood of sub-optimal care which will result in lowering the fatality rates.13
With the unpredictable behavior of pandemics and the possibility of a second wave of COVID-19 spread, health care systems should plan for a sustained system strategy that is adaptable for possible changes in the course of the current pandemic.14 This may include re-allocation of resources, establishing pandemics separate isolation and treatment facilities, risk factors linked screening strategy and remote triage and prioritizing provided services.
Inpatient trauma and emergent cases management
The implementation of social distancing, lock down and stay-home recommendations have played a role in reducing the trauma load slightly.15 Furthermore, many health care agencies recommended the limitation of inpatient care for emergencies only.3,16 This can be extended to trauma cases in which management can be delayed without considerable risk of mortality or significant morbidity. The knowledgeable decision making of the orthopaedic surgeon has a paramount importance in maintaining the balance between providing optimal care without exhausting the health care facility resources.
It is recommended to screen all patients undergoing surgical intervention.15,16 It is also recommended to have separate operating rooms for COVID-19 patients and non- COVID-19 patients.15-18 In cases where delayed surgical intervention is not possible until the retrieval of COVID-19 test results, decision to treat as positive patient should be considered. This will reduce the possibility of transmission to health care workers and other patients.15,18
Schwartz et al. recommended the “teams work strategy”, each team consisting of the minimum number of personnel needed to maintain the work flow. Two or more teams can be created and remain completely distinct to avoid possible cross transmission between the teams. Teams will work in 2 weeks cycle to cover the incubation period of COVID-19.19 This system allows for adherence to each hospital requirement for providing optimal care by each team and minimizes the risk of health care worker’s wide illness. The off-duty team can use remote working technologies (Telehealth) managing remote follow ups to reduce the burden on the active team or health care system.16
Operating on confirmed or potential COVID-19 patients should preferably be performed in negative pressure rooms or available rooms may be equipped with high efficiency particulate air (HEPA) filters. 15,20,21 It is presumed that HEPA filters with high frequency of air changes can reduce the viral load disseminated through the operating room OR significantly.22 Regional or peripheral blocks should be utilized if possible to avoid aerosols spread during intubation or extubation. If general anesthesia is the preferable choice, intubation/ extubation should be performed in a separate area or before the surgeon enters the room. The surgery should be performed with the fewest number of involved personnel in the OR and minimizing traffic in and out of the room as possible.17-19,21
Surgical staff working in COVID19 dedicated OR room should follow a clear institution protocol that provides maximum protection from disease transmission. Pinto et al. suggested a five-zones work flow areas; each zone marked with clear signs and equipped with appropriate materials such as PPE and marked wastebaskets.21 Figure 1. Summarizes instructions appropriate for each zone and steps for the surgical staff to follow to minimize the risk of nosocomial disease transmission.
Inpatient elective surgeries
The decision on resuming elective orthopaedic surgeries should judiciously depend on the institution or area status on the pandemic curve, availability of resources including: PPE, surgical staff, ICU beds and respirators, and the effectiveness and availability of screening tools at the institute.11,16
Prioritizing surgical cases is of paramount importance in the process of resuming non-urgent or emergent surgeries. In the process of progressive start-up phase, urgent-somewhat elective cases should be considered first. This may include anterior cruciate ligament tears, bucket handle meniscus, acute traumatic rotator cuff tears, biceps injuries and delayed nonemergent fracture cases.16,23 Elective cases, that are labeled as chronic problems that can be delayed with no significant potential harm to patient or clinical outcome, can be given a second priority until a higher level of safety for the patient and resources can be guaranteed. 16,23 It is also reasonable to further delay patients with higher risk of developing severe acute respiratory distress syndrome of coronavirus 2 (SARS-CoV 2) if infected. This includes patients with pre-existing respiratory conditions, obese patients and patients with diabetes.23,24
Figure 1.
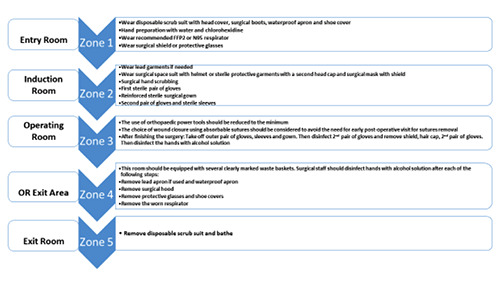
Work flow in the operating theater of confirmed or potential COVID-19 patients.
A general consensus has been formed that all patients should be screened for symptoms and tested for COIVD-19 before surgical intervention.16,23 Telehealth communication with potential patients can be utilized for symptoms screening. The Center of Disease Control recognizes fever, shortness of breath, cough, sore throat, malaise, muscle pain and new loss of taste or smell as potential symptoms of COVID-19.25 It is wise that any patient that expressed or showed flu like symptoms should not be passed on to the short list for surgery.
The AAOS recommends testing all patients planned for surgery 1-3 days prior to the scheduled date for COVID 19 using reverse trascriptase polymerase chain reaction (RT-PCR) or Enzyme- Linked Immunosorbent Assay (ELISA) antibody test.16 However, it is important to understand and educate the patient about the rate of false-negative tests to avoid the feeling of false security. Patients returned with a positive test should be delayed and not operated on for a minimum of three weeks and return of two negative COVID-19 tests at least 24 hours a part.23 Figure 2 represents a flowchart in triaging orthopaedic cases and managing work flow in accordance with institution resources.
We emphasize on applying the general rules for prevention of disease transmission including: appropriate distancing between patients, proper education about personal and respiratory hygiene and minimizing hospital stay to avoid nosocomial disease transmission. Moreover, protecting surgical staff is crucial using standard PPE, promoting the use of local and regional anesthesia and avoiding open air intubation/extubation if general anesthesia is performed. It is also important to reduce the use of aerosoles generating equipment and applying continuous suction in the surgical field.
Outpatient clinics
Recently a debate has surfaced on the transmission of COVID-19 from asymptomatic patients. Several reports linked asymptomatic COVID-19 as potential disease spreaders.10,26,27 Oran et al. reported that asymptomatic individuals accounts for 40% of SARS-Cov2 patients and may transmit the disease to others for an extended period of more than 14 days.26 The WHO however, reported that it is rare for an asymptomatic patient to be contagious.28 On a second report WHO clarified that pre-symptomatic patients, who develop symptoms later in the course of the disease, may still be contagious during the pre-symptomatic phase.29
With the lack of clear evidence and conflicting reports on disease transmission from asymptomatic individuals, it is crucial for both health care workers and the community to create a high level of awareness and adherence to transmission prevention measures. It is also important to limit the number of personnel present in the vicinity to the minimum, use remote communication methods for patients screening and triage, reduce the frequency of patient’s follow up visits, if possible, and implement clear staged process for patients attending the clinics.
Furthermore, it is recommended to test service providers in the outpatient clinics before resuming work and contact with patients to ensure that they won’t be a potential source of spread. A questionnaire that identifies patients with high risk for infection or potential infection can help scheduling patients with risk factors in time slots to allow for a 14 days’ self-quarantine before visiting the clinic. Such questionnaire should include questions identifying patients with symptoms of COVID-19, travel to COVID-19 hot zones within the last 14 days, direct contact with confirmed COVID-19 patients or health care workers managing COVID-19 cases in the last 14 days and living in a nursing home or assisted living facilities. It is also important to identify patients with underlying comorbidities with a higher risk of developing SARS-CoV 2. Upon entering the clinic, patient’s temperature should be taken and symptomatic patients may be sent to an allocated clinic for further evaluation. Patients need to be instructed about wearing disposable masks to reduce the likelihood of transmission of aerosols with special attention to limiting crowds and applying social distancing in the waiting areas. Clinical evaluation should be performed in a quick effective way; the subjective part of the clinical assessment such as history taking, can be done through a digital interface to limit the interaction between the patient and the medical staff. Follow up visit scheduling and payment can also be performed using a digital interface to minimize the contact between patients and administrative personnel. Figure 3 illustrates a safe plan to manage the return to work in outpatient’s clinics.
Figure 2.
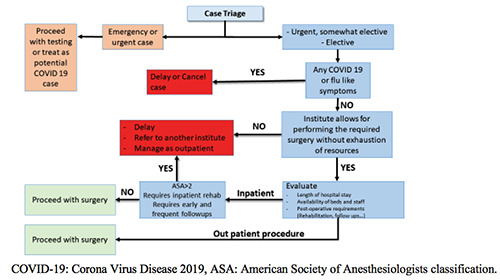
Managing orthopaedic cases in the era of COVID-19.
Figure 3.
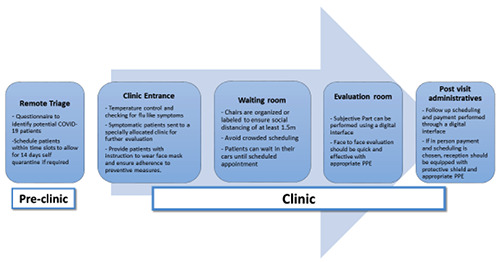
Plan for return to outpatient’s clinic work.
Conclusions
The current COVID-19 pandemic has a dual impact on the practice of orthopaedic surgery. In one way, orthopaedic surgeons have the responsibility of managing trauma cases for SARS-COV2 patients at facilities that are either scarce resources or overwhelmed with the number of patients. On the other hand, this pandemic halted the work flow for elective surgeries and outpatient clinics leading to accumulation of cases, which in turn needs more organization as hospitals resume work. In this article we propose comprehensive guidelines for the orthopaedic surgeon to maintain a safe and effective practice in the era of this pandemic. These guidelines consider the current recommendations and developments of this outbreak. We acknowledge that following the proposed guidelines will increase the cost of care provided. However, we think modification of baseline guidelines is possible to suit institutes with limited space, staffing or resources.
Funding Statement
Funding: None.
References
- 1.World Health Organization. (2020). WHO director-general’s opening remarks at the media briefing on covid- 19-11 march 2020. 2020. Available form: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-oncovid-19---11-march-2020. [Google Scholar]
- 2.COVID-19 Corona virus pandemic (2020) worlds meters info. https://www.worldometers.info/coronavirus. Accessed 10 August 2020 [Google Scholar]
- 3.American College of Surgeons (ACS). COVID-19 update: guidance for triage of non-emergent surgical procedures. 2020. Available from: https://www.facs.org/covid-19/clinical-guidance/triage. Accessed 6 June 2020 [Google Scholar]
- 4.Commins J. Surgeon general urges providers to consider stopping all elective surgeries–hospitals push back. Health Leaders. March 16, 2020. [Google Scholar]
- 5.Spina S, Marrazzo F, Migliari M, et al. The response of Milan’s Emergency Medical System to the COVID-19 outbreak in Italy. Lancet 2020;395:e49–e50. doi: 10.1016/S0140-6736(20)30493-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peeri NC, Shrestha N, Rahman MS, et al. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol 2020;49:717-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.VanDoremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020;382: 1564-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yeh HC, Turner RS, Jones RK, et al. Characterization of aerosols produced during surgical procedures in hospitals. Aerosol Sci Technol 1995;22:151-61. [Google Scholar]
- 9.Gandhi M, Yokoe DS, Havlir DV. Asymptomatic transmission, the Achilles’ heel of current strategies to control COVID-19. N Engl J Med 2020;382:2158-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nishiura H, Kobayashi T, Miyama T, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). MedRxiv 2020. doi: 10.1101/2020.02.03.20020248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American College of Surgeons. COVID 19 guidelines for triage of orthopaedic patients. https://www.facs.org/covid-19/clinical-guidance/elective-case/orthopaedics Accessed 13 June 2020. [Google Scholar]
- 12.Hou C, Chen J, Zhou Y, et al. The effectiveness of quarantine of Wuhan city against the Corona Virus Disease 2019 (COVID-19): A well-mixed SEIR model analysis. J Med Virol 2020;92:841-8. doi: 10.1002/jmv. 25827. [DOI] [PubMed] [Google Scholar]
- 13.Kenyon C. Flattening-the-curve associated with reduced COVID-19 case fatality rates-an ecological analysis of 65 countries. J Infect 2020;81:e98-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Friston KJ, Parr T, Zeidman P, et al. Second waves, social distancing, and the spread of COVID-19 across America. arXiv preprint 2020. arXiv:2004.13017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stinner DJ, Lebrun C, Hsu JR, et al. The orthopaedic trauma service and COVID-19: practice considerations to optimize outcomes and limit exposure. J Orthop Trauma 2020;34:333-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Academy of Orthopaedic Surgeons. Navigating the COVID 19 Pandemic. https://www.aaos.org/globalassets/about/covid-19/aaos-clinicalconsiderations-during-covid-19.pdf Accessed on 14 June 2020. [Google Scholar]
- 17.Ambrosio L, Vadalà G, Russo F, et al. The role of the orthopaedic surgeon in the COVID-19 era: cautions and perspectives. J Exper Orthop 2020;7:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mi B, Chen L, Xiong Y, et al. Characteristics and early prognosis of COVID-19 infection in fracture patients. J Bone Joint Surg Am 2020;102:750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwartz AM, Wilson JM, Boden SD, et al. Managing resident workforce and education during the COVID-19 pandemic: evolving strategies and lessons learned. JBJS Open Access 2020;5: e0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chow TT, Kwan A, Lin Z, Bai W. Conversion of operating theatre from positive to negative pressure environment. J Hosp Infect 2006;64:371-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rodrigues-Pinto R, Sousa R, Oliveira A. Preparing to perform trauma and orthopaedic surgery on patients with COVID-19. J Bone Joint Surg Am 2020;102:946-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perry JL, Agui JH, Vijayakimar R. Submicron and nanoparticulate matter removal by HEPA-rated media filters and packed beds of granular materials. NASA Technical Reports Server. 2016. [Google Scholar]
- 23.de Caro F, Hirschmann TM, Verdonk P. Returning to orthopaedic business as usual after COVID-19: strategies and options. Knee Surgery, Sports Traumatology, Arthroscopy, 2020;1:28: 1699-704. [Google Scholar]
- 24.Dreher M, Kersten A, Bickenbach J, et al. The characteristics of 50 hospitalized COVID-19 patients with and without ARDS. Deutsches Ärzteblatt International 2020;117:271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. Symptoms of Coronavirus. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html Accessed on 14 June 2020. [Google Scholar]
- 26.Oran DP, Topol EJ. Prevalence of Asymptomatic SARS-CoV-2 Infection: A Narrative Review. Ann Int Med 2020; 173:362-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Day M. Covid-19: identifying and isolating asymptomatic people helped eliminate virus in Italian village. BMJ 2020;368. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. Transmission of COVID 19 by asymptomatic cases. http://www.emro.who.int/health-topics/corona-virus/transmission-of-covid-19-by-asymptomaticcases.html Accessed on 14 June 2020. [Google Scholar]
- 29.World Health organization. WHO clarifies comments on asymptomatic COVID 19 spread. https://www.webmd.com/lung/news/20200609/whoclairifies-comments-on-asymptomaticcovid-spread Accessed on 14 June 2020. [Google Scholar]


