Abstract
Aim: The present study aims to investigate the association between serum small dense low-density lipoprotein (sdLDL) cholesterol level and the development of coronary heart disease (CHD) in subjects at high cardiovascular risk.
Methods: A total of 3,080 participants without prior cardiovascular disease (CVD), aged ≥ 40 years, were followed up for a median of 8.3 years, which were divided into two groups, those with serum sdLDL cholesterol levels of < 35 mg/dL or ≥ 35 mg/dL. Then, subjects were stratified by the status of diabetes, CVD-related comorbidities (defined as the presence of diabetes, chronic kidney disease, or peripheral artery disease), and the CVD risk assessment according to the Japan Atherosclerosis Society Guidelines. The hazard ratios (HRs) and 95% confidence intervals (CIs) were computed using a Cox proportional hazards model.
Results: During the follow-up, 79 subjects developed CHD. The risk for incident CHD was higher in subjects with serum sdLDL cholesterol of ≥ 35 mg/dL than those with sdLDL cholesterol of < 35 mg/dL (HR 2.09, 95%CI 1.26–3.45) after adjusting for traditional risk factors. In the subgroup analyses, the multivariable-adjusted HR for incident CHD increased significantly in those with serum sdLDL cholesterol of ≥ 35 mg/dL among subjects with diabetes (HR 2.76, 95%CI 1.09–7.01), subjects with CVD-related comorbidities (HR 2.60, 95%CI 1.21–5.58), and high-risk category defined as the presence of CVD-related comorbidities or a Suita score of ≥ 56 points (HR 1.93, 95%CI 1.02–3.65).
Conclusions: Elevated serum sdLDL cholesterol was associated with the development of CHD even in subjects at high cardiovascular risk.
Keywords: Small dense LDL cholesterol, Coronary heart disease, Risk assessment, Prospective study, High-risk population
Introduction
Coronary heart disease (CHD) is a common noncommunicable disease and one of the leading causes of mortality worldwide. According to a report from the Global Burden of Diseases study, in 2017, there were 8.93 million deaths from CHD, and CHD was the leading cause of years of life lost1). In Japan, heart disease is the second leading cause of death in 2017, with CHD accounting for over 30% of heart disease deaths2). Hence, preventing the development of CHD is a highly important issue in contemporary and future public health on a global scale.
Previous observational studies and clinical trials have revealed that serum low-density lipoprotein (LDL) cholesterol is a significant risk factor for the development of CHD3). The Guidelines for the Prevention of Atherosclerotic Cardiovascular Disease 2017 from the Japan Atherosclerosis Society recommend monitoring and intervention on LDL cholesterol for primary prevention of atherosclerotic cardiovascular disease (CVD), of which target levels of LDL cholesterol-lowering treatment are categorized according to the absolute risk of CHD estimated by the Suita score, a risk index used to estimate the 10-year risk of CHD for the Japanese population4–5).
Recently, the difference in the atherogenic effect across differently sized LDL particles has attracted attention. In particular, small dense LDL (sdLDL), which is small in size and highly dense, has been shown to have more atherogenic effect than other LDL particles6–8). Several prospective cohort studies have reported the significant association between serum sdLDL cholesterol and the development of CHD regardless of serum LDL cholesterol levels9–11). Our study group also reported a significant association between serum sdLDL cholesterol and the development of CHD in a general Japanese population; the cutoff value of sdLDL cholesterol for discriminating the risk of developing CHD was around 35 mg/dL12). However, it is still unknown whether the association between sdLDL cholesterol and CHD is observed even in individuals at high cardiovascular risk. It is of particular importance to investigate the association in subpopulations with varied cardiovascular risks to evaluate clinical usefulness of measuring sdLDL in routine care settings.
Aim
The present study aims to clarify the association between sdLDL cholesterol and CHD among Japanese general population stratified by predefined CHD risks using the risk stratification algorithm of the Japan Atherosclerosis Society 2017 Guidelines.
Methods
Study Population
A detailed description of the Hisayama study was published previously13). Briefly, a total of 3,384 residents aged 40 years or older (78.2% of the total population of this age group) underwent the screening survey for the present study in 2007 and 2008. After excluding 8 subjects who did not consent to participate in the study, 223 subjects who had past history of stroke or CHD, and 73 subjects for whom serum sdLDL cholesterol data were lacking, the remaining 3,080 subjects (1,290 men and 1,790 women) were enrolled in the present study.
The study was approved by the Kyushu University Institutional Review Board for Clinical Research, and written informed consent was obtained from all participants.
Follow-Up Survey
The subjects were followed up prospectively until November 2015 or their death (median, 8.3 years) by annual health examinations or by mail or telephone for any subject who did not undergo the examination or who moved out of the town as described previously14). The development of CHD was also checked by a daily monitoring system organized by the study team, local physicians, and members of the Health and Welfare Office of the town. Subjects with suspected CHD events were evaluated on the basis of all available clinical information, and their diagnoses were adjudicated by study team physicians. When a subject died, an autopsy was performed at the Department of Pathology of Kyushu University, if consent for autopsy was obtained. During the follow-up period, autopsy examination was performed for 192 (57.8%) of 332 deceased subjects. In addition to the deceased cases, four subjects were lost to follow up, all of whom were subjects who moved out of the town.
Small Dense Low-Density Lipoprotein Cholesterol Measurement
At the screening examination, portions of the plasma specimens were stored at −80°C until serum sdLDL cholesterol concentrations were measured in 2014 on a Hitachi 7180 automated chemistry analyzer using a homogeneous assay (sdLDL-EX "SEIKEN"; Denka Seiken, Tokyo)15). The subjects were divided into two groups, those with serum sdLDL cholesterol of < 35 and of ≥ 35 mg/dL, which is the cutoff value reported previously12).
Outcomes
The primary outcome of the present study was CHD. The criteria for the diagnosis of CHD included first-ever fatal and nonfatal myocardial infarction, silent myocardial infarction, sudden cardiac death within 1 hour after the onset of acute illness, coronary angioplasty, and bypass grafting. The diagnosis of myocardial infarction was based on detailed clinical information and at least two of the following findings: typical clinical symptoms, electrocardiogram (ECG) evidence of myocardial infarction, elevated cardiac enzymes, or morphologic findings, including echocardiographic, scintigraphic, or angiographic abnormalities compatible with myocardial injury, or myocardial necrosis or scars more than 1 cm in diameter at autopsy14, 16).
Other Variables
Information on medical history including the presence of peripheral artery disease; medication for hypertension, diabetes, and dyslipidemia; smoking habits; alcohol intake; and physical activity at baseline was obtained using a standard self-administered questionnaire and was checked by trained interviewers. Smoking and drinking habits were classified as either current use or not. Current smoking was defined as smoking at least one cigarette per day. Current drinking was defined as drinking at least one alcoholic beverage per month. The subjects engaging in sports or other forms of exertion ≥ 3 times a week during their leisure time made up a regular exercise group. Body height and weight were measured with the subjects in light clothing without shoes, and body mass index (BMI) was calculated (kg/m2). Blood pressure was measured three times in a sitting position using an automated sphygmomanometer (BP-203 RVIIIB; Omron Healthcare), and the mean of three measurements was used in the present analysis. Hypertension was defined as blood pressure ≥ 140/90 mmHg and/or current use of antihypertensive agents. ECG abnormalities were defined as left ventricular hypertrophy (Minnesota code 3-1), ST depression (4-1, 4-2, or 4-3), or atrial fibrillation/flutter (8-3). Blood samples were collected from an antecubital vein. Plasma glucose levels were measured by the hexokinase method. Diabetes mellitus was defined as a fasting plasma glucose level ≥ 126 mg/dL, 2-hour post load or casual glucose level of ≥ 200 mg/dL, or current use of glucose-lowering agents (i.e., oral glucose-lowering agents or insulin). Prediabetes was defined as a fasting plasma glucose level of 110 to 125 mg/dL and 2-hour post load glucose level of < 200 mg/dL or fasting plasma glucose level of < 126 mg/dL and 2-hour post load glucose level of 140 to 199 mg/dL. Hemoglobin A1c (HbA1c) was measured by latex aggregation immunoassay using a Determiner HbA1c kit (Kyowa Medex, Tokyo). Serum LDL cholesterol and high-density lipoprotein (HDL) cholesterol were measured enzymatically, and serum triglycerides were measured with colorimetric method. The estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation with a Japanese coefficient of 0.813, for which serum creatinine was measured enzymatically17). Chronic kidney disease was defined as eGFR < 60 mL/min/1.73 m2 or proteinuria (≥ 1+ on dipstick) according to the Kidney Disease Improving Global Outcomes guideline18).
Risk Assessments for Cardiovascular Disease
We performed the risk assessment for CVD according to the Guidelines for Prevention of Atherosclerotic Cardiovascular Disease 2017 from the Japan Atherosclerosis Society4) (Supplementary Fig. 1). CVD-related comorbidities were defined as the presence of diabetes, chronic kidney disease, and/or peripheral artery disease. First, subjects with CVD-related comorbidities were classified as a high-risk category. Next, the Suita scores were calculated with the variables of age, sex, smoking habits, blood pressure level, serum LDL and HDL cholesterol levels, and prediabetes among subjects without CVD-related comorbidities. Because data on family history of premature CHD were not available, 0 point was assigned to all participants. Subjects were classified into categories based on the total Suita score as follows: low-risk category (≤ 40 points), moderate-risk category (41–55 points), and high-risk category (≥ 56 points)4).
Supplementary Fig. 1.
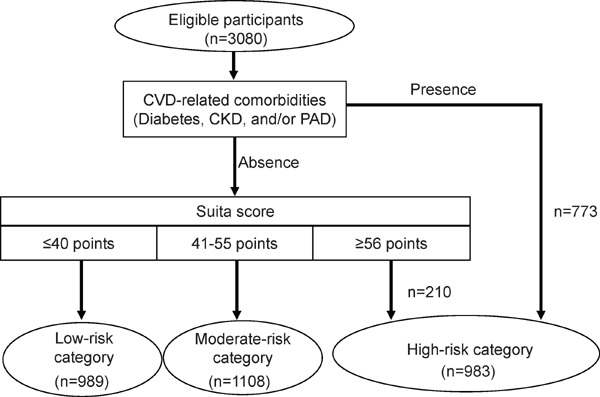
Flowchart of the risk assessment according to the guidelines from the Japan Atherosclerosis Society
Abbreviations: CKD, chronic kidney disease; CVD, cardiovascular disease; PAD, peripheral artery disease.
Suita score was calculated on the basis of the following risk factors at baseline for each participant: age, sex, smoking habits, blood pressure level, serum high-density lipoprotein cholesterol, serum low-density lipoprotein cholesterol, and prediabetes among subjects without CVD-related comorbidities. Eligible participants (n = 3,080) were selected from 3,384 study population, after excluding 8 subjects who did not consent to participate in the study, 223 subjects who had past history of CVD, and 73 subjects for whom serum sdLDL cholesterol data were lacking.
Statistical Analysis
The significance of differences in the mean values or frequencies of risk factors between subjects with sdLDL cholesterol of < 35 mg/dL and those with sdLDL cholesterol of ≥ 35 mg/dL was tested using Student's t test or the χ2 test, respectively. Serum triglyceride level was shown as median and interquartile range in the baseline characteristics, because of the skewed distribution. The incidence rate of CHD was calculated using the person-year method. The Cox proportional hazards model was used to estimate the hazard ratio (HR) and its 95% confidence intervals (CIs) for the development of CHD by subpopulations stratified by the status of (1) diabetes, (2) the CVD-related comorbidities, and (3) the CVD risk assessment. In the multivariable analysis, the risk estimates were adjusted for potential confounding factors at baseline—namely, age, sex, systolic blood pressure, use of antihypertensive agents, HbA1c, use of glucose-lowering agents, serum HDL cholesterol, lipid-modifying agents, BMI, eGFR, ECG abnormalities, current smoking, current drinking, and regular exercise. The heterogeneities in the association between subgroups were tested by adding multiplicative interaction terms to the relevant Cox model. A two-sided value of p < 0.05 was considered statistically significant in all analyses. Statistical analyses were conducted using Statistical Analysis Software version 9.4 (SAS Institute, Cary, NC).
Results
The baseline characteristics of the total study population and those with serum sdLDL cholesterol levels of less than 35 mg/dL and of 35 mg/dL or more are shown in Table 1. The mean values of systolic blood pressure, HbA1c, serum LDL cholesterol, serum non-HDL cholesterol, and eGFR; the median value of serum triglycerides; and the frequencies of male sex, diabetes, prediabetes, urinary protein, ECG abnormalities, current smoking, and current drinking were significantly higher in subjects with serum sdLDL cholesterol levels of ≥ 35 mg/dL compared to serum sdLDL cholesterol levels of < 35 mg/dL, whereas the mean values of age and serum HDL cholesterol were significantly lower.
Table 1. Baseline characteristics of overall subjects and characteristics according to small dense LDL cholesterol level.
| Variables | Overall subjects | Serum sdLDL cholesterol level |
p valuea | |
|---|---|---|---|---|
| < 35 mg/dL | ≥ 35 mg/dL | |||
| N | 3,080 | 1,728 | 1,352 | - |
| Age (years) | 63 (13) | 64 (14) | 62 (11) | < 0.001 |
| Men (%) | 41.9 | 36.1 | 49.3 | < 0.001 |
| Systolic blood pressure (mmHg) | 132 (19) | 129 (20) | 136 (18) | < 0.001 |
| Use of antihypertensive agents (%) | 29.5 | 29.4 | 29.7 | 0.87 |
| Diabetes (%) | 15.0 | 11.3 | 19.7 | < 0.001 |
| Prediabetes (%) | 23.1 | 18.5 | 29.1 | < 0.001 |
| HbA1c (%) | 5.5 (0.8) | 5.4 (0.7) | 5.6 (0.8) | < 0.001 |
| Use of glucose-lowering agents (%) | 6.5 | 6.0 | 7.1 | 0.23 |
| Serum LDL cholesterol (mg/dL) | 122 (32) | 107 (24) | 141 (30) | < 0.001 |
| Serum non-HDL cholesterol (mg/dL) | 142 (36) | 123 (26) | 167 (31) | < 0.001 |
| Serum HDL cholesterol (mg/dL) | 67 (18) | 72 (18) | 61 (16) | < 0.001 |
| Serum triglycerides (mg/dL)b | 100 (73.143) | 82 (62.107) | 136 (101.192) | < 0.001 |
| Use of lipid-modifying agents (%) | 13.9 | 14.7 | 12.9 | 0.14 |
| BMI (kg/m2) | 23 (4) | 22 (3) | 24 (3) | 0.68 |
| eGFR (ml/min/1.73 m2) | 75 (13) | 75 (13) | 76 (12) | < 0.001 |
| Urinary protein (%) | 5.9 | 5.2 | 6.9 | 0.046 |
| Chronic kidney disease (%) | 13.7 | 14.0 | 13.5 | 0.71 |
| Electrocardiogram abnormalities (%) | 15.3 | 14.2 | 16.8 | 0.046 |
| History of peripheral artery disease | 0.2 | 0.3 | 0.2 | 0.41 |
| Current smoking (%) | 19.9 | 16.6 | 24.3 | < 0.001 |
| Current drinking (%) | 47.6 | 42.8 | 53.9 | < 0.001 |
| Regular exercise (%) | 11.9 | 11.8 | 11.9 | 0.94 |
Abbreviations: BMI, body mass index; eGFR, estimated glomerular filtration rate; HbA1c, hemoglobin A1c; HDL, high-density lipoprotein; LDL, low-density lipoprotein; sdLDL, small dense low-density lipoprotein.
Data are presented as the mean values (standard deviation), percentages, or median (interquartile range).
The significance of differences in mean values and frequencies of risk factors between the level of sdLDL cholesterol were tested by Student's t test and chi-square test, respectively.
Only subjects with available fasting blood samples were included in the analysis using serum triglyceride (n = 3,056).
During the follow-up period, 79 subjects experienced a first-ever CHD event. The crude cumulative incidence of CHD was significantly higher in subjects with serum sdLDL cholesterol levels of ≥ 35 mg/dL than < 35 mg/dL (log-rank p < 0.001, Fig. 1). Table 2 demonstrates the age- and sex-adjusted and multivariable-adjusted HRs (95%CIs) of serum sdLDL cholesterol of ≥ 35 mg/dL against < 35 mg/dL for the development of CHD, in overall subjects and in the subgroups according to diabetic status, the presence or absence of CVD-related comorbidities (diabetes, chronic kidney disease, and/or peripheral artery disease), and the risk assessment status based on the guidelines from the Japan Atherosclerosis Society. In overall subjects, the age- and sex-adjusted HR for the development of CHD was 2.44 (95%CI, 1.52–3.90) for serum sdLDL cholesterol of ≥ 35 mg/dL as compared with serum sdLDL cholesterol of < 35 mg/dL. This association remained significant even after adjustment for age, sex, systolic blood pressure, use of antihypertensive agents, HbA1c, use of glucose-lowering agents, BMI, eGFR, ECG abnormalities, current smoking, current drinking, and regular exercise (HR 2.09, 95%CI 1.26–3.45). In the subgroup analysis, the multivariable-adjusted HRs for the development of CHD increased significantly in those with serum sdLDL cholesterol of ≥ 35 mg/dL compared to those with serum sdLDL cholesterol of < 35 mg/dL in both subjects with and without diabetes (without diabetes: HR 1.89, 95%CI 1.01–3.52; with diabetes: HR 2.76, 95%CI 1.09–7.01), in subjects with CVD-related comorbidities (HR 2.60, 95%CI 1.21–5.58), and in subjects in the high-risk category (HR 1.93, 95%CI 1.02–3.65). There was no evidence of significant heterogeneities in the association between these subgroups (all p for heterogeneity > 0.5). We also divided subjects into low-risk category and moderate-/high-risk category for the risk assessment status, and the multivariable-adjusted HR of the development of CHD was 5.77 (95%CI 0.25–133.23) among subjects in the low-risk category and 1.70 (95%CI 1.05–2.76) among subjects in the moderate-/high-risk category, without any evidence of heterogeneity between subgroups (p for heterogeneity = 0.77). When we focus on the results of the subjects in the high-risk category for the risk assessment status, the age- and sex-adjusted cumulative incidence of CHD was higher in subjects with serum sdLDL cholesterol levels of ≥ 35 mg/dL than those with < 35 mg/dL (p = 0.03, Supplementary Fig. 2).
Fig. 1.
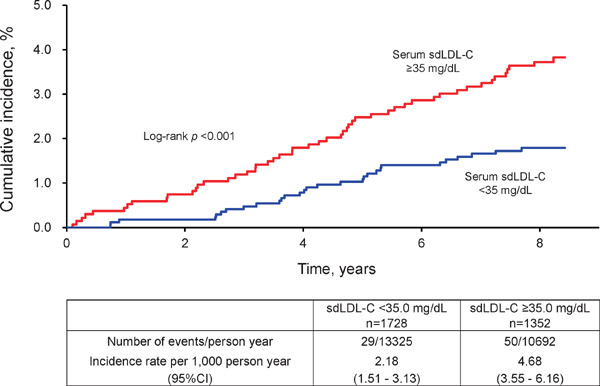
Crude cumulative incidence of coronary heart disease according to serum small dense low-density lipoprotein cholesterol
Abbreviations: sdLDL-C, small dense low-density lipoprotein cholesterol.
Table 2. Hazard ratios for the development of coronary heart disease according to serum small dense low-density lipoprotein cholesterol levels in subgroups of the status of cardiovascular risk.
| No. of events/subjects |
Crude incidence rate (per 1,000 person-years) |
HR (95%CI) of serum sdLDL-C ≥ 35 mg/dL vs. < 35 mg/dL. |
||||
|---|---|---|---|---|---|---|
| Serum sdLDL-C (mg/dL) |
Serum sdLDL-C (mg/dL) |
Age- and sex-adjusted | Multivariable-adjusted | |||
| < 35 | ≥ 35 | < 35 | ≥ 35 | |||
| Overall subjectsa | 29/1728 | 50/1352 | 2.18 | 4.68 | 2.44 (1.52–3.90) | 2.09 (1.26–3.45) |
| Diabetesb | ||||||
| Absence | 21/1533 | 29/1086 | 1.77 | 3.35 | 2.19 (1.23–3.90) | 1.89 (1.01–3.52) |
| Presence | 8/195 | 21/266 | 5.43 | 10.32 | 2.30 (0.999–5.29) | 2.76 (1.09–7.01) |
| p for heterogeneity | 0.81 | 0.87 | ||||
| CVD-related comorbiditiesc | ||||||
| Absence | 17/1340 | 25/967 | 1.61 | 3.22 | 2.35 (1.25–4.43) | 1.86 (0.94–3.69) |
| Presence | 12/388 | 25/385 | 4.32 | 8.5 | 2.21 (1.08–4.52) | 2.60 (1.21–5.58) |
| p for heterogeneity | 0.60 | 0.57 | ||||
| Risk assessment statusd | ||||||
| Low-/moderate-risk category | 14/1268 | 18/829 | 1.40 | 2.69 | 2.66 (1.28–5.55) | 2.02 (0.98–4.16) |
| high-risk category | 15/460 | 32/523 | 4.54 | 7.99 | 1.99 (1.05–3.76) | 1.93 (1.02–3.65) |
| p for heterogeneity | 0.90 | 0.89 | ||||
| Low-risk category | 1/707 | 1/282 | 0.17 | 0.43 | 4.02 (0.21–75.58) | 5.77 (0.25–133.23) |
| Moderate-/high-risk category | 28/1021 | 49/1070 | 3.71 | 5.85 | 2.04 (1.25–3.31) | 1.70 (1.05–2.76) |
| p for heterogeneity | 0.86 | 0.77 | ||||
Abbreviations: CI, confidence interval; HR, hazard ratio; sdLDL-C, small dense low-density lipoprotein cholesterol
For the analysis in the overall subjects, age, sex, systolic blood pressure, use of antihypertensive agents, hemoglobin A1c, use of glucose-lowering agents, serum high-density lipoprotein cholesterol, use of lipid-modifying agents, body mass index, estimated glomerular filtration rate, electrocardiogram abnormalities, current smoking, current drinking, and regular exercise were included in the relevant Cox model as covariates.
For the subgroup analysis of diabetic status, age, sex, systolic blood pressure, use of antihypertensive agents, serum high-density lipoprotein cholesterol, use of lipid-modifying agents, body mass index, estimated glomerular filtration rate, electrocardiogram abnormalities, current smoking, current drinking, and regular exercise were included in the relevant Cox model as covariates.
CVD-related comorbidities were defined as the presence of diabetes, chronic kidney disease, and/or peripheral artery disease. For the subgroup analysis of the status of CVD-related comorbidities, age, sex, systolic blood pressure, use of antihypertensive agents, serum high-density lipoprotein cholesterol, use of lipid-modifying agents, body mass index, electrocardiogram abnormalities, current smoking, current drinking, and regular exercise were included in the relevant Cox model as covariates.
For the risk assessment status were classified according to the guideline from Japan Atherosclerosis Society. For the subgroup analysis of the risk assessment status, use of antihypertensive agents, use of lipid-modifying agents, body mass index, electrocardiogram abnormalities, current drinking, and regular exercise were included as covariates.
Supplementary Fig. 2.
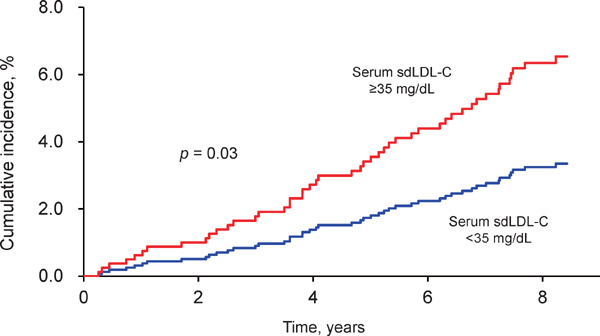
Age- and sex-adjusted cumulative incidence of coronary heart disease according to serum small dense low-density lipoprotein cholesterol among subjects in the high-risk category (n = 983)
Abbreviations: sdLDL-C, small dense low-density lipoprotein cholesterol.
Fig. 2 shows the joint influence of serum sdLDL cholesterol levels and the risk assessment status on the development for CHD. As compared to subjects with serum sdLDL cholesterol of < 35 mg/dL and at low-/moderate-risk category, the multivariable-adjusted HRs for the development of CHD increased significantly in subjects with serum sdLDL cholesterol of < 35 mg/dL and at high-risk category (HR 2.67, 95%CI 1.26–5.66) or in subjects with serum sdLDL cholesterol of ≥ 35 mg/dL and at low-/moderate-risk category (HR 2.05, 95%CI 1.01–4.16). Moreover, subjects with serum sdLDL cholesterol of ≥ 35 mg/dL and in the high-risk category had an additive excess risk of CHD events (HR 5.13, 95%CI 2.64–9.98). Similar joint excess risks of CHD events were observed according to the presence or absence of diabetes or CVD-related comorbidities (Supplementary Fig. 3).
Fig. 2.
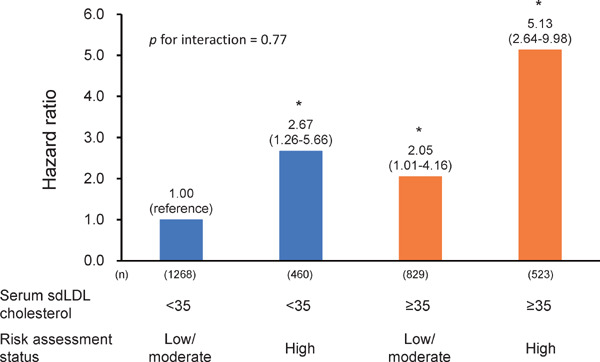
Multivariable-adjusted hazard ratios for the development of coronary heart disease according to serum small dense low-density lipoprotein cholesterol and the risk assessment status
Abbreviations: sdLDL, small dense low-density lipoprotein.
*p < 0.05 vs. reference.
Adjusted for use of antihypertensive agents, use of lipid-modifying agents, body mass index, ECG abnormalities, current drinking, and regular exercise.
Supplementary Fig. 3.
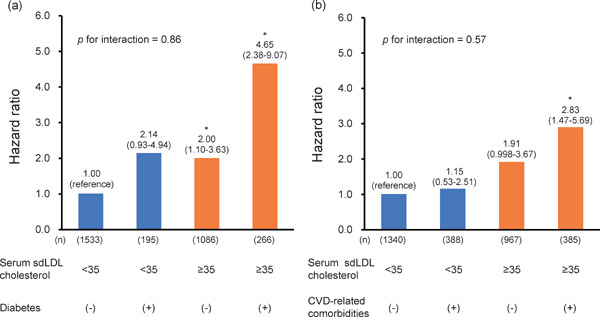
Multivariable-adjusted hazard ratios for the development of coronary heart disease according to serum small dense low-density lipoprotein cholesterol and presence or absence of (a) diabetes or (b) CVD-related comorbidities
Abbreviations: CVD, cardiovascular disease; sdLDL, small dense low-density lipoprotein.
*p < 0.05 vs. reference.
Adjusted for age, sex, systolic blood pressure, use of antihypertensive agents, high-density lipoprotein cholesterol, use of lipid-modifying agents, body mass index, estimated glomerular filtration rate, electrocardiogram abnormalities, current smoking, current drinking, and regular exercise. In the analysis for (b), the estimated glomerular filtration rate was excluded from the adjusted factors.
Finally, we examined the influence of serum sdLDL cholesterol on the development of CHD between subgroups of other lipid parameters—namely, serum LDL cholesterol, serum non-HDL cholesterol, serum HDL cholesterol, and serum triglycerides—in subjects in the high-risk category. The correlation between serum sdLDL cholesterol and other lipid parameters in those subjects were relatively strong (Supplementary Table 1). The multivariable-adjusted risk of CHD tended to be higher in subjects with serum sdLDL cholesterol of ≥ 35 mg/dL than in those with serum sdLDL cholesterol of < 35 mg/dL regardless of whether the levels of the other lipid parameters were higher or lower, although the HRs did not reach the level of statistical significance in subjects with lower levels of serum LDL and HDL cholesterol (Supplementary Fig. 4).
Supplementary Table 1. Correlation between serum small dense low-density lipoprotein cholesterol level and other lipid parameters among subjects in the high-risk category.
| Parameter | n | Spearman's rank correlation coefficient | p value |
|---|---|---|---|
| Serum LDL cholesterol | 983 | 0.65 | < 0.001 |
| Serum non-HDL cholesterol | 983 | 0.76 | < 0.001 |
| Serum HDL cholesterol | 983 | −0.30 | < 0.001 |
| Serum triglycerides | 974a | 0.62 | < 0.001 |
Abbreviations: HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Only subjects with available fasting blood samples were included in the analysis using serum triglycerides
Supplementary Fig. 4.
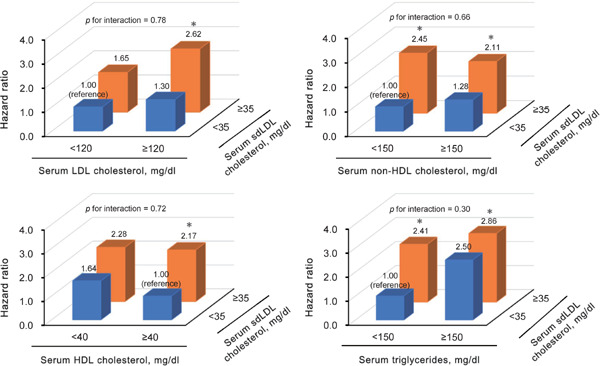
Multivariable-adjusted hazard ratios for the development of coronary heart disease according to serum sdLDL cholesterol and other lipid parameters among subjects in the high-risk category (n = 983)
Abbreviations: HDL, high-density lipoprotein; LDL, low-density lipoprotein; sdLDL, small dense low-density lipoprotein.
*p < 0.05 vs. reference.
Hazard ratios were adjusted for age, sex, systolic blood pressure, antihypertensive drugs, hemoglobin A1c, antidiabetic medication, HDL cholesterol, lipidlowering drugs, body mass index, estimated glomerular filtration rate, electrocardiogram abnormalities, current smoking, current drinking, and regular exercise.
In the analysis of subgroups of serum HDL cholesterol, serum HDL cholesterol was excluded from the adjusted factors.
In the analysis of serum triglycerides, only subjects with available fasting blood samples were included in the analysis using serum triglyceride (n = 974).
Discussion
The present study clearly demonstrated that a higher serum sdLDL cholesterol level was associated with increased risk for the development of CHD not only among the participants overall but also among subjects in the high-risk category for CVD, which was defined as recommended in the guidelines of the Japan Atherosclerosis Society. Subjects with higher cardiovascular risk and a higher serum sdLDL cholesterol level had an additively greater risk of CHD events than those with low/moderate cardiovascular risk and a lower serum sdLDL cholesterol level. Moreover, it is noteworthy that the excess risk of a higher serum sdLDL cholesterol level on CHD events was observed among subjects in the high-risk category for CVD regardless of the serum levels of other lipid parameters. These findings provide evidence that the measurement of serum sdLDL cholesterol is clinically valuable for estimating the future onset of CHD beyond the predefined cardiovascular risks.
There have been a few studies addressing the association between serum sdLDL cholesterol and CHD risk in the high-risk population for CVD. In the Multi-Ethnic Study of Atherosclerosis (MESA), a higher serum sdLDL cholesterol level was associated with the development of CHD among overall study participants, but the association was not statistically significant among subjects with type 2 diabetes11). Our result was inconsistent with this finding. The reasons for this discrepancy are not entirely clear, but it may be related to the accuracy of the follow-up data or statistical power of the MESA study, as the MESA study failed to reveal a significant association between serum LDL cholesterol and CHD, even though serum LDL cholesterol is an established risk factor for CHD in patients with diabetes19).
The strengths of the present study were its longitudinal population-based design, almost perfect follow-up of subjects, and accuracy in the diagnosis of CHD on the basis of medical records and autopsy findings. However, some potential limitations of this study should be noted. First, we were able to measure the serum sdLDL cholesterol level and other risk factors only once at baseline. We were also unable to obtain information about medical treatments during the follow-up period. In addition, information on the family history of early onset of CHD was not available, likely leading to an underestimation of the absolute risk based on the Suita score. This limitation could lead to misclassification of these variables, which in turn would weaken the association found in the current study, biasing the results toward the null hypothesis. Second, we could not conduct the subgroup analyses among subjects with or without chronic kidney disease or peripheral artery disease, because of the limited number of subjects with either disease. Third, we measured serum sdLDL cholesterol levels using frozen serum samples stored at −80°C for seven years, while serum sdLDL cholesterol levels were unlikely to be affected by the frozen storage20). Finally, since these analyses were conducted only in one cohort of Japanese, the generalizability of our findings might be limited. Therefore, our findings should be validated in other cohorts of various ethnic populations.
Conclusions
Elevated sdLDL cholesterol level was associated with the development of CHD among subjects at high-risk category as estimated according to the guidelines of the Japan Atherosclerosis Society. High-risk approaches for preventing CHD using serum sdLDL cholesterol measurement adhering with the existing guideline are likely to provide additional information against the burden of CHD in Japan. Further investigations are required to clarify whether serum sdLDL cholesterol would be an interventional target for reducing the risk of CHD events among subjects at high cardiovascular risk.
Acknowledgements and Notice of Grant Support
We would like to gratefully and sincerely thank Professor Yoshinao Oda, Professor Toru Iwaki, and their colleagues at the Department of Anatomic Pathology and Department of Neuropathology, Graduate School of Medical Sciences, Kyushu University, who provided expertise and insight into the autopsy findings that greatly assisted our research. The statistical analyses were carried out using the computer resources offered under the category of General Projects by the Research Institute for Information Technology, Kyushu University.
This study was supported in part by Grants-in-Aid for Scientific Research (A) (JP16H02692) and (B) (JP16H05850), JP17H04126, and JP18H02737) and (C) (JP17K09114, JP17K09113, JP17K01853, JP18K07565, JP18K09412,and JP19K07890) and (Early-Career Scientists) (JP18K17925, and JP18K17382) from the Ministry of Education, Culture, Sports, Science and Technology of Japan; by Health and Labour Sciences Research Grants of the Ministry of Health, Labour and Welfare of Japan (H29-Junkankitou-Ippan-003, and H30-Shokuhin-[Sitei]-005); and by the Japan Agency for Medical Research and Development (JP19dk0207025, JP19ek0210082, JP19ek0210083, JP19km0405202, JP19ek0210080, JP19fk0108075). In addition, this study was sponsored by DENKA SEIKEN Co., Ltd. (Tokyo, Japan). The sponsor of the study had no role in the study design, conduct of the study, data collection, data interpretation or preparation of the report.
Abbreviations
- BMI
body mass index
- CHD
coronary heart disease
- CI
confidence interval
- CVD
cardiovascular disease
- ECG
electrocardiogram
- eGFR
estimated glomerular filtration rate
- HbA1c
hemoglobin A1c
- HDL
high-density lipoprotein
- HR
hazard ratio
- LDL
low-density lipoprotein
- MESA
Multi-Ethnic Study of Atherosclerosis
- sdLDL
small dense low-density lipoprotein
Conflict of Interest
Toshiharu Ninomiya received research funding from DENKA SEIKEN Co., Ltd. The other authors declare that they have no conflicts of interest.
References
- 1). Collaborators GBDCoD: Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet, 2018; 392: 1736-1788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2). Vital Health and Social Statistics Office, Ministry of Health, Labour and Welfare: Vital Statistics. Available from:https://www.e-stat.go.jp/dbview?sid= 0003214721, Accessed 2020 Jan 17 [Google Scholar]
- 3). Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R, Simes R; Cholesterol Treatment Trialists' (CTT) Collaborators: Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet, 2005; 366: 1267-1278 [DOI] [PubMed] [Google Scholar]
- 4). Kinoshita M, Yokote K, Arai H, Iida M, Ishigaki Y, Ishibashi S, Umemoto S, Egusa G, Ohmura H, Okamura T, Kihara S, Koba S, Saito I, Shoji T, Daida H, Tsukamoto K, Deguchi J, Dohi S, Dobashi K, Hamaguchi H, Hara M, Hiro T, Biro S, Fujioka Y, Maruyama C, Miyamoto Y, Murakami Y, Yokode M, Yoshida H, Rakugi H, Wakatsuki A, Yamashita S; Committee for Epidemiology and Clinical Management of Atherosclerosis: Japan Atherosclerosis Society (JAS) Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2017. J Atheroscler Thromb, 2018; 25: 846-984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5). Nishimura K, Okamura T, Watanabe M, Nakai M, Takegami M, Higashiyama A, Kokubo Y, Okayama A, Miyamoto Y: Predicting coronary heart disease using risk factor categories for a Japanese urban population, and comparison with the framingham risk score: the suita study. J Atheroscler Thromb, 2014; 21: 784-798 [DOI] [PubMed] [Google Scholar]
- 6). Galeano NF, Al-Haideri M, Keyserman F, Rumsey SC, and Deckelbaum RJ: Small dense low density lipoprotein has increased affinity for LDL receptor-independent cell surface binding sites: a potential mechanism for increased atherogenicity. J Lipid Res, 1998; 39: 1263-1273 [PubMed] [Google Scholar]
- 7). Anber V, Griffin BA, McConnell M, Packard CJ, and Shepherd J: Influence of plasma lipid and LDL-subfraction profile on the interaction between low density lipoprotein with human arterial wall proteoglycans. Atherosclerosis, 1996; 124: 261-271 [DOI] [PubMed] [Google Scholar]
- 8). Tribble DL, Rizzo M, Chait A, Lewis DM, Blanche PJ, and Krauss RM: Enhanced oxidative susceptibility and reduced antioxidant content of metabolic precursors of small, dense low-density lipoproteins. Am J Med, 2001; 110: 103-110 [DOI] [PubMed] [Google Scholar]
- 9). Arai H, Kokubo Y, Watanabe M, Sawamura T, Ito Y, Minagawa A, Okamura T, Miyamato Y: Small dense low-density lipoproteins cholesterol can predict incident cardiovascular disease in an urban Japanese cohort: the Suita study. J Atheroscler Thromb, 2013; 20: 195-203 [DOI] [PubMed] [Google Scholar]
- 10). Hoogeveen RC, Gaubatz JW, Sun W, Dodge RC, Crosby JR, Jiang J, Couper D, Virani SS, Kathiresan S, Boerwinkle E, Ballantyne CM: Small dense low-density lipoprotein-cholesterol concentrations predict risk for coronary heart disease: the Atherosclerosis Risk In Communities (ARIC) study. Arterioscler Thromb Vasc Biol, 2014; 34: 1069-1077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11). Tsai MY, Steffen BT, Guan W, McClelland RL, Warnick R, McConnell J, Hoefner DM, Remaley AT: New automated assay of small dense low-density lipoprotein cholesterol identifies risk of coronary heart disease: the Multiethnic Study of Atherosclerosis. Arterioscler Thromb Vasc Biol, 2014; 34: 196-201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12). Higashioka M, Sakata S, Honda T, Hata J, Yoshida D, Hirakawa Y, Shibata M, Goto K, Kitazono T, Osawa H, Ninomiya T: Small dense low-density lipoprotein cholesterol and the risk of coronary heart disease in a Japanese community. J Atheroscler Thromb, 2020; 27: 669-682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13). Hata J, Ninomiya T, Hirakawa Y, Nagata M, Mukai N, Gotoh S, Fukuhara M, Ikeda F, Shikata K, Yoshida D, Yonemoto K, Kamouchi M, Kitazono T, Kiyohara Y: Secular trends in cardiovascular disease and its risk factors in Japanese: half-century data from the Hisayama Study (1961–2009). Circulation, 2013; 128: 1198-1205 [DOI] [PubMed] [Google Scholar]
- 14). Ninomiya T: Japanese Legacy Cohort Studies: The Hisayama Study. J Epidemiol, 2018; 28: 444-451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15). Ito Y, Fujimura M, Ohta M and Hirano T: Development of a homogeneous assay for measurement of small dense LDL cholesterol. Clin Chem, 2011; 57: 57-65 [DOI] [PubMed] [Google Scholar]
- 16). Thygesen K, Alpert JS, White HD; Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction: Universal definition of myocardial infarction. Eur Heart J, 2007; 28: 2525-2538 [DOI] [PubMed] [Google Scholar]
- 17). Horio M, Imai E, Yasuda Y, Watanabe T and Matsuo S: Modification of the CKD epidemiology collaboration (CKD-EPI) equation for Japanese: accuracy and use for population estimates. Am J Kidney Dis, 2010; 56: 32-38 [DOI] [PubMed] [Google Scholar]
- 18). Group KDIGOKCW: KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl, 2013; 3: 1-150 [DOI] [PubMed] [Google Scholar]
- 19). Huang ES, Meigs JB and Singer DE: The effect of interventions to prevent cardiovascular disease in patients with type 2 diabetes mellitus. Am J Med, 2001; 111: 633-642 [DOI] [PubMed] [Google Scholar]
- 20). Hirano T, Ito Y, Saegusa H and Yoshino G: A novel and simple method for quantification of small, dense LDL. J Lipid Res, 2003; 44: 2193-2201 [DOI] [PubMed] [Google Scholar]


