Dear Editor:
Candida guilliermondii is a uncommon newly emerging opportunistic pathogen found both in nature and as a component of the normal human microbial flora1,2. In recent years, the rate of C. guilliermondii infections has been increasing, and which are associated mainly with onychomycosis3. A case of Majocchi's granuloma resulting from a deep granulomatous dermatophyte infection and mimicking Kaposi sarcoma was reported4. However, a case of deep dermal Candida infection mimicking Kaposi sarcoma has not been reported yet.
A 79-year-old male presented with multiple erythematous to black verrucous nodules on his right foot that appeared 1 month prior. The lesions were distributed in a sporotrichoid lymphocutaneous pattern. The patient complained of tenderness and pain around the lesions, which were continuously discharging a exudate, forming a crust (Fig. 1A, B). In addition, the patient had onychomycosis, white and thick in appearance. The patient suffered from end-stage renal disease due to diabetes mellitus. He had received a kidney transplant 3 months prior and was on immunosuppressive treatment with tacrolimus and steroids.
Fig. 1. (A, B) Multiple erythematous to black nodules on the right foot at initial presentation. (C, D) Four months after treatment with oral terbinafine.
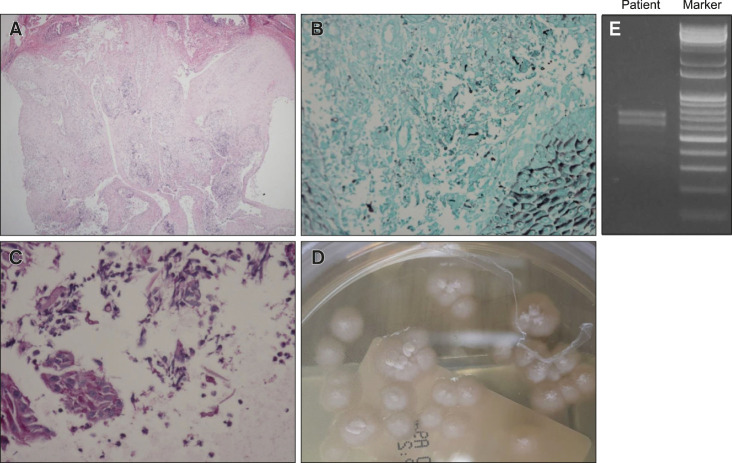
As the patient was treated with immunosuppressive therapy, we suspected the diagnosis of Kaposi sarcoma and deep fungal infection. The histopathological examination showed parakeratosis, pseudoepitheliomatous hyperplasia, and mixed cell infiltration in the dermis (Fig. 2A). Human herpes virus 8 (HHV-8), Periodic acid-Schiff (PAS), and Gomori's methenamine silver (GMS) staining was also performed. D-PAS and GMS staining showed multiple small yeast cells in the dermis (Fig. 2B, C) and HHV-8 staining was negative. Tissue culture on Sabouraud agar showed white, smooth, glabrous yeast-like colonies (Fig. 2D). To determine the strain of infected fungi, we did polymerase chain reaction (PCR) using internal transcribed spacer (ITS) primers. We detected two bands in PCR results and performed sequencing using ITS1 and ITS4 primers with extracted PCR products (Fig. 2E). Sequencing results of PCR product in the lower band was analyzed by using BLAST and confirmed C. guilliermondii. The patient was treated with terbinafine, 125 mg daily, considering the renal function and drug interaction with tacrolimus. After 4 months of treatment, the lesions improved dramatically (Fig. 1C, D).
Fig. 2. (A) Parakeratosis, pseudoepitheliomatous hyperplasia of epidermis and mixed cell infiltration in dermis (H&E, ×40). (B, C) Multiple small yeasts with narrow based budding in dermis (B: GMS stain, ×200; C: PAS stain, ×400). (D) White and smooth glabrous yeastlike colonies on Sabouraud agar. (E) Result of polymerase chain reaction amplification of the internal transcribed spacer (ITS) region of the fungus using ITS1 and ITS4 primers.
Superficial dermatomycosis is fairly prevalent in transplant recipients and its rate increases as patients receive massive immunosuppressive treatment. However, deep dermatomycosis involving the dermis and subcutaneous layer by dermatophytes and yeast, is relatively rare5. Deep dermatophytosis often presents with multiple nodules on lower extremities, accompanied by superficial fungal infection5. There is no report of a similar case involving yeast, let alone species as uncommon as C. guilliermondii. In our case, the patient presented with deep dermal dermatomycosis with suppurative granuloma, resembling Kaposi sarcoma, caused by C. guilliermondii. The patient had severe onychomycosis of toenails, which we suspected to be the cause of deep dermatomycosis.
In conclusion, this case demonstrates the clinical diversity of deep dermatomycosis in an immunocompromised patient, caused by C. guilliermondii. When multiple erythema tous nodules mimicking Kaposi sarcoma are found in lower extremities of immunocompromised patients, a deep dermatomycosis by Candida species should also be considered. Tissue culture and PCR are helpful for diagnosis if the infection is caused by a rare fungus species, such as C. guilliermondii.
ACKNOWLEDGMENT
We thank the patient for granting permission to publish this information.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
FUNDING SOURCE: This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by Ministry of Education, Science and Technology (NRF-2019R1A2C1004114).
DATA SHARING STATEMENT
Research data are not shared.
References
- 1.Cebeci Güler N, Tosun I, Aydin F. The identification of Meyerozyma guilliermondii from blood cultures and surveillance samples in a university hospital in Northeast Turkey: a ten-year survey. J Mycol Med. 2017;27:506–513. doi: 10.1016/j.mycmed.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 2.Nakazawa H, Nishina S, Senoo Y, Sakai H, Ito T, Kikuchi K, et al. Breakthrough Candida guilliermondii (Meyerozyma guilliermondii) fungemia after cord blood transplantation for extranodal NK-cell lymphoma with azole prophylaxis. Transpl Infect Dis. 2018;20:e12922. doi: 10.1111/tid.12922. [DOI] [PubMed] [Google Scholar]
- 3.Pfaller MA, Diekema DJ, Mendez M, Kibbler C, Erzsebet P, Chang SC, et al. Candida guilliermondii, an opportunistic fungal pathogen with decreased susceptibility to fluconazole: geographic and temporal trends from the ARTEMIS DISK antifungal surveillance program. J Clin Microbiol. 2006;44:3551–3556. doi: 10.1128/JCM.00865-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brod C, Benedix F, Röcken M, Schaller M. Trichophytic Majocchi granuloma mimicking Kaposi sarcoma. J Dtsch Dermatol Ges. 2007;5:591–593. doi: 10.1111/j.1610-0387.2007.06283.x. [DOI] [PubMed] [Google Scholar]
- 5.Okata-Karigane U, Hata Y, Watanabe-Okada E, Miyakawa S, Ota M, Uzawa Y, et al. Subcutaneous abscesses caused by Trichophyton rubrum in the unilateral groin of an immunocompromised patient: a case report. Med Mycol Case Rep. 2018;21:16–19. doi: 10.1016/j.mmcr.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data are not shared.