Abstract
Early adolescence is a pivotal developmental period when multiple health risk behaviors (MHRBs), such as obesity and substance use, are often established. Several psychosocial factors, often considered traits, have been independently associated with these increases, including executive function (EF), mindfulness disposition (MD), perceived stress, distress tolerance (DT), and anhedonia. However, these factors have not been evaluated for their conjoint relationships to determine whether different patterns may signal greater or lesser risk for obesity and substance use, and whether the same patterns relate to obesity and substance use in the same ways (same magnitude of risk). To evaluate these patterns, a latent profile analysis was conducted, resulting in a three-profile model. Profile 1 (8% of sample) was characterized by the lowest levels of EF, MD, DT and highest levels of stress and anhedonia, profile 2 (44%) intermediate levels, and profile 3 (48%) the highest levels of EF, MD, DT and lowest levels of stress and anhedonia. Youth classified to profile 1 reported significantly greater levels of both obesogenic and substance use behavior relative to other profiles. Findings suggest that adolescents engaging in obesogenic and substance use behaviors may share common profiles of psychosocial risk.
Introduction
Early adolescence is a pivotal developmental period that is marked by increased independence from parents and, for some youth, engagement in multiple health risk behaviors (MHRBs) (Spring, Moller, & Coons 2012). These transitional years are often characterized by increases in novelty-seeking, impulsivity, risk-taking, and a heightened sensitivity to rewarding stimuli (Spear, 2013)-all of which have been linked to increased MHRB. Two important sets of health risk behaviors, which tend to increase during early adolescence, include substance use (i.e. cigarette and alcohol use; Thatcher & Clark, 2008) and obesogenic behaviors (e.g. consumption of high-calorie/low-nutrient foods, sedentary behavior) (Pearson, Haycraft, J, & Atkin, 2017). Consumption of high calorie/low nutrient foods and drugs of abuse will typically activate brain regions and neurotransmitter systems associated with reward and behavior reinforcement (Volkow et al. 2011). Furthermore, repetition of these behaviors throughout early adolescence has the potential to lead to subsequent development of substance use and binge eating disorders (Kechter & Black, 2020).
Previous research has begun to examine MHRB in a dynamic context (Leech et al 2014). For example, Fleary (2017) conducted a latent class analysis to determine distinct groups of behavioral risk among adolescents including obesogenic and substance use. Observed patterns of risk behaviors indicate co-occurrence of such risk behaviors, with some evidence of shared determinants, which may be targeted by MHRB prevention programs (Hale, Fitzgerald-Yau, & Viner 2014; Pentz, Riggs, & Warren 2016). Evidence-based interventions that simultaneously address MHRBs based on an understanding of how they cluster allows for intervention at the full continuum of risk. Simultaneously investigating complex health risk behaviors (occurring concurrently in adolescents’ lives) by examining individual psychosocial characteristics can be informative, particularly since these characteristics (1) have been associated with MHRB (most commonly obesogenic behavior such as increased screen time, high-calorie low-nutrient food intake, and substance use behaviors and (2) are amenable to intervention (i.e., executive function, mindfulness disposition, perceived stress, distress tolerance, anhedonia).
Executive function (EF) and mindfulness disposition (MD) are highly associated metacognitive capacities. EF describes a set of higher order cognitive processes that underlie goal-directed behavior, including working memory, cognitive flexibility, and behavioral inhibition, as well as affective processes that involve emotion regulation (Diamond, 2013;). Lower levels of EF may leave youth especially vulnerable to poor decision-making and impulse control, resulting in the adoption of multiple health risk behaviors, including alcohol and tobacco use, as well as obesity-related risk behaviors like sedentary behavior and high-calorie/low-nutrient food and beverage intake (Allan, McMinn, & Daly, 2016; Pentz & Riggs, 2013; Cappelli et al., 2019). MD represents a trait indicative of the degree to which an individual is attentive to and aware of what is occurring in the present moment (Brown & Ryan, 2003). Lower levels of MD have been associated with negative physical health outcomes, as well as self-regulation problems, greater perceived stress, and psychopathology risk (Prazak et al., 2012; Garland, Hanley, Thomas, Knoll, & Ferraro, 2015; Prakash, Hussain, & Schirda, 2015). Recent neurological and behavioral studies have begun to explore the putative mechanisms underlying the effects of mindfulness on health risk behavior (Fossati, Vigorelli Porro, Maffei, & Borroni, 2012; Keng, Smoski, & Robins, 2011). For example, one study of 7th and 8th grade students reported significant positive associations between inhibitory control, working memory, and MD (Riggs, Black & Ritt-Olsen 2015). Another recent study of 7th grade students found MD and EF associated with perceived distress and perceived coping to similar magnitudes (Kechter et al., 2019). Taken together, this evidence suggests EF and MD are both higher-order cognitive processes that underlie goal-directed behavior and may somewhat overlap, both conceptually and empirically. However, little remains known about the relationships between these individual states/traits and MHRBs in the adolescent context.
In addition to the aforementioned cognitive factors, numerous affective factors have also been linked to greater MHRBs-including stress, distress tolerance, and anhedonia. Psychosocial stress is often conceptualized as a perceived threat (real or imagined) that exceeds one’s perceived abilities to cope (Cohen, Kamarck, & Mermelstein, 1983). Low distress tolerance (DT) refers to a person’s inability to withstand negative psychological and/or physical states and is frequently accompanied by the desire to escape negative emotional states (Leyro, Zvolensky, & Bernstein, 2010). Anhedonia is defined as the inability to experience happiness and pleasure from previously enjoyable stimuli and experiences (Ho & Sommers, 2013). While it is recognized as a staple characteristic in psychiatric illnesses, including major depression and schizophrenia, it is conceptualized here as a transdiagnostic emotional vulnerability (Leventhal & Zvolensky, 2015). The degree to which an adolescent perceives experiences (both external and internal) as distressing as well as their ability to tolerate this distress, may predict their engagement in MHRB. For example, previous investigations have found increased food intake generally (Adam & Epel, 2007), and particularly of sweet and salty energy dense foods (Nguyen-Michel, Unger, & Spruijt-Metz, 2007), can diminish distress among those exposed to psychobiological stressors (Dallman, 2010; Tomiyama, Dallman, & Epel, 2011). Similarly, sedentary behaviors such as screen time (e.g., television-viewing), have been interpreted as a coping mechanism that assists children in distracting themselves from a stressor (Roemmich, Gurgol, & Epstein, 2003). Stress reactivity and negative affect may be identifiable markers leading youth to engage in MHRBs to heighten reward response. For example, it has been proposed that anhedonic adolescents may be more likely to engage in highly hedonically-valenced behaviors, including MHRBs, and may experience more rewarding effects from substance use than their less anhedonic peers (Sussman & Leventhal, 2014).
The assessment of these specific psychological states/traits in the present study was intended to integrate separate bodies of literature examining each health risk behavior (e.g., substance use) per trait/state (e.g., mindfulness disposition) and better understand the extent to which commonly co-occurring MHRB and psychological traits/states cluster together. Such findings have the potential to inform tailored, precision medicine interventions targeted to subpopulations at elevated MHRB risk. The present study employed latent profile analysis to identify whether EF, MD, perceived stress, DI, and anhedonia cluster together in different patterns and whether such patterns influence MHRBs. Specifically cigarette, alcohol, and e-cigarette experimentation were assessed, along with multiple indicators of screen time and consumption of high-calorie/low-nutrient foods, among a diverse, normative sample of 7th grade students. We hypothesized that adolescents exhibiting the lowest levels of EF, MD, and DT with highest levels of stress and anhedonia would report the highest rates of substance use experimentation and obesogenic behavior.
Method
Sample
The sample consisted of 7th graders recruited from two Los Angeles public schools characterized by racially and socioeconomically diverse populations, representative of the regional public school population. Results from this survey were intended to inform the expansion of the theoretical model utilized in the previous Pathways to Health school-based MHRB intervention (Sakuma, Riggs, & Pentz, 2007; Pentz & Riggs 2013) to incorporate additional psychosocial constructs-namely mindfulness, anhedonia, and distress tolerance. Of the 496 enrolled, 410 had parental consent and self-assent, and were used for all subsequent analysis (82.7% of eligible; 22 were absent from measurement, 23 with parental decline, and 58 with administrative decline due to scheduling conflicts). The mean age of participants was 12.5 years, 48% were female, 45% were White, 25% Hispanic, 15% mixed/bi-racial, and 15% other races (Table 1). Thirty-five percent of this seventh-grade sample reported eligibility for the federal free lunch program-an indicator of low socioeconomic status.
Table 1.
Participant Characteristics
| Psychosocial Factors | Multiple Health Risk Behaviors | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N (%) | Executive Function Deficits M (SD) | MAAS Score M (SD) | Distress Tolerance M (SD) | Stress M (SD) | Anhedonia M (SD) | Cigarette Use N (%) | E-Cig Use N (%) | Alcohol Use N (%) | High-Calorie/Low-Nutrient Food Intake N (%) | Screen Time N (%) | |
| All Subjects | 410 (100) | N=350 | N=364 | N=181^ | N=366 | N=183^ | N=407 | N=406 | N=405 | N=383 | N=396 |
| Gender | |||||||||||
| Males | 212 (48) | 1.48 (.30) | 2.37 (.85) | 2.83 (1.09) | 1.76* (.29) | 1.93 (.80) | 16 (7.58) | 25 (11.90) | 14 (6.64) | 2.27 (.85) | 2.67 (1.18) |
| Females | 198 (52) | 1.53 (.32) | 2.48 (.91) | 3.03 (.99) | 1.82* (.32) | 2.04 (.76) | 12 (6.12) | 20 (10.20) | 11 (5.67) | 2.17 (.84) | 2.38 (.96) |
| SES | |||||||||||
| Free Lunch | 143 (35) | 1.55 (.33) | 2.53 (.99) | 2.89 (1.09 | 1.86*** (.30) | 2.17 (.82)* | 21*** (14.69) | 25 (17.73) | 14* (10.0) | 2.29 (.93) | 2.66 (1.10) |
| No Free Lunch | 226 (55) | 1.47 (.29) | 2.38 (.81) | 2.95 (1.01) | 1.74*** (.30) | 1.91 (.77)* | 5*** (2.24) | 16 (7.14) | 9 (4.02) | 2.17 (.82) | 2.42 (1.05) |
| Missing | 41 (10) | ||||||||||
| Ethnicity | |||||||||||
| White | 185 (45) | 1.50 (.33) | 2.43 (.89) | 2.96 (1.06) | 1.79 (.29) | 1.96 (.81) | 8 (4.40) | 13 (7.10) | 8 (4.37) | 2.26 (.87) | 2.43 (1.03) |
| African-American | 7 (2) | 1.51 (.29) | 2.89 (1.06) | 3.00 (1.45) | 1.83 (.13) | 1.75 (.66) | 1 (14.29) | 2 (28.57) | 0 (0) | 2.26 (.63) | 2.94 (2.20) |
| Hispanic | 104 (25) | 1.50 (.29) | 2.34 (.83) | 2.96 (1.01) | 1.81 (.31) | 1.95 (.72) | 8 (7.69) | 12 (11.65) | 6 (5.88) | 2.17 (.84) | 2.56 (.92) |
| Asian | 18 (4) | 1.39 (.21) | 2.46 (.94) | 2.85 (1.11) | 1.74 (.28) | 1.78 (.64) | 1 (5.56) | 2 (11.11) | 0 (0) | 1.82 (.60) | 2.41 (1.18) |
| Mixed/Bi-Racial | 61 (15) | 1.58 (.35) | 2.48 (.95) | 2.84 (1.25) | 1.79 (.34) | 1.95 (.71) | 6 (9.84) | 11 (18.33) | 8 (13.11) | 2.29 (.87) | 2.71 (1.28) |
| Other | 19 (5) | 1.52 (.25) | 2.41 (.86) | 2.42 (.92) | 1.76 (.31) | 2.41 (1.01) | 1 (5.26) | 2 (10.53) | 1 (5.26) | 2.47 (.85) | 3.04 (1.49) |
| Missing | 16 (4) | ||||||||||
Note.
Missingness was planned for the anhedonia and distress intolerance assessments via a split-form design. Only version (B) contained the Distress Tolerance and Anhedonia items, which was administered to N=200.
Measures
A cross-sectional, survey was administered via paper-and-pencil during school to consented/assented students. The survey included scales and sub-scales from the following, validated measures. A split-form to reduce participant burden and increase the total number of individual states/traits assessed (Rhemtulla & Little, 2012). Different split forms (A and B) were randomly administered by row in each classroom, such that both forms were administered within each classroom and school. The only difference in the forms with respect to the above variables were that only Form B included anhedonia and distress tolerance items.
Executive function was assessed by the following four subscales of the Behavior Rating Inventory of Executive Function-Self Report: inhibitory control, emotional control, working memory, and organization of materials (Patrick, Wightman, Schoeni, & Schulenberg, 2012). The BRIEF was designed to be an appropriate and ecologically valid measure of EF associated with goals and actions in everyday problem-solving situations encountered by school-age children, rather than an indicator of laboratory or structured task performance (Toplak, West, & Stanovich, 2013). A reverse-coded mean of the 40 items was used as an indicator of composite EF. Chronbach’s alpha demonstrated good reliability of the 40 items (α=.93). Reverse-coded mean scores ranged from 1 to 2.8 (out of 3).
Mindfulness disposition was assessed by the 15 item Mindful Attention Awareness Scale (Brown & Ryan, 2003), which is typically reverse-coded, but in order to achieve consistent directionality with the other psychosocial individual states/traits, it was kept as administered, with higher values indicating less mindful awareness. For age appropriateness, we adapted the item: “I drive places on ‘automatic pilot’ and then wonder why I went there” to “I walk into a room, and then wonder why I went there.” Chronbach’s alpha demonstrated good reliability of the 15 items (α=.88). Mean scores ranged from 1–5.7 (out of 6).
Perceived stress was assessed using the 10-item Cohen’s Perceived Stress Scale (Cohen et al., 1983), which demonstrated adequate reliability (α=.69). Example items include, “I felt that I could handle important things that were happening in my life” and “I felt difficulties were piling up so high that I could not overcome them.” Response options for stress experience in the last week ranged from 1 = “never” to 3 = “often” and mean scores were calculated so a higher score represents higher perceived stress, which ranged from 1.1 to 2.8 (out of 3).
Distress tolerance was assessed using the following 3 items, which comprise the Regulation subscale of the Distress Tolerance Scale (Simons & Gaher, 2005), designed to assess behavioral regulation efforts taken by participants to alleviate distress. Items include, “When I feel distressed or upset, I must do something about it immediately”; “I’ll do anything to stop feeling distressed or upset.”; and “I’ll do anything to avoid feeling distressed or upset.” Chronbach’s alpha for the 3 items was (α=.75). Item responses ranged from 1 to 5, where a higher score indicates greater ability to tolerate distress. For the current study, the mean was reversed-coded so that a higher score indicates greater distress tolerance Missingness was planned such that only subsample B (N=200) received the 3 distress tolerance items..
Anhedonia was assessed using the following four items, which were adapted from past work (Leventhal, Ramsey, Brown, LaChance, & Kahler, 2008), “I felt that I was just as good as other people”; “I felt hopeful about the future”; “I was happy”; “I enjoyed life.” These items prompted participants to consider their experiences over the past 2 weeks and select the appropriate box from the following: Rarely or none of the time (0–1 days); Some or a little of the time (2–3 days); Occasionally or a moderate amount of the time (4–5 days); Most or all of the time (6–7 days). Responses were recoded such that higher scores reflect greater levels of anhedonia. The four items demonstrated good reliability (α=.82) and reverse-coded mean scores ranged from 1 to 4. Again, missingness was planned such that only subsample B (N=200) were administered the 4 anhedonia items.
Cigarette, E-cigarette, and alcohol use experimentation were assessed by the following three questions which were adapted from The national Monitoring the Future survey on adolescent Substance Use (Johnston, 2014): “Have you ever… smoked a cigarette in your whole life?”; “used an e-cigarette, such as Smoking Everywhere, NJOY, Blu or Vapor King, even one or two times?”; “tried alcohol (beer, wine, liquor that is not for religious purposes)?” Lifetime reported use of each substance was coded dichotomously as any/none.
High-calorie/low-nutrient food intake (HCLN was measured with open-source food frequency questionnaire items, taken from previous work (Huh et al., 2011; Pentz, Spruijt-Metz, Chou, & Riggs, 2011): “How often do you… eat French fries or fried potatoes?”; “eat corn chips, potato chips, popcorn, crackers?”; “eat doughnuts, pastries, cake, cookies?”; “eat candy (chocolate, hard candy, candy bars)?”; “drink soda-not diet (1 can or glass)?” The following response options were provided: “1=Less than once a week; 2=Once a week; 3=2–3 times a week; 4=4–6 times a week; 5= Once a day; 6=2 or more of these a day”. A mean score of all 5 items assessed overall consumption of HCLN foods.
Screen time was assessed via the following items: “On a regular school day, how many hours per day do you (a) usually watch TV or video movies at home or away from school, (b) spend on a computer at home or away from school and (c) play video games that you sit down to play like PlayStation, Xbox, GameBoy, or arcade games. Responses ranged from 0 (“I don’t watch TV”) to 6 (“6 or more hours”). As in previous work, a composite score was created by taking the mean across these 3 items (Hoelscher, Day, Kelder, & Ward, 2003; Huh et al., 2011).
Analytic Plan
First, since a split-form with planned missingness was utilized, subsamples A (N=200) and B (N=210) were compared to determine whether there were any demographic, psychosocial, or health risk behavior differences. Responses from both subsamples were pooled for analysis as they did not differ significantly by demographics, psychosocial factors, or MHRB (p>.05). Latent Profile Analysis (LPA) is a statistical method used to classify individuals into distinct groups, which were themselves not directly measured (and thus considered “latent”), using continuous indicator variables. This technique is closely related to latent class analysis, which is utilized for categorical indicator variables. In our study, LPA was conducted to determine whether the assessed psychosocial factors cluster together into latent profiles, the extent to which sociodemographic factors (i.e. gender, socioeconomic status (SES), race/ethnicity) predict latent profile membership, and whether levels of MHRB differ between latent profiles. MPlus 7.4 was used for LPA, employing a robust full-information maximum likelihood estimator that leverages all available data in order to minimize the bias and variance of resulting parameter estimates, while accounting for missingness (Cham, Reshetnyak, Rosenfeld, & Breitbart, 2017). Unplanned missingness was low, with only 1% of participants missing data for MHRB), 8–15% missing data on any item assessing psychosocial factors and 0–10% missing data on demographic characteristics, Given that study personnel did not observe any systematic factor influencing unplanned non-response during data collection, we believe the missing at random assumption to be reasonable. In recent years, such latent variable modeling methods have been increasingly utilized in the field of behavioral medicine to identify high-risk subpopulations based on specific patterns of psychosocial and/or behavioral characteristics, in order to guide the development of future prevention interventions (Champion et al, 2018; Jao et al, 2018).
All five individual states/traits were used for latent profile estimation-perceived stress, EF, MD, DT, and anhedonia. Once the optimal class solution was determined, sociodemographic predictors of latent profile membership were tested via a three-step procedure (R3STEP), which accounts for classification uncertainty (i.e., measurement error) while ensuring that latent profile formation is not influenced by the following included covariates: participant gender, socioeconomic status (assessed by federal free school lunch eligibility vs. not), White ethnicity, and Hispanic ethnicity (Vermunt, 2010). Mean levels of self-reported screen time and high-calorie/low-nutrient food intake was estimated and compared across latent profiles using the BCH method--the optimal procedure for mean estimation of continuous distal outcomes associated with latent profile membership. Proportions of self-reported substance use were estimated and compared using the DCAT method, the optimal procedure for estimation of categorical distal outcomes associated with latent profile membership (Asparouhov, 2014).
To determine the most appropriate number of latent profiles (Nylund, 2007), we employed an iterative process where the 5-indicator model was fit with an increasing number of profiles, beginning with a single profile. The Lo-Mendell Rubin Test and multiple Information Criteria were calculated and compared to determine the best fitting, most parsimonious solution. In sum, the Lo-Mendell Rubin Test found a 3-profile solution to offer significantly improved fit relative to a 2-profile solution (p=.005), while a 4-profile solution did not significantly improve fit relative to a 3-profile solution (p=.29). Evaluation of AIC, BIC, and sample-size adjusted BIC also confirmed the optimality of a 3-profile solution with minimal improvement in fit observed beyond a 3-profile solution. Good separation of classes was observed for the optimal, 3-profile solution with an estimated relative entropy value of .8 (Celeux, 1996) and estimated classification probabilities ranging from .88-.92. For data visualization, posterior probabilities of latent class membership for each participant were then calculated using the three-class model and participant was assigned to the class for which he or she had the maximum posterior probability.
Results
Descriptive characteristics for each of the five psychosocial indicators used for the latent profile analyses are reported along with descriptive characteristics for the five health risk behaviors assessed in the study in Table 1. Psychosocial characteristics were invariant by race. However, low SES participants reported significantly higher stress, greater anhedonia, and lower levels of EF than their higher SES peers and females reported significantly higher stress than males. Strong zero-order correlations were observed with each of the two major domains of MRHB (i.e., substance use behaviors (r=.42-.50) and obesogenic behaviors (r=.34). Correlations were more heterogeneous in magnitude between the five assessed psychosocial factors, with the highest correlations observed between EF and MD (r=.74) and the lowest among distress tolerance and each of the other 4 assessed factors (|r|=.0-.06).
As visualized in Figure 1, latent Profile 1, which was the most likely class for 8% of our sample, was characterized by the lowest levels of EF, MD, DT, and greatest levels of stress and anhedonia of the three profiles. Conversely, profile 3, which was the most likely class for 48% of the sample, reported the greatest levels of EF, MD, DT and lowest levels of stress and anhedonia among the three profiles. Profile 2 comprised 44% of the sample and represented an intermediate class with psychosocial characteristics falling between Profiles 1 and 3. When mean values were compared between latent profiles 1 and 3, the differences (derived via independent samples t tests) were statistically significant for EF (two-sided p<.001), MD (p<.001), stress (p<.001), and anhedonia (p=.002)-but not for DT (p=.78). Estimated Hedges’ g effect sizes comparing mean differences between profiles 1 and 3 were as follows: EF (g=2.74), MD (g=2.34), stress (g=1.58), anhedonia (g=.93), and DT (g=.06).
Figure 1.
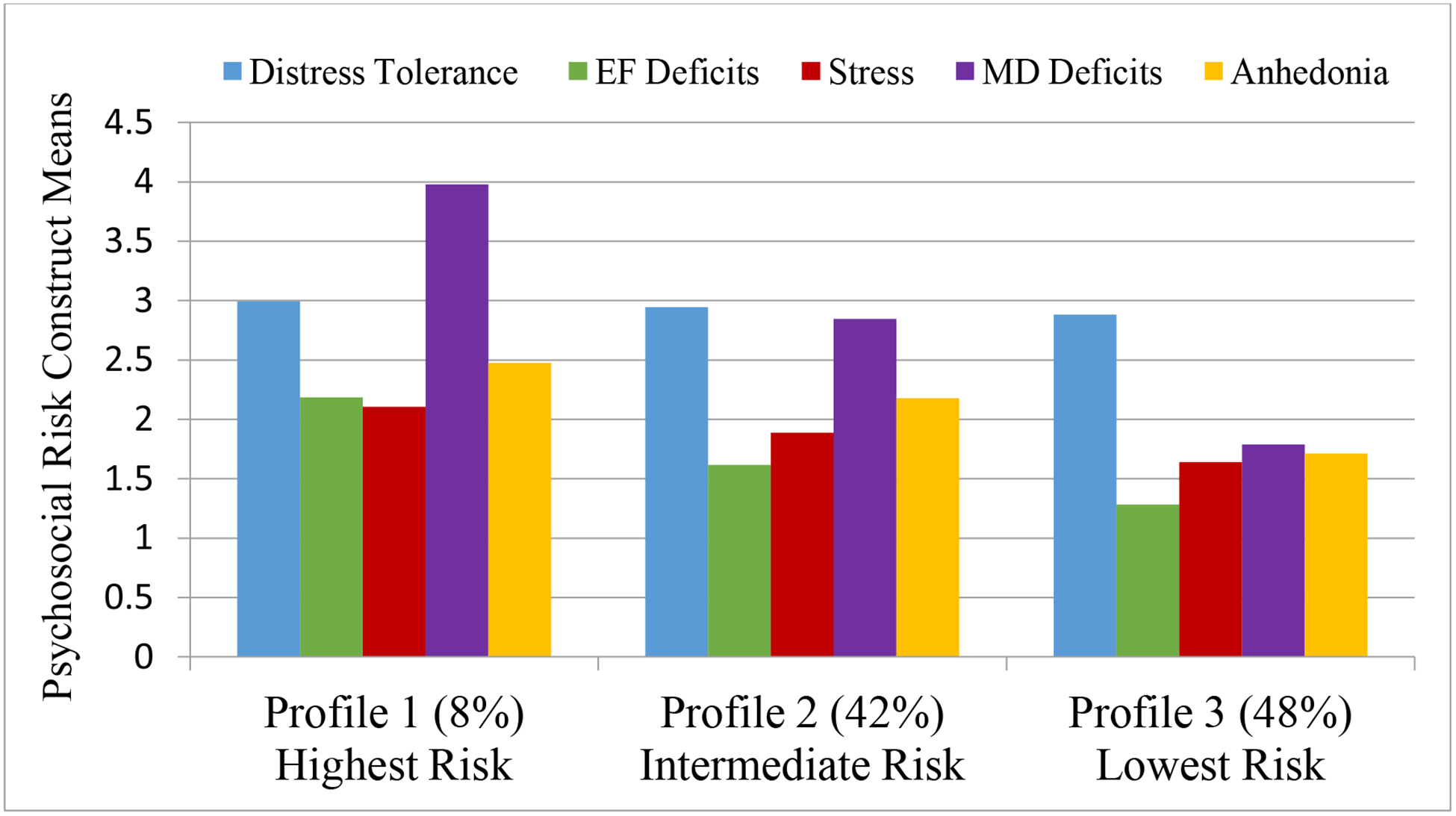
Psychosocial Characteristics by Latent Profile Membership (N=410)
Significant differences emerged between latent profiles regarding their relationship to both obesity and substance use risk (Figure 2). With respect to substance use, e-cigarette and cigarette use experimentation were more frequent among members of profiles 1 (p<.1) and 2 (p<.05), relative to profile 3, with the highest rates observed among members of profile 1. Alcohol use experimentation was also more common among members of profiles 1 (p<.05) and 2 (p<.01) relative to profile 3 with the highest rates observed within profile 1. Similarly, screen time and high-calorie/low-nutrient food consumption were each significantly more common among members of profiles 1 and 2, relative to profile 3 (p<.01). See Table 2 for the means and probabilities of each health risk behavior by most likely latent profile membership. When participant gender, SES, and race were tested as predictors of latent profile membership associations were only significant for SES. Specifically, relative to profile 3 members, profile 1 members were significantly more likely to be low SES (B=1.05; p=.04).
Figure 2.
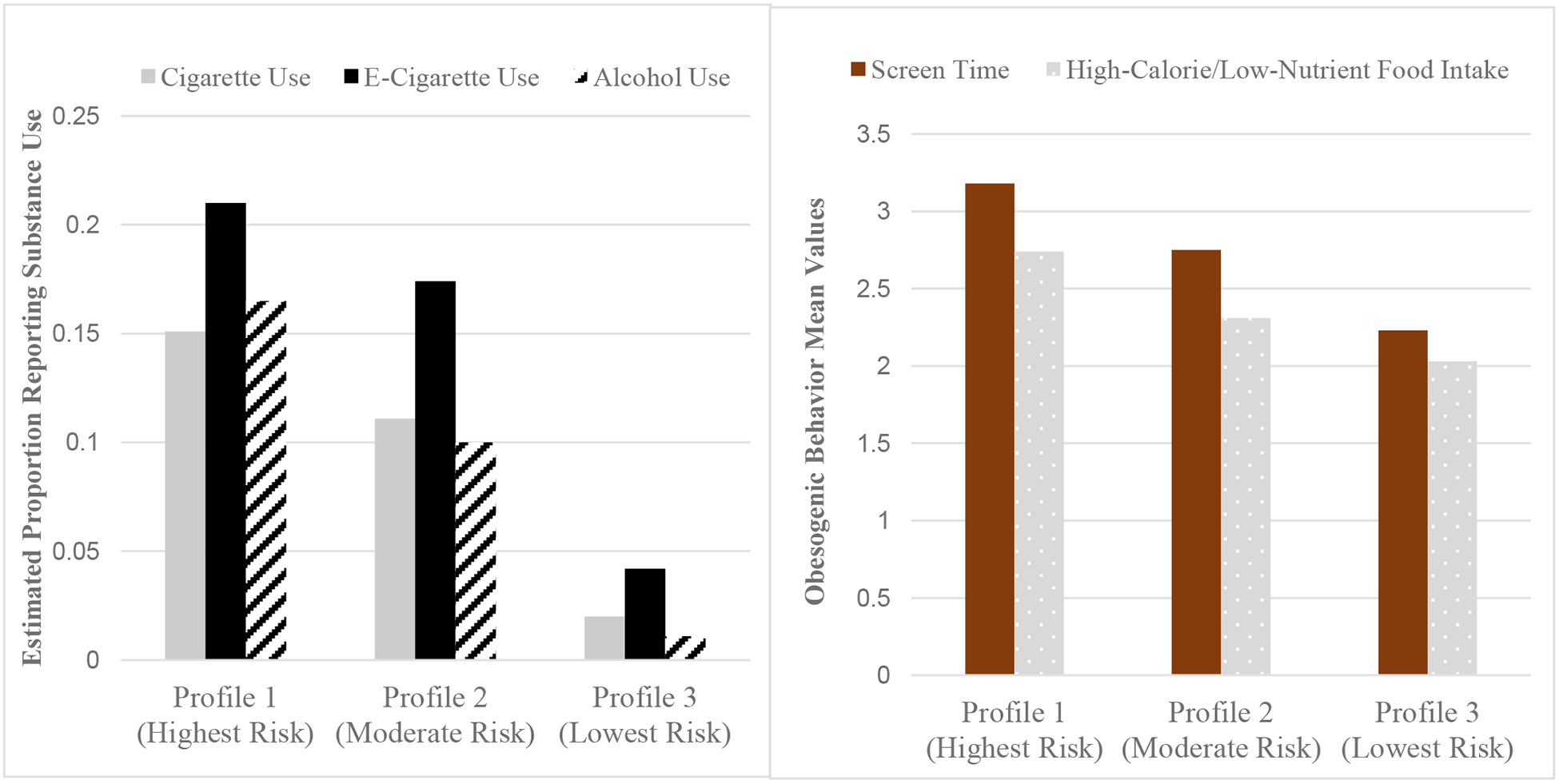
Estimated Probabilities of Substance Use and Obesogenic Behaviors by Latent Profile
Table 2.
Estimated proportions of participants reporting each health risk behavior by latent profile
| Highest Risk Profile 1 (8% of sample) | Moderate Risk Profile 2 (44% of sample) | Lowest Risk Profile 3 (48% of sample) | ||
|---|---|---|---|---|
| Substance Use | ||||
| .15 (.08)+ | .11 (.03)** | .02 (.01)+ ** | ||
| .21 (.09)+ | .17 (.04)** | .04 (.02)+ ** | ||
| .17 (.08)* | .10 (.03)** | .01 (.01)* ** | ||
| Obesogenic Behavior | ||||
| 3.18 (.28)** | 2.75 (.10)*** | 2.23 (.08)** *** | ||
| High-Calorie/Low-Nutrient Food Intake | 2.74 (.20)** + | 2.31 (.07)** + | 2.03 (.06)** ** | |
Pairwise contrast significant at two-sided p<.1+ p<.05* p<.01** p<.001***
Contrasts between 1 and 2 and 1 and 3 utilize black symbols, while red symbols indicate significant contrasts between Profiles 2 and 3.
Figure 3 shows that the latent highest risk profile (which represented 8% of the sample) has higher rates of MHRB than do individuals falling within the top 8% of each of its five constituent indicators.
Figure 3.
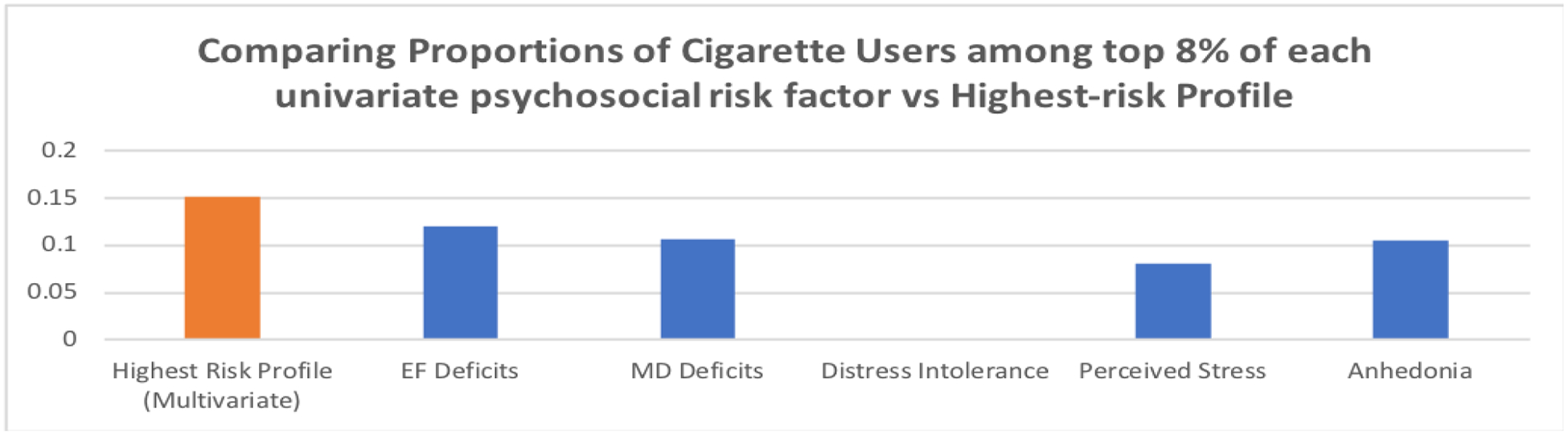
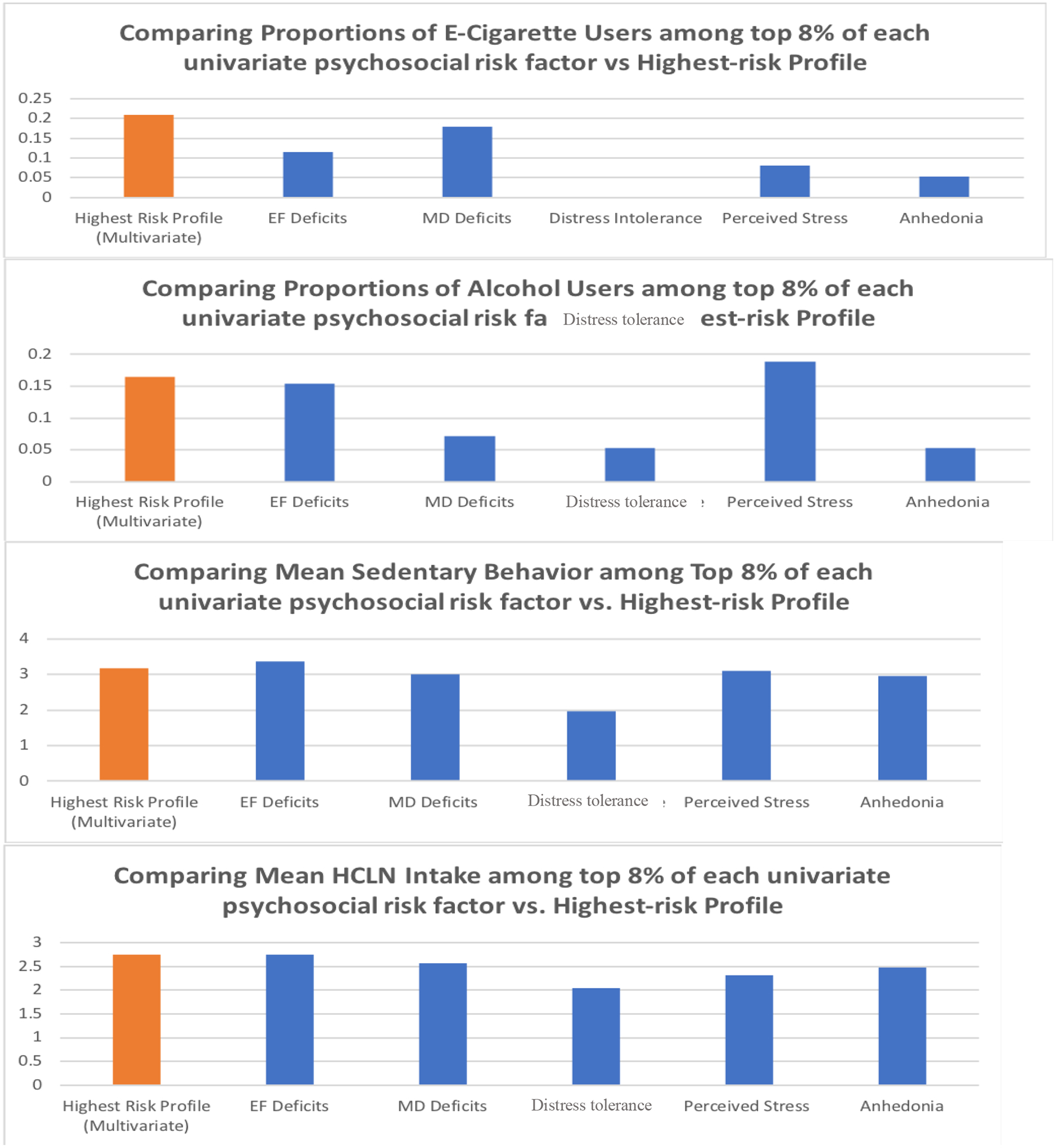
Comparing levels of MHRB between highest risk profile (8% of sample) vs. comparably sized subgroups reporting the highest levels of each individual psychosocial construct
Discussion
The current study identified three latent psychosocial risk profiles, which were associated with different patterns of both substance use and obesogenic behavior in a socio-demographically diverse cohort of 7th grade students. MHRBs typically are established, and increase throughout, adolescence. Thus developing and tailoring intervention programs that promote positive health behaviors among the populations most at risk have the potential to impact not only adolescent well-being but also the public health burden that follows substance use and obesity-related sequelae. In order to build the most efficacious programs, researchers and clinicians must examine data using a holistic, person-centered approach. This includes characterizing behaviors alongside well-understood individual psychosocial characteristics in order to synthesize these highly intersecting pieces of the human experience. The presented latent profile analyses demonstrate clear clustering of these characteristics and their reliable associations with MHRBs. Specifically, profile 1 represented 8% of the sample and was characterized by the lowest levels of EF, MD, and DT with highest levels of perceived stress and symptoms of anhedonia, exhibited increased risk for both substance use and obesogenic behaviors. Cigarette, e-cigarette, and alcohol use experimentation were each reported by over 15% of the highest risk profile, compared to well below 5% of the lowest risk profile. This suggests that not only are these differences statistically significant, but highly clinically significant as well, given that students in risk profile 1 are 6.5, 4, and 14 times more likely to report cigarette, e-cigarette, and alcohol use experimentation than their counterparts in risk profile 3. Similarly, screen time and consumption of high-calorie/low-nutrient foods were each significantly greater among the highest risk profile, relative to the lowest risk profile. It is notable that the observed 1 point difference in mean composite screen time scores between the highest and lowest risk profiles is equivalent to an approximately 3 hour/day difference in aggregate daily out-of-school screen-time (TV, computer, and/or videogames). At the same time, a 1 point mean difference in high-calorie/low-nutrient food intake from 2 to 3, would be comparable to increasing intake of each of the 5 assessed HCLN foods from once weekly, to 2–3 times weekly, rendering the observed .74 point difference a meaningful increase in obesogenic food consumption. Therefore, if future longitudinal research work supports the hypothesis that the formation of these psychosocial risk classes indeed precedes MHRB, then secondary prevention programs could be used to supplement universal prevention interventions by specifically targeting maladaptive intake behaviors for the higher risk populations comprising Profile 1.
Early adolescence is a key developmental period for MHRB initiation/escalation and represents a time when cognitive and environmental influences emerge that can increase susceptibility to MHRB. For example, during early adolescence functional networks of neural regions implicated in executive functioning (e.g., behavioral inhibition, emotional regulation) are less myelinated than corresponding brain regions involved in reward sensitivity, which can render adolescents at increased risk of initiating or continuing MHRB which are increasingly normative (Gogtay et al., 2004). Access to nicotine, alcohol, and fast food also generally increases during this time as adolescents gain autonomy and play a larger role in their own heath decisions. Further, during middle school, peer influences on behavior (including MHRB) tend to increase substantially while parental monitoring can diminish (Simons-Morton, et al 2001). In the context of adolescent substance use, psychological dysregulation has been proposed as an overarching individual-level construct and that may interact with these socioenvironmental influences to increase MRHB risk. Given that psychological dysregulation has been defined as deficiency within cognitive, behavioral, and emotional domains when adapting to environmental challenges, it is possible that the latent profiles identified here represent elevated, moderate and low levels of psychological dysregulation (Tarter et al, 2003). In this conceptualization, low levels of executive function and mindfulness disposition would be indicative of dysfunction within the cognitive domain, anhedonia and perceived stress would be indicative of dysfunction within the emotional domain, while lower levels of distress tolerance (since the behavioral regulation subscale of the DTS was utilized) would be indicative of dysfunction within the behavioral domain. Given the low correlations observed here between the regulation subdomain of distress tolerance and the other 4 latent profile indicators, future research should consider incorporating assessment of externalizing behavior or other more established indicators of behavioral dysregulation (e.g., The Childhood Behavior Checklist; Achenbach & Ruffle, 2000) that may provide further separation between the latent profiles. To the extent that the profiles identified here may represent different levels of psychological dysregulation, these data extend previous work linking psychological dysregulation with increased risk of alcohol and tobacco use to other MHRB including obesogenic behaviors and e-cigarette use (Thatcher & Clark, 2008).
In recent years, e-cigarettes have become a substantial public health concern due to increasing use among adolescents (Prevention, 2016), their lack of demonstrated safety, as well as their associations with poly-substance and future cigarette use (Barrington-Trimis et al., 2016; Leventhal et al., 2015; Public health consequences of e-cigarettes, 2018). To wit, in the present sample, reported e-cigarette use rates were higher than those for alcohol or cigarettes. Given their lack of regulation, perceptions of safety, surreptitiousness, and ease of acquisition relative to other nicotine products, e-cigarettes present a complex, novel prevention target. These data indicate that prevention programs which can help adolescents achieve high EF, MD, and DT, while reducing anhedonia and perceived stress, may have downstream effects on MHRB, including use of e-cigarettes and other alternative tobacco products. Moreover, interventions, such as mindfulness-based interventions, which target multiple shared psychosocial antecedents of MHRB and the behaviors themselves may be particularly promising (Kechter & Black, in press) in light of current findings that adolescents comprising the highest risk profile (taking into account all 5 psychosocial factors) reported higher rates of MHRB than did comparably sized quantiles of adolescents with the poorer levels on each individual factor.
While participant gender and racial/ethnic background did not reliably predict latent profile membership, low SES students were significantly more likely to be assigned to profile 1-characterized by low EF and MD in addition to high anhedonia and perceived stress. This finding extends previous national survey research linking socioeconomic privation and increased cigarette use risk, by positing a pathway through increased psychosocial risk involving multiple determinants (e.g., low EF and high stress and anhedonia) that extends to alcohol and e-cigarette use as well (Patrick et al., 2012; Pampel, Krueger, & Denney, 2010). While it is important to note that there are well-acknowledged limitations to characterizing student SES via reported free lunch eligibility alone (Harwell & LeBeau, 2010)-these findings are consistent with the idea that SES in general may have a significant association with MHRBs, and that this increased MHRB risk is associated with specific profiles of individual-level psychosocial characteristics, which themselves are amenable to intervention. Furthermore, socioeconomic deprivation itself has been conceptualized as a key modifiable health risk factor (Stringhini et al, 2017) and can be meaningfully influenced by local (Rasella et al 2013), national (Lleras-Muney, 2005), and international policies. In light of other evidence that socioeconomic privation is independently associated with worse EF, greater perceived stress, and greater MHRB risk (Pentz & Riggs, 2013; Ursache, Noble, & Blair 2016; Denny, Kreuger, & Pampel, 2014), this suggests that participant SES should be an important consideration for MHRB prevention interventions as well as those targeting the aforementioned psychosocial characteristics.
Limitations and Future Directions
A few limitations of this investigation should be noted. First, this study relies upon cross-sectional latent profile analysis, and further longitudinal research is needed to better examine the temporality and putative causal relationships between risk indicators common for both substance use and obesogenic behaviors among early adolescents. For example, it is plausible that greater engagement in MHRB leads to adverse psychosocial outcomes or that these constructs are related in a bidirectional manner, which cross-sectional surveys are poorly-equipped to characterize. Furthermore, an important limitation of this cross-sectional survey research is the possibility of response and monomethod biases, however care was taken in both the parental consent and student assent forms to emphasize that responses would be kept strictly confidential and not shared with parents, peers, nor teachers. Future research should consider augmenting student self-report with parent- and/or teacher-report as well as possible computerized task-based measures of EF and DT, which could potentially lead to less biased, more precise measurement of these key constructs. In particular, incorporation of multi-method and or comprehensive assessment of EF and mindfulness than the self-report survey-based behavioral inventories utilized here, may permit more clear differentiation between the unique contributions of each construct to the establishment of the aforementioned latent profiles of MHRB risk. It is notable that EF and mindfulness were not only highly correlated (r=.74) in the present study, but that both exhibited nearly identical correlations with the examined health behaviors. As such, it remains unclear whether the responses obtained from the MAAS and BRIEF-SR reflect distinct underlying meta-cognitive processes, despite utilizing validated survey measures for both constructs. However, we believe that retaining both EF and MD in our final models is useful given 1) that a key aim of this study was to understand the extent to which these variables cluster together and with MHRB, and 2) the BRIEF and MAAS are each routinely administered to adolescents, but in distinct contexts-therefore if they are highly correlated and exhibit similar associations with MHRB-this may help guide the selection of minimally burdensome scales to administer in future school-based work. That said, future studies incorporating more comprehensive multi-modal and/or multi-factorial assessment may still find particular subdomains of MD or EF to be more dissociable and uniquely predictive of MHRB. Future longitudinal work may also consider the temporal sequence of MD and EF, and how they may function both as potential mediators of prevention intervention effectiveness as well as outcomes of interest. For example, a recent review (Semenov & Zelazo 2019) describes numerous putative mechanisms through which cultivation of a mindful disposition can support mobilization of EF resources-for example by reducing the influence of automatic, bottom-up stimuli on attention and other cognitive processes while also strengthening top-down meta-cognitive networks. In their conceptualization, individuals with high disposition toward receptive awareness of and attention to the present moment (what is measured by the MAAS) will likely find it easier to engage the top-down EF skills assessed by the BRIEF-SR (e.g. working memory, inhibitory control, emotional regulation). Furthermore, frequent practice of mindfulness has also been shown to directly influence the same neural networks involved in mobilization of EF. Conversely, without sufficient EF resources, children may find it difficult to engage in mindfulness practice due to the overwhelming salience of distracting bottom-up stimuli.
Furthermore in this study, DT was measured using a subscale of the distress tolerance scale that captures self-regulation. The DTS regulation subscale assesses the degree to which individuals behave in ways to immediately terminate distress. The three other DTS subscales (absorption, appraisal, tolerance) more closely capture the perceived ability to maintain attention and experience distress, without a behavioral focus. Therefore, it remains unknown if these other, unassessed aspects of DT have similar relationships to the latent psychosocial risk profiles observed here. Similar to DT, anhedonia was measured using only 4-items adapted from a previous study (Leventhal, Ramsey, Brown, LaChance, & Kahler, 2008). However, several previous investigations using these 4 items have shown adequate utility measuring anhedonia in children (Shafer 2006). Finally, sedentary behavior measured in this study only included screen time, and did not include other sedentary behaviors such as reading. However, links between screen time and MHRB have been previously documented (Robinson et al., 2017) However, future investigations examining sedentary behavior should incorporate additional behaviors (e.g. reading, homework). That said, despite these design and measurement limitations, our findings have transdiagnostic implications for how we may best identify and target youth most at-risk for initiation and escalation of MHRB, including substance use and obesogenic behaviors.
Future work assessing these individual-level psychosocial states/traits over time can evaluate the longitudinal stability of these latent profiles and the effects of transitioning between profiles over time. Insights gleaned from such work have the potential to improve MHRB screening and prevention efforts by identifying the most important and malleable psychosocial individual states/traits to target and the subpopulations who may be most likely to benefit from targeted interventions.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- Achenbach TM & Ruffle TM (2000). The Child Behavior Checklist and Related Forms for Assessing Behavioral/Emotional Problems and Competencies. Pediatrics in Review, 21(265). doi: 10.1542/pir.21-8-265 [DOI] [PubMed] [Google Scholar]
- Adam TC, & Epel ES (2007). Stress, eating and the reward system. Physiology & Behavior, 91(4), 449–458. doi: 10.1016/j.physbeh.2007.04.011 [DOI] [PubMed] [Google Scholar]
- Allan JL, McMinn D, & Daly M (2016). A Bidirectional Relationship between Executive Function and Health Behavior: Evidence, Implications, and Future Directions. Frontiers in Neuroscience, 10, 386. doi: 10.3389/fnins.2016.00386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asparouhov T M. B; . (2014). Auxiliary variables in mixture modeling: Using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. Mplus Web Notes, 21(2), 1–22. [Google Scholar]
- Barrington-Trimis JL, Urman R, Berhane K, Unger JB, Cruz TB, Pentz MA, … McConnell R (2016). E-Cigarettes and Future Cigarette Use. Pediatrics, 138(1). doi: 10.1542/peds.2016-0379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakemore SJ, & Choudhury S (2006). Development of the adolescent brain: implications for executive function and social cognition. Journal of Child Psychology and Psychiatry, 47(3–4), 296–312. doi: 10.1111/j.1469-7610.2006.01611.x [DOI] [PubMed] [Google Scholar]
- Brown KW, & Ryan RM (2003). The benefits of being present: mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822–848. [DOI] [PubMed] [Google Scholar]
- Cappelli C, Pike JR, Riggs NR, Warren CM, & Pentz MA (2019). Executive function and probabilities of engaging in long-term sedentary and high calorie/low nutrition eating behaviors in early adolescence. Social Science & Medicine, 237, 112483. doi: 10.1016/j.socscimed.2019.112483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celeux G,; Soromenho G;. (1996). An entropy criterion for assessing the number of clusters in a mixture model. Journal of Classification, 13, 195–212. [Google Scholar]
- Cham H, Reshetnyak E, Rosenfeld B, & Breitbart W (2017). Full Information Maximum Likelihood Estimation for Latent Variable Interactions With Incomplete Indicators. Multivariate Behavioral Research, 52(1), 12–30. doi: 10.1080/00273171.2016.1245600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Champion KE, Mather M, Spring B, Kay-Lambkin F, Teesson M, Newton NC. (2018). Clustering of multiple risk behaviors among a sample of 18-year old Australians and associations with mental health outcomes: A latent class analysis. Frontiers in public health, 6(135). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. [PubMed] [Google Scholar]
- Cummings JR, Bornovalova MA, Ojanen T, Hunt E, MacPherson L, & Lejuez C (2013). Time doesn’t change everything: the longitudinal course of distress tolerance and its relationship with externalizing and internalizing symptoms during early adolescence. Journal of Abnormal Child Psychology, 41(5), 735–748. doi: 10.1007/s10802-012-9704-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallman MF (2010). Stress-induced obesity and the emotional nervous system. Trends in Endocrinology and Metabolism, 21(3), 159–165. doi: 10.1016/j.tem.2009.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daubenmier J, Kristeller J, Hecht FM, Maninger N, Kuwata M, Jhaveri K, … Epel E (2011). Mindfulness Intervention for Stress Eating to Reduce Cortisol and Abdominal Fat among Overweight and Obese Women: An Exploratory Randomized Controlled Study. Journal of Obesity, 10.1155/2011/651936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denny JT, Kreuger PM, & Pampel FC (2014). Socioeconomic status and health behaviors. The Wiley Blackwell Encyclopedia of Health, Illness, Behavior, and Society. doi: 10.1002/9781118410868.wbehibs54 [DOI] [Google Scholar]
- Der-Avakian A, & Markou A (2012). The neurobiology of anhedonia and other reward-related deficits. Trends in Neurosciences, 35(1), 68–77. doi: 10.1016/j.tins.2011.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond A (2013). Executive functions. Annual Review of Psychology, 64, 135–168. doi: 10.1146/annurev-psych-113011-143750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felton JW, Banducci AN, Shadur JM, Stadnik R, MacPherson L, & Lejuez CW (2017). The developmental trajectory of perceived stress mediates the relations between distress tolerance and internalizing symptoms among youth. Development and Psychopathology, 29(4), 1391–1401. doi: 10.1017/S0954579417000335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleary S (2017). Combined Patterns of Risk for Problem and Obesogenic Behaviors in Adolescents: A Latent Class Analysis Approach. Journal of School Health, 87(3), 182–193. 10.1111/josh.12481 [DOI] [PubMed] [Google Scholar]
- Fossati A, Vigorelli Porro F, Maffei C, & Borroni S (2012). Are the DSM-IV personality disorders related to mindfulness? An Italian study on clinical participants. Journal of Clinical Psychology, 68(6), 672–683. doi: 10.1002/jclp.21848 [DOI] [PubMed] [Google Scholar]
- Garland EL, Hanley AW, Thomas EA, Knoll P, & Ferraro J (2015). Low dispositional mindfulness predicts self-medication of negative emotion with prescription opioids. Journal of Addiction Medicine, 9(1), 61–67. doi: 10.1097/ADM.0000000000000090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gogtay N, Giedd JN, Lusk L, Hayashi KM, Greenstein D, Vaituzis AC, Nugent TF, Herman DH, Clasen LS, Toga AW, Rapoport JL, Thompson PM (2004). Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci U S A 101(21), 8174–8179. doi: 10.1073/pnas.0402680101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale DR, Fitzgerald-Yau N, Viner RM (2014). A Systematic Review of Effective Interventions for Reducing Multiple Health Risk Behaviors in Adolescence. American Journal of Public Health. 104(5): e19–e41. doi: 10.2105/AJPH.2014.301874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey PO, Pruessner J, Czechowska Y, & Lepage M (2007). Individual differences in trait anhedonia: a structural and functional magnetic resonance imaging study in non-clinical subjects. Molecular Psychiatry, 12(8), 703, 10.1038/sj.mp.4002021 [DOI] [PubMed] [Google Scholar]
- Harwell M, & LeBeau B (2010). Student eligibility for a free lunch as an SES measure in education research. Educational Researcher, 39(2), 120–131. doi: 10.3102/0013189X10362578 [DOI] [Google Scholar]
- Heckman JJ (2006). Skill formation and the economics of investing in disadvantaged children. Science, 312(5782), 1900–1902. doi: 10.1126/science.1128898 [DOI] [PubMed] [Google Scholar]
- Ho N, & Sommers M (2013). Anhedonia: a concept analysis. Archives of Psychiatric Nursing, 27(3), 121–129. doi: 10.1016/j.apnu.2013.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoelscher DM, Day RS, Kelder SH, & Ward JL (2003). Reproducibility and validity of the secondary level School-Based Nutrition Monitoring student questionnaire. Journal of Americamn Dietetic Association, 103(2), 186–194. doi: 10.1053/jada.2003.50031 [DOI] [PubMed] [Google Scholar]
- Huh J, Riggs NR, Spruijt-Metz D, Chou CP, Huang Z, & Pentz M (2011). Identifying patterns of eating and physical activity in children: a latent class analysis of obesity risk. Obesity (Silver Spring), 19(3), 652–658. doi: 10.1038/oby.2010.228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jao NC, Robinson LD, Kelly PJ, Ciecierski CC, & Hitsman B (2018). Unhealthy behavior clustering and mental health status in United States college students. Journal of American College Health, 1–11. doi: 10.1080/07448481.2018.1515744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD O. M. PM; Bachman JG;. (2014). Monitoring the future national survey results on drug use, 1975–2013. Retrieved from Ann Arbor, MI: [Google Scholar]
- Katterman SN, Kleinman BM, Hood MM, Nackers LM, & Corsica JA (2014). Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eating Behaviors, 15(2), 197–204. doi: 10.1016/j.eatbeh.2014.01.005 [DOI] [PubMed] [Google Scholar]
- Kechter A, Black DS, Riggs NR, Warren C, Ritt-Olson A, Chou CP, & Pentz MA (in press). Perceived Distress Associated with Mindfulness Disposition and Executive Function in Early Adolescents. Journal of Child and Family Studies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kechter A & Black DS (2020) Mindfulness-Based Interventions Applied to Addiction Treatment In S. Sussman, Cambridge Handbook of Substance and Behavioral Addictions. [Google Scholar]
- Keng SL, Smoski MJ, & Robins CJ (2011). Effects of mindfulness on psychological health: a review of empirical studies. Clinical Psychology Review, 31(6), 1041–1056. doi: 10.1016/j.cpr.2011.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khurana A, Romer D, Betancourt LM, Brodsky NL, Giannetta JM, & Hurt H (2015). Experimentation versus progression in adolescent drug use: A test of an emerging neurobehavioral imbalance model. Development and Psychopathology, 27(3), 901–913. doi: 10.1017/S0954579414000765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leech R, McNaughton S, & Timperio A (2014). The clustering of diet, physical activity and sedentary behavior in children and adolescents: a review. The International Journal of Behavioral Nutrition and Physical Activity, 11(1), 4–4. 10.1186/1479-5868-11-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, Ramsey SE, Brown RA, LaChance HR, Kahler CW. Dimensions of depressive symptoms and smoking cessation. Nicotine & Tobacco Research. 2008b;10(3):507–517. doi: 10.1080/14622200801901971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, Strong DR, Kirkpatrick MG, Unger JB, Sussman S, Riggs NR, … Audrain-McGovern J (2015). Association of Electronic Cigarette Use With Initiation of Combustible Tobacco Product Smoking in Early Adolescence. JAMA, 314(7), 700–707. doi: 10.1001/jama.2015.8950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal A, & Zvolensky M (2015). Anxiety, depression, and cigarette smoking: a transdiagnostic vulnerability framework to understanding emotion-smoking comorbidity. Psychological Bulletin, 141(1), 176–212. 10.1037/bul0000003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, & Bernstein A (2010). Distress tolerance and psychopathological symptoms and disorders: a review of the empirical literature among adults. Psychological Bulletin, 136(4), 576–600. doi: 10.1037/a0019712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lleras-Muney A (2005). The relationship between education and adult mortality in the United States. The Review of Economic Studies, 72(1), 189–221. doi: 10.3386/w8986 [DOI] [Google Scholar]
- Nguyen-Michel ST, Unger JB, & Spruijt-Metz D (2007). Dietary correlates of emotional eating in adolescence. Appetite, 49(2), 494–499. doi: 10.1016/j.appet.2007.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund K L. A. T; Muthén BO;. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural equation modeling, 14(4), 535–569. doi: 10.1080/10705510701575396 [DOI] [Google Scholar]
- Pampel FC, Krueger PM, & Denney JT (2010). Socioeconomic Disparities in Health Behaviors. Annual Review of Sociology, 36, 349–370. doi: 10.1146/annurev.soc.012809.102529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Wightman P, Schoeni RF, & Schulenberg JE (2012). Socioeconomic status and substance use among young adults: a comparison across constructs and drugs. Journal of Studies on Alcohol and Drugs, 73(5), 772–782. doi: 10.15288/jsad.2012.73.772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson N, Haycraft E, P. J. J, & Atkin AJ (2017). Sedentary behaviour across the primary-secondary school transition: A systematic review. Prevention Medicine, 94, 40–47. doi: 10.1016/j.ypmed.2016.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pentz MA, & Riggs NR (2013). Longitudinal relationships of executive cognitive function and parent influence to child substance use and physical activity. Prevention Science, 14(3), 229–237. doi: 10.1007/s11121-012-0312-3 [DOI] [PubMed] [Google Scholar]
- Pentz MA, Riggs RR, & Warren CM (2016). Improving substance use prevention efforts with executive function training. Drug and Alcohol Dependence, June 1;163 Suppl 1:S54–9. doi: 10.1016/j.drugalcdep.2016.03.001. [DOI] [PubMed] [Google Scholar]
- Pentz MA, Spruijt-Metz D, Chou CP, & Riggs NR (2011). High calorie, low nutrient food/beverage intake and video gaming in children as potential signals for addictive behavior. International Journal of Environmental Research and Public Health, 8(12), 4406–4424. doi: 10.3390/ijerph8124406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prakash RS, Hussain MA, & Schirda B (2015). The role of emotion regulation and cognitive control in the association between mindfulness disposition and stress. Psychology and Aging, 30(1), 160–171. doi: 10.1037/a0038544 [DOI] [PubMed] [Google Scholar]
- Prazak M, Critelli J, Martin L, Miranda V, Purdum M, & Powers C (2012). Mindfulness and its Role in Physical and Psychological Health. Applied Psychology: Health and Well-Being, 4(1), 91–105. doi: 10.1111/j.1758-0854.2011.01063.x [DOI] [PubMed] [Google Scholar]
- Prevention, C. f. D. C. a. (2016). E-cigarette Use Among Youth and Young Adults: A Report of the Surgeon General. Retrieved from Atlanta, GA: [PubMed] [Google Scholar]
- Public health consequences of e-cigarettes. (2018). Retrieved from Washington, DC:
- Rasella D, Aquino R, Santos CA, Paes-Sousa R, & Barreto ML (2013). Effect of a conditional cash transfer programme on childhood mortality: a nationwide analysis of Brazilian municipalities. The lancet, 382(9886), 57–64. doi: 10.1016/S0140-6736(13)60715-1 [DOI] [PubMed] [Google Scholar]
- Rhemtulla M, & Little T (2012). Tools of the Trade: Planned Missing Data Designs for Research in Cognitive Development. Journal of Cognition and Development, 13(4). doi: 10.1080/15248372.2012.717340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggs NR, Black D, Ritt-Olsen A (2015). Associations Between Dispositional Mindfulness and Executive Function in Early Adolescence. Journal of Child and Family Studies, 24, 2745–2751. doi: 10.1007/s10826-014-0077-3 [DOI] [Google Scholar]
- Robinson TN, Banda JA, Hale L, Lu AS, Fleming-Milici F, Calvert SL, & Wartella E (2017). Screen media exposure and obesity in children and adolescents. Pediatrics, 140(Supplement 2), S97–S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemmich JN, Gurgol CM, & Epstein LH (2003). Influence of an interpersonal laboratory stressor on youths’ choice to be physically active. Obesity Research, 11(9), 1080–1087. doi: 10.1038/oby.2003.148 [DOI] [PubMed] [Google Scholar]
- Sakuma KLK, Riggs NR, & Pentz MA (2011). Translating evidence based violence and drug use prevention to obesity prevention: development and construction of the Pathways program. Health education research, 27(2), 343–358. doi: 10.1093/her/cyr095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semenov AD, Zelazo PD. Mindful Family Routines and the Cultivation of Executive Function Skills in Childhood. Human Development. 2019;63(2):112–31. [Google Scholar]
- Shadur JM, Ninnemann AL, Lim A, Lejuez CW, & MacPherson L (2017). The prospective relationship between distress tolerance and cigarette smoking expectancies in adolescence. Psychology of Addictive Behaviors, 31(5), 625–635. doi: 10.1037/adb0000300 [DOI] [PubMed] [Google Scholar]
- Shafer AB (2006). Meta- analysis of the factor structures of four depression questionnaires: Beck, CES‐ D, Hamilton, and Zung. Journal of clinical psychology, 62(1), 123–146. doi: 10.1002/jclp.20213 [DOI] [PubMed] [Google Scholar]
- Simons JS, & Gaher RM (2005). The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion, 29, 83–102. doi: 10.1007/s11031-005-7955-3 [DOI] [Google Scholar]
- Simons-Morton B, Haynie DL, Crump AD, Eitel P, & Saylor KE (2001). Peer and parent influences on smoking and drinking among early adolescents. Health Education & Behavior, 28(1), 95–107. doi: 10.1177/109019810102800109 [DOI] [PubMed] [Google Scholar]
- Sinha R (2008). Chronic stress, drug use, and vulnerability to addiction. Annals of the New York Academy of Sciences, 1141, 105–130. doi: 10.1196/annals.1441.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear LP (2013). Adolescent neurodevelopment. Journal of Adolescent Health, 52(2 Suppl 2), S7–13. doi: 10.1016/j.jadohealth.2012.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spring B, Moller AC, & Coons MJ (2012). Multiple health behaviours: overview and implications. Journal of public health, 34(suppl_1), i3–i10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringhini S, Carmeli C, Jokela M, Avendaño M, Muennig P, Guida F, … & Chadeau-Hyam M (2017). Socioeconomic status and the 25× 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1· 7 million men and women. The Lancet, 389(10075), 1229–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S, & Leventhal A (2014). Substance misuse prevention: addressing anhedonia. New Directions for Youth Development, 2014(141), 45–56, 10.1002/yd.20085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarter RE, Kirisci L, Mezzich A, Cornelius JR, Pajer K, Vanyukov M, … & Clark D (2003). Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. American Journal of Psychiatry, 160(6), 1078–1085. doi: 10.1176/appi.ajp.160.6.1078 [DOI] [PubMed] [Google Scholar]
- Thatcher DL, & Clark DB (2008). Adolescents at risk for substance use disorders: role of psychological dysregulation, endophenotypes, and environmental influences. Alcohol Research & Health, 31(2), 168–176. [PMC free article] [PubMed] [Google Scholar]
- Tomiyama AJ, Dallman MF, & Epel ES (2011). Comfort food is comforting to those most stressed: evidence of the chronic stress response network in high stress women. Psychoneuroendocrinology, 36(10), 1513–1519. doi: 10.1016/j.psyneuen.2011.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toplak ME, West RF, & Stanovich KE (2013). Practitioner review: do performance-based measures and ratings of executive function assess the same construct? Journal of Child Psychology and Psychiatry, 54(2), 131–143. doi: 10.1111/jcpp.12001 [DOI] [PubMed] [Google Scholar]
- Ursache A, Noble KG, & Blair C (2016). Socioeconomic status, subjective social status, and perceived stress: associations with stress physiology and executive functioning. Behavioral Medicine, 41(3), 145–154. doi: 10.1080/08964289.2015.1024604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermunt J (2010). Latent class modeling with covariates: Two improved three-step approaches. . Political Analysis, 18(450–469). doi: 10.1093/pan/mpq025 [DOI] [Google Scholar]
- Young CB, Chen T, Nusslock R, Keller J, Schatzberg AF, & Menon V (2016). Anhedonia and general distress show dissociable ventromedial prefrontal cortex connectivity in major depressive disorder. Translational Psychiatry, 6, e810. doi: 10.1038/tp.2016.80 [DOI] [PMC free article] [PubMed] [Google Scholar]


