Abstract
Palisaded neutrophilic and granulomatous dermatitis (PNGD) is an uncommon skin eruption and characterized histopathologically by the presence of granulomatous inflammation with or without leukocytoclastic vasculitis. PNGD is known to be associated with various immune-mediated connective tissue diseases such as rheumatoid arthritis and lupus erythematosus. However, to our knowledge, a case of PNGD in a patient with Behçet's disease is extremely rare and only one case has been reported in foreign literature to date. Herein, we report an unusual case of a 60-year-old female with Behçet's disease who presented multiple erythematous to flesh-colored papules on the extremities, buttocks, and ear lobes and was diagnosed with PNGD. After the treatment of systemic corticosteroids, colchicine and azathioprine, the skin lesions and oral ulcers improved. The patient is under observation without recurrence of skin lesions for 6 months.
Keywords: Behcet syndrome, Palisaded neutrophilic granulomatous dermatitis
INTRODUCTION
Palisaded neutrophilic and granulomatous dermatitis (PNGD) is an uncommon condition characterized histopathologically by the presence of granulomatous inflammation with or without leukocytoclastic vasculitis1. PNGD has a varied clinical presentations consisting of multiple discrete, 2 to 10 mm erythematous to violaceous papules or plaques, typically located over extensor surfaces or the trunk2. PNGD has been most commonly associated with underlying systemic diseases such as rheumatoid arthritis (26.8%), followed closely by lupus erythematosus (11.3%)3. However, a case of PNGD in patient with Behçet's disease is extremely rare and so far only one case has been reported in foreign literature3,4,5.
CASE REPORT
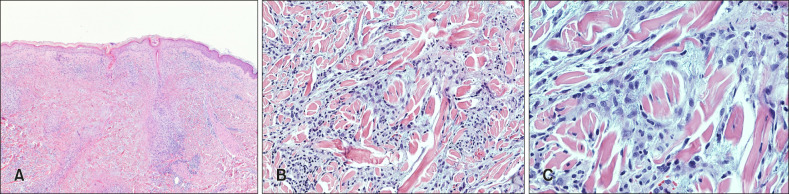
The patient was a 60-year-old female who presented with a 3-year history of tender, erythematous, papules involving the both arms, thighs, knees, buttocks, and ear lobes that continued to wax and wane (Fig. 1). The patient had no significant medical history other than recurrent uveitis and oral ulcer over the last three years. Physical examination revealed multiple erythematous to flesh-colored papules on her both extremities, buttocks, and ear lobes and oral ulcers. She was diagnosed with panuveitis by an ophthalmic examination and there was no specific finding on the gynecological evaluation. Skin biopsy on papular lesions of the right arm showed multiple interstitial and palisading histiocytic infiltrations that surround degenerated collagen and scattered neutrophils and nuclear dust (Fig. 2). Superficial to mid-dermal perivascular infiltrates and extravasated erythrocytes were observed. Alcian blue and Periodic acid-Schiff staining revealed no mucin deposition in the area of granulomatous inflammation. On laboratorytests, complete blood cell count, blood biochemistry, and urinalysis were within normal limits. There was no abnormal finding on chest radiography. Additional screening tests showed negative results for human leukocyte antigen (HLA) B27 real time polymerase chain reaction, HLA B51, antidouble stranded DNA antibody (Ab), anti-β2 glycoprotein1 Ab, anti-cardiolipin Ab, anti-neutrophilic cytoplasmic Ab, and lupus anticoagulant testing, but positive for anti-nuclear Ab at a titer of 1:160. Diagnosis of systemic lupus erythematosus could be ruled out based on the American College of Rheumatology criteria for classification of systemic lupus erythematosus in 1997. According to diagnostic criteria established by the International Study Group for Behçet's disease in 1990, she was diagnosed with Behçet's disease. Given the clinical and histopathologic manifestations, the diagnosis of PNGD associated with Behçet's disease was made. After treatment of panuveitis with high dose steroids, the dose of systemic corticosteroids was reduced to the 20 mg of prednisolone per day and 0.6 mg of colchicine and 50 mg of azathioprine per day were added for the treatment of Behçet's disease. The skin lesions and oral ulcers were subsided after the treatment and she is under observation without recurrence of skin rashes for 6 months.
Fig. 1. (A) Clinical photograph of multiple erythematous to flesh-colored papules on extensor surface of the right upper arm and (B) left buttock. We received the patient's consent form about publishing all photographic materials.
Fig. 2. Microscopic feature of palisaded neutrophilic and granulomatous dermatitis. (A) Multiple well-developed granulomas with fibrosis in the upper and lower dermis (H&E, ×40). (B) Degenerated collagen, scant neutrophils and nuclear dust were surrounded by an interstitial and palisading histiocytic infiltrations in the dermis (H&E, ×200). (C) Closed view (H&E, ×400).
DISCUSSION
Recurrent oral aphthous ulcer is the most frequent manifestation of Behçet's disease and should be differentiated from those of recurrent oral ulcers due to other causes, such as trauma, infection (herpes simplex, syphilis, human immunodeficiency virus), mucocutaneous disease (lichen planus, erythema multiforme), immunobullous disease (pemphigus) and squamous cell carcinoma6,7. Genital aphthous ulcers are morphologically similar to the oral ulcers but usually larger and deeper. Recurrent genital ulcerations should be differentiated from venereal disease such as syphilis, chancroid and herpes simplex virus infection7,8. Crohn's disease, sarcoidosis and infectious uveitis must be ruled out in case of recurrent uveitis8. Papulopustular or acne-like lesions are the most common (28%~96%) cutaneous manifestations7. However such lesions are nonspecific and are difficult to clinically differentiate from other diseases, such as acne vulgaris or folliculitis. Recent studies have demonstrated that histopathological findings of vasculitis in papulopustular lesions may be regarded as significant diagnostic criteria for patients suspected of Behçet's disease9. In our case, the patient showed recurrent oral ulcers and uveitis. Multiple erythematous papules on both extremities, buttocks and ear lobes were identified. A skin biopsy revealed histological findings consistent with PNGD. Based on clinical and pathological findings on biopsy, the patient was diagnosed with Behçet's disease combined with PNGD.
The histopathologic appearance of PNGD vary from diffuse interstitial inflammation composed of histiocytes or lymphocytes or eosinophils, and/or little neutrophils to dense neutrophilic infiltrates with degenerated collagen and palisading granulomas with fibrosis and scant neutrophilic debris10,11. Early lesions show dense neutrophilic infiltrates with or without leukocytoclastic vasculitis and degenerated collagen. Fully developed lesions represent palisaded granulomas with dermal fibrosis and scant neutrophilic debris that surround degenerated collagen2,12. In its apparent late stage, PNGD appears to resolve with fibrosis and shows histopathologic features similar to necrobiosis lipoidica12. In this case, the histologic findings were consistent with fully developed lesions. Each developmental stage has a specific differential diagnosis such as leukocytoclastic vasculitis, rheumatoid nodules, granuloma annulare, and necrobiosis lipoidica2,11. Compared with leukocytoclastic vasculitis, PNGD has much more neutrophilic infiltrations and nuclear dust throughout the dermis and it also shows more severe collagen degenerations12,13. Rheumatoid nodules are generally deeper in the dermis and have more sclerosis in the area surrounded by the granuloma11. Granuloma annulare has far fewer nuclear debris, thinner degenerated collagen and more abundant mucin deposits. Necrobiosis lipoidica is characterized by palisaded granuloma with degenerated collagen that extend not only throughout the dermis but also into the septa of subcutis fat2,11,12,13.
Interstitial granulomatous dermatitis (IGD) is a rare dermatosis, histologically characterized by an interstitial infiltrate of histiocytes in the reticular dermis. Rarely, neutrophils and eosinophils can be found and vasculitis is generally absent. IGD is associated with various systemic conditions and medications such as antihypertensives, lipid-lowering agents, and anticonvulsants14. Considering the overlapping clinical and histopathologic findings and systemic disease associations, IGD and PNGD are thought to exist on the same clinicopathological spectrum while others have considered that IGD has a distinct clinical presentation with associated histopathology15,16. It might be difficult to differentiate IGD from interstitial granuloma annulare (IGA) which show interstitial granulomatous pattern. In IGA, prominent mucin deposition and focal histiocytic infiltrates are observed14. In our case, based on the patient's medical history, she did not take any medications known to be associated with the development of granulomatous dermatitis14,15. The histopathologic features displayed a fully developed lesion of PNGD. Despite vasculopathy was observed, leukocytoclastic vasculitis was not a feature at this stage17. In our patient, the absence of dermal mucin, pandermal interstitial and palisading pattern of histiocytes surrounding degenerated collagen and numerous neutrophilic infiltrates were distinguishing features of PNGD.
PNGD is an unusual disease entity associated with variable and heterogeneous systemic diseases. Although there are many reports related to other autoimmune disease, the reports of PNGD associated with Behçet's disease is extremely rare. To our knowledge, only one case of PNGD associated with Behçet's disease has been reported in foreign literature4. Therefore, we suggest that dermatologists should pay attention to this rare disease entity, especially in patient with underlying systemic diseases and further studies on the prognosis of PNGD associated with Behçet's disease are needed.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
FUNDING SOURCE: None.
DATA SHARING STATEMENT
Research data are not shared.
References
- 1.Choi SH, Ha SM, Ko DY, Song KH, Kim KH. Abrupt onset of palisaded neutrophilic and granulomatous dermatitis in a patient with rheumatoid arthritis. Korean J Dermatol. 2014;52:567–570. [Google Scholar]
- 2.Deen J, Banney L, Perry-Keene J. Palisading neutrophilic and granulomatous dermatitis as a presentation of Hodgkin lymphoma: a case and review. J Cutan Pathol. 2018;45:167–170. doi: 10.1111/cup.13076. [DOI] [PubMed] [Google Scholar]
- 3.Hantash BM, Chiang D, Kohler S, Fiorentino D. Palisaded neutrophilic and granulomatous dermatitis associated with limited systemic sclerosis. J Am Acad Dermatol. 2008;58:661–664. doi: 10.1016/j.jaad.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 4.Kim SK, Park CK, Park YW, Jun JB, Yoo DH, Bae SC. Palisaded neutrophilic granulomatous dermatitis presenting as an unusual skin manifestation in a patient with Behçet's disease. Scand J Rheumatol. 2005;34:324–327. doi: 10.1080/03009740510015195. [DOI] [PubMed] [Google Scholar]
- 5.Kim SM, Yoon TY, Yoon TJ. A case of palisaded neutrophilic and granulomatous dermatitis. Korean J Dermatol. 2008;46:1129–1133. [Google Scholar]
- 6.Davatchi F. Behcet's disease. Int J Rheum Dis. 2014;17:355–357. doi: 10.1111/1756-185X.12378. [DOI] [PubMed] [Google Scholar]
- 7.Kokturk A. Clinical and pathological manifestations with differential diagnosis in Behçet's disease. Patholog Res Int. 2012;2012:690390. doi: 10.1155/2012/690390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saadoun D, Wechsler B. Behçet's disease. Orphanet J Rare Dis. 2012;7:20. doi: 10.1186/1750-1172-7-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi MJ, Cho SB, Cho S, Kim DY, Bang D. Eosinophilic pustular folliculitis in a patient with Behçet's disease. Int J Case Rep Med. 2016;2016:832328 [Google Scholar]
- 10.Gulati A, Paige D, Yaqoob M, Proby CM, Cerio R, Harwood CA. Palisaded neutrophilic granulomatous dermatitis associated with systemic lupus erythematosus presenting with the burning rope sign. J Am Acad Dermatol. 2009;61:711–714. doi: 10.1016/j.jaad.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 11.Stiff KM, Cohen PR. Palisaded granulomatous dermatitis associated with ulcerative colitis: a comprehensive literature review. Cureus. 2017;9:e958. doi: 10.7759/cureus.958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chu P, Connolly MK, LeBoit PE. The histopathologic spectrum of palisaded neutrophilic and granulomatous dermatitis in patients with collagen vascular disease. Arch Dermatol. 1994;130:1278–1283. [PubMed] [Google Scholar]
- 13.Hyun DN, Park JS, Chung H, Jang HC. A case of palisaded neutrophilic and granulomatous dermatitis (rheumatoid papule) Korean J Dermatol. 2007;45:847–850. [Google Scholar]
- 14.Kim SM, Cho SH, Lee JD, Kim HS. Interstitial granulomatous dermatitis in a patient with prostate cancer. Ann Dermatol. 2017;29:337–340. doi: 10.5021/ad.2017.29.3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huizenga T, Kado JA, Pellicane B, Borovicka J, Mehregan DR, Mehregan DA. Interstitial granulomatous dermatitis and palisaded neutrophilic granulomatous dermatitis. Cutis. 2018;101:E19–E21. [PubMed] [Google Scholar]
- 16.Kern M, Shiver MB, Addis KM, Gardner JM. Palisaded neutrophilic and granulomatous dermatitis/interstitial granulomatous dermatitis overlap: a striking clinical and histologic presentation with "burning rope sign" and subsequent mirrorimage contralateral recurrence. Am J Dermatopathol. 2017;39:e141–e146. doi: 10.1097/DAD.0000000000000901. [DOI] [PubMed] [Google Scholar]
- 17.Chou CL, Wang KH, Chiang YY. Palisaded neutrophilic and granulomatous dermatitis associated with the initiation of etanercept in rheumatoid arthritis: a case report. Dermatol Sin. 2011;29:129–133. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data are not shared.