Abstract
Background
The alignment of human lower limb has been an area of ongoing study for decades. The purpose of this study was to analyze the axial and rotational alignment from hip to ankle in a Caucasian aged non-arthritic cohort.
Methods
A non-arthritic cohort of aged patients was retrospectively analyzed by computer tomography. Anatomical–mechanical angle of femur (AMA), femur inclination (FI), femoral anteversion (FA), posterior condylar angle (PCA), proximal tibial torsion (TEAs-PTC and TEAs-PTT) and tibial fibular torsion (PTC-TFA) were measured.
Results
The median age of the patients was 76 years (range 67 to 91 years). Regarding axial alignment, the AMA was 5 (2.94; 6.80). No significance differences were reported by side and age. AMA was significantly lower in men. The FI was 125.3 (120.0; 134.8) with no differences in terms of side, age or gender. Regarding torsion alignment, the median values of FA, PTC-TFA and TEAs-PTT were, respectively, 16.8, 28.5 and − 1.4. No differences were reported by age. Right tibia was externally rotated by 1.5 degrees as compared to the left side (P 0.035).
Conclusion
The broad variability of the parameters analyzed highlights the necessity for a more anatomical and individualized approach during surgery of lower limb. The present study offers the fundament to understand and treat lower limb deformities. Hence, these data can constitute the normal reference values useful to investigate lower limb malalignment. Moreover, it helps to assess the possible changes of axial and rotational alignment in idiopathic OA of lower limb.
Level of evidence III
Retrospective cohort study
Keywords: Lower limb, Alignment, Rotational, Aged non-arthritic cohort
Introduction
The alignment of human lower limb has been an area of ongoing study for decades. However, a clear definition of “normal axial and rotational alignment” in non-arthritic adults has not been established yet. Any femur, patella and tibia axial and rotational malalignment might have a direct effect on the load transmitted through the joint leading to increase cartilage wear and degeneration [1]. Knee surgeons learned from total knee arthroplasty (TKA) procedures that a malposition of implants due to axial and/or rotational malalignment can result in higher revision rates and lower patient-reported outcome scores [2–4]. Likewise, it is conceivable that the axial and rotational alignment of lower limb may be crucial for the biomechanics of native hip knee and ankle. The deleterious effect of axial malalignment (i.e., valgus and varus deformities) of hip, knee and ankle joints is well recognized in the developing of osteoarthritis (OA) [5]. On the other hand, the pathological role of torsion malalignment of lower limb is relatively neglected [6]. Indeed, only few studies reported that a tibia torsion malalignment might be responsible for patellofemoral instability, medial gonarthrosis, patellar chondromalacia and Osgood–Schlatter disease [7–10]. Regarding the question of what constitutes “normal” alignment, there have been detailed studies of apparently healthy populations [11, 12]. Unfortunately, these studies have several limitations. Firstly, they are carried out with the use of plain radiographs considering only deformities in the coronal plane. Secondly, they included a wide age range of population where some patients might be too young to have idiopathic OA. Therefore, the role of rotational alignment in healthy and pathological conditions deserves to be deepened. The purpose of the present study was to analyze the axial and rotational alignment from hip to ankle in a Caucasian aged non-arthritic cohort.
Material and methods
The study protocol was approved by the institutional ethics review board at our institution. A total of 115 full lower extremity computer tomography (CT) studies for oncological diseases workup were performed at our hospital between January 1, 2015, and December 31, 2019. At January 2020, patients’ files and the hospital’s digital database were reviewed retrospectively. A study flowchart is shown in Fig. 1. All scans were obtained using the same instrumentation (Pace General Electric, 4 s scanning time, 512 × 512 reconstruction matrix, 2 mm slice thickness, 125 kV, 460 mAs, with high resolution). All measurements were taken using the same software (Centricity Web V3.0, GE Medical Systems Information Technologies). Each CT examination required 6–9 sections [13]. CT sections were taken: (A) at the center of the femoral head; (B) at the base of the femoral neck; (C) in the midtrochlear region of the femoral condyle, identified by the Roman arch appearance of the intercondylar groove with the apex of the Roman arch corresponding to 1/3 of the height of the condyle [14]; (D) at the proximal tibial epiphyseal (PTE) level, which lies midway between the tibial plateau and the upper end of the proximal tibiofibular joint; (E) at the proximal end of the anterior tibial tuberosity (TT), (F) at the distal tibiofibular joint (TF). From the sections, these straight lines were delineated: a line passing through the center of the femoral head and neck, transepicondylar surgical axes (TEAs), posterior condylar axes (PCAx), a tangent to the most posterior prominent point of the medial and lateral tibial condyles (PTC) in PTE section; a tangent to the posterior surface of the tibia at TT sections (PTT), a line joining the center of both malleoli as described by Rosen et al. [15] (TFA). Three authors (LF, MB and SU) marked the lines on tomograms twice. The interval between those measurements was 4 weeks to avoid a possible memory effect. Once, the lines were established and the authors agreed, the angles were measured. The tomograms thus obtained were analyzed measuring: (1) anatomical–mechanical angle of femur (AMA) (Fig. 2); (2) femoral anteversion (FA) and inclination angles (FI); (3) posterior condylar angle (PCA) [16]; (4) TEAs-PTC angle; (5) TEAs-PTT angle; (6) TEAs-TFA angle; (7) PTC-TFA angle as shown in Fig. 3. A negative value was defined as internal torsion and a positive value as external torsion.
Fig. 1.
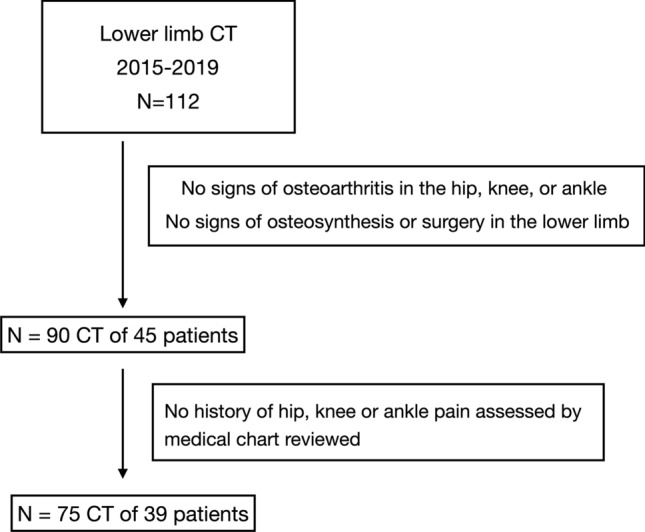
Patient flowchart
Fig. 2.

Axial alignment of lower limb: lines and angles analyzed in the present study. AMA anatomical–mechanical angle, FI femoral inclination
Fig. 3.
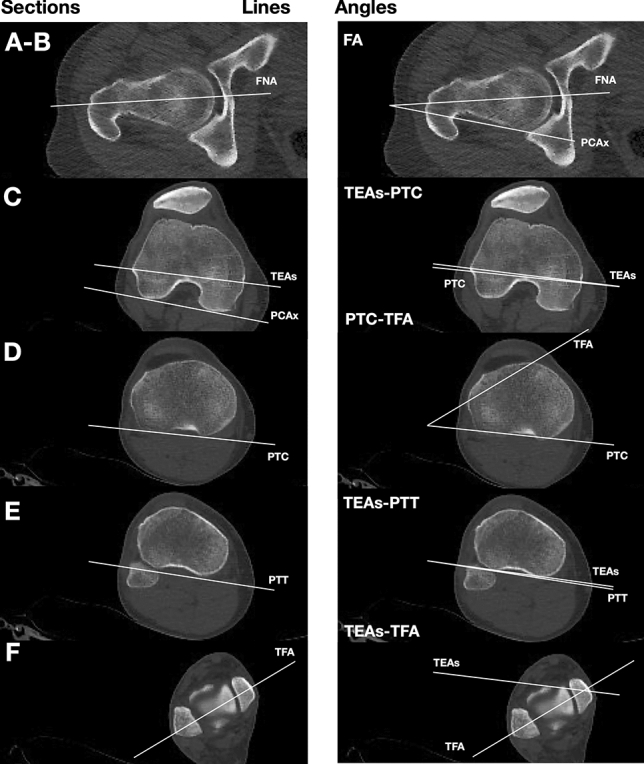
Torsion alignment of the lower limb: lines and angles analyzed in the present study. From the scout view, we find the following CT sections as explained in the text (a–f)
Statistical analysis
We reported the median value, the 2.5th percentile and the 97.5th percentile for each tomograms measure considered. The following characteristics were considered to stratify the analysis: side of the limb, gender of the patient and age. In terms of age, patients were stratified in two classes: age equal or lower than 75 years and age over 75 years. We verified if the variables were normally distributed through Shapiro–Wilk test. We compared the distributions of variables through nonparametric tests because the variables were not normally distributed (except for FA). Specifically, we used Wilcoxon rank-test for paired samples when analyzing the variables between right and left limbs, while a Wilcoxon rank-test for independent sample was implemented to analyze the differences between men and women and age groups in each limb. Finally, we implemented a Friedman test [17] to multiple compare the relationship between the angles and the variables considered, i.e., side of the limb, gender and age group. P values less than 0.05 were interpreted as indicative of statistically significant differences. Statistical analyses were performed with the R statistical program [18].
Results
A review of medical records at our institution identified 115 patients who underwent lower limb CT. At the end, 75 full lower extremity CT studies were included in the study; thirty-nine patients were included in the study, 36 with both limbs, 3 with a single limb. The median age of the patients was 76 years (range 67–91 years), while 19 (49%) patients were women. The summary statistics of the variables for both the limbs and stratified by side of the limb are reported in Table 1. The PTC-TFA angle was significantly higher in the right limb, while the FA was significantly higher in the left limb; no significant differences were observed in the other measures. None of the other measures showed a statistically significant difference between right and left limb. The comparison of tomograms measures by gender in each limb is shown in Table 2. There were no significant differences between males and females’ limbs, except for AMA, FA and PCA angles. The values of FA were significantly higher in female in the right limb, as well as the PCA values; AMA values were significantly higher in female both limbs. In Table 3, we compared the age groups stratifying by limb, and we found no statistically significant differences. Friedman’s test for multiple comparisons highlighted that variables considered affected somehow only the FA value (p. 0.008).
Table 1.
Median and percentiles for each variable considered stratified by side of the limb
| Limb (n = 75) | Right Limb (n = 36a) | Left Limb (n = 36a) | p value | |
|---|---|---|---|---|
| Median (2.5%; 97.5%) | Median (2.5%; 97.5%) | Median (2.5%; 97.5%) | ||
| FA | 16.8 (1.0; 34.2) | 12.3 (− 0.4; 36.0) | 19.5 (1.6; 32.0) | 0.010 |
| PCA | 3 (− 0.2; 6.2) | 3 (− 0.1; 5.3) | 3 (− 0.3; 5.6) | 0.837 |
| TEA-PTC | 1 (− 6.6; 8.2) | 1.8 (− 6.2; 9.1) | 1.3 (− 6.7; 7.3) | 0.661 |
| TEA-PTT | − 1.4 (− 7.9; 4.2) | − 1.2 (− 7.2; 3.3) | − 1.75 (− 7.7; 4.4) | 0.483 |
| TEA-TFA | 30.5 (12.5; 43.5) | 31.4 (18.0; 43.5) | 30.4 (9.2; 43.1) | 0.142 |
| PTC-TFA | 28.5 (12.0; 45.4) | 29.4 (17.5; 44.2) | 27.9 (11.4; 45.3) | 0.035 |
| AMA | 5 (2.9; 6.8) | 5 (3.0; 6.8) | 5 (2.9; 6.4) | 0.606 |
| FI | 125.3 (120.0; 134.8) | 125.1 (119.8; 134.3) | 125.5 (121.5; 134.8) | 0.770 |
The p values refer to the significance of a rank Wilcoxon statistics for dependent sample
FA femoral anteversion, PCA posterior condylar angle, TEA-PTC angle between transepicondylar surgical axis and tangent to the posterior prominent point of the medial and lateral tibial condyles, TEA-PTT angle between transepicondylar surgical axis and tangent to the posterior surface of the tibia at TT sections, TEA-TFA: angle between transepicondylar surgical axis and line joining the center of both malleoli, AMA anatomical–mechanical angle of femur, FI femoral inclination
aSingle limbs were excluded in order to apply a rank test for dependent sample
Table 2.
Median and percentiles for each variable considered stratified by side of the limb and gender of the patient
| Panel A: right limb (n = 38) | |||
|---|---|---|---|
| Male (n = 20) Median (2.5%; 97.5%) |
Female (n = 18) Median (2.5%; 97.5%) |
p value | |
| FA | 10.9 (− 3.0; 25.0) | 22.6 (5.0; 36.6) | 0.003 |
| PCA | 2.8 (− 0.5; 4.5) | 3.3 (1.0; 6.2) | 0.044 |
| TEA-PTC | 0.1 (− 6.7; 9.2) | 2.4 (− 2.2; 7.0) | 0.260 |
| TEA-PTT | − 1.2 (− 4.5; 2.8) | − 1.7 (− 10.9; 3.3) | 0.578 |
| TEA-TFA | 29.6 (19.1; 41.2) | 33.0 (15.0; 43.8) | 0.465 |
| PTC-TFA | 28.6 (17.1; 44.1) | 30.2 (16.3; 43.0) | 0.619 |
| AMA | 4.8 (2.8; 6.6) | 6 (3.9; 6.6) | 0.009 |
| FI | 124.8 (119.0; 132.2) | 125.8 (120.9; 132.9) | 0.265 |
| Panel B: left limb (n = 37) | |||
|---|---|---|---|
| Male (n = 19) Median (2.5%; 97.5%) |
Female (n = 18) Median (2.5%; 97.5%) |
p value | |
| FA | 19 (1.3; 28.1) | 20.5 (9.3; 33.0) | 0.194 |
| PCA | 3 (− 1.5; 5.7) | 3 (0.0; 5.3) | 0.532 |
| TEA-PTC | 1 (− 6.4; 7.6) | 1.46 (− 5.4; 5.7) | 0.483 |
| TEA-PTT | − 1 (− 4.9; 3.1) | − 2.1 (− 10.3; 4.6) | 0.438 |
| TEA-TFA | 30.1 (10.0; 39.7) | 31.0 (12.4; 46.8) | 0.395 |
| PTC-TFA | 26.2 (12.0; 44.0) | 29.2 (12.9; 43.5) | 0.236 |
| AMA | 4.6 (3.1; 6.0) | 5.8 (2.9; 6.6) | 0.012 |
| FI | 125.1 (120.8; 132.6) | 125.7 (122.9; 134.6) | 0.446 |
The p values refer to the significance of a rank Wilcoxon statistics for independent samples
FA femoral anteversion, PCA posterior condylar angle, TEA-PTC angle between transepicondylar surgical axis and tangent to the posterior prominent point of the medial and lateral tibial condyles, TEA-PTT angle between transepicondylar surgical axis and tangent to the posterior surface of the tibia at TT sections, TEA-TFA angle between transepicondylar surgical axis and line joining the center of both malleoli, AMA anatomical–mechanical angle of femur, FI femoral inclination
Table 3.
Median and percentiles for each variable considered stratified by side of the limb and age of the patient
| Panel A: right limb (n = 38) | |||
|---|---|---|---|
| Age ≤ 75 years (n = 18) Median (2.5%; 97.5%) |
Age > 75 years (n = 20) Median (2.5%; 97.5%) |
p value | |
| FA | 12 (4.9; 33.2) | 13.4 (− 4.1; 33.4) | 0.988 |
| PCA | 3 (0.4; 5.6) | 3 (− 0.4; 5.7) | 0.308 |
| TEA-PTC | 0.6 (− 6.8; 7.0) | 1.9 (− 4.1; 9.2) | 0.629 |
| TEA-PTT | − 1.2 (− 3.6; 3.8) | − 1.9 (− 10.5; 2.2) | 0.278 |
| TEA-TFA | 32.9 (16.3; 43.8) | 28.1 (17.1; 40.0) | 0.373 |
| PTC-TFA | 29.6 (16.7; 48.4) | 28.5 (16.6; 41.5) | 0.619 |
| AMA | 5 (3.7; 6.9) | 5 (2.8; 6.3) | 0.596 |
| FI | 125 (120.9; 132.4) | 125.8 (119.0; 132.6) | 0.318 |
| Panel B: left limb (n = 37) | |||
|---|---|---|---|
| Age ≤ 75 years (n = 17) Median (2.5%; 97.5%) |
Age > 75 years (n = 20) Median (2.5%; 97.5%) |
p value | |
| FA | 20 (9.8; 28.0) | 17.3 (1.3; 32.9) | 0.751 |
| PCA | 3 (0.5; 5.7) | 3 (− 1.4; 5.2) | 0.397 |
| TEA-PTC | 2 (− 6.6; 5.8) | 1 (− 4.4; 7.6) | 0.976 |
| TEA-PTT | − 2.5 (− 6.2; 3.1) | − 0.5 (− 9.3; 4.6) | 0.103 |
| TEA-TFA | 31.1 (9.8; 40.4) | 30.2 (14.6; 46.4) | 0.796 |
| PTC-TFA | 28.6 (12.0; 44.6) | 27.2 (11.3; 43.4) | 0.784 |
| AMA | 5 (4.0; 6.2) | 5 (2.5; 6.5) | 0.655 |
| FI | 125 (120.7; 134.5) | 125.8 (123.0; 132.5) | 0.436 |
The p values refer to the significance of a rank Wilcoxon statistics for independent samples
FA femoral anteversion, PCA posterior condylar angle, TEA-PTC angle between transepicondylar surgical axis and tangent to the posterior prominent point of the medial and lateral tibial condyles, TEA-PTT: angle between transepicondylar surgical axis and tangent to the posterior surface of the tibia at TT sections, TEA-TFA angle between transepicondylar surgical axis and line joining the center of both malleoli, AMA anatomical–mechanical angle of femur, FI femoral inclination
Regarding axial alignment, the AMA was 5 (2.9; 6.8). No significance differences were reported by side. AMA was significantly lower in men in both the limbs. The FI was 125.3 (120.0; 134.8) with no statistically significant differences in terms of side age or gender. Regarding torsion alignment, the median values of FA, PTC-TFA and TEAs-PTT were, respectively, 16.8, 28.5 and − 1.4. Differences in terms of side, age and gender are summarized in Tables 2 and 3. A wide variability was observed for all tomogram’s measures in each patients’ group (Fig. 4).
Fig. 4.
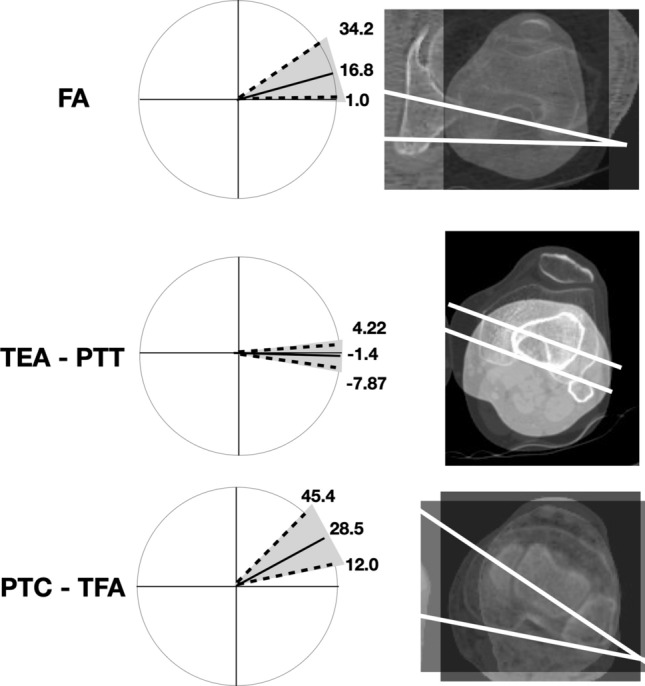
Graphic and CT representation of “normal” lower limb alignment observed in a Caucasian non-arthritic aged 36 subjects (left side). A wide variability was observed for each tomogram. Femoral torsion (FA) is measured as the angle between a line in the femoral neck axis and a line joining the posterior borders of both condyles. Femoral–tibial torsion (TEAs-PTT) is measured as the angle between transepicondylar surgical axes (TEAs) and a tangent to the posterior surface of the tibia at TT sections (PTT). Tibial torsion (PTC-TFA) is measured as the angle between a line joining the posterior borders of the tibial plateaus at the level of the tibial insertion of the posterior cruciate ligament and a line joining the center of the medial and the lateral malleolus. Dotted line: 2.5th and 97.5th percentile for each variable analyzed. Solid line: median of distribution of variable
Discussion
The main contribution of the present study was to describe the torsion alignment of lower limb in an aged non-arthritic cohort. The study was carried out by CT which is considered the most accurate method to measure the lower limb alignment [13]. The anatomical landmarks used have been chosen by consensus of orthopedics and radiologists [19]. In contrast to other studies (Table 4), we selected only aged subjects without OA in order to consider a cohort that presumably will never develop idiopathic OA.
Table 4.
Studies of axial and rotational alignment of lower limb in non-arthritic subjects
| Authors | Year | Subjects (male %) |
Age | Ethnic group |
Method of measure | Statistics | FA | Tibial fibular torsion |
|---|---|---|---|---|---|---|---|---|
| Barahona et al. [13] | 2019 |
32 (56%) |
55 (median) | Caucasian (Chile) | CT | Interquantile (25 to 75) | 9 (5 to 14) | 30 (24 to 34) |
| Mullaji et al. [26] | 2008 |
100 (84%) |
26–40 | Indian | CT | Mean ± SD | N/A | 21.6 ± 7.6 |
| Tamari et al. [23] | 2006 | 25 | > 60 |
Caucasian (Australia) |
Inclinometer | Mean ± SD | 12.7 ± 8.7 | 40.2 ± 8.4 |
| 39 | Japanese | 16.1 ± 12.0 | 39.1 ± 11.1 | |||||
| Lang et al. [25] | 1998 | 7 | 26–73 | Caucasian | CT | Mean ± SD | N/A |
33.14 ± 12.24 L 34.43 ± 8.16 R |
| Strecker et al. [24] | 1997 |
355 (65%) |
16–78 |
Caucasian (Germany) |
CT | Mean ± SD | 23.77 ± 18.27 (right side) | 34.85 ± 15.85° |
| 24.46 ± 16.30 (left side) | ||||||||
| Reikerås et al. [28] | 1989 |
50 (48%) |
16–70 | Caucasian (Norway) | CT | Mean ± SD | N/A |
32.3 ± 8.5 F-R 30.7 ± 10.4 F-L 35.3 ± 7.6 M-R 34.0 ± 10.3 M-L |
| Clements et al. [27] | 1988 |
100 (40%) |
18–61 | Caucasian (Sweden) | Fluoroscope | Mean ± SD | N/A | 30.7 ± 5.2 |
| Jend et al. [29] | 1981 | 70 | > 18 | Caucasian (Germany) | CT | Mean ± SD | N/A | 40 ± 9 |
FA femoral anteversion, CT computer tomography, N/A not applicable, F female, M male, R right, L left, SD standard deviation
It has been well established that coronal malalignment increases the risk of tibiofemoral OA [5]. Varus and valgus alignment shifts the load-bearing axis, respectively, medial and lateral to knee center, creating a moment arm that increases forces across the tibial plateau [1]. The median value of AMA measured in the present study was 5 (2.9; 6.8) that represents the “normal” and physiological alignment of lower limb with a load-bearing axis that runs through center hip, knee and ankle [20]. A possible limit of the present study was that we evaluated an axial non-weight-bearing alignment through CT. However, Paternostre et al. reported a not significance difference between weight and non-weight-bearing alignment in terms of varus and valgus [21].
The median value of FA measured in the present study was 16.8 (1.0; 34.2). By comparing the distributions of the angles among the sides, we found that only FA was significantly lower in the right limb. This difference has been reported also by previous studies [22], and by analogy, we did not find any reasonable explanation for this result. We also found that females presented a significantly higher FA in the right side (p. 0.003). It is interesting to note that “normal” FA here observed was characterized by a wide range of values in agreement with previous studies on healthy patients (Table 4) [13, 23, 24]. Therefore, a FA that differs from the median value might not be an indicator of pathological condition by itself. Further studies are necessary to considering the influence of FA in hip, knee or ankle pathologies.
The median value of tibiofibular torsion (PTC-TFA) measured in the present study was 28.5 degrees, which is in accordance with the values obtained from Caucasian limbs [24, 25] and markedly greater than the values obtained from Indian and Japanese subjects (Table 4) [26]. This difference could be related to genetic or cultural (i.e., gait and postural) differences. Right tibiae showed an increased median of external torsion of 1.5° compared with left tibiae (Table 1, p = 0.035); this agrees with most published data [24, 26–29], even though clinical significance of this right-left difference is not known.
In addition to current knowledge about axial and rotational alignment of human lower limb, in the present study, we analyzed the relationships between TEAs, PTC and PTT in healthy subjects. The median value of angle formed by TEAs and PTT was − 1.4 (− 7.9; 4.2) degree with no differences in terms of side and gender. These results suggest that the posterior tibial surface in correspondence of the proximal extremity of tibial tuberosity was normally slightly internally rotated in this cohort. This angle is original in the literature, and thus, it cannot be compared with measurements of other studies. This study had several limitations. First, inter-observer and intra-observer bias was not determined. However, previous studies reported excellent inter-rater reliability, suggesting that bias was minimal [13]. Although the sample size was underpowered to estimate normal values for the general cohort, there are no studies in the literature that analyze the rotational alignment in aged healthy cohort.
Conclusion
In conclusion, the present study provides a detailed overview about the variability of axial and rotational alignment in Caucasian aged non-osteoarthritic cohort. The broad variability of the parameters analyzed highlights the necessity for a more anatomical and individualized approach during surgery of lower limb. The present study also offers the fundament to understand and treat lower limb deformities. Hence, these data can constitute the normal reference values useful to investigate lower limb malalignment. Moreover, it helps to assess in further studies the possible changes of axial and rotational alignment in idiopathic OA of lower limb.
Funding
Open access funding provided by Universitá Politecnica delle Marche within the CRUI-CARE Agreement.
Compliance with ethical standards
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Clement ND, Deehan DJ. Knee biomechanics: Will we ever know the truth? Bone Jt Res. 2018;7(5):325–326. doi: 10.1302/2046-3758.75.BJR-2017-0360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L. Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res. 2001 doi: 10.1097/00003086-200111000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez MH, Mekhail AO. The failed total knee arthroplasty: evaluation and etiology. J Am Acad Orthop Surg. 2004;12(6):436–446. doi: 10.5435/00124635-200411000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Aglietti P, Sensi L, Cuomo P, Ciardullo A. Rotational position of femoral and tibial components in TKA using the femoral transepicondylar axis. Clin Orthop Relat Res. 2008;466:2751–2755. doi: 10.1007/s11999-008-0452-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma L, Song J, Dunlop D, et al. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis. 2010;69(11):1940–1945. doi: 10.1136/ard.2010.129742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cooke D, Scudamore A, Li J, Wyss U, Bryant T, Costigan P. Axial lower-limb alignment: comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthr Cartil. 1997;5(1):39–47. doi: 10.1016/s1063-4584(97)80030-1. [DOI] [PubMed] [Google Scholar]
- 7.Turner MS, Smillie IS. The effect of tibial torsion on the pathology of the knee. J Bone Jt Surg Ser B. 1981;63(3):396–398. doi: 10.1302/0301-620x.63b3.7263753. [DOI] [PubMed] [Google Scholar]
- 8.Gigante A, Bevilacqua C, Bonetti MG, Greco F. Increased external tibial torsion in Osgood–Schlatter disease. Acta Orthop Scand. 2003;74(4):431–436. doi: 10.1080/00016470310017749. [DOI] [PubMed] [Google Scholar]
- 9.Fairbank JCT, Pynsent PB, Van Poortvliet JA, Phillips H. Mechanical factors in the incidence of knee pain in adolescents and young adults. J Bone Jt Surg Ser B. 1984;66(5):685–692. doi: 10.1302/0301-620x.66b5.6501361. [DOI] [PubMed] [Google Scholar]
- 10.Turner MS. The association between tibial torsion and knee joint pathology. Clin Orthop Relat Res. 1994 doi: 10.1097/00003086-199405000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Hsu RWW, Himeno S, Coventry MB, Chao EYS. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–227. doi: 10.1097/00003086-199006000-00029. [DOI] [PubMed] [Google Scholar]
- 12.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Jt Surg Ser A. 1987;69(5):745–749. doi: 10.2106/00004623-198769050-00016. [DOI] [PubMed] [Google Scholar]
- 13.Barahona M, Guzman M, Barrientos C, et al. A novel approach to lower-limb axial alignment analysis: a CT study. J Am Acad Orthop Surg Glob Res Rev. 2019;3:11. doi: 10.5435/JAAOSGlobal-D-19-00139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eckhoff DG, Johnson KK. Three-dimensional computed tomography reconstruction of tibial torsion. Clin Orthop Relat Res. 1994 doi: 10.1097/00003086-199405000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Rosen H, Sandick H. The measurement of tibiofibular torsion. J Bone Jt Surg Am. 1955;37(4):847–855. doi: 10.2106/00004623-195537040-00014. [DOI] [PubMed] [Google Scholar]
- 16.Griffin FM, Insall JN, Scuderi GR. The posterior condylar angle in osteoarthritic knees. J Arthroplasty. 1998;13(7):812–815. doi: 10.1016/S0883-5403(98)90036-5. [DOI] [PubMed] [Google Scholar]
- 17.Hollander MA, Wolfe D, Chicken E. Nonparametric statistical methods. Hoboken: Wiley; 2015. [Google Scholar]
- 18.R: The R Project for Statistical Computing. https://www.r-project.org/. Accessed May 2, 2020
- 19.Schröter S, Nakayama H, Ihle C, et al. Torsional osteotomy. J Knee Surg. 2019 doi: 10.1055/s-0039-1678677. [DOI] [PubMed] [Google Scholar]
- 20.Paley D. Principles of deformity correction. Berlin Heidelberg: Springer; 2002. [Google Scholar]
- 21.Paternostre F, Schwab PE, Thienpont E. The difference between weight-bearing and non-weight-bearing alignment in patient-specific instrumentation planning. Knee Surg Sport Traumatol Arthrosc. 2014;22(3):674–679. doi: 10.1007/s00167-013-2687-5. [DOI] [PubMed] [Google Scholar]
- 22.Walker JM, Goldsmith CH. Morphometric study of the fetal development of the human hip joint: significance for congenital hip disease. Yale J Biol Med. 1981;54(6):411–437. [PMC free article] [PubMed] [Google Scholar]
- 23.Tamari K, Tinley P, Briffa K, Aoyagi K. Ethnic-, gender-, and age-related differences in femorotibial angle, femoral antetorsion, and tibiofibular torsion: cross-sectional study among healthy Japanese and Australian Caucasians. Clin Anat. 2006;19(1):59–67. doi: 10.1002/ca.20170. [DOI] [PubMed] [Google Scholar]
- 24.Strecker W, Keppler P, Gebhard F, Kinzl L. Length and torsion of the lower limb. J Bone Jt Surg Ser B. 1997;79(6):1019–1023. doi: 10.1302/0301-620X.79B6.7701. [DOI] [PubMed] [Google Scholar]
- 25.Lang LM, Volpe RG. Measurement of tibial torsion. J Am Podiatr Med Assoc. 1998;88(4):160–165. doi: 10.7547/87507315-88-4-160. [DOI] [PubMed] [Google Scholar]
- 26.Mullaji A, Sharma A, Marawar S, Kohli A. Tibial torsion in non-arthritic Indian adults: a computer tomography study of 100 limbs. Indian J Orthop. 2008;42(3):309–313. doi: 10.4103/0019-5413.41854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clementz BG. Tibial torsion measured in normal adults. Acta Orthop. 1988;59(4):441–442. doi: 10.3109/17453678809149399. [DOI] [PubMed] [Google Scholar]
- 28.Reikerås O, Høiseth A. Torsion of the leg determined by computed tomography. Acta Orthop. 1989;60(3):330–333. doi: 10.3109/17453678909149288. [DOI] [PubMed] [Google Scholar]
- 29.Jend HH, Heller M, Dallek M, Schoettle H. Measurement of tibial torsion by computer tomography. Acta Radiol Ser Diagn. 1981;22(3A):271–276. doi: 10.1177/028418518102203A10. [DOI] [PubMed] [Google Scholar]


