Abstract
Background
The profession of nurses involves exposure to harmful agents. Despite numerous international studies on the occurrence of sleep disorders in nurses, most studies lacked an assessment of the dependence on the occurrence of the situation causing fear and anxiety which is a highly contagious.
Aim
Determining the relationship between the occurrence of sleep disorders and socio-demographic variables of medical personnel during the COVID-19 epidemic.
Design
This is a cross-sectional study conducted online involving 336 health professionals.
Results
Insomnia among staff was determined at the level of Subthreshold insomnia and Clinical insomnia (moderate severity). Suspicion or confirmed COVID-19 had an effect on the occurrence of sleep disorders in the study group of medical personnel.
Conclusion
Taking into account the statistical error of 6%, the sleep disorders concern about 40% of professionally active nurses and midwives in Poland. Worsening of insomnia was observed in people with the possibility of contact with a patient with COVID-19 in the workplace. Insomnia was more common in respondents over 25 years of age. Psychosocial interventions are needed to help healthcare staff better respond to COVID-19 and future epidemics.
Keywords: COVID-19, Insomnia Severity Index, Nurses, Health care workers
1. Introduction
Insomnia is an element that commonly affects society. Often, insomnia is not recognized and treatment for this condition is not undertaken, which greatly disturbs our functioning in society. Insomnia is classified as a disease that can cause, among others depression and mental disorders. It occurs quite commonly, but nevertheless it is rarely studied and described in general literature (Morin et al., 2011).
It was important to create a tool that would allow to easily assess the severity of insomnia in different groups of people. Insomnia Severity Index Scale (ISI) is such a tool (Morin et al., 2011). According to current literature, it is important to implement such elements at the stage of managing the health care unit that will allow to maintain full physical and mental health in professional groups. Insomnia is associated with many complications. Research conducted by Caruso et al. proved that nurses are particularly vulnerable to cardiovascular, mental and cancer diseases, as well as type 2 diabetes, hormonal disorders and many others. Insomnia can contribute to these conditions (Caruso et al., 2019).
Maintaining psycho-physical well-being in healthcare workers is of great importance when working during the COVID-19 pandemic. One of the elements that affects this element is sleep and its presence in the everyday life of each of us. According to Killgore, et al., there is an increased risk of suicide during a pandemic in vulnerable populations. Health care workers are one of these groups (Killgore et al., 2020). Every day they struggle with patients who are suspected or found of a virus that is currently taking its toll. The essence of our research was to show the level of severity of insomnia in healthcare professionals. Sleep, like many other elements, allows you to function properly every day. Sleep disturbance, if prolonged, can lead to serious complications related to human physiology. One such complication is, among others delirium, which can develop in a short time and can have other serious complications (Krupa and Ozga, 2019). According to research conducted by Killgore, et al., there is statistical evidence that suicidal thoughts are associated with the increase in insomnia (Killgore et al., 2020). It is important to intervene to prevent the spread of insomnia.
No research efforts have been made in Poland to assess the prevalence of sleep disorders among healthcare professionals in the light of COVID-19 pandemics. The aim of the study was to determine the relationship between the occurrence of sleep disorders and socio-demographic variables of medical personnel during the COVID-19 epidemic.
2. Methods
2.1. Sample/setting
This study was designed as a cross-sectional study covering all healthcare professionals in Poland. Due to the epidemic and national bans in force, only remote communication was used. Research conducted electronically, due to the prevailing COVID-19 pandemic from 14 to 21 of April 2020, (7 days). Data began to be collected 30 days after the appearance of the first cases infected with coronavirus, and the Government of the Republic of Poland demanded that Polish citizens stay at home. The survey was disseminated on websites related to health care (Facebook, Twitter, Nursing Organizations Websites; https://ptpaio.pl/), and by providing a prepared online form in the application for sending messages. The study has the approval of the Bioethics Committee (9/05/2020). We informed all participants about the purpose of the study. To ensure confidentiality of participant information, we did not provide any identifying information in the online questionnaire. In order to remain anonymity the IP addresses of the computers used by the participants were not tracked, and the information about their workplace or whether there was any contact with a suspected or COVID-19 positive patient, was coded.
2.2. Instruments
The respondents' sleep quality was measured using the Insomnia Severity Index (ISI) (Morin et al., 2011). The ISI is a short instrument assessing sleep disturbances, The questionnaire covers problems with falling asleep and staying asleep at night as well as effects of these problems in daily functioning. Comprising seven questions, the survey asks respondents to rate their perceptions related to their sleep in the last 14 days. Each item is assessed using Likert scale (0 = no problem; 4 = very severe problem). The total score (0–28 points) helps to characterise the intensity of insomnia. The total ISI score was divided into no clinically significant insomnia (0–7), subthreshold insomnia (8–14), moderately severe clinical insomnia (15–21) and severe clinical insomnia (22–28) (Morin et al., 2011).
2.3. Statistical analysis
All statistical calculations were carried out using the IBM SPSS 23 statistical package and the Excel 2016 spreadsheet. Qualitative type variables were presented using cardinalities and percentages, and the quantitative variable was characterized using an arithmetic mean and standard deviation. The significance of differences between more than two groups was checked by the Kruskal-Wallis test (if significant differences were obtained, Bonferroni's post hoc tests were used, and between the two groups by the Mann-Whitney U test. In all calculations, the significance level was p ≤ 0.05. To determine the sample size, a calculator was used to compute the minimum (required) number of people in the sample (in the study on a sample coming from the population), assuming individual parameters. The confidence level for the result was established, which means how confident we can be in the obtained results, α = 0.95 means that it is 95%. Subsequently, we indicated the fraction size 0.5, the maximum error was 6%. The required number of people in the study was 266. The population size was estimated on the basis of the data from the National Chamber of Nurses and Midwives, and, as of December 31st, 2019, there were 257,833 employed nurses and midwives (NIPiP, 2020).
3. Results
Respondents were asked about sex, age, occupation, place of work. In subsequent questions, respondents were asked to provide information about whether they had contact with COVID-19 patients. The study group consisted of 336 people, of which 88.7% were women and 11.3% were men. Prior to relevant questions, the respondents were asked to provide their age, occupation, workplace and information on possible contact with patients infected with COVID-19. The data are presented in Table 1 .
Table 1.
Characteristics of the study group (N = 336).
| N | % | |
|---|---|---|
| Sex | ||
| Woman | 298 | 88.7 |
| Man | 38 | 11.3 |
| Job | ||
| Nurse | 290 | 86.3 |
| Paramedic | 13 | 3.9 |
| Doctor | 20 | 6.0 |
| Midwife | 4 | 1.2 |
| Other | 9 | 2.7 |
| Age | ||
| 20–25 years old | 58 | 17.3 |
| 26–31 years old | 35 | 10.4 |
| 32–40 years old | 57 | 17.0 |
| 41–50 years old | 113 | 33.6 |
| More than 50 years | 73 | 21.7 |
| Workplace | ||
| Hospital | 220 | 65.7 |
| Ambulatory | 115 | 34.3 |
| Do you have contact with patients with COVID-19? | ||
| Yes | 60 | 17.9 |
| No | 82 | 24.4 |
| Don't know | 194 | 57.7 |
| Have you suspected COVID-19 in any of your patients? | ||
| Yes | 205 | 61.0 |
| No | 91 | 27.1 |
| Don't know | 40 | 11.9 |
| Is there a possibility that a COVID-19 patient will be in your workplace? | ||
| Yes | 306 | 91.1 |
| No | 6 | 1.8 |
| Don't know | 24 | 7.1 |
N = number of responders.
3.1. Insomnia Severity Index (ISI) in study
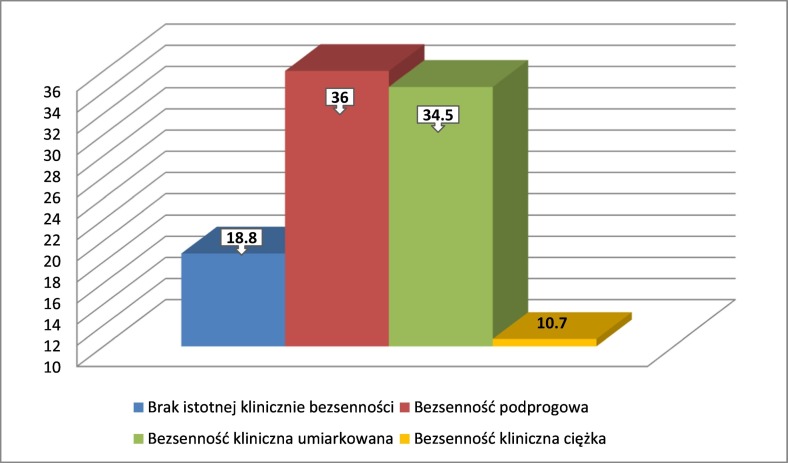
According to the authors of the ISI scale, insomnia should be divided into categories. Respondents were classified according to the guidelines of the authors of the scale (Morin et al., 2011): 0–7 No clinically significant insomnia, 8–14 Subthreshold insomnia, 15–21 Clinical insomnia (moderate severity), 22–28 Clinical insomnia (severe). Descriptive results are presented in Table 2 , and Fig. 1 .
Table 2.
Statistics for the ISI scale in the studied group.
| ISI | N | % |
|---|---|---|
| No clinically significant insomnia | 63 | 18.8 |
| Subthreshold insomnia | 121 | 36.0 |
| Clinical insomnia (moderate severity) | 116 | 34.5 |
| Clinical insomnia (severe) | 36 | 10.7 |
N = responders; ISI=Insomnia Severity Index.
Fig. 1.
Graphic results of the ISI scale in the examined group.
The mean value of the ISI scale was 13.39 (±6.51) and was slightly higher in women than in men - 13.73 (±6.37) and 10.73 (±7.04), respectively. Every third respondent obtained a score no higher than 21 points, and every fifth respondent did not exceed the 10 point threshold, i.e. norm, and therefore did not show insomnia symptoms. Among the respondents, 10.7% obtained at least 22 points, which is defined as clinically severe insomnia.
Categorization of the ISI scale results showed that the problem of insomnia did not affect 18.8% (63 people) of the medical personnel surveyed, when 36.0% of the group (121 people) had a risk and the clinical form of insomnia (moderate and severe) concerned 45% of respondents (152 people).
3.2. Factors affecting the occurrence of insomnia
For women, the risk of insomnia was more often reported than for men - 13.73% (46 women) and 10.73% (36 men), respectively. 18.8% of people received standard results. Analysis showed a relationship between variables. A statistically significantly higher level of insomnia severity was more common in women than men.
Studies have shown a relationship between variables. Statistically, the highest intensity of insomnia was found by nurses, higher than a paramedic, doctor and other profession (H (3) = 13.10; p < 0.05). There were no statistically significant differences p > 0.05 between the remaining groups.
Further analysis by means of multiple comparisons showed that statistically significantly the smallest difficulty in falling asleep had subjects aged 20–25 years, significantly less than the remaining group of subjects (H (4) = 44.49; p < 0.001). There were no statistically significant differences p > 0.05 between the remaining groups.
Analysis showed a relationship between variables. The subjects who worked in the hospital had a statistically significantly higher level of insomnia than those who worked in the clinic. It may also result from the fact that the hospital employees constituted 220 people (65.7%), and the clinic employees 115 people (34.3%).
The analysis by the method of multiple comparisons showed that statistically significantly the greatest intensity of insomnia had subjects who had contact with patients with COVID-19 or knew about it, significantly higher than subjects who did not have contact (H (2) = 17.48; p < 0.001). There were no statistically significant differences p > 0.05 between the remaining groups.
It was demonstrated that statistically significant increase in insomnia was reported by subjects who suspected or did not know COVID-19 in one of their patients, significantly higher than subjects who did not suspect the virus in their patients (H (2) = 11.48; p < 0.05). There were no statistically significant differences p > 0.05 between the remaining groups. The analysis showed that statistically significantly the greatest severity of insomnia was observed in subjects with the possibility of contact with a patient with COVID-19 in the workplace and those who did not know it, significantly greater than subjects in whom there was no possibility of contact with a patient with COVID-19 at the workplace (H (2) = 6.14; p < 0.05). There were no statistically significant differences p > 0.05 between the remaining groups. Information on the possibility of a virus in the respondent's ward significantly affected their severity of insomnia (Table 3).
Table 3.
Correlations between the occurrence of insomnia in the study group.
| Severity of insomnia vs sex | N | M | SD | Z | p |
|---|---|---|---|---|---|
| Female | 298 | 13.73 | 6.37 | 2,47 | 0.013 |
| Male | 38 | 10.73 | 7.04 | ||
| Severity of insomnia vs job | N | M | SD | H | df | p |
|---|---|---|---|---|---|---|
| Nurse | 290 | 13.83 | 6.42 | 13,10 | 3 | 0.004 |
| Paramedic | 13 | 7.38 | 5.86 | |||
| Doctor | 20 | 11.35 | 6.01 | |||
| Midwife | 9 | 11.66 | 6.72 | |||
| Other | ||||||
| Severity of insomnia vs age | N | M | SD | H | df | p |
|---|---|---|---|---|---|---|
| 20–25 years old | 58 | 8.79 | 5.82 | 44.49 | 4 | 0.000 |
| 26–31 years old | 35 | 13.40 | 6.40 | |||
| 32–40 years old | 57 | 13.35 | 6.23 | |||
| 41–50 years old | 113 | 14.27 | 6.25 | |||
| More than 50 years | 73 | 14.73 | 5.99 | |||
| Severity of insomnia vs workplace | N | M | SD | Z | p |
|---|---|---|---|---|---|
| Hospital | 220 | 14.12 | 6.39 | 2.85 | 0.004 |
| Ambulatory | 115 | 12.12 | 6.48 | ||
| Severity of insomnia vs care for patients with COVID-19 | N | M | SD | H | df | p |
|---|---|---|---|---|---|---|
| Yes | 60 | 14.43 | 6.83 | 17.48 | 2 | 0.000 |
| No | 82 | 10.64 | 7.14 | |||
| Don't know | 194 | 14.24 | 5.79 | |||
| Severity of insomnia vs suspected COVID-19 in a patient being cared for | N | M | SD | H | df | p |
|---|---|---|---|---|---|---|
| Yes | 205 | 13.89 | 6.55 | 11.48 | 2 | 0.003 |
| No | 91 | 11.53 | 6.06 | |||
| Don't know | 40 | 15.10 | 6.51 | |||
| Severity of insomnia vs the possibility of providing patient care with COVID 19 at the workplace | N | M | SD | H | df | p |
|---|---|---|---|---|---|---|
| Yes | 306 | 13.41 | 6.48 | 6.14 | 2 | 0.046 |
| No | 6 | 7.33 | 6.91 | |||
| Don't know | 24 | 14.66 | 6.11 |
N = responders; M = average; SD = standard deviation; df = degrees of freedom; H – Kruskal Wallis test; p = significance level.
4. Discussion
In this study, it has been shown that the severity of insomnia among health care workers during the COVID-19 pandemic is present and statistical significance has been demonstrated in each element of the study. Additional correlations have shown that the increase in insomnia is also related to age, gender, occupation and place of work. Nurses have the highest level of insomnia. Similar results were shown in his studies by Albougami and Manzar (2019). Statistical significance demonstrated in the own study on subsequent elements of the scale proves that COVID-19 carries the risk of many complications, including insomnia. In their research, Schmidt and Morin showed slightly lower statistical values in the group of people they tested (Morin et al., 2011; Schmidt et al., 2010). Periods of pandemics and epidemics bring about many serious health problems mainly from an emotional point of view (Brooks et al., 2020; Cénat et al., 2020). Although scientists are currently at the stage of research into sleep disorders during COVID-19, there is little evidence of similar studies during the epidemic that occurred in the past. This proves that both own and cited studies are an important element in creating scientific evidence for subsequent epidemics that are predicted in the next decade. Attention should be paid to a very important element, which are the risk factors for insomnia (Huang & Zhao, 2020; Rossi et al., 2020; Voitsidis et al., 2020). A study of French scientists on a group of the French population showed that health crises involving insomnia are associated with anxiety associated with fear of infection, fear of economic and financial well-being. These elements can have a huge impact on the quality of sleep among the population (Kokou-Kpolou et al., 2020). Our own research showed a relationship between the severity of insomnia at the age of respondents. The relationship between age and insomnia was also described in his research by Patel et al. which indicates that the older a person is, the more he is exposed to the medical and mental effects of insomnia (Patel et al., 2018).
There must be balance in all aspects of human life - its loss leads to disorders, in this case sleep disorders, referred to as insomnia. When analyzing the results of own research and of other authors, attention should be paid to the problem of insomnia in the professional group of nurses. Many elements affect insomnia. Managers of healthcare units should provide adequate psychological and medical care for employees who have direct contact with “positive” patients. The risk of infection is associated with many complications, mainly emotional, among health care professionals. In the same situation there are employees who are afraid that in the future they may come across a patient whose test will show a positive result. The severity of insomnia is a big problem. Insomnia management is not reviewed during apprenticeship studies. Nobody talks about crisis management in medical studies and how to deal with such problems. If in-hospital training is conducted, it is only sporadically. Regular meetings with the psychologist of healthcare professionals can be helpful during subsequent epidemics. Lack of support from decision makers means that during the epidemic the percentage of people on sick leave increases. In addition, many employees need pharmaceutical support because they are otherwise unable to cope with stress caused by fear of the virus. The provision of adequate psychological and even psychiatric care in the workplace is an element that can significantly reduce the level of insomnia.
5. Study limitations
This study has several limitations. First, we only included nurses working in hospitals and clinics. Doctors and other employees accounted for a very small percentage of the respondents. Accordingly, the possibility of generalizing our findings may be limited. As Facebook, Twitter, and Nursing Organizations Websites were used in this study, it is possible that only users with active accounts in the above-mentioned social media could participate in the survey.
6. Conclusion
Taking into account the statistical error of 6%, the sleep disorders concern about 40% of professionally active nurses and midwives in Poland. Worsening of insomnia was observed in people with the possibility of contact with a patient with COVID-19 in the workplace. Insomnia was more common in respondents over 25 years of age. Psychosocial interventions are needed to help healthcare staff better respond to COVID-19 and outbreaks of future pandemics.
Financial disclosure statement
The author has no financial relationships relevant to this article to disclose.
CRediT authorship contribution statement
Term: SK, DO; Conceptualization: DF, WMD; Methodology: WMD, DO; Software: KL, PW; Validation: SK, DO, WMD; Formal analysis: SK, DO; Investigation: SK, DO, PW; Resources: KL, WMD; Data Curation: DO, DF; Writing - Original Draft: SK, DO, DF; Writing - Review & Editing: SK, DO, WMD; Visualization: SK, DF; Supervision: SK; Project administration: SK, DF, DO, PW; Funding acquisition: No one.
Declaration of competing interest
The author has no conflicts of interest relevant to this article to disclose.
References
- Albougami A., Manzar D. Insomnia severity index: A psychometric investigation among Saudi nurses. Sleep & Breathing. 2019;23:987–996. doi: 10.1007/s11325-019-01812-8. [DOI] [PubMed] [Google Scholar]
- Caruso C.C., Baldwin C.M., Berger A., Chasens E.R., Edmonson J.E., Holmes Gobel B.…Tucker S. Policy brief: Nurse fatigue, sleep, and health, and ensuring patient and public safety. Nursing Outlook. 2019;67(5):615–619. doi: 10.1016/j.outlook.2019.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Research. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W.D.S., Cloonen S.A., Taylor E.C., Fernandez F., Grandner M.A., Dailey N.S. Suicidal ideation during the COVID-19 pandemic: The role of insomnia. Psychiatry Research. 2020;27:113–134. doi: 10.1016/j.psychres.2020.113134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokou-Kpolou C.K., Megalakaki O., Laimou D., Kousouri M. Insomnia during COVID-19 pandemic and lockdown: Prevalence, severity, and associated risk factors in France population. Psychiatry Research. 2020;26 doi: 10.1016/j.psychres.2020.113128. 113128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krupa S., Ozga D. Review of the literature on the occurrence of delirium after veno-venous and veno-arterial extracorporeal membrane oxygenation: A systematic review. Dementia and Geriatric Cognitive Disorders Extra. 2019;9(3):374–380. doi: 10.1159/000502685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin C.M., Belleville G., Bélanger L., Ivers H. The insomnia severity index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIPiP (Naczelna Izba Pielęgniarek i Położnych) 2020. https://nipip.pl/liczba-pielegniarek-poloznych-zarejestrowanych-zatrudnionych/ (In Polish)
- Patel D., Steinberg J., Patel P. Insomnia in the elderly: A review. Journal of Clinical Sleep Medicine. 2018;14(6):1017–1024. doi: 10.5664/jcsm.7172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F.…Di Lorenzo G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. An N=18147 web-based survey. medRxiv. 2020 doi: 10.1101/2020.04.09.20057802. 04.09.20057802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt R.E., Richter M., Gendolla G.H., Van der Linden M. Young poor sleepers mobilize extra effort in an easy memory task: Evidence from cardiovascular measures. Journal of Sleep Research. 2010;19(3):487–495. doi: 10.1111/j.1365-2869.2010.00834.x. [DOI] [PubMed] [Google Scholar]
- Voitsidis P., Gliatas I., Bairachtari V., Papadopoulou K., Papageorgiou G., Parlapani E.…Diakogiannis I. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Research. 2020;289:113076. doi: 10.1016/j.psychres.2020.113076. [DOI] [PMC free article] [PubMed] [Google Scholar]