Abstract
Introduction
Youth engagement in HIV research is generally recognized as essential, but often neglected or minimally implemented in practice. Engagement is a process of working collaboratively with diverse groups of people to address common issues. We conducted a scoping review of youth HIV prevention interventions in sub‐Saharan Africa to identify and categorize forms and levels of youth engagement across the lifespan of intervention research.
Methods
We followed Arksey and O'Malley's framework for organizing a scoping review. We searched seven databases for related articles on identified intervention studies through May 28th 2020. Included studies focused on youth (10 to 24 years old) HIV prevention interventions in sub‐Saharan Africa. Two reviewers independently examined citations and full manuscripts for inclusion. Data were extracted on study characteristics, location, description of youth engagement and extent of engagement. Youth engagement approaches were categorized based on Hart’s ladder as substantial engagement (strong youth decision‐making power), moderate engagement (shared decision making with adults), minimal engagement (no youth decision‐making power) or no engagement.
Results
We identified 3149 citations and included 112 studies reporting on 74 unique HIV interventions. Twenty‐two interventions were in low‐income countries, 49 in middle‐income countries, and three were in both. Overall, only nine interventions (12%) had substantial or moderate youth engagement, two‐thirds (48, 65%) had minimal youth engagement and 17 interventions (23%) had no youth engagement. We also identified specific engagement strategies (e.g. youth‐led research, crowdsourcing) that were feasible in multiple settings and resulted in substantial engagement.
Conclusions
We found limited youth engagement in youth HIV prevention intervention studies in sub‐Saharan Africa. However, several activities resulted in substantial youth engagement and could be relevant in many low‐and‐middle‐income‐country (LMIC) settings.
Keywords: HIV, youth, engagement, research, Sub‐Saharan Africa
1. INTRODUCTION
Young people (15‐24 years old) in sub‐Saharan Africa accounted for 19% of the estimated 1.7 million new HIV infections globally in 2019, whereas adolescents (10 to 19 years old) in the region made up 8% of total new HIV infections [1, 2]. The number of young people in Africa is estimated to increase by 42% by 2030 [3]. The demographic youth bulge in Africa suggests that HIV prevention will continue to be a critical issue in the coming years. However, similar to other low and middle income countries (LMICs), African nations may have fewer formal and informal mechanisms for stakeholder engagement [4]. We define engagement as a process of working collaboratively with diverse groups of people to address common issues [5, 6].
Youth engagement is essential for effective intervention development. The Joint United Nations Programme on HIV/AIDS (UNAIDS), the United States Agency for International Development (USAID), and other organizations encourage youth engagement in the development of HIV interventions [7, 8]. Youth engagement in HIV interventions increases HIV knowledge, reduces HIV stigma, and facilitates behaviour change [8, 9]. In the context of research, youth engagement can enhance recruitment, create more youth‐friendly interventions and promote dissemination and sustainability [10, 11]. While many studies have examined the effectiveness of youth HIV interventions in sub‐Saharan Africa [8, 12, 13], the extent to which youth are engaged at various stages of intervention research activities (pre‐intervention, intervention and post‐intervention) is rarely explored. Furthermore, the measurement of youth engagement is not standardized. Categorizing levels of youth engagement across study phases will help identify important gaps in the research process, while describing types of engagement approaches that have been used in partnership with youth, providing a resource for HIV prevention research.
The purpose of this study was to categorize and determine the extent of youth engagement in HIV prevention research in sub‐Saharan Africa using a scoping review. We chose a scoping review because of the following reasons: youth engagement strategies were not sufficiently similar to allow pooling; we are not examining the effect of an intervention on an outcome and this prevented assessment of risk of bias; substantial heterogeneity in key operational definitions; identifying research gaps in the existing literature may be well addressed through a scoping review [14].
2. METHODS
2.1. Search strategy
We conducted a scoping review of published literature based on Arksey and O’Malley’s framework for conducting scoping reviews [14]. Scoping reviews examine the extent, range, and nature of research activity for a given topic [14]. On January 15, 2020, we searched five medical research databases (PubMed, Global Health, Scopus, Embase and Cochrane), one clinical trial database (ClinicalTrials.gov), and one non‐peer‐reviewed literature source (Open Gray). Included publications were HIV prevention studies in sub‐Saharan Africa focused on youth (aged 10 to 24 years). The search strategy included variations of the following terms: stakeholder engagement, youth, HIV and low‐and‐middle‐income countries (defined per World Bank guidance) [15]. We exported the records from our search and removed duplicates using Covidence, an online article screening, and data extraction programme.
2.2. Study selection
Inclusion criteria were behavioural and biomedical research studies with human subjects conducted between January 2000 and January 2020, focused primarily (>50%) on youth, related to HIV prevention intervention, and conducted in sub‐Saharan Africa. Studies with stakeholder engagement in the manuscript but without youth engagement were still included. We excluded records that were focused on secondary prevention for youth living with HIV; were cross‐sectional or observational; were systematic or narrative reviews; were secondary data analyses; or were not written in English.
SA and KMT independently reviewed titles and abstracts for inclusion, and KM and DC resolved any discrepancies when needed. Following the title and abstract screening phase, SA and KMT conducted independent full‐text reviews, further excluding studies based on our pre‐established criteria. Data extracted included a description and degree of youth engagement in each study (described below), country, intervention type (behavioural, biomedical or both) and gender of study participants.
The unit of analysis in this review was youth HIV prevention intervention studies. However, descriptions of these interventions were published in more than one journal article. Thus, after identifying the final set of interventions to include using the search strategy described above, we conducted a secondary search for all related articles describing these interventions to ensure that we holistically captured available data on youth engagement. We searched PubMed and ClinicalTrials.gov on 15 January 2020 using search terms gleaned from article abstracts describing our final set of included interventions (e.g. study acronyms, names of study groups, clinical trial registration numbers). From the resulting related articles, we repeated the process of data extraction pertaining to youth engagement activities in our included intervention studies. We updated our search on May 28 2020.
2.3. Categorizing engagement
We used Hart’s ladder to specify the extent of youth engagement [16]. Hart’s ladder is a typology that describes different degrees of youth engagement in projects or programmes. It has eight steps, which progress in a bottom to top fashion, from no engagement to different degrees of engagement. We modified Hart’s ladder by grouping the steps with youth engagement into substantial, moderate, minimal and no youth engagement, based on the decision‐making power of the youth in the research study (Figure 1). Substantial youth engagement was defined as research activities that were youth‐initiated and directed. Adults either created an enabling environment or made relevant contributions, with youth having substantial decision‐making power and opportunities for youth leadership. Moderate youth engagement was defined as adult‐initiated activities with shared decision making between youth and adults. Minimal youth engagement was defined as youth being consulted to get their opinions, assigned specific roles or informed about events surrounding research activities, without any decision‐making power. No youth engagement was defined as the absence of participatory approaches or activities during research. We assumed that meaningful youth engagement would be described in the research study.
Figure 1.
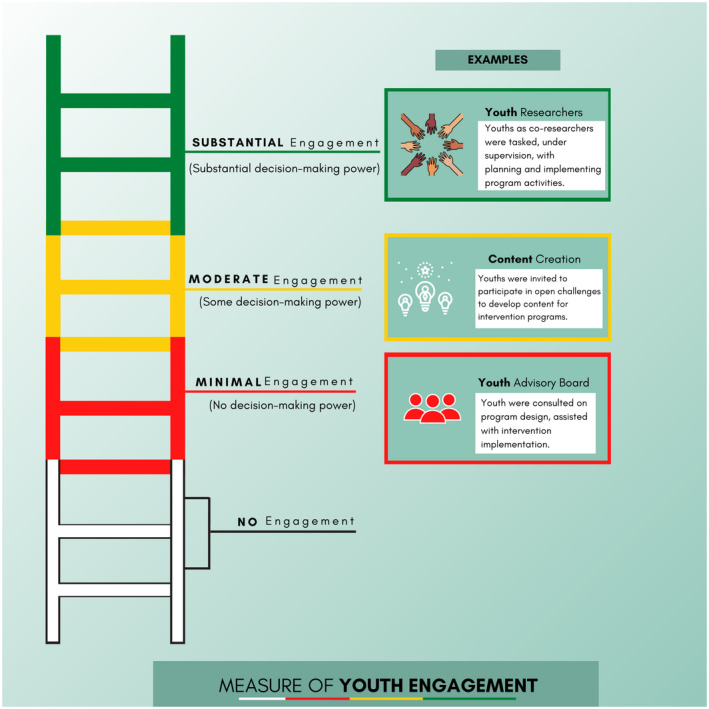
Categorizing youth engagement, adapted from Hart’s ladder [16].
2.4. Data analysis
We used thematic analyses to summarize textual data describing various youth engagement activities employed in identified research studies and were then classified using a conceptual framework based on our modified Hart’s ladder. Two researchers (SA and KMT) independently analysed textual data into the four categories. Engagement activities identified were then categorized and independently coded once for each intervention as per the modified Hart’s ladder described above. We used the University of Witwatersrand Reproductive Health and HIV Institute (Wits RHI) Good Participatory Practice Implementation Model, adapted from the UNAIDS Good Participatory Practice Guidelines to categorize the timing of engagement activities as pre‐intervention, intervention or post‐intervention research phases [7, 17]. Pre‐intervention phase referred to planning and readiness activities, including stakeholder advisory mechanisms, protocol development, ethical approval, field testing and related formative research activities. Intervention phase referred to activities during the actual implementation of the HIV prevention intervention studies. Post‐intervention phase referred to dissemination, results reporting and related activities.
SA and KMT conducted data extraction for all identified studies for the review. To ensure consistency in coding, they first independently extracted and coded ten studies and then assessed their process for intercoder reliability by dialogue. This ensured standardization of extracted data for categorizing the studies and minimized the risk of misclassification. After the two reviewers concluded the process for checking for intercoder reliability the remaining selected studies were then divided evenly between SA and KMT for independent data extraction. Each study was given a score for degree of engagement at each research phase based on the coded engagement activities. An overall assessment was made for each study based on the research phase with the highest score for that study. Given the substantial heterogeneity in key operational definitions of engagement [18], we did not pool findings. We did not require an ethical board review for this scoping review study.
3. RESULTS
Our search strategy yielded 3149 citations and 2684 unique citations. Aside from the citations identified through our database searches, one study was added by hand. After excluding ineligible citations, we examined 146 full‐text manuscripts. Of these, 85 manuscripts met the eligibility criteria and were included (Figure 2). Following our secondary search for studies that described the interventions identified, we found 27 additional manuscripts. Thus, the total number of manuscripts reviewed was 112 [19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103, 104, 105, 106, 107, 108, 109, 110, 111, 112, 113, 114, 115, 116, 117, 118, 119, 120, 121, 122, 123, 124, 125, 126, 127, 128, 129, 130]. These manuscripts described 74 unique intervention research studies (Table 1) [19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 129, 130]. Of the 74 unique intervention studies identified, 72 were solely behavioural interventions and two had both behavioural and biomedical components that included HIV, sexually transmitted infections (STI) and pregnancy screening. Thirty‐five interventions were conducted in southern Africa, 22 in East Africa, 12 in West Africa, two in Central Africa and three were multi‐regional. Twenty‐two intervention studies were in low‐income countries, 49 in middle‐income countries and three in both country income levels. Sixty‐three interventions focused on populations with male and female genders, nine focused only on women and two focused solely on men. Thirty‐seven interventions were conducted before 2010 (Table S1) and 37 interventions were conducted after 2010 (Table S2). Most interventions with youth engagement used multiple engagement approaches at different phases of research (Table 2).
Figure 2.
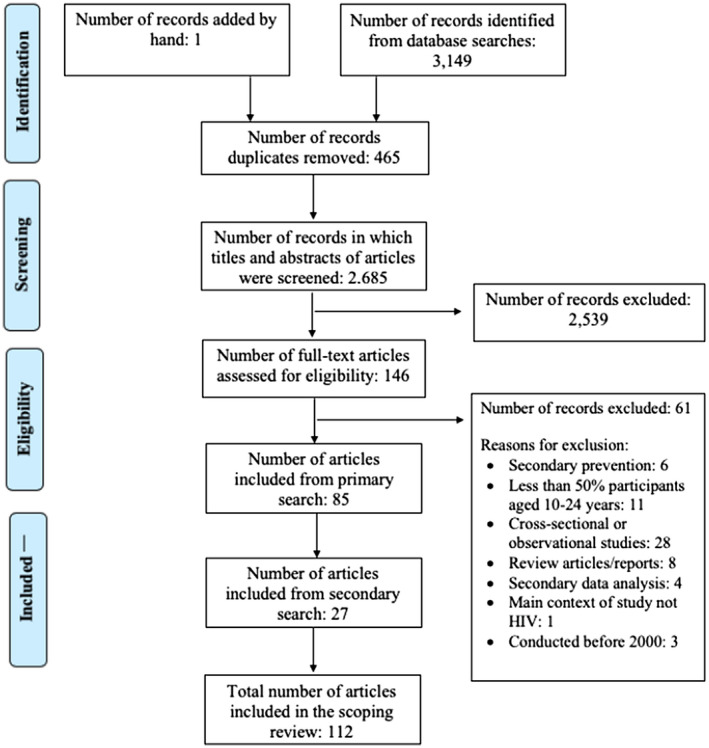
Flow chart of included studies in this scoping review.
Table 1.
Characteristics of youth HIV prevention interventions in sub‐Saharan Africa between 2000 to 2020 (N = 74)
| n | % | |
|---|---|---|
| Region | ||
| Central | 2 | 2.7 |
| East | 22 | 29.7 |
| South | 34 | 45.9 |
| West | 13 | 17.6 |
| Multi‐region | 3 | 4.1 |
| Country income level a | ||
| Low income | 22 | 29.7 |
| Middle income | 49 | 66.2 |
| Both | 3 | 4.1 |
| Gender of participants | ||
| Only women | 9 | 12.2 |
| Only men | 2 | 2.7 |
| All genders | 63 | 85.1 |
| Intervention type b | ||
| Behavioural | 72 | 97.3 |
| Behavioural and biomedical | 2 | 2.7 |
Based on World Bank criteria
there were no solely biomedical interventions.
Table 2.
Examples of youth engagement approaches used at each phase of youth HIV prevention intervention research in sub‐Saharan Africa from 2000 to 2020 (N = 74)
| Pre‐intervention phase | Intervention phase | Post‐intervention phase | |
|---|---|---|---|
| Substantial youth engagement: youth‐initiated activities | Trained youth researchers initiated and planned intervention research | Trained youth researchers implemented intervention research | Trained youth researchers analysed research findings |
| Crowdsourcing a open call | Youth initiated post‐intervention sustainability activities | ||
| Moderate youth engagement: adult‐initiated shared decision making with youth | Translated intervention components to youth‐acceptable language |
Media and content creation Facilitated research activities Developed and delivered drama performances Developed workplans for lectures and community outreaches Led health seminars and key intervention components |
Intervention data dissemination |
| Minimal youth engagement: no decision‐making power |
Youth/Community advisory boards Focus group discussions Qualitative interviews Surveys Photovoice |
Consulted for programme adaptation during on‐going implementation |
Focus group discussions Qualitative interviews Surveys |
Crowdsourcing is the process of having a group solve a problem whose solution has public benefit; this solution is then shared widely with the public [131].
3.1. Overall assessment
Three intervention studies (4%) had substantial engagement in at least one research phase whereby youth initiated and carried out some research activities from start to finish (Figure 3, Video S1 abstract) [19, 20, 21]. Of these three interventions, one had substantial youth engagement in all three phases of research [20]. For this intervention, street‐connected youth peer educators were trained to conduct research. These peer educators or youth researchers initiated, planned, and implemented a series of HIV prevention programme activities within their communities that targeted similar groups of youth, and carried out data analysis of their programme effectiveness [20]. Substantial youth engagement was also identified with engagement approaches that used crowdsourcing of ideas for interventions [21], and youth‐initiated post‐intervention community HIV prevention effort [19]. Crowdsourcing is the process of having a group solve a problem whose solution has public benefit; this solution is then shared widely with the public [131].
Figure 3.
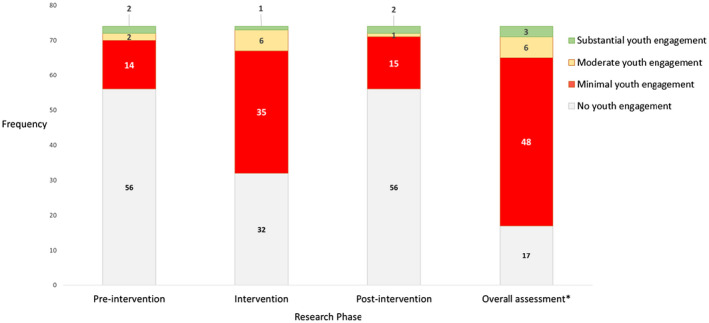
Degree of youth engagement in HIV prevention interventions at different phases of research in sub‐Saharan Africa from 2000 to 2020 (N = 74). Substantial youth engagement: youth‐initiated activities; Moderate youth engagement: shared decision making with adults; Minimal youth engagement: no decision‐making power. *An overall assessment was made for each intervention based on the research phase with the highest level of engagement.
Moderate youth engagement was identified in six interventions (8%) whereby youth, under supervision, were empowered to decide how to deliver intervention components, implying shared decision making with adults (Video S1 abstract) [22, 23, 24, 25, 26, 27]. Most interventions (48, 65%) had minimal engagement, with youth having no decision‐making power [28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 67, 68, 69, 70, 71, 72, 75, 87, 90, 130], and some interventions (17, 23%) had no engagement at any phase of research [66, 88, 89, 129].
We identified two studies which utilized digital and social media‐based interventions or mHealth [21, 90]. Of these two studies, one was categorized as having substantial youth engagement, whereas the other had minimal youth engagement. Both studies were conducted after 2010. We also assessed of the extent of youth engagement over time by comparing engagement in studies conducted in or before 2010 [19, 20, 22, 34, 39, 40, 41, 45, 46, 47, 48, 52, 53, 54, 59, 60, 66, 68, 72, 73, 77, 78, 80, 82, 83, 88, 89, 109, 115, 121, 130], to studies conducted after 2010 [21, 24, 28, 29, 30, 42, 43, 44, 50, 51, 56, 57, 58, 60, 62, 63, 64, 67, 69, 70, 71, 75, 76, 79, 81, 84, 85, 86, 90, 100, 110, 111, 129]. We found youth engagement in 28 out of 37 interventions (76%) conducted in or before 2010, and in 30 out of 37 interventions (81%) conducted after 2010.
3.2. Pre‐intervention phase
We identified two interventions with substantial youth engagement at the pre‐intervention phase of research (Figure 3) [20, 21]. The first was a crowdsourcing open call for ideas on HIV self‐testing delivery methods focused on engaging youth [21]. In the second study, street‐connected youth peer educators initiated and planned a programme of activities within their Non‐Governmental Organization (NGO) including regular HIV prevention clubs, individual counselling and seminars, with support from NGO staff. They also developed post‐intervention survey questionnaires for their research [20].
Two interventions had moderate youth engagement at the pre‐intervention research phase [23, 24]. In the first intervention, youth researchers carried out unstructured observations, facilitated informal discussion groups with community members, and worked with community members to highlight components of the intervention research that were important to their community. In this way, youth helped direct the research objectives [23]. In the second study, street‐connected youth peer educators adapted and translated intervention components into terms that similar youth use and comprehend [24]. The youth also nominated representatives to engage in focus group discussions, and elected representatives who communicated ideas and concerns to the study team regarding the proposed programmes [24].
Fourteen interventions (19%) had minimal youth engagement at the pre‐intervention phase [28, 31, 33, 35, 36, 43, 45, 49, 54, 59, 60, 67, 71, 87]. These interventions used youth advisory boards or committees (3, 4%) [59, 67], photovoice (1, 1%) [28], focus group discussions (10, 14%) [28, 31, 33, 35, 43, 45, 54, 60, 71, 87], qualitative interviews (4, 5%) [36, 43, 60, 87], and surveys (3, 4%) [28, 45, 49], to get youth’s views and opinions, or areas of focus for intervention. In as much as the youth were consulted through these aforementioned mechanisms, it was unclear the extent to which youth opinions shaped final decisions with regards to research components or outcomes.
About three quarters of studies (56, 76%) had no youth engagement at the pre‐intervention phase [19, 22, 29, 30, 32, 44, 46, 47, 48, 50, 51, 52, 53, 55, 56, 57, 58, 61, 62, 63, 64, 65, 66, 68, 69, 70, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 88, 89, 90, 129, 130].
3.3. Intervention phase
The intervention phase had the highest number of interventions with youth engagement (42, 57%) [19, 20, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 39, 42, 43, 44, 45, 46, 47, 49, 51, 52, 53, 56, 57, 58, 59, 61, 63, 64, 65, 67, 68, 69, 70, 71, 72, 75]. There was one intervention study with substantial youth engagement at this phase of research. In the study with street connected youth, substantial engagement continued from the pre‐intervention to the intervention phase. These youth implemented their planned programme of activities that targeted other street‐connected youth in their communities [20].
There were six studies (8%) with moderate youth engagement at the intervention phase [19, 22, 23, 25, 26, 27]. All six studies utilized trained peer educators who were empowered to decide how to deliver intervention components, implying shared decision making with adults on intervention implementation. In one intervention, peer educators developed their workplans for class‐based lectures and community outreaches [22]. In two other interventions, both school‐based, peer educators led key intervention components including seminars and health education activities, informal group discussions, individual counselling, drama, songs and other performances [26, 27]. Another study, which was also school‐based, had peer educators lead student clubs in which members of the clubs created songs, videos, journalistic articles and other types of media that promoted knowledge and dialogue related to HIV, as well as encouraged peers to get tested. The best media content created were selected to be used for a city‐wide post‐intervention HIV campaign [25]. One intervention had drama performances by the peer educators as its main component, with youth playing a major role in directing drama content [19]. In another intervention (described earlier as having moderate youth engagement at pre‐intervention phase), youth researchers guided and facilitated research activities initially agreed upon with community members [23].
All interventions assessed as having minimal youth engagement at the intervention phase (35, 47%) utilized trained peer educators [24, 28, 29, 30, 31, 32, 33, 34, 42, 43, 44, 45, 46, 47, 49, 51, 52, 53, 56, 57, 58, 59, 61, 63, 64, 65, 67, 68, 69, 70, 71, 72, 75]. In all of these interventions, peer educators were assigned to lead discussions or teach their peers about high risk and protective behaviours related to HIV and sexual/reproductive health; the peer educators did not modify the interventions in any way or have any decision‐making power during intervention implementation. Two of these interventions also involved peer educators in drama performances or role plays, although it was not reported that peer educators had any say in the performance content [45, 53].
There were 32 interventions (43%) with no youth engagement approach used at the intervention phase [21, 35, 36, 37, 38, 54, 55, 60, 66, 73, 74, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 129, 130].
3.4. Post‐intervention phase
There were two interventions with substantial youth engagement at the post‐intervention phase [19, 20]. In one study – described earlier as having substantial engagement at pre‐intervention and intervention research phases – street‐connected youth peer educators carried out data analysis to assess the effectiveness of their programme and determined areas for improvement [20]. In the second intervention with substantial engagement at the post‐intervention phase, peer educators initiated and organized post‐intervention community HIV testing and counselling health fairs in conjunction with district health officials, following survey responses from community members who attended their drama performances [19]. This study also had moderate youth engagement at the intervention phase.
One intervention had moderate youth engagement post‐intervention, with shared decision making with adults [23]. In this intervention – also described earlier as having moderate engagement at both pre‐intervention and intervention phases – youth researchers discussed research findings with their community during a one‐day report‐back session [23].
Interventions with minimal youth engagement at the post‐intervention phase (15, 20%) [22, 24, 28, 34, 37, 38, 40, 41, 43, 44, 48, 50, 55, 90, 130] used different engagement approaches to get youth’s opinions and feedback about the intervention and study components such as surveys (4, 5%) [24, 34, 44, 55], focus group discussions (13, 18%) [22, 24, 28, 37, 38, 40, 41, 44, 48, 50, 90, 102, 132], and individual qualitative interviews (3, 4%) [28, 44, 102]. Two studies assigned peer educators to collect data by administering structured questionnaires to study participants post‐intervention [24, 55]. In these interventions with minimal youth engagement, youth had no described decision‐making power to determine post‐intervention phase outcomes.
About three‐quarters of studies (56, 76%) had no youth engagement activity at the post‐intervention phase [21, 25, 26, 27, 29, 30, 31, 32, 33, 35, 36, 39, 42, 45, 46, 47, 49, 51, 52, 53, 54, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 129].
4. DISCUSSION
This scoping review describes the extent of youth engagement in HIV prevention interventions in sub‐Saharan Africa. Most interventions had minimal or no youth engagement. Despite the recognized importance of youth engagement in HIV research [133, 134], prior youth HIV literature reviews have not focused on engagement of youth, but rather on youth as recipients of interventions [12, 135], or on evaluating peer‐led programmes among youth [135, 136]. This scoping review extends the literature by measuring the extent of youth engagement, focusing on engaging sub‐Saharan African youth, and rigorously examining youth engagement in selected interventions.
We found that youth engagement was minimal or absent in many youth HIV prevention studies from sub‐Saharan Africa. This finding is consistent with a broader literature suggesting that youth are often excluded from meaningful engagement in HIV interventions [137, 138]. This finding suggests that while youth frequently participate in the research process, they are not often engaged in activities that share decision‐making power with adults or provide opportunities for youth leadership. This may be related to ethical concerns about the competing demands among youth [139], lack of youth training and capacity building opportunities [137, 140], or adult perceptions about limited youth capacity [141]. It may also be associated with a lack of parental consent; given the stigmatized nature of HIV, parents may have more concerns allowing their youth to engage in HIV prevention research than other less stigmatized health interventions [142]. Additionally, studies may not have the funding or time necessary for robust youth engagement . However, there were some examples of substantial engagement in which youth extensively developed, implemented and analysed interventions. This suggests that there are feasible opportunities for considerable youth engagement at all phases of intervention research.
We identified two creative ways to engage youth in HIV prevention research. One intervention held a crowdsourcing open call for youth to share their ideas on how to promote HIV self‐testing among youth [21]. This intervention engaged a large number of youth with a diverse set of ideas on HIV interventions that are relevant to their needs. This crowdsourcing approach has been used in other LMIC settings [143]. Other interventions identified in this review described youth as co‐researchers who were tasked, under supervision, with planning and implementing programme activities, disseminating research findings or organizing post‐intervention community HIV testing and counselling [19, 20, 23]. Crowdsourcing and youth as co‐researchers are mechanisms that foster youth engagement in the HIV research process. These participatory approaches provide an environment for meaningful youth engagement, which can lead to the development of health services that are appropriately tailored to the needs of youth.
The review had several limitations. First, our search strategy included “engagement” in the terms. As a result, we likely over‐estimated the extent of youth engagement in HIV prevention research in sub‐Saharan Africa. Second, some studies may not have described youth engagement. However, we also did a secondary search to identify additional manuscripts related to the same intervention. In addition, research checklists [144], best practice statements [145, 146], and guidelines [7], underline the importance of reporting youth engagement in HIV research. Third, our review does not capture HIV interventions with youth engagement described in non‐English journals. While a limitation, evidence suggests that excluding non‐English studies does not impact review findings from systematic reviews [147, 148]. Fourth, youth engagement categorization was only done by one reviewer for each intervention. There is a risk for misclassification bias. In order to reduce this bias, the two coders created standardized criteria and compared notes on the same ten studies. Fifth, we did not address efficacy of the analysed studies in our review. This is because the purpose of our review was to not to assess the efficacy of engagement, but to simply describe the extent of youth engagement in HIV studies.
Findings from this review have public health and programmatic implications. There is a disconnect between advocacy for meaningful youth engagement and current youth engagement in practice. HIV interventions can fill this gap by using creative approaches to meaningfully engage youth at all phases of the research process. These creative approaches can include opportunities for youth to create and lead HIV interventions in their communities. From a policy perspective, youth engagement may improve the process of developing new programmes for youth [149]. Policymakers should be informed by the needs of youth, which can best happen when youth are engaged in the HIV research process [149]. Moreover, youth may need more training and support in order to have greater power in decision making related to research studies. It is important that efforts to increase capacity‐building and provide mentorship to youth are considered during the design of studies, when research priorities are being established. Guidance on ethical issues [150] related to appropriate youth engagement may also facilitate this process. Finally, research that demonstrates the value of additional engagement is needed. There is a compelling scientific rationale for youth engagement that could serve as the foundation for further studies.
5. CONCLUSIONS
Our scoping review shines a light on how youth engagement can transform both the process and outputs of HIV research. In terms of process, our co‐authorship team included four youth researchers who each made unique and valuable contributions, underlining the benefit of robust youth inclusion. Our youth co‐authors led the development of the infographic and video, steering the scoping review towards a younger readership. Researchers describing HIV research studies should explicitly consider youth research audiences in order to make research findings relevant to youth. At the same time, strong youth engagement will require researchers to not only trust youth and give them agency, but to provide the mentorship and support necessary to achieve these goals. The studies including digital youth engagement also demonstrate how youth engagement can benefit the outputs of HIV research, developing innovative interventions, services, and approaches. One of the silver linings of COVID‐19 may be to accelerate digital engagement in HIV studies. The expanding opportunity for digital youth engagement merits further research and action.
COMPETING INTEREST
The authors declare that they have no conflict of interest.
AUTHORS’ CONTRIBUTIONS
All authors substantially contributed to project conception, reviewed edited the manuscript, gave final approval of the version to be published and agreed to be accountable for all aspects of this review. SA and KMT: led the scoping review process (project conceptualization, developing and implementing the search strategy, title, abstract and full‐text review, data extraction, writing the manuscript). KM: project conceptualization, developing the search strategy, full‐text review, reviewing and editing the manuscript. DC: project conceptualization, developing the search strategy, title and abstract review, reviewing and editing the manuscript. MAI and KPC: developing the video abstract, reviewing and editing the manuscript. ECN and LPE: developing the infographic (Figure 1), reviewing and editing the manuscript. SD: conducting secondary search of studies, reviewing and editing the manuscript. NER, JJO, SN, WT: project conceptualization, developing the search strategy, reviewing and editing the manuscript. CO, UN, YM, TG, DO, JI, OE: data interpretation, reviewing and editing the manuscript. JDT: project conceptualization, overall guidance and oversight of the scoping review process, reviewing and editing the manuscript.
Supporting information
Table S1. HIV prevention interventions in sub‐Saharan Africa conducted before 2010.
Table S2. HIV prevention interventions in sub‐Saharan Africa conducted after 2010.
Video S1. Video abstract of the scoping review. Link available here: https://drive.google.com/file/d/1Dxxzt89PmHTkV7E‐ihjeZDeh5‐I53tba/view
ACKNOWLEDGEMENTS
We thank the Prevention and Treatment through a Comprehensive Care Continuum for HIV‐affected Adolescents in Resource Constrained Settings (PATC3H) Consortium (NICHD UG3HD096929), the 4 Youth By Youth (4YBY) organization, the Nigerian Institute of Medical Research and the Social Entrepreneurship To Spur Health (SESH).
Asuquo, S. E. , Tahlil, K. M. , Muessig, K. E. , Conserve, D. F. , Igbokwe, M. A. , Chima, K. P. , Nwanunu, E. C. , Elijah, L. P. , Day, S. , Rosenberg, N. E. , Ong, J. J. , Nkengasong, S. , Tang, W. , Obiezu‐Umeh, C. , Nwaozuru, U. , Merino, Y. , Gbaja‐Biamila, T. , Oladele, D. , Iwelunmor, J. , Ezechi, O. and Tucker, J. D. Youth engagement in HIV prevention intervention research in sub‐Saharan Africa: a scoping review. J Int AIDS Soc. 2021; 24(00):e25666
Contributor Information
Sarah E Asuquo, Email: saraheyoasuquo@gmail.com.
Kadija M Tahlil, Email: kadija@live.unc.edu.
Kathryn E Muessig, Email: kate_muessig@med.unc.edu.
Donaldson F Conserve, Email: conserve@mailbox.sc.edu.
Mesoma A Igbokwe, Email: mesocgeorge@gmail.com.
Kelechi P Chima, Email: kelechichima13@gmail.com.
Ezienyi C Nwanunu, Email: ezienyinwanunu@gmail.com.
Lana P Elijah, Email: promiselana2@gmail.com.
Suzanne Day, Email: suzanne.day@med.unc.edu.
Nora E Rosenberg, nrosenbe@email.unc.edu.
Jason J Ong, Email: Jason.ong@lshtm.ac.uk.
Susan Nkengasong, Email: snkengasong@hotmail.com.
Weiming Tang, Email: weiming_tang@med.unc.edu.
Chisom Obiezu‐Umeh, Email: chisom.obiezuumeh@slu.edu.
Ucheoma Nwaozuru, Email: ucheoma.nwaozuru@slu.edu.
Yesenia Merino, ymerino@email.unc.edu.
Titilola Gbaja‐Biamila, Email: titigbajabiamila@yahoo.com.
David Oladele, Email: daveohlay@yahoo.com.
Juliet Iwelunmor, Email: juliet.iwelunmor@slu.edu.
Oliver Ezechi, Email: oezechi@yahoo.co.uk.
Joseph D Tucker, Email: jdtucker@med.unc.edu.
REFERENCES
- 1. Global Statistics . HIV.gov n.d. [cited 2020 July 10]. Available from: https://www.hiv.gov/hiv‐basics/overview/data‐and‐trends/global‐statistics
- 2.AIDSinfo. UNAIDS n.d. [cited 2020 May 19]. Available from: http://aidsinfo.unaids.org/
- 3. United Nations Department of Economic and Social Affairs, Populations Division . Youth population trends and sustainable development. Geneva, Switzerland: United Nations; 2015. [Google Scholar]
- 4. Day S, Blumberg M, Vu T, Zhao Y, Rennie S, Tucker JD. Stakeholder engagement to inform HIV clinical trials: a systematic review of the evidence. J Int AIDS Soc. 2018;21:e25174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. CTSA Consortium . Principles of community engagement. 2nd ed. Bethesda: National Institutes of Health; 2011. [Google Scholar]
- 6. Tindana PO, Singh JA, Tracy CS, Upshur REG, Daar AS, Singer PA, et al. Grand challenges in global health: community engagement in research in developing countries. PLoS Med. 2007;4:e273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. UNAIDS . AIDS Vaccine Advocacy Coalition, editors. Good participatory practice: Guidelines for biomedical HIV prevention trials. 2nd ed. Washington, DC; 2011. [Google Scholar]
- 8. Gaje AJ, Do M, Grant D. Guidelines on best practices for adolescent and youth friendly HIV services. Washington, DC: USAID; 2017. [Google Scholar]
- 9. Sun WH, Miu HYH, Wong CKH, Tucker JD, Wong WCW. Assessing participation and effectiveness of the peer‐led approach in youth sexual health education: systematic review and meta‐analysis in more developed countries. J Sex Res. 2018;55:31–44. [DOI] [PubMed] [Google Scholar]
- 10. Ellen JM, Wallace M, Sawe FK, Fisher K. Community engagement and investment in biomedical HIV prevention research for youth: rationale, challenges, and approaches. J Acquir Immune Defic Syndr. 2010;54(Suppl 1):S7–11. [DOI] [PubMed] [Google Scholar]
- 11. Lo Y‐R, Chu C, Ananworanich J, Excler J‐L, Tucker JD. Stakeholder engagement in HIV cure research: lessons learned from other HIV interventions and the way forward. AIDS Patient Care STDS. 2015;29:389–99. 10.1089/apc.2014.0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Napierala Mavedzenge SM, Doyle AM, Ross DA. HIV prevention in young people in sub‐Saharan Africa: a systematic review. J Adolesc Health. 2011;49:568–86. [DOI] [PubMed] [Google Scholar]
- 13. UNAIDS . Inter‐agency Task Team on Young People, …. Preventing HIV/AIDS in young people: a systematic' ' review of the evidence from developing countries. 2006.
- 14. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. [Google Scholar]
- 15. World Bank Country and Lending Groups . World Bank Data Help Desk n.d. [cited 2020 May 19]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519‐world‐bank‐country‐and‐lending‐groups
- 16. Hart R. Children’s participation: from tokenism to citizenship (vol. 4). Florence, Italy: International Child Development Centre; 1979. [Google Scholar]
- 17. Baron D, Essien T, Pato S, Magongo M, Mbandazayo N, Scorgie F, et al. Collateral benefits: how the practical application of Good Participatory Practice can strengthen HIV research in sub‐Saharan Africa. J Int AIDS Soc. 2018;21:e25175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ahmed SM, Palermo A‐GS. Community engagement in research: frameworks for education and peer review. Am J Public Health. 2010;100:1380–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Carlson M, Brennan RT, Earls F. Enhancing adolescent self‐efficacy and collective efficacy through public engagement around HIV/AIDS competence: a multilevel, cluster randomized‐controlled trial. Soc Sci Med. 2012;75:1078–87. [DOI] [PubMed] [Google Scholar]
- 20. Mitchell K, Nyakake M, Oling J. How effective are street youth peer educators?: lessons learned from an HIV/AIDS prevention programme in urban Uganda. Health Education. 2007;107:364–76. [Google Scholar]
- 21. Iwelunmor J, Ezechi O, Obiezu‐Umeh C, Gbaja‐Biamila T, Nwaozuru U, Oladele D, et al. The 4 youth by youth HIV self‐testing crowdsourcing contest: a qualitative. Evaluation. 2020;15:e0233698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Arnold R, Maticka‐Tyndale E, Tenkorang E, Holland D, Gaspard A, Luginaah I, et al. Evaluation of school‐ and community‐based HIV prevention interventions with junior secondary school students in Edo State, Nigeria. Afr J Reprod Health. 2012;16:103–25. [PubMed] [Google Scholar]
- 23. Chigudu H. Deepening our understanding of community‐based participatory research: lessons from work around reproductive rights in Zimbabwe. Gender Develop. 2007;15:259–70. [Google Scholar]
- 24. Embleton L, Di Ruggiero E, Odep Okal E, Chan AK, Logie CH, Ayuku D, et al. Adapting an evidence‐based gender, livelihoods, and HIV prevention intervention with street‐connected young people in Eldoret, Kenya. Glob Public Health. 2019;14:1703–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Massey PM, Prelip M, Rideau A, Glik DC. School‐based HIV prevention in Dakar, Senegal: findings from a peer‐led program. Int Q Community Health Educ. 2012;33:129–41. [DOI] [PubMed] [Google Scholar]
- 26. Michielsen K, Beauclair R, Delva W, Roelens K, Van Rossem R, Temmerman M. Effectiveness of a peer‐led HIV prevention intervention in secondary schools in Rwanda: results from a non‐randomized controlled trial. BMC Public Health. 2012;12:729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Visser MJ. HIV/AIDS prevention through peer education and support in secondary schools in South Africa. Sahara‐J J Soc Aspects HIV/AIDS. 2007;4:678–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Aarø LE, Mathews C, Kaaya S, Katahoire AR, Onya H, Abraham C, et al. Promoting sexual and reproductive health among adolescents in southern and eastern Africa (PREPARE): project design and conceptual framework. BMC Public Health. 2014;14:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Adam MB. Effectiveness trial of community‐based I Choose Life‐Africa human immunodeficiency virus prevention program in Kenya. Am J Trop Med Hyg. 2014;91:645–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Adeomi AA, Adeoye OA, Asekun‐Olarinmoye EO, Abodunrin OL, Olugbenga‐Bello AI, Sabageh AO. Evaluation of the effectiveness of peer education in improving HIV knowledge, attitude, and sexual behaviours among in‐school adolescents in Osun State, Nigeria. AIDS Res Treat. 2014;2014:131756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Agha S. An evaluation of the effectiveness of a peer sexual health intervention among secondary‐school students in Zambia. AIDS Educ Prev. 2002;14:269–81. [DOI] [PubMed] [Google Scholar]
- 32. Ajibade P. Enhancing sexual and reproductive health information of adolescents as a panacea to curb HIV and AIDS in Nigeria. J Human Ecol. 2015;52:183–191. [Google Scholar]
- 33. Ajuwon AJ, Titiloye MA, Oshiname FO. Effects of peer education on the knowledge and use of HIV counselling and testing services among young persons in Ibadan, Nigeria. Afr J Biomed Res. 2015;18:161–70. [DOI] [PubMed] [Google Scholar]
- 34. Aninanya GA, Debpuur CY, Awine T, Williams JE, Hodgson A, Howard N. Effects of an adolescent sexual and reproductive health intervention on health service usage by young people in northern Ghana: a community‐randomised trial. PLoS One. 2015;10:e0125267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Atwood KA, Kennedy SB, Shamblen S, Tegli J, Garber S, Fahnbulleh PW, et al. Impact of school‐based HIV prevention program in post‐conflict Liberia. AIDS Educ Prev. 2012;24:68–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bogart LM, Skinner D, Thurston IB, Toefy Y, Klein DJ, Hu CH, et al. Let’s Talk!, A South African worksite‐based HIV prevention parenting program. J Adolesc Health. 2013;53:602–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. de Bruin WE, Panday‐Soobrayan S. Learners’ perspectives on the provision of condoms in South African public schools. AIDS Care. 2017;29:1529–32. [DOI] [PubMed] [Google Scholar]
- 38. Burke HM, Packer C, González‐Calvo L, Ridgeway K, Lenzi R, Green AF, et al. A longitudinal qualitative evaluation of an economic and social empowerment intervention to reduce girls’ vulnerability to HIV in rural Mozambique. Eval Program Plann. 2019;77:1–10. [DOI] [PubMed] [Google Scholar]
- 39. Burke HM, Pedersen KF, Williamson NE. An assessment of cost, quality and outcomes for five HIV prevention youth peer education programs in Zambia. Health Educ Res. 2012;27:359–69. [DOI] [PubMed] [Google Scholar]
- 40. Geary CW, Burke HM, Johnson L, Liku J, Castelnau L, Neupane S, et al. Personal involvement of young people in HIV prevention campaign messages: the role of message format, culture, and gender. Health Educ Behav. 2008;35:190–206. [DOI] [PubMed] [Google Scholar]
- 41. Casale MAJ, Flicker S, Nixon SA. Fieldwork challenges: lessons learned from a north‐south public health research partnership. Health Promot Pract. 2011;12:734–43. [DOI] [PubMed] [Google Scholar]
- 42. Chenneville T, Gabbidon K, Drake H, Rodriguez L. Preliminary findings from the HIV SEERs project: a community‐based participatory research program to reduce HIV stigma among youth in Kenya. J Assoc Nurses AIDS Care. 2019;30:462–73. [DOI] [PubMed] [Google Scholar]
- 43. Chiyaka T, Mushati P, Hensen B, Chabata S, Hargreaves JR, Floyd S, et al. Reaching young women who sell sex: methods and results of social mapping to describe and identify young women for DREAMS impact evaluation in Zimbabwe. PLoS One. 2018;13:e0194301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cooper S, Dickinson D. Just jokes! Icebreakers, innuendo, teasing and talking: The role of humour in HIV/AIDS peer education among university students. Afr J AIDS Res. 2013;12:229–238. [DOI] [PubMed] [Google Scholar]
- 45. Cowan FM, Pascoe SJS, Langhaug LF, Dirawo J, Chidiya S, Jaffar S, et al. The Regai Dzive Shiri Project: a cluster randomised controlled trial to determine the effectiveness of a multi‐component community‐based HIV prevention intervention for rural youth in Zimbabwe–study design and baseline results. Trop Med Int Health. 2008;13:1235–44. [DOI] [PubMed] [Google Scholar]
- 46. Daniels U. Improving health, improving lives: impact of the African Youth Alliance and new opportunities for programmes. Afr J Reprod Health. 2007;11:18–27. [PubMed] [Google Scholar]
- 47. Denison JA, Tsui S, Bratt J, Torpey K, Weaver MA, Kabaso M. Do peer educators make a difference? An evaluation of a youth‐led HIV prevention model in Zambian Schools. Health Educ Res. 2012;27:237–47. [DOI] [PubMed] [Google Scholar]
- 48. Dunbar MS, Maternowska MC, Kang M‐SJ, Laver SM, Mudekunye‐Mahaka I, Padian NS. Findings from SHAZ!: a feasibility study of a microcredit and life‐skills HIV prevention intervention to reduce risk among adolescent female orphans in Zimbabwe. J Prev Interv Community. 2010;38:147–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Harrison A, Hoffman S, Mantell JE, Smit JA, ChengShiun L, Exner TM, et al. Gender‐focused HIV and pregnancy prevention for school‐going adolescents: The Mpondombili pilot intervention in KwaZulu‐Natal, South Africa. J HIV/AIDS Soc Serv. 2016;15:29–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hershow RB, Gannett K, Merrill J, Kaufman EB, Barkley C, DeCelles J, et al. Using soccer to build confidence and increase HCT uptake among adolescent girls: a mixed‐methods study of an HIV prevention programme in South Africa. Sport Soc. 2015;18:1009–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hewett PC, Austrian K, Soler‐Hampejsek E, Behrman JR, Bozzani F, Jackson‐Hachonda NA. Cluster randomized evaluation of adolescent girls empowerment programme (AGEP): study protocol. BMC Public Health. 2017;17:386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Isikwenu OO, Omokiti J, Nurudeen D. A holistic approach to reproductive health interventions: talk 2 Me case study. Afr J Reprod Health. 2010;14:147–8. [PubMed] [Google Scholar]
- 53. Jaganath D, Mulenga C, Hoffman RM, Hamilton J, Boneh G. This is My Story: participatory performance for HIV and AIDS education at the University of Malawi. Health Educ Res. 2014;29:554–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Jemmott JB, Jemmott LS, O’Leary A, Ngwane Z, Icard LD, Bellamy SL, et al. School‐based randomized controlled trial of an HIV/STD risk‐reduction intervention for South African adolescents. Arch Pediatr Adolesc Med. 2010;164:923–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Jewkes R, Sikweyiya Y, Nduna M, Shai NJ, Dunkle K. Motivations for, and perceptions and experiences of participating in, a cluster randomised controlled trial of a HIV‐behavioural intervention in rural South Africa. Cult Health Sex. 2012;14:1167–82. [DOI] [PubMed] [Google Scholar]
- 56. Karamagi E, Sensalire S, Nabwire J, Byabagambi J, Awio AO, Aluma G, et al. Quality improvement as a framework for behavior change interventions in HIV‐predisposed communities: a case of adolescent girls and young women in northern Uganda. AIDS Res Ther. 2018;15:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kibel M, Shah P, Ayuku D, Makori D, Kamaara E, Choge E, et al. Acceptability of a pilot intervention of voluntary medical male circumcision and HIV education for street‐connected youth in Western Kenya. J Adolesc Health. 2019;64:43–8. [DOI] [PubMed] [Google Scholar]
- 58. Magala I, Mwesigwa R, Senkirikimbe WS, Nalubega R, Nsubuga M, Nalwanga C, et al. Strategies for scaling up HIV prevention among adolescents: TASO masaka safe male circumcision experience. J AIDS. Clin Res. 2016;7:1000624. [Google Scholar]
- 59. Mwangi M, Mbeki C, Clewett J. A peer education programme for San adolescents in Namibia. Exchange on HIV/AIDS, Sexuality and Gender 2007:14–15.
- 60. Miller KS, Cham HJ, Taylor EM, Berrier FL, Duffy M, Vig J, et al. Formative work and community engagement approaches for implementing an HIV intervention in Botswana schools. Am J Public Health. 2016;106:1439–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Miller AN, Mutungi M, Facchini E, Barasa B, Ondieki W, Warria C. An outcome assessment of an ABC‐based HIV peer education intervention among Kenyan university students. J Health Commun Int Perspect. 2008;13:345–56. [DOI] [PubMed] [Google Scholar]
- 62. Mwale M, Muula AS. The efficacy of peer education in sexual behavioral change among school‐going adolescents in Northern Malawi: a quasi experiment. J HIV/AIDS Soc Serv. 2019;18:229–47. [Google Scholar]
- 63. Nabunya P, Ssewamala FM, Mukasa MN, Byansi W, Nattabi J. Peer mentorship program on HIV/AIDS knowledge, beliefs, and prevention attitudes among orphaned adolescents: an evidence based practice. Vulner Child Youth Studies. 2015;10:345–56. [PMC free article] [PubMed] [Google Scholar]
- 64. Ssewamala FM, Karimli L, Torsten N, Wang JS‐H, Han C‐K, Ilic V, et al. Applying a family‐level economic strengthening intervention to improve education and health‐related outcomes of school‐going AIDS‐orphaned children: lessons from a randomized experiment in Southern Uganda. Prev Sci. 2016;17:134–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Rosenberg NE, Bhushan NL, Vansia D, Phanga T, Maseko B, Nthani T, et al. Comparing youth‐friendly health services to the standard of care through “girl power‐Malawi”: a quasi‐experimental cohort study. JAIDS J Acquir Immune Defic Syndr. 2018;79:458–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. MacPhail C, Adato M, Kahn K, Selin A, Twine R, Khoza S, et al. Acceptability and feasibility of cash transfers for HIV prevention among adolescent South African women. AIDS Behav. 2013;17:2301–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. St Lawrence JS, Seloilwe E, Magowe M, Dithole K, Kgosikwena B, Kokoro E, et al. Cross‐cultural adaptation of an adolescent HIV prevention program: social validation of social contexts and behavior among Botswana adolescents. AIDS Educ Prev. 2013;25:269–86. [DOI] [PubMed] [Google Scholar]
- 68. Swartz S, Deutsch C, Makoae M, Michel B, Harding JH, Garzouzie G, et al. Measuring change in vulnerable adolescents: findings from a peer education evaluation in South Africa. Sahara‐J J Soc Aspects HIV/AIDS. 2012;9:242–54. [DOI] [PubMed] [Google Scholar]
- 69. Timol F, Vawda MY, Bhana A, Moolman B, Makoae M, Swartz S. Addressing adolescents’ risk and protective factors related to risky behaviours: findings from a school‐based peer‐education evaluation in the Western Cape. Sahara‐J J Soc Aspects HIV/AIDS. 2016;13:197–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Menna T, Ali A, Worku A. Effects of peer education intervention on HIV/AIDS related sexual behaviors of secondary school students in Addis Ababa, Ethiopia: a quasi‐experimental study. Reprod Health. 2015;12:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Wechsberg WM, Browne FA, Carney T, Myers B, Minnis A, MacDonald R, et al. The Young Women’s Health CoOp in Cape Town, South Africa: Study protocol for a cluster‐randomised trial for adolescent women at risk for HIV. BMC Public Health. 2018;18:859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Wyss S, Ablordeppey J, Okrah J, Kyei A. Reaching disenfranchised youth and mobile populations in Ghana through voluntary counselling and testing services for HIV. Afr J AIDS Res. 2007;6:121–8. [DOI] [PubMed] [Google Scholar]
- 73. Ajewole IC, Osagbemi GK. Effects of health education intervention on knowledge, attitude and practice of youths concerning HIV/AIDS in rural Nigerian community. Afr J Clin Exp Microbiol. 2007;8:89–93. [Google Scholar]
- 74. Akpabio II, Asuzu MC, Fajemilehin BR, Ofi B. Effects of parental involvement in HIV/AIDS preventive education on secondary student knowledge about transmission and prevention in Akwa Ibom State, Nigeria. Int Q Community Health Educ. 2008;29:71–87. [DOI] [PubMed] [Google Scholar]
- 75. Buhari ASM, Kamaldeen AS, Abdulraheem IS. Impact of peer education training on knowledge of HIV/AIDS among in‐school youth in north central Nigeria. Int J Pharm Res Bio‐Sci. 2012;1:159–67. [Google Scholar]
- 76. Erulkar A, Ferede A, Girma W, Ambelu W. Evaluation of “Biruh Tesfa” (Bright Future) program for vulnerable girls in Ethiopia. Vulner Child Youth Stud. 2013;8:182–192. [Google Scholar]
- 77. Bekele A, Ali A. Effectiveness of IEC interventions in reducing HIV/AIDS related stigma among high school adolescents in Hawassa, Southern Ethiopia. Ethiopian J Health Develop. 2008;22:232–42. [Google Scholar]
- 78. Bell CC, Bhana A, Petersen I, McKay MM, Gibbons R, Bannon W, et al. Building protective factors to offset sexually risky behaviors among black youths: a randomized control trial. J Natl Med Assoc. 2008;100:936–944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Cho H, Hallfors DD, Mbai II, Itindi J, Milimo BW, Halpern CT, et al. Keeping adolescent orphans in school to prevent human immunodeficiency virus infection: evidence from a randomized controlled trial in Kenya. J Adolesc Health. 2011;48:523–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Hallfors DD, Cho H, Mbai I, Milimo B, Itindi J. Process and outcome evaluation of a community intervention for orphan adolescents in western Kenya. J Community Health. 2012;37:1101–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Dancy BL, Jere DL, Kachingwe SI, Kaponda CPN, Norr JL, Norr KF. HIV risk reduction intervention for rural adolescents in Malawi. J HIV AIDS Soc Serv. 2014;13:271–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Djeddah C, Mavanga R, Hendrickx L.Junior farmer field and life schools: experience from Mozambique. AIDS, poverty, and hunger: challenges and responses Highlights of the International Conference on HIV/AIDS and Food and Nutrition Security, Durban, South Africa, 14–16 April, 2005 2006.
- 83. Duflo E, Dupas P, Ginn T, Barasa GM, Baraza M, Pouliquen V, et al. HIV prevention among youth: a randomized controlled trial of Voluntary Cand Testing for HIV and male condom distribution in rural Kenya. PLoS One. 2019;14:e0219535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Frohlich JA, Mkhize N, Dellar RC, Mahlase G, Montague CT, Karim QA. Meeting the sexual and reproductive health needs of high‐school students in South Africa: experiences from rural KwaZulu‐Natal. S Afr Med J. 2014;104:687–90. [DOI] [PubMed] [Google Scholar]
- 85. Hector J, Davies M‐A, Dekker‐Boersema J, Aly MM, Abdalad CCA, Langa EBR, et al. Acceptability and performance of a directly assisted oral HIV self‐testing intervention in adolescents in rural Mozambique. PLoS One. 2018;13:e0195391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Indravudh PP, Fielding K, Kumwenda MK, Nzawa R, Chilongosi R, Desmond N, et al. Community‐led delivery of HIV self‐testing to improve HIV testing, ART initiation and broader social outcomes in rural Malawi: study protocol for a cluster‐randomised trial. BMC Infect Dis. 2019;19:814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Camlin CS, Koss CA, Getahun M, Owino L, Itiakorit H, Akatukwasa C, et al. Understanding demand for prep and early experiences of prep use among young adults in rural Kenya and Uganda: a qualitative study. AIDS Behav. 2020;24(7):2149–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Rotheram‐Borus MJ, Lightfoot M, Kasirye R, Desmond K. Vocational training with HIV prevention for Ugandan youth. AIDS Behav. 2012;16:1133–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Duveskog M, Sutinen E, Vesisenaho M, Gasso C.HIV/AIDS education in Tanzania blended with a programming course. International Conference on Information Technology: Research and Education, 2003. Proceedings. ITRE2003, IEEE; 2003, p. 179–183.
- 90. Haruna H, Hu X, Chu SKW, Mellecker RR, Gabriel G, Ndekao PS. Improving Sexual health education programs for adolescent students through game‐based learning and gamification. Int J Environ Res Public Health. 2018;15:2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Embleton L, Di Ruggiero E, Logie CH, Ayuku D, Braitstein P. Piloting an evidence‐based intervention for HIV prevention among street youth in Eldoret, Kenya. Int J Public Health. 2020;65(4):433–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Cho H, Deming ME, Park J‐H, Iritani B. Gender differences in HIV/HSV‐2: evidence from a school support randomized controlled trial among orphaned adolescents in Kenya. AIDS Behav. 2019;23:2396–406. [DOI] [PubMed] [Google Scholar]
- 93. Mathews C, Eggers SM, de Vries PJ, Mason‐Jones AJ, Townsend L, Aarø LE, et al. Reaching the hard to reach: longitudinal investigation of adolescents’ attendance at an after‐school sexual and reproductive health programme in Western Cape, South Africa. BMC Public Health. 2015;15:608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Mathews C, Eggers SM, Townsend L, Aarø LE, de Vries PJ, Mason‐Jones AJ, et al. Effects of PREPARE, a Multi‐component, School‐Based HIV and Intimate Partner Violence (IPV) Prevention Programme on Adolescent Sexual Risk Behaviour and IPV: Cluster Randomised Controlled Trial. AIDS Behav. 2016;20:1821–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Mmbaga EJ, Kajula L, Aarø LE, Kilonzo M, Wubs AG, Eggers SM, et al. Effect of the PREPARE intervention on sexual initiation and condom use among adolescents aged 12–14: a cluster randomised controlled trial in Dar es Salaam, Tanzania. BMC Public Health. 2017;17:322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Agha S, Van Rossem R. Impact of a school‐based peer sexual health intervention on normative beliefs, risk perceptions, and sexual behavior of Zambian adolescents. J Adolesc Health. 2004;34:441–52. [DOI] [PubMed] [Google Scholar]
- 97. Atwood KA, Kennedy SB, Shamblen S, Taylor CH, Quaqua M, Bee EM, et al. Reducing sexual risk taking behaviors among adolescents who engage in transactional sex in post‐conflict Liberia. Vulner Child Youth Stud. 2012;7:55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Geary CW, Burke HM, Castelnau L, Neupane S, Sall YB, Wong E, et al. MTV’s “Staying Alive” global campaign promoted interpersonal communication about HIV and positive beliefs about HIV prevention. AIDS Educ Prev. 2007;19:51–67. [DOI] [PubMed] [Google Scholar]
- 99. Lenzi R, Packer C, Ridgeway K, Moon TD, Green AF, González‐Calvo L, et al. Exploring intersections of localised gender norms and unanticipated effects of a sexual and reproductive health intervention: implications of respect and being a “good girl” in Zambézia Province, Mozambique. Cult Health Sex. 2019;21:575–90. [DOI] [PubMed] [Google Scholar]
- 100. Burke HM, Field S, González‐Calvo L, Eichleay MA, Moon TD. Quasi‐experimental evaluation using confirmatory procedures: A case study of an economic and social empowerment intervention to reduce girls’ vulnerability to HIV in rural Mozambique. Eval Program Plann. 2019;77:101721. [DOI] [PubMed] [Google Scholar]
- 101. Chenneville T, Gabbidon K, Drake H. The HIV SEERs project: a qualitative analysis of program facilitators’ experience. J Int Assoc Provid AIDS Care. 2019;18:2325958218822308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Chimbindi N, Birdthistle I, Shahmanesh M, Osindo J, Mushati P, Ondeng’e K, et al. Translating DREAMS into practice: early lessons from implementation in six settings. PLoS One. 2018;13:e0208243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Cowan FM, Pascoe SJS, Langhaug LF, Mavhu W, Chidiya S, Jaffar S, et al. The Regai Dzive Shiri project: results of a randomized trial of an HIV prevention intervention for youth. AIDS. 2010;24:2541–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Cowan FM, Langhaug LF, Mashungupa GP, Nyamurera T, Hargrove J, Jaffar S, et al. School based HIV prevention in Zimbabwe: feasibility and acceptability of evaluation trials using biological outcomes. AIDS. 2002;16:1673–8. [DOI] [PubMed] [Google Scholar]
- 105. Dunbar MS, Kang Dufour M‐S, Lambdin B, Mudekunye‐Mahaka I, Nhamo D, Padian NS. The SHAZ! project: results from a pilot randomized trial of a structural intervention to prevent HIV among adolescent women in Zimbabwe. PLoS One. 2014;9:e113621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Merrill KG, Merrill JC, Hershow RB, Barkley C, Rakosa B, DeCelles J, et al. Linking at‐risk South African girls to sexual violence and reproductive health services: A mixed‐methods assessment of a soccer‐based HIV prevention program and pilot SMS campaign. Eval Program Plann. 2018;70:12–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Austrian K, Soler‐Hampejsek E, Behrman JR, Digitale J, Jackson Hachonda N, Bweupe M, et al. The impact of the Adolescent Girls Empowerment Program (AGEP) on short and long term social, economic, education and fertility outcomes: a cluster randomized controlled trial in Zambia. BMC Public Health. 2020;20:349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Jewkes R, Wood K, Duvvury N. I woke up after I joined Stepping Stones“: meanings of an HIV behavioural intervention in rural South African young people”s lives. Health Educ Res. 2010;25:1074–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Jewkes R, Nduna M, Levin J, Jama N, Dunkle K, Khuzwayo N, et al. A cluster randomized‐controlled trial to determine the effectiveness of Stepping Stones in preventing HIV infections and promoting safer sexual behaviour amongst youth in the rural Eastern Cape, South Africa: trial design, methods and baseline findings. Trop Med Int Health. 2006;11:3–16. [DOI] [PubMed] [Google Scholar]
- 110. Rosenberg NE, Gichane MW, Vansia D, Phanga T, Bhushan NL, Bekker L‐G, et al. Assessing the impact of a small‐group behavioral intervention on sexual behaviors among adolescent girls and young women in Lilongwe Malawi: A quasi‐experimental cohort study. AIDS Behav. 2020;24:1542–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Kadede K, Ruel T, Kabami J, Ssemmondo E, Sang N, Kwarisiima D, et al. Increased adolescent HIV testing with a hybrid mobile strategy in Uganda and Kenya. AIDS. 2016;30:2121–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Wechsberg WM, Zule WA, Ndirangu J, Kline TL, Rodman NF, Doherty IA, et al. The biobehavioral Women’s Health CoOp in Pretoria, South Africa: study protocol for a cluster‐randomized design. BMC Public Health. 2014;14:1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Wechsberg WM, Bonner CP, Zule WA, van der Horst C, Ndirangu J, Browne FA, et al. Addressing the nexus of risk: Biobehavioral outcomes from a cluster randomized trial of the Women’s Health CoOp Plus in Pretoria, South Africa. Drug Alcohol Depend. 2019;195:16–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Wechsberg WM, Ndirangu JW, Speizer IS, Zule WA, Gumula W, Peasant C, et al. An implementation science protocol of the Women’s Health CoOp in healthcare settings in Cape Town, South Africa: A stepped‐wedge design. BMC Womens Health. 2017;17:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Akpabio II, Asuzu MC, Fajemilehin BR, Ofi AB. Effects of school health nursing education interventions on HIV/AIDS‐related attitudes of students in Akwa Ibom State, Nigeria. J Adolesc Health. 2009;44:118–123. [DOI] [PubMed] [Google Scholar]
- 116. Abu‐Saeed MB, Abu‐Saeed K. Attitudinal changes using peer education training in the prevention of HIV/AIDS: a case study of youths in north central Nigeria. Adv Pharm Bull. 2013;3:45–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Hallfors DD, Cho H, Hartman S, Mbai I, Ouma CA, Halpern CT. Process evaluation of a clinical trial to test school support as HIV prevention among orphaned adolescents in western kenya. Prev Sci. 2017;18:955–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Carney T, Browne FA, Myers B, Kline TL, Howard B, Wechsberg WM. Adolescent female school dropouts who use drugs and engage in risky sex: effects of a brief pilot intervention in Cape Town, South Africa. AIDS Care. 2019;31:77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Chapman J, do Nascimento N, Mandal M. Role of male sex partners in HIV risk of adolescent girls and young women in Mozambique. Global Health: Science and Practice. 2019;7(3):435–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Dlamini SN, Maticka‐Tyndale E, Omorodion F, Anucha U, Lowik AJ. HP4RY Team. What does a decolonizing/decentralizing methodology in examining sexual lives entail? Afr. J Reprod Health. 2012;16:55–70. [PubMed] [Google Scholar]
- 121. Harrison A, Smit J, Hoffman S, Nzama T, Leu C‐S, Mantell J, et al. Gender, peer and partner influences on adolescent HIV risk in rural South Africa. Sex Health. 2012;9:178–86. 10.1071/SH10150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Kamo N, Carlson M, Brennan RT, Earls F. Young citizens as health agents: use of drama in promoting community efficacy for HIV/AIDS. Am J Public Health. 2008;98:201–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Karim AM, Williams T, Patykewich L, Ali D, Colvin CE, Posner J, et al. The impact of the African Youth Alliance program on the sexual behavior of young people in Uganda. Stud Fam Plann. 2009;40:289–306. [DOI] [PubMed] [Google Scholar]
- 124. Onokerhoraye AG. HIV prevention for rural youth in Nigeria: background overview. WHARC; 2012. [PubMed]
- 125. Kilburn KN, Pettifor A, Edwards JK, Selin A, Twine R, MacPhail C, et al. Conditional cash transfers and the reduction in partner violence for young women: an investigation of causal pathways using evidence from a randomized experiment in South Africa (HPTN 068). J Int AIDS Soc. 2018;21:e25043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Pettifor A, MacPhail C, Hughes JP, Selin A, Wang J, Gómez‐Olivé FX, et al. The effect of a conditional cash transfer on HIV incidence in young women in rural South Africa (HPTN 068): a phase 3, randomised controlled trial. Lancet Glob Health. 2016;4:e978–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Jennings L, Ssewamala FM, Nabunya P. Effect of savings‐led economic empowerment on HIV preventive practices among orphaned adolescents in rural Uganda: results from the Suubi‐Maka randomized experiment. AIDS Care. 2016;28:273–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Mantell JE, Harrison A, Hoffman S, Smit JA, Stein ZA, Exner TM. The Mpondombili Project: preventing HIV/AIDS and unintended pregnancy among rural South African school‐going adolescents. Reprod Health Matters. 2006;14:113–22. [DOI] [PubMed] [Google Scholar]
- 129. Bekolo CE, Yimdjo Fogue TD, Williams TD. Feasibility of integrating HIV testing into local youth development p rogrammes in Cameroon. Pan Afr Med J. 2018;29:189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Boungou Bazika JC. Effectiveness of small scale income generating activities in reducing risk of HIV in youth in the Republic of Congo. AIDS Care. 2007;19 Suppl 1:S23–4. [DOI] [PubMed] [Google Scholar]
- 131. Han L, Chen A, Wei S, Ong JJ, Iwelunmor J, Tucker JD, et al. Crowdsourcing in health and health research: a practical guide. Geneva, Switzerland: World Health Organization; 2018. https://www.who.int/tdr/publications/year/2018/crowdsourcing‐practical‐guide/en/. [Google Scholar]
- 132. Bazika JCB. Effectiveness of small scale income generating activities in reducing risk of HIV in youth in the Republic of Congo. AIDS Care. 2007;19:S23–4. [DOI] [PubMed] [Google Scholar]
- 133. Child Survival Working Group . Meaningful engagement of adolescents and young people in national and local HIV programming. Geneva, Switzerland: WHO; 2018. [Google Scholar]
- 134. Oliveras C, Cluver L, Bernays S, Armstrong A. Nothing about us without RIGHTS‐meaningful engagement of children and youth: from research prioritization to clinical trials, implementation science, and policy. J Acquir Immune Defic Syndr. 2018;78 Suppl 1:S27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Michielsen K, Chersich MF, Luchters S, De Koker P, Van Rossem R, Temmerman M. Effectiveness of HIV prevention for youth in sub‐Saharan Africa: systematic review and meta‐analysis of randomized and nonrandomized trials. AIDS. 2010;24:1193–202. [DOI] [PubMed] [Google Scholar]
- 136. Simoni JM, Nelson KM, Franks JC, Yard SS, Lehavot K. Are peer interventions for HIV efficacious? A systematic review. AIDS Behav. 2011;15:1589–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Reed SJ, Miller RL. The benefits of youth engagement in HIV‐preventive structural change interventions. Youth Soc. 2014;46:529–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Pettifor A, Stoner M, Pike C, Bekker L‐G. Adolescent lives matter: preventing HIV in adolescents. Curr Opin HIV AIDS. 2018;13:265–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Mbunda T, Tarimo EAM, Chalamilla G, Bakari M, Sandström E, Kulane A. The influence of community members on participation by youth in an HIV vaccine trial in Tanzania. PLoS One. 2016;11:e0168660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Melles MO, Ricker CL. Youth participation in HIV and sexual and reproductive health decision‐making, policies, programmes: perspectives from the field. Int J Adolesc Youth. 2017;23:1–9. [Google Scholar]
- 141. Checkoway BN, Gutierrez LM. Youth participation and community change. J Community Pract. 2006;14:1–9. [Google Scholar]
- 142. DiClemente RJ, Ruiz MS, Sales JM. Barriers to adolescents’ participation in HIV biomedical prevention research. J Acquir Immune Defic Syndr. 2010;54 Suppl 1:S12–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Beres LK, Winskell K, Neri EM, Mbakwem B, Obyerodhyambo O. Making sense of HIV testing: social representations in young Africans’ HIV‐related narratives from six countries. Glob Public Health. 2013;8:890–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Res Involv Engagem. 2017;3:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. MacQueen KM, Harlan SV, Hannah S, Slevin KW, Bass E, Moffett J. Stakeholder Engagement Toolkit. 2012.
- 146. PolicyLink . Addressing disparities for healthier places. PolicyLink; n.d. [Google Scholar]
- 147. Jüni P, Holenstein F, Sterne J, Bartlett C, Egger M. Direction and impact of language bias in meta‐analyses of controlled trials: empirical study. Int J Epidemiol. 2002;31:115–23. [DOI] [PubMed] [Google Scholar]
- 148. Nussbaumer‐Streit B, Klerings I, Dobrescu AI, Persad E, Stevens A, Garritty C, et al. Excluding non‐English publications from evidence‐syntheses did not change conclusions: a meta‐epidemiological study. J Clin Epidemiol. 2020;118:42–54. [DOI] [PubMed] [Google Scholar]
- 149. World Health Organization . Global Accelerated Action for theHealth of Adolescents (AA‐HA!) Guidance to Support Country Implementation – Summary. Geneva: World Health Organization; 2017. [Google Scholar]
- 150. Day S, Kapogiannis B, Shah S, Wilson E, Ruel T, Conserve D, et al. Adolescent HIV research ethics in resource‐constrained settings: low and middle‐income country research consortium experience and scoping review. Lancet HIV. 2020;7(12):e844–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. HIV prevention interventions in sub‐Saharan Africa conducted before 2010.
Table S2. HIV prevention interventions in sub‐Saharan Africa conducted after 2010.
Video S1. Video abstract of the scoping review. Link available here: https://drive.google.com/file/d/1Dxxzt89PmHTkV7E‐ihjeZDeh5‐I53tba/view


