Abstract
Objectives:
Experiences of racial discrimination are common for Black Americans and have been associated with depression and sleep disturbance, factors likely involved in the insidious development of health disparities. The current study replicates these associations and examines longitudinal linkages.
Methods:
Black American couples (Men: N=248, Mage=40, SD=9; Women: N=277, Mage=37, SD=7) and their children, aged 9 to 14 (N=276, Mage=11, SD=1), completed measures of experiences of racial discrimination, depressive symptoms, and sleep problems at baseline and 8-month follow-up. In separate analyses for men, women, and youth, we examined concurrent and prospective associations of racial discrimination with depressive symptoms and sleep problems, then used longitudinal indirect effect models to examine whether depressive symptoms in response to racial discrimination led to increased sleep problems, or vice versa.
Results:
Racial discrimination was associated concurrently with depressive symptoms and sleep problems for all family members. Prospective associations were also found with depressive symptoms and sleep problems in fathers and youth, and sleep problems in mothers. Longitudinal models showed significant indirect effects of racial discrimination on change in sleep problems through depressive symptoms for fathers and mothers, and a similar, but non-significant, pattern in youth. There were no indirect effects on change in depressive symptoms through sleep problems.
Conclusions:
Persistent associations of racial discrimination with depressive symptoms and sleep problems reflect a lasting impact of racial discrimination. Because discrimination’s effects on depression may contribute to increased sleep problems over time, interventions that buffer the effects of discrimination on depressive symptoms may also reduce sleep problems.
Keywords: discrimination, depressive symptoms, sleep problems, Blacks
Experiences of racial discrimination are common for Black Americans and, along with institutional, cultural and structural racism (Neblett, 2019), contribute to racial health disparities (Carter et al., 2019; Pascoe & Smart Richman, 2009; Williams, 2012). Understanding processes connecting racial discrimination to health is important for informing therapy, policy, and public health interventions. Sleep problems and depressive symptoms are two proximal indicators of reactions to stress (Fiksdal et al., 2019; Goosby, Straley, & Cheadle, 2017), and consistent with a biopsychosocial model (Clark, Anderson, Clark, & Williams, 1999), may play important roles in transforming stressful experiences to poorer health and wellbeing (Hisler & Brenner, 2019). Sleep problems and depressive symptoms are highly comorbid (Riemann, Berger, & Voderholzer, 2001), and both have been associated with experiences of racial discrimination in Black Americans (Mossakowski, 2003; Noh & Kaspar, 2003; Simons et al., 2002; Slopen, Lewis, & Williams, 2016; Wong, Eccles, & Sameroff, 2003). However, much of the extant research is cross-sectional, with limited research on Black men and children/adolescents. To better understand physical and psychological responses to racial discrimination, more longitudinal studies of these associations as well as studies including Black men and youth are needed (Lewis et al., 2013; Steffen & Bowden, 2006; Yip et al., 2019). The current study therefore first examines cross-sectional and prospective associations of perceived experiences of racial discrimination with depressive symptoms and sleep problems in Black men, women, and youth, and then tests longitudinal pathways leading from experiences of racial discrimination to changes in depressive symptoms and sleep problems.
Racial Discrimination: A Substantial Psychosocial Stressor for Black Americans
Black Americans frequently experience multiple chronic contextual stressors, resulting from both institutionalized racism (e.g., lower socioeconomic status [SES], housing and food insecurity, neighborhood disadvantage; Hardeman, Murphy, Karbeah, & Kozhimannil, 2018) and interpersonal racism (i.e., perceived everyday experiences of discrimination; Landrine & Klonoff, 1996; Seaton, Caldwell, Sellers, & Jackson, 2008). Structural racism and internalized schemas linked to repeated social messages about race can reinforce experiences of interpersonal racism, resulting in messages of exclusion, disempowerment, and devaluation (Priest et al., 2018) and potentiating biological consequences as well as consequences for sleep (Hicken, Lee, Ailshire, Burgard, & Williams, 2013; Lewis et al., 2013).
In the current investigation we test the proposition that perceived experiences of racial discrimination will be linked to depression and sleep disturbance concurrently and over time. The sample is drawn from rural counties in the Southeastern US where poverty rates are elevated, unemployment rates are above the national average (Carl Vinson Institute of Government, 2003; Probst et al., 2002), and entrenched oppressive social structures lead to frequent experiences of discrimination (Cutrona, Clavél, & Johnson, 2016; Tickamyer & Duncan, 1990; Williams, Neighbors, & Jackson, 2003). Together, these factors create a context in which experiences of discrimination are likely to convey threat and intimidation. We focus on perceived experiences of racial discrimination because these have been tied to multiple negative mental and physical health outcomes in Black adults (Carter et al., 2019; Carter, Lau, Johnson, & Kirkinis, 2017; Pascoe & Smart Richman, 2009) and children (Goosby, Malone, Richardson, Cheadle, & Williams, 2015; Greene, Way, & Pahl, 2006). Although other stressors such as low SES and neighborhood disadvantage are also associated with poorer mental and physical health outcomes (Pickett, 2001; Williams & Jackson, 2005), racial disparities in health are pronounced even among affluent individuals (Colen, Ramey, Cooksey, & Williams, 2018), implying an independent, pervasive role of interpersonal racism in influencing health outcomes (Geronimus, 1992; Geronimus, Hicken, Keene, & Bound, 2006).
The vast majority of Black adults experience racial discrimination; one study found that 98% of Black adults reported experiencing at least one incidence of racial discrimination in the past year (Landrine & Klonoff, 1996). These experiences are commonplace among Black children as well, especially as they enter adolescence, when they experience racial discrimination from both peers and adults (Greene et al., 2006; Priest et al., 2018). These experiences impact Black children’s psychological (Brody et al., 2006; Greene et al., 2006) and physical (Goosby et al., 2015) health, and their academic achievement (Wong et al., 2003). Longitudinal analyses are therefore necessary to address the ways it may exert its influence.
Pathways from Racial Discrimination to Depressive Symptoms and Sleep Problems
The biopsychosocial model of racism proposed by Clark, Anderson, Clark, and Williams (1999) provides a framework to conceptualize the multifaceted impact of racism as a stressor for Black Americans. This framework suggests that the perception of an environmental stimulus as racial discrimination triggers psychological and physiological stress responses (Clark et al., 1999). Perception of racial discrimination as a chronic stressor elicits a state of vigilance associated with chronic activation of stress response systems (i.e., “fight or flight”; Goosby et al., 2017). When combined with the use of more passive, maladaptive coping responses (e.g., rumination), this can affect the development of depressive symptoms by posing transient threats to self-esteem and contributing to a sense of helplessness (Kim, 2014; Madubata, Odafe, Talavera, Hong, & Walker, 2018). Consistent with this idea, experiences of racial discrimination have been robustly associated with depressive symptoms (Britt-Spells, Slebodnik, Sands, & Rollock, 2018; Pieterse, Todd, Neville, & Carter, 2012).
Chronic experiences of racial discrimination by Black Americans may also contribute to sleep problems. A growing body of research has found associations between race, racial discrimination, and sleep problems, independent of a variety of SES measures such as education, income level, employment, and self-identified social class (for review, see Slopen et al., 2016). Black Americans on average experience more sleep problems and less ideal sleep duration (i.e., both shorter and longer durations associated with greater health problems; Buxton & Marcelli, 2010) compared to White Americans (Hall et al., 2009; Petrov & Lichstein, 2016). Differences in adults’ self-reported measures of sleep quality have been corroborated by polysomnographic studies finding that Black Americans on average have less deep sleep (i.e., slow wave sleep) and more light sleep (stages 1 and 2) than White Americans (Thomas, Bardwell, Ancoli-Israel, & Dimsdale, 2006; Tomfohr, Pung, Edwards, & Dimsdale, 2012). Both Thomas and colleagues (2006) and Tomfohr and colleagues (2012) found that differences in perceived discrimination mediated the effect of race on sleep architecture. Similarly, Slopen and Williams (2014) found that race no longer significantly predicted self-reported sleep problems after controlling for experiences of racial discrimination. These patterns appear to be mirrored in Black children and adolescents: a recent literature review of youth ages 6–19 found that Black youth have shorter sleep duration and poorer sleep quality than White youth (Guglielmo, Gazmararian, Chung, Rogers, & Hale, 2018). In addition, a recent longitudinal study of college students by Fuller-Rowell and colleagues (2017) found that discrimination mediated growing differences in sleep quality between White and Black American students over 1.5 years at a predominantly White university. Thus, although multiple factors likely contribute to racial differences in sleep, racial discrimination appears to play a significant role.
Because depressive symptoms are often comorbid with sleep problems (Riemann et al., 2001), and like sleep problems, are also associated with chronic inflammation and high allostatic load (Dooley et al., 2018; Fiksdal et al., 2019), depressive symptoms may represent a sensitive index of racial discrimination’s impact on multiple systems, potentially forecasting effects on sleep. This raises the possibility that chronic experiences of racial discrimination perceived by Black Americans may contribute to sleep problems both directly through physiological mechanisms (i.e., chronic activation of stress responses) and indirectly through depressive symptoms. Indeed, a meta-analysis of the effects of discrimination on sleep found that associations between discrimination and sleep are generally attenuated when controlling for depressive symptoms (Slopen et al., 2016), suggesting that at least part of the relationship between racial discrimination and sleep problems may be related to effects of discrimination on depressive symptoms.
At the same time, the relation between sleep and depression could be bidirectional (Riemann et al., 2001), and it is foreseeable that changes in sleep resulting from hypervigilance could lead to increases in depressive symptoms over time. Indeed, Steffen and Bowden (2006) found that sleep disturbance mediated the relationship between perceived racism and depressive symptoms in Hispanic-American immigrants, though this cross-sectional study cannot determine temporal order. A recent longitudinal study spanning nine years found that self-reported sleep mediated the effect of everyday discrimination on later physical and mental health, including depressive symptoms, in a large sample of middle-aged, mostly European American adults (Hisler & Brenner, 2019). Additional longitudinal work considering different timeframes and with ethnic minority populations is needed to better understand how effects of racial discrimination may unfold over time.
Do Effects of Racial Discrimination Replicate Across Sex and Developmental Stage?
Many previous studies investigating the effects of race and/or racial discrimination on sleep include only women (Hall et al., 2009; Lewis et al., 2013) or group men and women together (Grandner et al., 2012; Hoggard & Hill, 2018; Thomas et al., 2006). Doing so may obscure unique patterns among men and women. Some studies find that Black American women are more likely to report increased exposure to stressful life events and discrimination than Black American men and are more likely than men to report poor subjective sleep quality (Johnson et al., 2016). At the same time, there is evidence to suggest that Black American men may experience unique gendered racial discrimination (e.g., being perceived as physically or sexually violent; Schwing, Wong, & Fann, 2013). In addition, men may underreport depressive symptoms or experience depression differently than women (S. Rice, Fallon, & Bambling, 2011; Ridge, Emslie, & White, 2011). Given the multifaceted influence of gender on appraisal and exposure to racial discrimination, associations between racial discrimination, depressive symptoms, and sleep problems must be investigated separately among men and women.
In addition, expression of sleep problems and depressive symptoms in youth may not follow the same patterns as for adults. Differences have been observed in Major Depressive Disorder symptom profiles between adolescents and adults, with adolescents tending to experience more vegetative symptoms such as insomnia (Rice et al., 2019). There are also developmental considerations in children’s ability to recognize and be influenced by racial discrimination (Brown, Alabi, Huynh, & Masten, 2011; Spears Brown & Bigler, 2005), and, conversely, youth may be more sensitive to experiences of racial discrimination as an extension of typically high sensitivity to social evaluation during this life stage (Somerville, 2013). Several studies have found effects of racial discrimination on depressive symptoms in Black American youth (Brody et al., 2006; Madubata et al., 2018; Simons et al., 2002), and effects of racial discrimination on sleep have also been found in adolescents (Majeno, Tsai, Huynh, McCreath, & Fuligni, 2018). However, only a few recent studies (e.g., Goosby, Cheadle, Strong-Bak, Roth, & Nelson, 2018; Yip, Wang, & El-sheikh, 2019) have examined associations between racial discrimination and sleep problems in Black youth. In a recent small study using daily diaries and actigraphy in 35 White, Black, and biracial 11–14-year-olds, Goosby and colleagues (2018) found that adolescents reporting higher average discrimination experiences also had poorer average sleep quality. Surprisingly, however, youths’ sleep quality was better (i.e., lower wake after sleep onset [WASO] scores) on days they reported experiencing discrimination. A larger study of 13–15-year-olds by Yip and colleagues (2019) also using daily diaries of discrimination experiences and actigraphy, along with self-reported sleep, found that on days adolescents experienced discrimination they fell asleep faster (potentially indicating greater exhaustion), reported more disturbed sleep, experienced more next-day dysfunction, and reported feeling sleepier the following day, but had no difference in actigraphy-measured WASO. Longer-term longitudinal research is needed to investigate potential cumulative effects of chronic racial discrimination experiences in Black youth.
The Present Study
The present study extends research on experiences of perceived racial discrimination, depressive symptoms, and sleep problems using two waves of data from mothers, fathers, and their early adolescent children living in the rural South. This longitudinal design allows us to examine potential pathways and directionality of effects of racial discrimination on depression and sleep. Our first research question was whether recent experiences of racial discrimination (retrospective report of discrimination over the past 6 months) would be associated with concurrently measured sleep problems and depressive symptoms, and whether recent experiences of racial discrimination would be prospectively associated with sleep problems and depressive symptoms measured eight months later. We hypothesized that for all family members, recent experiences of racial discrimination would be positively associated with concurrent and subsequent sleep problems and depressive symptoms. Our second research question investigated indirect effects of racial discrimination on subsequent sleep problems and depressive symptoms in order to better understand longitudinal pathways between discrimination, sleep problems, and depressive symptoms. Specifically, we examined whether racial discrimination had significant indirect effects on changes in sleep problems through earlier depressive symptoms, and whether discrimination had significant indirect effects on changes in depressive symptoms through earlier sleep problems. All models were examined separately for Black mothers, fathers, and youth.
Method
Participants and Procedures
This study used data from the Protecting Strong African American Families (ProSAAF) project, a randomized controlled trial of a family-centered intervention to promote strong couple, co-parenting, and parent-child relationships in Black American families (full study overview is provided in Barton et al., 2018). All participants were members of Black families residing in small rural towns and communities in the southern U.S. Families with a child between the ages of 9 and 14 years (Mage = 10.87, SD = 0.90) were recruited. Of the total sample of 346 families who began the ProSAAF trial, 63% were married, with a mean length of marriage of 9.97 years (range: 0 to 56 years). Unmarried couples had been living together for an average of 6.73 years (range: < 1 to 23). Men’s mean age was 40.07 years (SD = 9.12; range: 21 to 83) and women’s mean age was 36.73 (SD = 7.27; range: 23 to 73). Men’s median education level was high school or graduate equivalency diploma (ranging from < Grade 9 to a doctorate or professional degree) and women’s median education level was some college or trade school (ranging from < Grade 9 to a master’s degree). Over half (51%) of participating families had incomes below 100% of the poverty line, and 68% had incomes below 150% of the poverty line. Median monthly income was $1375 (SD = $1375; range $1 to $7500) for men and $1220 (SD = $1440; range $1 to $10,000) for women. All procedures were approved by the University of Georgia Institutional Review Board (study title: “Protecting Strong African American Families”; IRB approval number 2012104112); parents and youth provided informed consent and assent prior to data collection and program participation.
The current study utilized data from the second and third waves of the ProSAAF data collection (hereafter referred to as Time 1 [T1] and Time 2 [T2], respectively), because sleep problems were not assessed at wave 1. Data for T1 and T2 were collected approximately 8 months apart, between 2013 and 2016. The intervention preceded T1, and there was a booster session halfway between T1 and T2. Since intervention response was not a focus of the present study, and the intervention was not designed to influence consequences of discrimination, intervention status was a covariate in all analyses. Only participants who completed all measures at both T1 and T2 were included in analyses; this included 277 women, 248 men, and 276 youth (46% Female, 54% Male). Participants included in the analyses were not statistically different from the full sample in age, experiences of racial discrimination, sleep problems, or depressive symptoms (ps > .20).
Measures
Racial discrimination.
Nine items from the Daily Life Experience subscale of the Racism and Life Experience scales (Harrell, Merchant, & Young, 1997) were used to assess experiences of perceived racial discrimination at T1. Previous research has reported evidence of this scale’s validity and reliability for measuring perceived experiences of racism (Alvarez, Juang, & Liang, 2006). The scale asks participants to report the frequency of experiencing various racial stressors over the past 6 months, and includes items such as: “Have you been ignored, overlooked, or not given service because of your race?” and “Have you been treated as if you were stupid, or been talked to like you were slow because of your race?” with responses on a 4-point Likert scale (1 = never, 2 = once or twice, 3 = a few times, 4 = frequently). Scores were summed with higher scores indicating higher levels of discrimination. Alpha coefficients at T1 were .91 for fathers, .92 for mothers, and .90 for youth. At T1, the majority of mothers (73.3%), fathers (83.9%) and youth (69.2%) reported experiencing at least one instance of racial discrimination in the past 6 months.
Depressive symptoms.
Depressive symptoms were measured at T1 and T2 using the Center for Epidemiological Studies Depression Scale (CES-D; Radloff, 1977). The CES-D is a widely used measure of depression and has been validated in rural communities (Husaini, Neff, Harrington, Hughes, & Stone, 1980). Items assessed how often in the past week participants experienced symptoms such as feeling depressed, feeling everything they did was an effort, happiness (reverse coded), loneliness, enjoying life (reverse coded), feeling sad, and feeling unmotivated. Responses range from 0 = Rarely or none of the time (0–1 day) to 3 = Most or all of the time (6–7 days). The full CES-D includes 20 items, but an item on restless sleep was removed for the analyses to prevent artificial inflation of the correlation between sleep problems and depression. Depressive symptom scores were summed with higher values indicating higher frequency of depressive symptoms. Alpha coefficients at T1 were .81 for fathers (.80 with restless sleep question omitted), .85 for mothers (.84 with restless sleep question omitted), and .78 for youth (.78 with restless sleep question omitted). At T2, alpha coefficients were .83 for fathers (.82 with restless sleep question omitted), .88 for mothers (.87 with restless sleep question omitted), and .80 for youth (.80 with restless sleep question omitted). Depressive symptoms were relatively common in the sample, with 26.6% of fathers, 27.8% of mothers, and 30.4% of youth reporting clinically relevant depressive symptoms on the CES-D at T1 (scores ≥ 16; Radloff, 1977).
Sleep problems.
Adults’ sleep problems were assessed at T1 and T2 using the 9-item sleep problems index of the Medical Outcomes Study Sleep Scale (MOS; Hays, Martin, Sesti, & Spritzer, 2005). Sample items include “How often did you get enough sleep to feel rested in the morning?” (reverse scored) and “How often did you awaken from your sleep and have trouble falling asleep again?”, with responses ranging from 1 = none of the time to 5 = all of the time. MOS Sleep Scale scores are summed and linearly transformed to yield a possible range of 0 to 100, with higher values representing more sleep problems (i.e., poorer sleep quality). A random sample of 1011 adults 18 and over in the U.S. (81% White) yielded a mean sleep problems index of 25.79 (Hays et al., 2005). In agreement with expected comparatively elevated sleep problems in Black Americans, mean sleep problems were somewhat higher in the present sample of Black mothers (T1: M = 36.42, SD = 15.60) and fathers (T1: M = 32.94, SD = 16.42) than in Hays et al.’s general U.S. population sample. Alpha coefficients at T1 were .81 for fathers and .77 for mothers; at T2 alphas were .81 for fathers and .83 for mothers.
Youth sleep problems were assessed at T1 and T2 using an abbreviated two-item scale adapted from this measure, consisting of the following questions: “How many times each week did you feel sleepy during the day?” and “How many times each week did you have trouble falling asleep?” with responses ranging from 1 = none of the time to 5 = all of the time. The Spearman-Brown coefficient was calculated for the youth sleep problems scale, as this statistic is less biased than either Cronbach’s alpha or the Pearson correlation for evaluating the reliability of two-item measures (Eisinga, Grotenhuis, & Pelzer, 2013).The Spearman-Brown coefficient for youth was .59 at T1 and .56 at T2. At T1, 22.5% of youth reported feeling sleepy during the day all or most of the time, and 35.9% reported having trouble falling asleep all or most of the time.
Descriptive statistics for the study sample are reported in Table 1 and bivariate correlations among study variables are reported in Table 2.
Table 1.
Descriptive Statistics
| Variables | Fathers (N = 248) | Mothers (N = 277) | Youth (N = 276) |
|---|---|---|---|
| M (SD) | M (SD) | M (SD) | |
| T1 Racial Discrimination | 17.29 (5.96) | 14.17 (5.33) | 12.94 (5.12) |
| T1 Depressive Symptomsa | 12.15 (7.76) | 12.85 (8.44) | 13.16 (8.07) |
| T2 Depressive Symptomsa | 11.96 (8.70) | 12.57 (9.67) | 12.52 (8.31) |
| T1 Sleep Problems | 32.94 (16.42) | 36.42 (15.60) | 4.87 (1.95) |
| T2 Sleep Problems | 30.24 (16.62) | 33.16 (17.75) | 4.66 (1.96) |
Notes. T1 = Time 1; T2 = Time 2 (8 months after T1).
Means and standard deviations for the CES-D are calculated using full 20-item score totals including the sleep disturbance item, which was excluded from the scale for correlations, regressions, and indirect effect analyses.
Table 2.
Correlations Among Study Variables for Fathers, Mothers, and Youth
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| Mothers (N = 285–335) | |||||||
| 1. T1 Discrimination | ---- | ||||||
| 2. T1 Depression | .13* | ---- | |||||
| 3. T2 Depression | .10† | .66*** | ---- | ||||
| 4. T1 Sleep problems | .11† | .50*** | .38*** | ---- | |||
| 5. T2 Sleep problems | .23*** | .50*** | .54*** | .62*** | ---- | ||
| 6. Intervention | .01 | −.01 | .02 | .06 | .17** | ---- | |
| 7. Age | −.05 | −.04 | −.05 | .01 | −.05 | −.03 | ---- |
| Fathers (N = 258–333) | |||||||
| 1. T1 Discrimination | ---- | ||||||
| 2. T1 Depression | .23*** | ---- | |||||
| 3. T2 Depression | .22*** | .65*** | ---- | ||||
| 4. T1 Sleep problems | .32*** | .48*** | .39*** | ---- | |||
| 5. T2 Sleep problems | .22*** | .43*** | .49*** | .59*** | ---- | ||
| 6. Intervention | .05 | −.02 | .02 | .10 | .07 | ---- | |
| 7. Age | −.02 | .05 | .04 | −.03 | −.05 | .00 | ---- |
| Youth (N = 285–344) | |||||||
| 1. T1 Discrimination | ---- | ||||||
| 2. T1 Depression | .46*** | ---- | |||||
| 3. T2 Depression | .22*** | .45*** | ---- | ||||
| 4. T1 Sleep problems | .22*** | .39*** | .30*** | ---- | |||
| 5. T2 Sleep problems | .21*** | .30*** | .34*** | .45*** | ---- | ||
| 6. Intervention | .02 | −.04 | .05 | .05 | .01 | ---- | |
| 7. Age | −.03 | .02 | .10* | .07 | .00 | −.02 | ---- |
| 8. Sex | −.03 | .07 | .18** | .13* | .18** | .08 | .02 |
Note. Ns vary due to missing data; pairwise deletion was used for bivariate correlations.
p < .10.
p < .05.
p < .01.
p < .001
Analytic Strategy
We began by conducting a series of multiple regression analyses (four per family member) using IBM SPSS 25 to address our first research question regarding whether experiences of racial discrimination were concurrently or prospectively associated with sleep problems and, similarly, whether experiences of racial discrimination were concurrently or prospectively associated with depressive symptoms, controlling for age, sex (for youth), and intervention status. We then addressed our second research question regarding indirect effects of discrimination on subsequent sleep problems and depressive symptoms. To do so, we first examined pathways from T1 racial discrimination to change in sleep problems through T1 depressive symptoms by calculating indirect effects and 95% bootstrap confidence intervals based on 5,000 resamples using the PROCESS computational macro for IBM SPSS Statistics 25 (Model 4; Preacher & Hayes, 2008). Change was modeled by including T2 sleep problems as the outcome and T1 sleep problems as a predictor variable. Next we investigated the reverse pathways in the same manner, calculating indirect effects of T1 racial discrimination on change in depressive symptoms (i.e., T2 depressive symptoms as the outcome and T1 depressive symptoms as a predictor variable) through T1 sleep problems. Age, intervention status, and sex (for youth) were included as covariates in all analyses.
Results
Cross-Sectional and Prospective Associations Between Racial Discrimination and Depressive Symptoms and Sleep Problems
To address our first research question, we examined cross-sectional and prospective associations between racial discrimination and depressive symptoms, and between racial discrimination and sleep problems. Results are shown in Table 3. For fathers and youth, T1 racial discrimination had significant positive associations with T1 and T2 depressive symptoms (fathers T1: b = .32, p < .001; fathers T2: b = .32, p < .001; youth T1: b = .72, p < .001; youth T2: b = .37, p < .001) and T1 and T2 sleep problems (fathers T1: b = .85, p < .001; fathers T2: b = .57, p = .001; youth T1: b = .09, p < .001; youth T2: b = .09, p < .001), such that fathers and youth who experienced more racial discrimination reported more depressive symptoms and sleep problems at both time points. For mothers, racial discrimination was positively associated with T1 depressive symptoms (mothers T1: b = .18, p = .04) and T1 and T2 sleep problems (mothers T1: b = .34, p = .05; mothers T2: b = .78, p < .001), but not with T2 depressive symptoms (mothers T2: b = .17, p = .10).
Table 3.
T1 Racial Discrimination as a Predictor of T1 and T2 Sleep Problems and Depressive Symptoms: Regression Coefficients, Standard Errors, and Model Summary Information
| Antecedent | T1 Outcomes | T2 Outcomes | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 Depression | T1 Sleep Problems | T2 Depression | T2 Sleep Problems | |||||||||
| b | SE | P | b | SE | P | b | SE | p | b | SE | p | |
| Mothers (N = 277) | ||||||||||||
| T1 Discrimination | .18 | .09 | .04 | .34 | .18 | .05 | .17 | .10 | .10 | .78 | .19 | <.001 |
| Age | −.05 | .07 | .43 | .06 | .13 | .66 | −.05 | .08 | .49 | −.10 | .14 | .49 |
| Intervention | −.05 | .96 | .96 | 2.05 | 1.87 | .27 | .25 | 1.09 | .82 | 5.92 | 2.06 | .004 |
| Constant | 11.36 | 2.87 | <.001 | 28.56 | 5.60 | <.001 | 11.15 | 3.26 | <.001 | 22.98 | 6.16 | <.001 |
| F test | F(3,273) = 1.64, p = .18 | F(3,273) = 1.67, p = .17 | F(3,273) = 1.14, p = .33 | F(3,273) = 8.30, p < .001 | ||||||||
| Fathers (N = 248) | ||||||||||||
| T1 Discrimination | .32 | .08 | <.001 | .85 | .17 | <.001 | .32 | .09 | <.001 | .57 | .18 | .001 |
| Age | .02 | .01 | .04 | −.01 | .02 | .63 | .01 | .01 | .38 | −.02 | .021 | .46 |
| Intervention | −.92 | .90 | .31 | 3.12 | 1.98 | .12 | −.37 | 1.03 | .72 | 1.22 | 2.08 | .56 |
| Constant | 5.53 | 1.47 | <.001 | 17.09 | 3.25 | <.001 | 5.65 | 1.68 | <.001 | 20.54 | 3.41 | <.001 |
| F test | F(3,244) = 7.79, p < .001 | F(3,244) = 10.01, p < .001 | F(3,244) = 4.83, p = .003 | F(3,244) = 3.87, p = .01 | ||||||||
| Youth (N = 276) | ||||||||||||
| T1 Discrimination | .72 | .08 | <.001 | .09 | .02 | <.001 | .37 | .09 | <.001 | .09 | .02 | <.001 |
| Age | .36 | .46 | .44 | .18 | .13 | .17 | .95 | .51 | .07 | .06 | .13 | .65 |
| Intervention | −1.14 | .82 | .17 | .12 | .23 | .61 | .34 | .92 | .71 | −.15 | .23 | .52 |
| Sex | 1.09 | .82 | .19 | .54 | .23 | .02 | 2.89 | .92 | .002 | .65 | .23 | .005 |
| Constant | −1.81 | 5.26 | .73 | .95 | 1.47 | .52 | −7.64 | 5.87 | .20 | 2.06 | 1.47 | .16 |
| F test | F(4,271) = 20.84, p < .001 | F(4,271) = 5.80, p < .001 | F(4,271) = 7.50, p < .001 | F(4,271) = 5.48, p < .001 | ||||||||
Notes. T1 = Time 1, T2 = Time 2 (8 months after T1). Significant effects are shown in bold text.
Indirect Effects of Racial Discrimination on Change in Sleep and Depressive Symptoms
Our second research question addressed pathways from racial discrimination to change in sleep problems through depressive symptoms and pathways from racial discrimination to change in depressive symptoms through sleep problems. Indirect effects (IEs) for fathers, mothers, and youth are reported in Table 4 and coefficients for paths in the mediation analyses predicting changes in sleep problems from T1 to T2 are shown in Figure 1. Although there was no significant total effect of racial discrimination on change in sleep for fathers (b = .03, 95% CI [−.08, .14]), there was a significant IE of fathers’ racial discrimination on increases in sleep problems from T1 to T2 through T1 depressive symptoms (IE = .05, 95% CI [.01, .09]). Mothers’ experiences of racial discrimination had both a significant total effect on change in sleep from T1 to T2 (b = .17, 95% CI [.12, .36]), and also had a significant IE on increased sleep problems through T1 depressive symptoms (IE = .03, 95% CI [.00, .07]). For mothers, direct effects of T1 racial discrimination on T2 sleep problems remained significant after controlling for the indirect path through depressive symptoms (b = .15, 95% CI [.08, .27]), reflecting that immediate effects on depressive symptoms did not fully account for increases in sleep problems. For youth, the IE of racial discrimination on changes in sleep from T1 to T2 through T1 depressive symptoms was not significant, but was comparable to IEs observed in adults, with similar magnitude but a broader confidence interval (IE = .04, 95% CI [−.02, .12]). A significant total effect of racial discrimination on increases in youth’s sleep from T1 to T2 (b = .13, 95% CI [.02, .24]) became non-significant (b = .09, 95% CI [−.03, .21]) after accounting for indirect effects through T1 depressive symptoms.
Table 4.
Indirect Effects of Racial Discrimination on Change in Sleep Problems and Depressive Symptoms from Time 1 to Time 2
| Mothers | Fathers | Youth | |||||
|---|---|---|---|---|---|---|---|
| Outcome | Mediator | IE | 95% CI | IE | 95% CI | IE | 95% CI |
| ΔSleep Problems | T1 Depression | .03 | [.00, .07] | .05 | [.01, .09] | .04 | [−.02, .12] |
| ΔDepression | T1 Sleep Problems | .01 | [−.01, .03] | .03 | [−.01, .07] | .03 | [−.00, .06] |
Notes. Age, and intervention status were included as covariates in all models; sex was also included as a covariate for the youth models. Statistically significant results (i.e., with 95% confidence intervals not including zero) are bolded for emphasis. IE = indirect effect (standardized).
Figure 1.
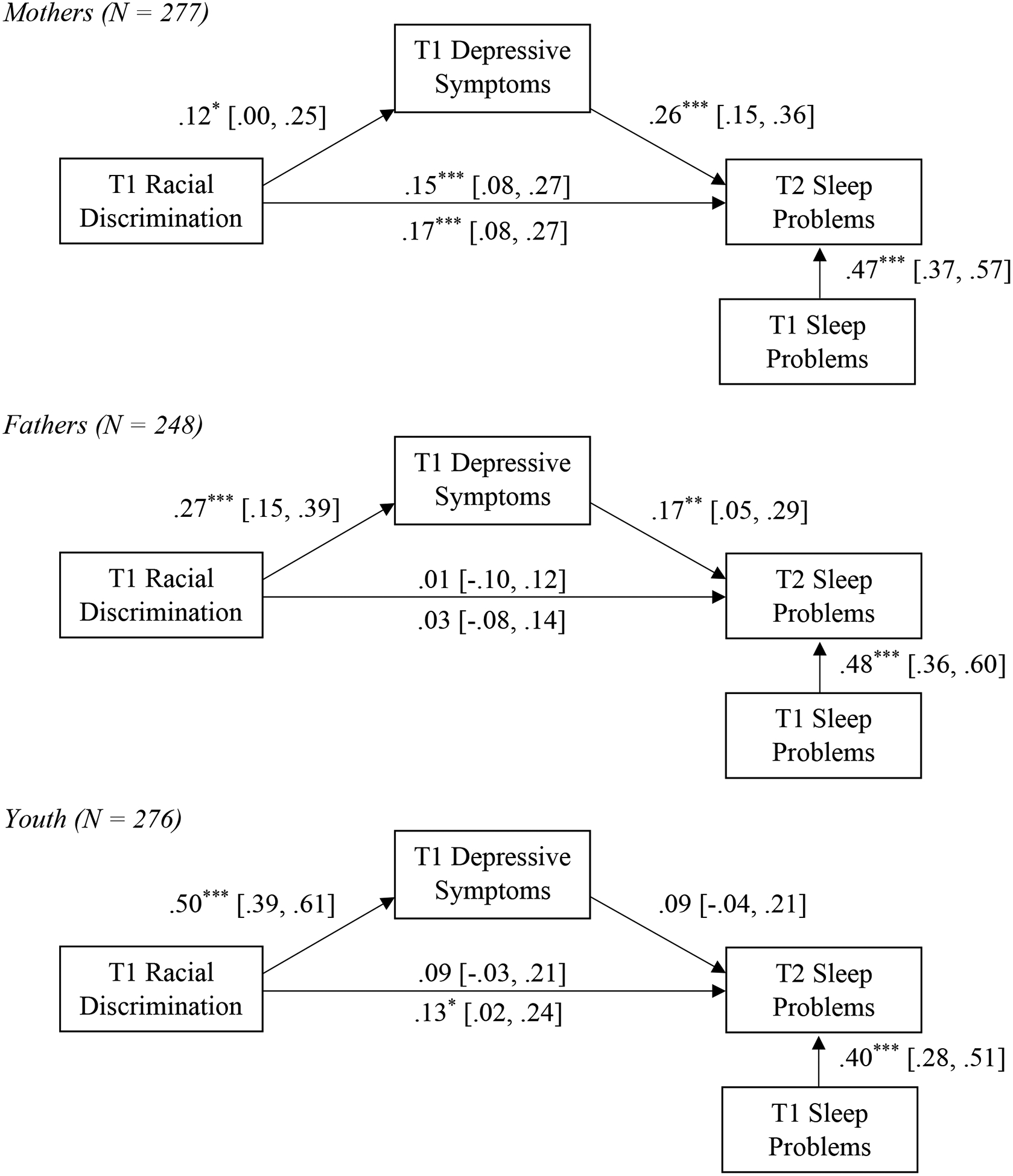
Path models for mothers, fathers, and youth showing the effect of racial discrimination on change in sleep problems through depression. All models include age and intervention status as covariates; youth models also include sex as a covariate. Standardized coefficients are shown with 95% confidence interval in brackets. Total effects of racial discrimination on change in sleep problems before accounting for indirect effects are shown on the underside of path. *p < .05. **p < .01. ***p < .001.
We also calculated indirect effects of racial discrimination on T1 to T2 change in depressive symptoms through T1 sleep problems. No indirect effects of racial discrimination on eight-month change in depressive symptoms from T1 to T2 through T1 sleep problems were observed for fathers, mothers, or youth (see Table 4; all path coefficients are shown in Supplemental Figure S1).
Discussion
Racial discrimination and other chronic stressors experienced by Black Americans may contribute to physical and mental health disparities through a variety of mechanisms that require additional attention and explication. The current study included cross-sectional and longitudinal analyses to examine linkages between perceived experiences of racial discrimination, depressive symptoms, and sleep problems for fathers, mothers, and their early adolescent children in 277 Black families in rural Southern counties. Results replicated associations of racial discrimination with both sleep problems and depressive symptoms, adding to the growing body of literature on the role of interpersonal racism in mental and physical health disparities (Carter et al., 2019) and supporting the supposition that these associations are significant across age and sex. For men, reports of racial discrimination were associated with concurrent and future reports of sleep problems and depressive symptoms, indicating relatively immediate and sustained effects of racial discrimination on both sleep problems and depressive symptoms. Similar associations were observed for youth, for whom reports of racial discrimination were also concurrently and prospectively associated with both sleep problems and depressive symptoms. Although these associations were similar overall for women, unexpectedly, racial discrimination was found to be concurrently but not prospectively associated with depressive symptoms. This suggests that racial discrimination experiences may have a more immediate impact on women’s depression, triggering quicker increases that are not sustained over the assessment period of eight months. It is possible that Black women may use different coping strategies (e.g., drawing on social support) than Black men, which in turn may help them process experiences of racial discrimination over time and reduce the impact of these experiences on depressive symptomatology. In future studies it will be important to consider this possibility and to evaluate follow-up assessments of varying lengths to better understand the lasting effects of racial discrimination on depressive symptoms for men and women.
Despite the differences observed between men and women in the long-term associations between racial discrimination and depressive symptoms, indirect effect analyses indicated that for both men and women, perceived racial discrimination led to subsequent change in sleep problems through depressive symptoms. This implies that depressive symptoms may play a role in the maintenance and development of sleep problems following experiences of racial discrimination in Black adults. For men, this indirect effect was observed despite a nonsignificant total effect of racial discrimination on change in sleep problems; this is unsurprising given that power to detect total effects is typically much lower than power to detect indirect effects, especially when the magnitude of the total effect is small as expected in this case (Agler & De Boeck, 2017). A small, nonsignificant total effect on change in sleep from the time of reported discrimination to eight months later is aligned with the conclusion from the cross-sectional and prospective associations described above that, for men, the effect of discrimination on sleep may be relatively immediate and sustained. For women, there was a significant relation between racial discrimination and subsequent change in sleep problems, and this relation remained significant after accounting for indirect effects through depressive symptoms. This suggests there may be differences in timing/pathways of these associations between women and men, such that women’s physiological responses to stressors like discrimination may continue to unfold over time. Some researchers have recognized the traumatic nature of experiences of racial discrimination and argued that these experiences can be associated with posttraumatic stress-like reactions (e.g., Bryant-Davis & Ocampo, 2005). The longitudinal increase in physiological (i.e., sleep) symptoms found in women in this study is consistent with the idea that experiencing racial discrimination triggers a trauma response (i.e., increased difficulty sleeping may be part of a hypervigilance reaction to trauma, which may be maintained or increase months or years after a traumatic experience). Further research should investigate whether other posttraumatic stress symptoms, such as anger, avoidance, hypervigilance, intrusion, and low self-esteem, precede or accompany sleep problems in response to perceived racial discrimination.
For youth, experiences of racial discrimination predicted subsequent increases in sleep problems, without a significant indirect effect through depressive symptoms. However, the magnitude of indirect effects through depressive symptoms were similar to those seen in adults, only with a broader confidence interval. Given that the youth sleep problems questionnaire included only two items, the limited range and precision of this scale may have contributed to the apparent difference in findings for indirect effect analyses between adults and children. In addition, the particularly strong association between racial discrimination and depressive symptoms observed for youth at T1 reduced power to detect indirect effects, due to high multicollinearity between racial discrimination and depressive symptoms in predicting sleep problems and determining the value of the “b” path. The nonsignificant indirect effect for youth may therefore reflect insufficient power. At the same time, it is likely that, as suggested in models for women, factors other than depressive symptoms also played a significant role in the increase in sleep problems in the eight months following reported experiences of racial discrimination for youth. Measures of anxiety and/or other posttraumatic stress disorder symptoms, for instance, may more fully capture the psychological response to discrimination and potential mechanisms leading to physical health decrements in youth. Overall, the present study supports the influence of racial discrimination on mental and physical health, as well as the role of the psychological response to racially discriminatory experiences in maintaining and magnifying sleep problems.
Strengths and Limitations
Results of this study are limited in several ways. First, the timeframe of eight-month follow-up is arbitrary, and effects could differ if measured over a shorter or longer period of time. The relatively longer time scale of the present study is an advantage in examining cumulative effects of chronic discrimination over time, but it does not allow for more precisely ordering effects of experiences of discrimination, as a daily diary study might. For example, previous research using daily diaries found a day lag between experiencing discrimination and reports of depressive symptoms (Torres & Ong, 2010); another study found that retrospective reports of discrimination predicted actigraphy-assessed sleep quality whereas immediate decrements were not detected in response to daily dairy reports of discrimination (Goosby et al., 2018).
A second limitation is that all measures were self-report surveys. Associations between reports of racial discrimination and reports of depressive symptoms could therefore reflect a common underlying variable rather than covariation in the constructs of interest. In addition, although experiences of racial discrimination over the past 6 months were treated as preceding concurrently measured sleep and depression due to their shorter (or unspecified) timeframes, temporal precedence cannot be guaranteed at T1 due to potential limitations inherent in retrospective self-report. In addition, self-report measures of sleep are subject to reporting bias (Matthews et al., 2018). However, although self-reported sleep duration has been found to be inaccurate as compared to objective sleep measures (Jackson, Patel, Jackson, Lutsey, & Redline, 2018), self-reported sleep quality (which is conceptually overlapping with sleep problems as we report here) has been associated with relevant health outcomes such as metabolic syndrome and cognitive functioning, and provides meaningful additional information to supplement objective sleep measures like actigraphy and polysomnography (Bernstein, Devito, & Calamia, 2019; Bowman et al., 2019). Thus the concurrent and predictive validity supported in these studies reduces concern about our use of this measure. In addition, this study did not include anxiety as either a covariate or mediator. Anxiety is often comorbid with depression, and may also play a role in the psychological response to racial discrimination and contribute to sleep problems. As noted above, experiencing racial discrimination may also function as trauma and elicit symptoms of posttraumatic stress, which could include depression and anxiety, but also a self-maintaining cycle of symptoms like anger, avoidance, hypervigilance, intrusion, and low self-esteem (Carter & Sant-Barket, 2014). A posttraumatic stress response may be especially likely in a sample like this one, which was collected from rural counties in the Southeastern US where many individuals experience risk factors for Post-Traumatic Stress Disorder (PTSD) such as poverty and unemployment (Lowe, Galea, Uddin, & Koenen, 2014). In light of our findings that depressive symptoms did not fully account for the association between racial discrimination and increases in sleep problems over time, future research should also consider the role anxiety and other posttraumatic symptoms may play in these processes.
The present study also has several strengths. First, for convenience and accessibility, the majority of research is done on individuals living in or near urban centers and college towns, but the present sample of Black Americans was drawn from rural counties in the Southern US. Families living in these communities are not only infrequently included in research, but also have relatively high rates of poor health outcomes (Miller, Chen, Yu, & Brody, 2017). Second, associations between racial discrimination, depressive symptoms, and sleep problems were replicated across family members, adding to the relatively scant literature including Black men and children in examining the impact of racial discrimination on sleep. Third, use of a prospective longitudinal design within indirect effect models allowed for establishment of temporal precedence in relations between depressive symptoms and sleep problems. Given continued prevalence of injustices and prejudice enacted against minorities in the US, it is important to consider the long-term effects of racial discrimination on Black Americans’ health and wellbeing and the implications of current research for culturally-informed interventions. Based on these findings, it may be important to acknowledge the stress of racial discrimination in behavioral and psychological treatments aimed at addressing depression and sleep difficulties for Black Americans. In addition, interventions which effectively decrease depressive symptoms may also reduce accumulating, long-term effects of racial discrimination on sleep.
Future Directions
The present study demonstrated effects of racial discrimination on sleep problems and depressive symptoms in all Black American family members, as well as indirect effects on changes in sleep through depressive symptoms for men and women (and possibly youth). This study therefore provides some support for the hypothesis that depressive symptoms may serve as an index of racial discrimination’s impact on multiple systems and forecast effects on sleep. Future research should examine longer term patterns of health outcomes and the physiological and psychological mechanisms that underlie these patterns, including potential alternative psychological mechanisms through anxiety or posttraumatic stress symptoms, especially for women and youth. In addition, in order to prevent the accumulation and expansion of these effects, it will be important to examine the factors that may buffer effects of interpersonal racism (as measured in this study) on depression and sleep. These factors may include race-specific protective factors such as racial socialization, or more general factors such as protective parenting (Brody et al., 2006) or social support (Odafe, Salami, & Walker, 2017). Conversely, it will be important to consider potential exacerbating factors, such as experience of vicarious discrimination (Wofford, Defever, & Chopik, 2019), neighborhood-level segregation (Williams & Collins, 2001), and financial hardship (Hall et al., 2009). It will also be important to test for these patterns in other groups who also experience significant discrimination, in order to ascertain how universal or specific these processes are, as well as to consider the role of intersecting marginalized identities (e.g., female, Black) in potentially exacerbating the psychological and physiological impacts of discrimination. Lastly, continued longitudinal research on these associations will be important. In particular, repeated assessments of racial discrimination, depressive symptoms, and sleep would be useful to allow for better characterization of the relative influence of within-person and between person effects (for discussion of between- and within-person effects, see Curran & Bauer, 2011). These analyses would expand on the between-person effects described here (e.g., women with higher levels of racial discrimination report higher levels of concurrent depressive symptoms relative to women with lower levels of racial discrimination) by testing whether, for example, for a given woman, depressive symptoms are higher at times when she experiences more racial discrimination than is typical (relative to her own average). This type of analysis would provide a useful elaboration of these processes. Better understanding pathways of response to racial discrimination and the factors that influence these effects can inform conceptual frameworks outlining the insidious effects of racial discrimination and inform treatment for and prevention of depression, sleep problems, and related health problems among Black Americans.
Supplementary Material
Public Significance Statement:
Experiences of racial discrimination are common and associated with poorer mental and physical health for Black Americans. This study linked racial discrimination to depressive symptoms and sleep problems for men, women, and their children in the rural South. Over time, higher levels of depressive symptoms following racial discrimination may lead to increases in sleep problems for Black Americans.
Acknowledgments
This research was supported by the National Institute on Aging R01 AG059260 and NICHD R01HD069439.
References
- Agler R, & De Boeck P (2017). On the interpretation and use of mediation: Multiple perspectives on mediation analysis. Frontiers in Psychology, 8, 1–11. 10.3389/fpsyg.2017.01984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez AN, Juang L, & Liang CTH (2006). Asian Americans and racism: When bad things happen to “model minorities.” Cultural Diversity and Ethnic Minority Psychology, 12, 477–492. 10.1037/1099-9809.12.3.477 [DOI] [PubMed] [Google Scholar]
- Barton AW, Beach SRH, Wells AC, Ingels JB, Corso PS, Sperr MC, … Brody GH (2018). The Protecting Strong African American Families program: A randomized controlled trial with rural African American couples. Prevention Science, 19, 904–913. 10.1007/s11121-018-0895-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein JPK, Devito A, & Calamia M (2019). Subjectively and objectively measured sleep predict differing aspects of cognitive functioning in adults. Archives of Clinical Neuropsychology, 1–11. 10.1093/arclin/acz017 [DOI] [PubMed] [Google Scholar]
- Bowman MA, Duggan KA, Brindle RC, Kline CE, Krafty RT, Thayer JF, & Hall MH (2019). Prospective associations among objectively and subjectively assessed sleep and the metabolic syndrome. Sleep Medicine, 58, 1–6. 10.1016/j.sleep.2019.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britt-Spells AM, Slebodnik M, Sands LP, & Rollock D (2018). Effects of perceived discrimination on depressive symptoms among Black men residing in the United States: A meta-analysis. American Journal of Men’s Health, 12, 52–63. 10.1177/1557988315624509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Chen Y, Murry VM, Ge X, Simons RL, Gibbons FX, … Cutrona CE (2006). Perceived discrimination and the adjustment of African American youths: A five-year longitudinal analysis with contextual moderation effects. Child Development, 77, 1170–1189. 10.1111/j.1467-8624.2006.00927.x [DOI] [PubMed] [Google Scholar]
- Brown CS, Alabi BO, Huynh VW, & Masten CL (2011). Ethnicity and gender in late childhood and early adolescence: Group identity and awareness of bias. Developmental Psychology, 47, 463–471. 10.1037/a0021819 [DOI] [PubMed] [Google Scholar]
- Bryant-Davis T, & Ocampo C (2005). Racist incident–based trauma. The Counseling Psychologist, 33, 479–500. 10.1177/0011000005276465 [DOI] [Google Scholar]
- Buxton OM, & Marcelli E (2010). Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Social Science & Medicine, 71, 1027–1036. 10.1016/j.socscimed.2010.05.041 [DOI] [PubMed] [Google Scholar]
- Carl Vinson Institute of Government. (2003). Dismantling persistent poverty in Georgia. Athens, GA: University of Georgia. [Google Scholar]
- Carter RT, Johnson VE, Kirkinis K, Roberson K, Muchow C, & Galgay C (2019). A meta-analytic review of racial discrimination: Relationships to health and culture. Race and Social Problems, 11, 15–32. 10.1007/s12552-018-9256-y [DOI] [Google Scholar]
- Carter RT, Lau MY, Johnson V, & Kirkinis K (2017). Racial discrimination and health outcomes among racial/ethnic minorities: A meta-analytic review. Journal of Multicultural Counseling and Development, 45, 232–259. 10.1002/jmcd.12076 [DOI] [Google Scholar]
- Carter RT, & Sant-Barket SM (2014). Assessment of the impact of racial discrimination and racism: How to use the race-based traumatic stress symptom scale in practice. Traumatology, 21(1), 32–39. 10.1037/trm0000018 [DOI] [Google Scholar]
- Clark R, Anderson NB, Clark VR, & Williams DR (1999). Racism as a stressor for African Americans: A biopsychosocial model. American Psychologist, 54, 805–816. [DOI] [PubMed] [Google Scholar]
- Colen CG, Ramey DM, Cooksey EC, & Williams DR (2018). Racial disparities in health among nonpoor African Americans and Hispanics: The role of acute and chronic discrimination. Social Science & Medicine, 199, 167–180. 10.1016/j.socscimed.2017.04.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran PJ, & Bauer DJ (2011). The disaggregation of within-person and between-person effects in longitudinal models of change. Annual Review of Psychology, 62, 583–619. 10.1146/annurev.psych.093008.100356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutrona CE, Clavél FD, & Johnson MA (2016). African American couples in rural contexts In Crockett LJ & Carlo G (Eds.), Rural ethnic minority youth and families in the United States: Theory, research, and applications (pp. 127–142). Cham, Switzerland: Springer International Publishing; 10.1007/978-3-319-20976-0 [DOI] [Google Scholar]
- Dooley LN, Kuhlman KR, Robles TF, Eisenberger NI, Craske MG, & Bower JE (2018). The role of inflammation in core features of depression: Insights from paradigms using exogenously-induced inflammation. Neuroscience and Biobehavioral Reviews, 94, 219–237. 10.1016/j.neubiorev.2018.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisinga R, Grotenhuis M. te, & Pelzer B(2013). The reliability of a two-item scale: Pearson, Cronbach, or Spearman-Brown? International Journal of Public Health, 58, 637–642. 10.1007/s00038-012-0416-3 [DOI] [PubMed] [Google Scholar]
- Fiksdal A, Hanlin L, Kuras Y, Gianferante D, Chen X, Thoma MV, & Rohleder N (2019). Associations between symptoms of depression and anxiety and cortisol responses to and recovery from acute stress. Psychoneuroendocrinology, 102, 44–52. 10.1016/j.psyneuen.2018.11.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller-Rowell TE, Curtis DS, El-Sheikh M, Duke AM, Ryff CD, & Zgierska AE (2017). Racial discrimination mediates race differences in sleep problems: A longitudinal analysis. Cultural Diversity and Ethnic Minority Psychology, 23, 165–173. 10.1037/cdp0000104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT (1992). The weathering hypothesis and the health of African-American women and infants: Evidence and speculations. Ethnicity & Disease, 2, 207–221. [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, & Bound J (2006). “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. American Journal of Public Health, 96, 826–833. 10.2105/AJPH.2004.060749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goosby BJ, Cheadle JE, Strong-Bak W, Roth TC, & Nelson TD (2018). Perceived discrimination and adolescent sleep in a community sample. RSF: The Russell Sage Foundation Journal of the Social Sciences, 4, 43–61. 10.7758/RSF.2018.4.4.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goosby BJ, Malone S, Richardson EA, Cheadle JE, & Williams DT (2015). Perceived discrimination and markers of cardiovascular risk among low-income African American youth. American Journal of Human Biology, 27, 546–552. 10.1002/ajhb.22683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goosby BJ, Straley E, & Cheadle JE (2017). Discrimination, sleep, and stress reactivity: pathways to African American-White cardiometabolic risk inequities. Population Research and Policy Review, 36, 699–716. 10.1007/s11113-017-9439-z [DOI] [Google Scholar]
- Grandner MA, Hale L, Jackson N, Patel NP, Gooneratne NS, & Troxel WM (2012). Perceived racial discrimination as an independent predictor of sleep disturbance and daytime fatigue. Behavioral Sleep Medicine, 10, 235–249. 10.1080/15402002.2012.654548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene ML, Way N, & Pahl K (2006). Trajectories of perceived adult and peer discrimination among Black, Latino, and Asian American adolescents: Patterns and psychological correlates. Developmental Psychology, 42, 218–236. 10.1037/0012-1649.42.2.218 [DOI] [PubMed] [Google Scholar]
- Guglielmo D, Gazmararian JA, Chung J, Rogers AE, & Hale L (2018). Racial/ethnic sleep disparities in US school-aged children and adolescents: A review of the literature. Sleep Health, 4, 68–80. 10.1016/j.sleh.2017.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall MH, Matthews KA, Kravitz HM, Gold EB, Buysse DJ, Bromberger JT, … Sowers M (2009). Race and financial strain are independent correlates of sleep in midlife women: The SWAN sleep study. Sleep, 32, 73–82. 10.5665/sleep/32.1.73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardeman RR, Murphy KA, Karbeah J, & Kozhimannil KB (2018). Naming institutionalized racism in the public health literature: A systematic literature review. Public Health Reports, 133, 240–249. 10.1177/0033354918760574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays RD, Martin SA, Sesti AM, & Spritzer KL (2005). Psychometric properties of the Medical Outcomes Study Sleep measure. Sleep Medicine, 6, 41–44. 10.1016/j.sleep.2004.07.006 [DOI] [PubMed] [Google Scholar]
- Hicken MT, Lee H, Ailshire J, Burgard SA, & Williams DR (2013). “Every shut eye, ain’t sleep”: The role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race and Social Problems, 5, 100–112. 10.1007/s12552-013-9095-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hisler GC, & Brenner RE (2019). Does sleep partially mediate the effect of everyday discrimination on future mental and physical health? Social Science & Medicine, 221, 115–123. 10.1016/j.socscimed.2018.12.002 [DOI] [PubMed] [Google Scholar]
- Hoggard LS, & Hill LK (2018). Examining how racial discrimination impacts sleep quality in African Americans: Is perseveration the answer? Behavioral Sleep Medicine, 16, 471–481. 10.1080/15402002.2016.1228648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husaini BA, Neff JA, Harrington JB, Hughes MD, & Stone RH (1980). Depression in rural communities: Validating the CES-D scale. Journal of Community Psychology, 8, 20–27. [DOI] [Google Scholar]
- Jackson CL, Patel SR, Jackson WB, Lutsey PL, & Redline S (2018). Agreement between self-reported and objectively measured sleep duration among white, black, Hispanic, and Chinese adults in the United States: Multi-ethnic study of atherosclerosis. Sleep, 41(6), 1–12. 10.1093/sleep/zsy057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson DA, Lisabeth L, Lewis TT, Sims M, Hickson DA, Samdarshi T, … Roux AVD (2016). The contribution of psychosocial stressors to sleep among African Americans in the Jackson Heart Study. Sleep, 39, 1411–1419. 10.5665/sleep.5974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M (2014). Racial/ethnic disparities in depression and its theoretical perspectives. Psychiatric Quarterly, 85(1), 1–8. 10.1007/s11126-013-9265-3 [DOI] [PubMed] [Google Scholar]
- Landrine H, & Klonoff EA (1996). The Schedule of Racist Events: A measure of racial discrimination and a study of its negative physical and mental health consequences. Journal of Black Psychology, 22, 144–168. [Google Scholar]
- Lewis TT, Troxel WM, Kravitz HM, Bromberger JT, Matthews KA, & Hall MH (2013). Chronic exposure to everyday discrimination and sleep in a multiethnic sample of middle-aged women. Health Psychology, 32, 810–819. 10.1037/a0029938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe SR, Galea S, Uddin M, & Koenen KC (2014). Trajectories of posttraumatic stress among urban residents. American Journal of Community Psychology, 53, 159–172. 10.1007/s10464-014-9634-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madubata IJ, Odafe MO, Talavera DC, Hong JH, & Walker RL (2018). Helplessness mediates racial discrimination and depression for African American young adults. Journal of Black Psychology, 44, 626–643. 10.1177/0095798418811476 [DOI] [Google Scholar]
- Majeno A, Tsai KM, Huynh VW, McCreath H, & Fuligni AJ (2018). Discrimination and sleep difficulties during adolescence: The mediating roles of loneliness and perceived stress. Journal of Youth and Adolescence, 47, 135–147. 10.1007/s10964-017-0755-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Patel SR, Pantesco EJ, Buysse DJ, Kamarck TW, Lee L, & Hall MH (2018). Similarities and differences in estimates of sleep duration by polysomnography, actigraphy, diary, and self-reported habitual sleep in a community sample. Sleep Health, 4, 96–103. 10.1016/j.sleh.2017.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, Yu T, & Brody GH (2017). Metabolic syndrome risks following the great recession in rural black young adults. Journal of the American Heart Association, 6(9), 1–9. 10.1161/JAHA.117.006052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossakowski KN (2003). Coping with perceived discrimination: Does ethnic identity protect mental health? Journal of Health and Social Behavior, 44, 318–331. [PubMed] [Google Scholar]
- Neblett EW (2019). Racism and health: Challenges and future directions in behavioral and psychological research. Cultural Diversity and Ethnic Minority Psychology, 25(1), 12–20. 10.1037/cdp0000253 [DOI] [PubMed] [Google Scholar]
- Noh S, & Kaspar V (2003). Perceived discrimination and depression: Moderating effects of coping, acculturation, and ethnic support. American Journal of Public Health, 93, 232–238. 10.2105/AJPH.93.2.232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odafe MO, Salami TK, & Walker RL (2017). Race-related stress and hopelessness in community-based African American adults: Moderating role of social support. Cultural Diversity and Ethnic Minority Psychology, 23, 561–569. 10.1037/cdp0000167 [DOI] [PubMed] [Google Scholar]
- Pascoe EA, & Smart Richman L (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135, 531–554. 10.1037/a0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrov ME, & Lichstein KL (2016). Differences in sleep between black and white adults: An update and future directions. Sleep Medicine, 18, 74–81. 10.1016/j.sleep.2015.01.011 [DOI] [PubMed] [Google Scholar]
- Pickett KE (2001). Multilevel analyses of neighbourhood socioeconomic context and health outcomes: A critical review. Journal of Epidemiology & Community Health, 55, 111–122. 10.1136/jech.55.2.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieterse AL, Todd NR, Neville HA, & Carter RT (2012). Perceived racism and mental health among black american adults: A meta-analytic review. Journal of Counseling Psychology, 59(1), 1–9. 10.1037/a0026208 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. 10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Priest N, Slopen N, Woolford S, Philip JT, Singer D, Kauffman AD, … Williams D (2018). Stereotyping across intersections of race and age: Racial stereotyping among White adults working with children. PLOS ONE, 13(9), e0201696 10.1371/journal.pone.0201696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Probst JC, Samuels ME, Jespersen KP, Willert K, Swann RS, & McDuffie JA (2002). Minorities in Rural America: An overview of population characteristics. Columbia, SC: University of South Carolina, Norman J. Arnold School of Public Health. [Google Scholar]
- Radloff LS (1977). The CES-D scale. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Rice F, Riglin L, Lomax T, Souter E, Potter R, Smith DJ, … Thapar AK (2019). Adolescent and adult differences in major depression symptom profiles. Journal of Affective Disorders, 243, 175–181. 10.1016/j.jad.2018.09.015 [DOI] [PubMed] [Google Scholar]
- Rice S, Fallon B, & Bambling M (2011). Men and depression: The impact of masculine role norms throughout the lifespan. The Australian Educational and Developmental Psychologist, 28, 133–144. 10.1375/aedp.28.2.133 [DOI] [Google Scholar]
- Ridge D, Emslie C, & White A (2011). Understanding how men experience, express and cope with mental distress: Where next? Sociology of Health & Illness, 33, 145–159. 10.1111/j.1467-9566.2010.01266.x [DOI] [PubMed] [Google Scholar]
- Riemann D, Berger M, & Voderholzer U (2001). Sleep and depression — results from psychobiological studies: An overview. Biological Psychology, 57, 67–103. 10.1016/S0301-0511(01)00090-4 [DOI] [PubMed] [Google Scholar]
- Schwing AE, Wong YJ, & Fann MD (2013). Development and validation of the African American men’s gendered racism stress inventory. Psychology of Men & Masculinity, 14(1), 16–24. 10.1037/a0028272 [DOI] [Google Scholar]
- Seaton EK, Caldwell CH, Sellers RM, & Jackson JS (2008). The prevalence of perceived discrimination among African American and Caribbean Black youth. Developmental Psychology, 44, 1288–1297. 10.1037/a0012747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons RL, Murry V, McLoyd V, Lin K-H, Cutrona C, & Conger RD (2002). Discrimination, crime, ethnic identity, and parenting as correlates of depressive symptoms among African American children: A multilevel analysis. Development and Psychopathology, 14, 371–393. 10.1017/S0954579402002109 [DOI] [PubMed] [Google Scholar]
- Slopen N, Lewis TT, & Williams DR (2016). Discrimination and sleep: A systematic review. Sleep Medicine, 18, 88–95. 10.1016/j.sleep.2015.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, & Williams DR (2014). Discrimination, other psychosocial stressors, and self-reported sleep duration and difficulties. Sleep, 37(1), 147–156. 10.5665/sleep.3326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerville LH (2013). The teenage brain: Sensitivity to social evaluation. Current Directions in Psychological Science, 22(2), 121–127. 10.1177/0963721413476512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spears Brown C, & Bigler RS (2005). Children’s perceptions of discrimination: A developmental model. Child Development, 76, 533–553. 10.1111/j.1467-8624.2005.00862.x [DOI] [PubMed] [Google Scholar]
- Steffen PR, & Bowden M (2006). Sleep disturbance mediates the relationship between perceived racism and depressive symptoms. Ethnicity & Disease, 16, 16–21. [PubMed] [Google Scholar]
- Thomas KS, Bardwell WA, Ancoli-Israel S, & Dimsdale JE (2006). The toll of ethnic discrimination on sleep architecture and fatigue. Health Psychology, 25, 635–642. 10.1037/0278-6133.25.5.635 [DOI] [PubMed] [Google Scholar]
- Tickamyer AR, & Duncan CM (1990). Poverty and opportunity structure in rural America. Annual Review of Sociology, 16, 67–86. Retrieved from https://www.jstor.org/stable/2083263 [Google Scholar]
- Tomfohr L, Pung MA, Edwards KM, & Dimsdale JE (2012). Racial differences in sleep architecture: The role of ethnic discrimination. Biological Psychology, 89(1), 34–38. 10.1016/j.biopsycho.2011.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres L, & Ong AD (2010). A daily diary investigation of Latino ethnic identity, discrimination, and depression. Cultural Diversity and Ethnic Minority Psychology, 16, 561–568. 10.1037/a0020652 [DOI] [PubMed] [Google Scholar]
- Williams DR (2012). Miles to go before we sleep: Racial inequities in health. Journal of Health and Social Behavior, 53, 279–295. 10.1177/0022146512455804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Collins C (2001). Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports, 116, 404–416. 10.1016/S0033-3549(04)50068-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Jackson PB (2005). Social sources of racial disparities in health. Health Affairs, 24(2), 325–334. 10.1377/hlthaff.24.2.325 [DOI] [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, & Jackson JS (2003). Racial/ethnic discrimination and health: Findings from community studies. American Journal of Public Health, 93, 200–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wofford N, Defever AM, & Chopik WJ (2019). The Vicarious Effects of Discrimination: How Partner Experiences of Discrimination Affect Individual Health. Social Psychological and Personality Science, 10, 121–130. 10.1177/1948550617746218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong CA, Eccles JS, & Sameroff A (2003). The influence of ethnic discrimination and ethnic identification on African American adolescents’ school and socioemotional adjustment. Journal of Personality, 71, 1197–1232. 10.1111/1467-6494.7106012 [DOI] [PubMed] [Google Scholar]
- Yip T (2015). The effects of ethnic/racial discrimination and sleep quality on depressive symptoms and self-esteem trajectories among diverse adolescents. Journal of Youth and Adolescence, 44, 419–430. 10.1007/s10964-014-0123-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yip T, Cheon YM, Wang Y, Cham H, Tryon W, & El-Sheikh M (2019). Racial disparities in sleep: Associations with discrimination among ethnic/racial minority adolescents. Child Development, 1–18. 10.1111/cdev.13234 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


