Abstract
Choledochal cyst and gallbladder duplication are rare congenital anomalies. They typically are surgical problems of infancy or childhood but rarely may present in adults also. Despite high resolution imaging, the differentiation of type II choledochal cyst from gallbladder duplication often causes the diagnostic dilemma; which may result in high risk for intraoperative iatrogenic injury. Operative management of choledochal cyst is the definite treatment because of its malignant potential. A type II choledochal cyst arising from the hepatic hilum presenting as gallbladder duplication on imaging has not been reported earlier in the literature and here we present a case report of the same which was managed successfully.
Keywords: biliary intervention, gastrointestinal surgery, general surgery
Background
Hepatobiliary anomalies in close proximity to the gallbladder fossa such as choledochal cyst, gallbladder duplication, duodenal duplication or gallbladder adenomyomas needs to be distinguished accurately prior to surgery with high resolution imaging like MRI.1 Despite high resolution imaging, the differentiation of type II choledochal cyst from gallbladder duplication often causes the diagnostic dilemma.2 Laparoscopy is the best tool for diagnosis and operative management. These patients often associated with other hepatobiliary pathology, high risk for intraoperative iatrogenic injury. A type II choledochal cyst arising from the hepatic hilum presenting as gallbladder duplication on imaging has not been reported earlier in the literature was managed successfully. It is also imperative that resection of the choledochal cyst should be done to prevent its transformation into future cancer.3
Case presentation
A 32-year-old woman hailing from North India presented with recurrent dull aching pain abdomen in right upper quadrant for 3 years. There was no history of jaundice, nausea and fever. She also complained of occasional dyspepsia post meal, for which she took no treatment.
Investigations
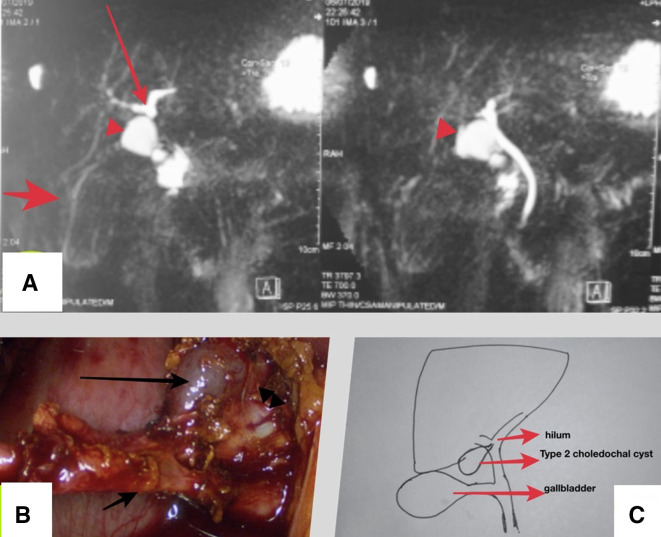
Sonography was done which revealed chronic cholecystitis with dilated proximal bile duct. Her lab investigations were within normal limit except with haemoglobulin level 11.2g/dL, white blood cell count of 6.8X109/L. Serum alkaline phosphatase was 154 IU/L, slightly in near higher limit of our institute values, but total and conjugated bilirubin were normal 0.7 and 0.3 mg/dL, respectively. Magnetic Resonance Cholangiopancreatography (MRCP) showed cholelithiasis and a 1.4×1.3 cm cystic structure superior to gallbladder communicating with common hepatic duct via a linear duct and differential of duplicated gallbladder or type II choledochal cyst was made (figure 1A). However, there was no evidence of abnormal pancreatobiliary junction on reviewing of MRCP.
Figure 1.
(A) Magnetic resonance cholangiopancreatography showing cholelithiasis and 1.4×1.3 cm cystic structure superior to gallbladder communicating with common hepatic duct via a linear duct. (B) Intraoperative laparoscopic view showing dissected calots triangle, gallbladder and a small cystic lesion located at the hilum. (C) Diagrammatic representation of intraoperative finding (courtesy—Dr Amaresh Aruni coauthor).
Treatment
She was taken up for surgery and on laparoscopy the findings were distended gallbladder, long cystic duct with normal insertion, calot’s triangle dissected and cholecystectomy was done. There was single long cystic duct and artery. After cholecystectomy, another cystic structure filled with mucus arising from the hepatic hilum was noted and diagnosis of type II choledochal cyst was made (figure 1B, C). During excision of the cyst, there was an iatrogenic traction injury at hilum with bile effluent from pin point opening. The procedure was converted to open in view of technical difficulties and repaired primarily. Intraoperative cholangiogram was not done as the injury was readily identified and repaired without any technical difficulty. The reason for mucus filled cyst despite communication with hilum was due to acute angulation between the point of the origin and the cyst. The postoperative period was uneventful. Histology had features of chronic cholecystitis in the gall bladder specimen while the cyst showed flattened lining epithelium with absence of submucosal glands or muscle layer suggesting choledochal cyst.
Outcome and follow-up
She did well in postoperative period. Her oral feed was started in postoperative day 1 which was tolerated well and was discharged on day 2. Currently she is in follow-up in outpatient department and is doing well.
Discussion
Choledochal cysts are congenital anomaly of biliary ducts, typically are surgical problems of infancy or childhood; however, in 20% of patients the diagnosis is delayed until adulthood.4 Bile duct cysts account for approximately 1% of all benign biliary disease.5 Incidence ranges from 1 in 100 000 to 1 in 150 000 individuals in western countries to 1 in 13 000 in certain parts of Asia.6 Choledochal cyst and gallbladder duplication both are rare congenital anomalies of the biliary tree primordium and are difficult to differentiate clinically and radiologically. Incidence of duplicated gallbladder reported is 1 in 12 000 cholecystectomies and 1 in 4000 autopsies.1 Type II choledochal cyst is rare with an incidence of 2.3%, Quaissi et al classified type II cysts according to the location in relation to the hepatoduodenal ligament as upper, middle and lower with incidence reported 58%, 21% and 21%, respectively.7 A type II choledochal cyst arising from the hepatic hilum presenting as gallbladder duplication on imaging has not been reported earlier. The aetiology of type 2 Choledochal Cysts was suggested by Hayes et al as that the diverticulum is a remnant of an earlier stage of bile duct development when it represents network of cells than tubular ducts.8 Ultrasonography is the initial investigative modality, however, MRCP has become the gold standard method of imaging the bile ducts and their anomalies. MRCP has a 96%–100% detection rate for bile duct cysts, 53%–100% rate for diagnosing anomalous Pancreatico-biliary Juction.9 Laparoscopy is very helpful in evaluation of normal anatomy, anomalies, clears the diagnosis and proceeding with definitive procedure, however, histopathology confirms the diagnosis. The management of isolated type II choledochal cyst is surgical excision. Cholecystectomy is the procedure of choice for symptomatic gallbladder duplication. Minimally invasive approaches are used increasingly for the biliary disease and gallbladder pathologies due to superior visualisation of the structure around the cyst, gallbladder, hepatic hilum and associated anomalies. The magnification conferred by laparoscope helps assess the structures in detail, fine dissection and anastomosis at the hilar area.10 However, it must be emphasised that laparoscopic excision of bile duct cysts is technically challenging and requires experience in both complex biliary operations and advanced laparoscopic surgery.11 Caveats of performing surgery include higher risk of biliary injury due to variant anatomy.12 Malignant transformation of choledochal cyst is a serious complication and risk increases with age, excision is most desirable in children and adults whenever it is suspected.3 13
Learning points.
Choledochal cyst and gallbladder duplication are rare congenital anomalies, though advancement in imaging one should proceed with certain differentials before surgery.
Choledochal cyst if identified should be treated operatively, due to its malignant potential.
Biliary ductal system is associated with anatomical anomalies and should be dealt preoperatively by imaging, intraoperatively by careful dissection and cholangiogram if required.
Acknowledgments
We would like to thank Professor Arunanshu Behera for his intraoperative assessment and preparing this manuscript.
Footnotes
Contributors: CT contributed to writing and editing, critical review. AC contributed to manuscript preparation and final submission. AA contributed to manuscript preparation, critical review and data collection. VNS contributed to review and data collection.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ayodele A, Chukwuma A, Oloruntobi R. Choledochal cyst or gallbladder duplication? diagnostic laparoscopy for chronic abdominal pain in a 10 year old boy. Int Surg J 2015;2:696–9. 10.18203/2349-2902.isj20151106 [DOI] [Google Scholar]
- 2.Lee HK, Park SJ, Yi BH, et al. Imaging features of adult choledochal cysts: a pictorial review. Korean J Radiol 2009;10:71–80. 10.3348/kjr.2009.10.1.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tidjane A, Serradj NB, Bengueddach A, et al. P-132 malignant transformation of choledochal cysts: description of a North African series of 7 cases. Annals of Oncology 2020;31:S132–3. 10.1016/j.annonc.2020.04.214 [DOI] [Google Scholar]
- 4.Bhargava V, Sade R. Clinical study and management of choledochal cyst. Int J Sci Stud 2018;6:155–63. [Google Scholar]
- 5.Saxena R, Pradeep R, Chander J, et al. Benign disease of the common bile duct. Br J Surg 1988;75:803–6. 10.1002/bjs.1800750828 [DOI] [PubMed] [Google Scholar]
- 6.Olbourne NA Choledochal cysts. A review of the cystic anomalies of the biliary tree. Ann R Coll Surg Engl 1975;56:26–32. [PMC free article] [PubMed] [Google Scholar]
- 7.Ouaïssi M, Kianmanesh R, Belghiti J, et al. Todani type II congenital bile duct cyst: European multicenter study of the French surgical association and literature review. Ann Surg 2015;262:130–8. 10.1097/SLA.0000000000000761 [DOI] [PubMed] [Google Scholar]
- 8.Schweizer P Pathogenesis of choledochal cyst: a hereditary disease? Pediatr Surg Int 1995;10. [Google Scholar]
- 9.Fitoz S, Erden A, Boruban S. Magnetic resonance cholangiopancreatography of biliary system abnormalities in children. Clin Imaging 2007;31:93–101. 10.1016/j.clinimag.2006.11.002 [DOI] [PubMed] [Google Scholar]
- 10.Bhojwani R, Jain N, Mishra S. Laparoscopic evaluation and resection of type-II choledochal cyst arising from right hepatic duct mimicking gall bladder duplication. J Minim Access Surg 2018;15:158–60. 10.4103/jmas.JMAS_101_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palanivelu C, Rangarajan M, Parthasarathi R, et al. Laparoscopic management of choledochal cysts: technique and outcomes--a retrospective study of 35 patients from a tertiary center. J Am Coll Surg 2008;207:839–46. 10.1016/j.jamcollsurg.2008.08.004 [DOI] [PubMed] [Google Scholar]
- 12.Zhang B, Wu D, Fang Y, et al. Early complications after laparoscopic resection of choledochal cyst. Pediatr Surg Int 2019;35:845–52. 10.1007/s00383-019-04489-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Todani T, Watanabe Y, Narusue M, et al. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg 1977;134:263–9. 10.1016/0002-9610(77)90359-2 [DOI] [PubMed] [Google Scholar]