Abstract
Background OpenNotes, the sharing of medical notes via a patient portal, has been extensively studied in adults but not in pediatric populations. This has been a contributing factor in the slower adoption of OpenNotes by children's hospitals. The 21st Century Cures Act Final Rule has mandated the sharing of clinical notes electronically to all patients and as health systems prepare to comply, some concerns remain particularly with OpenNotes for pediatric populations.
Objectives After a gradual implementation of OpenNotes at an academic pediatric center, we sought to better understand how pediatric patients and families perceived OpenNotes. This article presents the detailed steps of this informatics-led rollout and patient survey results with a focus on pediatric-specific concerns.
Methods We adapted a previous OpenNotes survey used for adult populations to a pediatric outpatient setting (with parents of children <12 years old). The survey was sent to patients and families via a notification email sent as a standard practice after a clinic visit, in English or Spanish.
Results Approximately 7% of patients/families with access to OpenNotes read the note during the study period, and 159 (20%) of those patients responded to the survey. Of the survey respondents, 141 (89%) of patients and families understood their notes; 126 (80%) found the notes always or usually accurate; 24 (15%) contacted their clinicians after reading a note; and 153 (97%) patients/families felt the same or better about their doctor after reading the note.
Conclusion Although limited by relatively low survey response rate, OpenNotes was well-received by parents of pediatric patients without untoward consequences. The main concerns pediatricians raise about OpenNotes proved to not be issues in the pediatric population. Our results demonstrate clear benefits to adoption of OpenNotes. This provides reassurance that the transition to sharing notes with pediatric patients can be successful and value additive.
Keywords: documentation, communication, safety, quality, patient-centered
Background and Significance
OpenNotes has been a decades long academic research implementation experiment built on a simple premise—it makes it easy for patients and their caregivers to access their own clinical notes. On May 1, 2020, the Office of the National Coordinator for Health Information Technology (ONC) published the 21st Century Cures Act Final Rule, which significantly boosts the OpenNotes movement by requiring that healthcare providers make a minimum dataset (including notes) electronically available to patients. 1 Previous research on OpenNotes implementations provides evidence that sharing notes with patients has the potential to transform clinical care delivery, make care safer, and build stronger more trusting relationships between patients and their clinicians. 2
Most of the research to date on OpenNotes has been performed in primary care adult healthcare settings, and there has been a dearth of data with experiences in pediatric populations. The underlying concept of OpenNotes with pediatric patients is the same; however, there are privacy considerations around maintaining confidentiality between adolescents and their parents when notes are shared. 3 While children's hospitals are working to overcome these hurdles for adolescents, several institutions have shared notes with parents of younger children. There has been limited study of these experiences, and that may be one factor contributing to slower adoption of OpenNotes in pediatric healthcare centers. This article attempts to fill that gap, replicating the original adult OpenNotes survey by Bell et al in a pediatric subspecialty population at a single pediatric academic healthcare institution. 4
Methods
This evaluation was conducted at Stanford Children's Health, which is a pediatric and obstetric healthcare system comprised of Lucile Packard Children's Hospital Stanford (a 361 bed, freestanding, quaternary care, academic pediatric and obstetric hospital) and more than 60 ambulatory clinical sites throughout the Bay Area (approximated 580,000 visits/year). We use the Epic (Epic Systems, Verona, Wisconsin, United States) electronic health record, and notes are shared via the Epic MyChart® patient portal. The portal has a range of features enabled, messaging, results review, appointment scheduling among others available in both English and Spanish. In 2016, the organization activated the functionality to share ambulatory progress notes through the patient portal but required individual clinicians to manually share each note. Individual divisions were invited to turn all of their clinicians notes to share by default, which has been shown to be associated with significantly higher rates of note release. 5 By the end of 2018, most medical and surgical specialties, but not primary care, were sharing notes by default.
Because of challenges around adolescent confidentiality, notes were only shared with patient proxies (parents/guardians) for patients aged between 0 and 11 years and with patients aged 18 years or older, but not with patients aged between 12 and 17 years or their proxies. The patient population analyzed for this manuscript includes patients aged between 0 and 11 years cared for at Stanford Children's Health prior to September 2018 whose guardians had access to OpenNotes through the patient portal. This analysis is based on surveys that were sent to patient proxies during a 5-month time period from April to September 2018. Across the 51,879 patients aged between 0 and 11 years during the study period, 33,128 guardians, covering 31,422 patients (61%), had access to the patient portal. Access to the portal is offered to all patients and their families but does require them to sign up with an email address, which can be a limiting factor for some patients/families. Due to the nature of our staged OpenNotes implementation, only a subset of patients/families (11,297 [36%]) at Stanford Children's Health had access to OpenNotes.
We leveraged the email notification function of the patient portal to send links to surveys using Qualtrics software (Qualtrics, Provo, Utah, United States). As part of our operational and quality improvement efforts at our organization, a general survey was sent to all groups ascertaining perspectives on the patient portal and its effect on care. Patients with access to OpenNotes received additional survey questions based on the original OpenNotes study in adults. 4 The survey included questions with Likert scale responses and open-ended, free text questions. They covered topics including why proxies read the notes, whether they thought the notes were accurate, whether they contacted the provider about the note, and how they felt about the provider as a result of reading the note. 4 The surveys were sent in English or Spanish depending on the preferred language selected in the patient portal.
Results
Of the 11,297 patients/families that had access to their notes, ∼7% ( n = 794) viewed their notes at any point in time during the study period. The demographics of those patients were 42% female and fairly evenly distributed across all age ranges from birth to 11 years with a slightly higher readership in the younger age ranges (0–3 years). Ninety-four percent patients chose English as their language of preference followed by 2% Spanish, 1% Mandarin, with a small number of many other languages ( Fig. 1 ). Combining both the English ( n = 141) and Spanish ( n = 18) surveys together, there was an overall survey response rate of 20% (159/794).
Fig. 1.
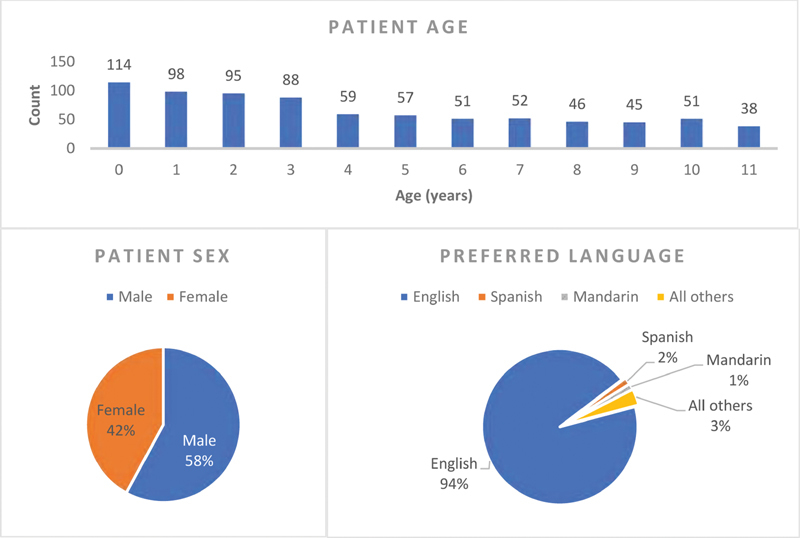
Demographic characteristics of patients ( n = 746) whose proxies viewed their OpenNotes during the study period.
The first question asked was “What are your reasons for reading a visit note (select all that apply)?” The top reasons families chose were wanting to read their child's notes to better know (76%) their child's health and understand (72%) what the doctor said. Additional questions added to the original survey were “Does OpenNotes help you better understand your child's care?” and “Does OpenNotes help you better remember your child's doctor's visit?” 92% and 91% of respondents, respectively, stated that OpenNotes helped improve their understanding and recollection of the visit. Another question asked, “Does OpenNotes help you better understand the other information available in the patient portal such as lab test results?” The vast majority (88%) said “yes” that the notes helped them understand other portal information.
One previously described concern relates to the accuracy of notes; however, when asked the question “How often did the notes accurately describe the visit?,” 80% of respondents described the notes as always or usually accurate. Nine percent of respondents described it as sometimes accurately describing the visit and only 1% of respondents said that the notes never accurately described the visit ( Fig. 2A ). The next question was “How easy was it to understand your child's notes?” 89% of respondents considered the notes to be either “Very Easy” (60%) or “Somewhat Easy” (29%) to understand. Only 1% considered them “Very Difficult” and 4% considered them “Somewhat Difficult” ( Fig. 2B ).
Fig. 2.
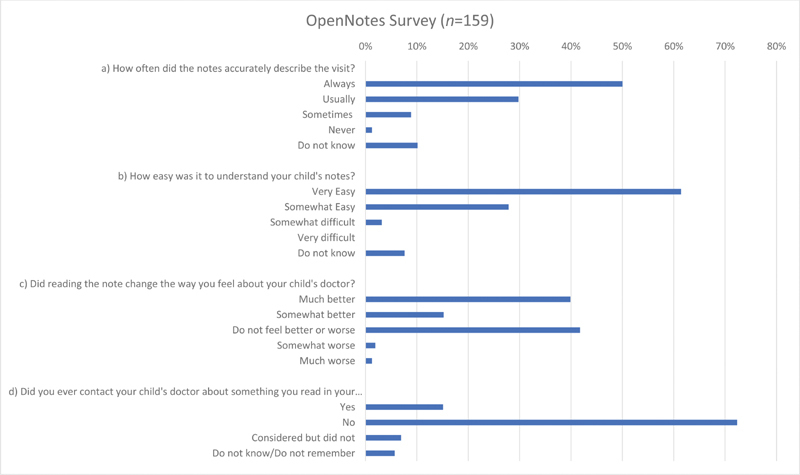
OpenNotes survey results. ( A ) How often did the notes accurately describe the visit? ( B ) How easy was it to understand your child's notes? ( C ) Did reading the note change the way you feel about your child's doctor? ( D ) Did you ever contact your child's doctors' office about something you read in your child's notes?
OpenNotes effect on parent's perception of their child's doctor was generally positive. While 42% of parents did not feel better or worse, 15% felt somewhat better, and 40% felt much better about their child's doctor after reading the notes. Only 2% said they felt somewhat worse and 1% indicated they felt much worse ( Fig. 2C ). The last question dealt with parents' actions after reading the note. The question “Did you ever contact your child's doctors' office about something you read in your child's notes?” showed that the vast majority, 72%, did not. Fifteen percent said they reached out while 7% considered but did not and 6% did not know ( Fig. 2D ).
There was also an opportunity to have free text responses about experiences with OpenNotes, and they largely tracked along similar lines as the above survey questions. “The doctor gave somewhat of a conflicting opinion from my child's previous doctor on the East Coast (we recently relocated). Seeing the Clinic Notes as part of the “After Visit Summary” though MyChart was very helpful to understand why he thought the care plan would be different moving forward.” This comment highlights how having access to the notes can help families better understand medical decision making.
Discussion
This study is one of the first evaluations of the response to OpenNotes in a pediatric population and demonstrated overwhelming positive reception in patients/families who responded to the survey. The majority of patients and families understood their notes; they largely found them accurate; most did not contact their clinicians after reading a note; and the majority found that reading their notes improved trust with their clinician. These results are aligned with previous adult population OpenNotes surveys.
Previous research in adults has shown that clinical notes are helpful for patients for several reasons, such as helping patients remember and understand their visits. This research has also focused on common concerns from clinicians that we have also heard echoed in a range of institutional division meetings. These concerns ranging from patients not understanding notes or that patients would contact clinicians with too many questions have not borne out in research or practice. 6 Our study shows the pediatric experience is similar to that of adults' OpenNotes experience. We did not perform a direct statistical comparison as the number surveyed in our study was significantly lower than that of the adult survey; additionally, there was no follow-up with patients' and families beyond their survey responses and furthermore no clinicians were surveyed.
The top reasons families cited for wanting to read their child's notes were to “better know their child's health” and also “understand what the doctor said.” In the adult OpenNotes survey, these were also the top two reasons for wanting to read a note at 58 and 55%, respectively. 4
One common concern brought up by physicians is that patients may not find the notes accurate. 7 The vast majority found the notes “always” or “usually” accurate and it was only 1% of respondents who said they are never accurate. This trend is similar to the previous adult study where patients found notes “always” (70%) and “usually” (25%) and “never” (<1%) accurate. 4 Notes are meant to be documentation of what was discussed at the visit and there may be occasions where disagreements are documented, and this could represent the 1% where participants said they were not accurate. Nonetheless, most patients described the notes to be accurate.
Another common comment or potential concern of physicians is that patients will not be able to understand the notes as they are written in medical jargon and some clinicians wonder if they have to change how they write. 8 Again, the vast majority of respondents found that notes were “Very easy” or “Somewhat easy” to understand. This result is similar to previous findings where 74% of adults found the notes “very easy” and 23% found them “somewhat easy” to understand.” 4 Several authors have pointed out that patients can understand the notes even with the medical language because it is about them and they have the context in which to interpret the meaning of the note. 9
Some clinicians have been concerned that after reading notes patients would be upset and that this could worsen the doctor patient relationship. 7 In fact, the opposite was true in this study with 40% of respondents stating that they feel “much better” about their child's doctor, and only a very small percent having a negative response. The negative reactions were similar to the adult study in which <1% felt “somewhat worse” and “much worse” after reading notes. 4 However, the improved relationship seen in our study was of a greater magnitude than in the previous adult study where only 20% felt “much better” and 17% felt “somewhat better.” The fact that most participants felt better about their child's doctor after reading notes demonstrates how transparency can help build better relationships.
Finally, a concern that is shared by some clinicians is that patients may call with a large number of questions after reading their notes. 7 This has not been shown to be the case in previous studies 4 and in this survey the vast majority did not contact their child's doctor with a question. A small portion “considered it but did not” and one explanation could be that they waited until a following visit to discuss. Fifteen percent did reach out to their child's doctors that was higher than the 7% seen in the adult study but was still a minority of patients. 4 A possible institutional factor that may have driven this increase could be explained by investment in a general culture of patient engagement efforts driven by our patient-family advisory council. Another potential hypothesis is that the parents in the study live in Silicon Valley and might be more technology and information savvy, leading to more frequent interactions. Anecdotally, through a variety of institutional forums clinicians did not express concerns about receiving increased messages, except some primary care physicians who reported a perceived increase in patient messages to them about specialty care visits. This relationship between note viewership and messaging could be explored in more detail in the future by auditing portal logs. More crucially, previous studies have demonstrated that reaching out may be a sign that a patient or family member uncovered an important safety issue or needed to clarify something important about their care, so this might indicate a sign of increased patient engagement. 10 11
There were several significant limitations in our study. First, the sample size was small with only a 20% response rate in a single institution. Second, readership of OpenNotes was low, which has been a common finding in other OpenNotes studies. 12 Additionally, this study was limited to pediatric subspecialty clinics so further research is needed in pediatric primary care. Finally, because of the complexities of adolescent confidentiality and autonomy, adolescents and their proxies were not included in this study, and further work is necessary to determine the appropriate approach to OpenNotes in this population.
Starting November 2, 2020, we will be expanding our OpenNotes program to include all eight United States Core Data for Interoperability (USCDI) note types (progress, consult, history and physical, discharge summary, imaging narrative, pathology, report, laboratory report, procedure) for all specialties in ambulatory and inpatient. Our next step also includes efforts to separate out sensitive adolescent data protected by California state law in our adolescent notes to prepare for going live with OpenNotes for teens and their proxies. Further research is required into methods to meaningfully and securely communicate appropriate information with teens and their guardians.
Conclusion
This study is the first to replicate an OpenNotes survey used in adult patients with a pediatric population and provides evidence that OpenNotes are as valuable for pediatric patients as they are for adults. Having pediatric population specific results can help advance adoption among Children's hospitals that have been reticent around OpenNotes. Patients' families are able to understand the notes, and the notes can help them better remember the visits. The transparency helped build increased trust of the clinician and did not lead to an increased burden of messages. We hope this research will provide reassurance as organizations implement the ONC Cures Act Final Rule for pediatric patients. Given the complexity of adolescent confidentiality and varying state laws that may supersede the ONC Cures Act Final Rule, further research is needed on the implementation and implications of OpenNotes in the adolescent population.
Clinical Relevance Statement
Notes affect every aspect of clinical care. OpenNotes has started as a voluntary initiative a decade ago and has demonstrated through a body of literature that transparent access to notes for patients improves clinical care in a myriad of ways. Due to additional complexity around adolescent confidentiality and the lack of data for pediatric populations, OpenNotes was not widely adopted in pediatric care settings. Now with the 21st Century Cures Act Final Rule, all healthcare settings will have to effectively participate in OpenNotes. This research provides evidence supporting the benefits of OpenNotes for pediatric patients while also assuaging concerns from clinicians.
Multiple Choice Questions
-
Clinicians commonly voice concern that their patients (or families) won't be able to understand, or will be confused by reading, their clinical notes. When provided access to doctors notes via online patient portals (aka OpenNotes), what percent of patients' report being not being able to understand their own notes?
No patients find clinical notes difficult to understand.
3% of patients find clinical notes difficult to understand.
13% of patients find clinical notes difficult to understand.
63% of patients find clinical notes difficult to understand.
Correct Answer: The correct answer is option b. A study by Walker and Leveille published in 2019 evaluated responses of patients who had read at least one clinical note in the previous year at three large health systems in Boston, Seattle, and rural Pennsylvania. Few patients reported being confused by their notes (737/22,304, 3.3%). 2
-
Another common concern raised by clinicians is that their relationship with their patients will be negatively affected if patients read their notes. What percentage of patients' report feeling worse about their clinician after reading their notes?
Less than 1% of patients feel worse about their clinician after reading their notes.
5% of patients feel worse about their clinician after reading their notes.
15% of patients feel worse about their clinician after reading their notes.
40% of patients feel worse about their clinician after reading their notes.
Correct Answer: The correct answer is option a. In both this study and in Bell et al, 2015 <1% of patients reported feeling worse or much worse after reading their notes. 4
Conflict of Interest None declared.
Protection of Human and Animal Subjects
The survey described in this paper was determined by the Stanford University IRB to be exempt (IRB-45385).
References
- 1.Office of the National Coordinator for Health Information Technology, Department of Health and Human Services 21st Century Cures Act: Interoperability, information blocking, and the ONC health IT certification program Final rule 85 Federal Register 25642–25961 2020. Codified at 45 CFR §170, 45 CFR §171. Available at:https://www.federalregister.gov/documents/2020/05/01/2020-07419/21st-century-cures-act-interoperability-information-blocking-and-the-onc-health-it-certification
- 2.Walker J, Leveille S, Bell S. OpenNotes after 7 years: patient experiences with ongoing access to their clinicians' outpatient visit notes. J Med Internet Res. 2019;21(05):e13876. doi: 10.2196/13876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bourgeois F C, DesRoches C M, Bell S K. Ethical challenges raised by OpenNotes for pediatric and adolescent patients. Pediatrics. 2018;141(06):e20172745. doi: 10.1542/peds.2017-2745. [DOI] [PubMed] [Google Scholar]
- 4.Bell S K, Mejilla R, Anselmo M. When doctors share visit notes with patients: a study of patient and doctor perceptions of documentation errors, safety opportunities and the patient-doctor relationship. BMJ Qual Saf. 2017;26(04):262–270. doi: 10.1136/bmjqs-2015-004697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bialostozky M, Huang J S, Kuelbs C L. Are you in or are you out? Provider note sharing in pediatrics. Appl Clin Inform. 2020;11(01):166–171. doi: 10.1055/s-0040-1701679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mishra V K, Hoyt R E, Wolver S E, Yoshihashi A, Banas C. Qualitative and quantitative analysis of patients' perceptions of the patient portal experience with OpenNotes. Appl Clin Inform. 2019;10(01):10–18. doi: 10.1055/s-0038-1676588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walker J, Leveille S G, Ngo L. Inviting patients to read their doctors' notes: patients and doctors look ahead: patient and physician surveys. Ann Intern Med. 2011;155(12):811–819. doi: 10.7326/0003-4819-155-12-201112200-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klein J W, Jackson S L, Bell S K. Your patient is now reading your note: opportunities, problems, and prospects. Am J Med. 2016;129(10):1018–1021. doi: 10.1016/j.amjmed.2016.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Esch T, Mejilla R, Anselmo M, Podtschaske B, Delbanco T, Walker J. Engaging patients through open notes: an evaluation using mixed methods. BMJ Open. 2016;6(01):e010034. doi: 10.1136/bmjopen-2015-010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bell S K, Gerard M, Fossa A. A patient feedback reporting tool for OpenNotes: implications for patient-clinician safety and quality partnerships. BMJ Qual Saf. 2017;26(04):312–322. doi: 10.1136/bmjqs-2016-006020. [DOI] [PubMed] [Google Scholar]
- 11.Sulieman L, Steitz B, Rosenbloom S T. Analysis of employee patient portal use and electronic health record access at an academic medical center. Appl Clin Inform. 2020;11(03):433–441. doi: 10.1055/s-0040-1713412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Santa J, Wachenheim D, Chin H, Fellows A.Implementing OpenNotes: Improving patient access to notes on patient portals. Published November 2018. Accessed March 5, 2020 at:http://www.opennotes.org/wp-content/uploads/2019/01/Implementing_OpenNotes_Improving_Patient_Access_to_Notes_on_Patient_Portals.pdf


