Abstract
Background
The COVID-19 pandemic has created unprecedented challenges for healthcare globally, the brunt of which has been borne by the health care providers (HCPs). These challenges are felt more keenly in India, as they stretch an insufficiently resourced healthcare system. The long hours, cross over of responsibilities, lack of resources to adequately care for patients, and concerns around safety of self and loves ones, have led to a spike in anxiety, depression, insomnia and other stress – related disorders in healthcare providers. Sudarshan Kriya Yoga (SKY) is a mind-body intervention that has been studied in multiple clinical populations. Prior to this study, there has been no exploration of the impact of SKY on healthcare providers, specifically the impact of a mind-body intervention like SKY on HCPs during a pandemic.
Objective
This study aims to investigate the impact of SKY on the well-being of HCPs during the COVID-19 pandemic.
Methods
We conducted a pilot feasibility study with a single arm pre-post design. SKY was taught to participants in a 4-day online breath and meditation workshop. We measured outcomes related to depression, anxiety, resilience, life satisfaction, and quality of sleep.
Results
Ninety-two subjects completed the study survey before and after the intervention. A significant reduction was observed in the levels of stress, anxiety and depression immediately after the program. In addition, the participants reported sig1nificant improvement in life satisfaction, resilience, and the quality of their sleep.
Conclusion
The results indicate that SKY breathing technique had a positive impact on the well-being of healthcare professionals during the pandemic. Participants experienced improved quality of sleep, enhanced satisfaction with life, and increased resilience after SKY. This pilot study provides important data for future multi-site randomized controlled trials to study the impact of yogic techniques on well-being of the HCPs.
Keywords: Sudarshan Kriya Yoga, healthcare providers, well-being, pandemic, resilience
Introduction
The current COVID-19 pandemic has spread across the globe, affecting people of all nationalities, irrespective of their gender, age, ethnicity or socioeconomic status. Due to its highly infectious nature, ease of transmission and associated lack of standardized treatment, the novel SARS-CoV-2 virus has produced a significant morbidity and mortality, staggering at both scientific and societal levels.1 In addition, the pandemic has affected the health and well-being of humans in unintended ways. For eg. the physical distancing necessary to control the spread of the virus often worsens the feelings of social isolation for those with anxiety and depression.2
Healthcare providers (HCP) have been exceptionally strained during the pandemic. They have a higher risk of exposure to the virus.3 They work longer hours without enough recovery time. They deal with the worry of infecting their families and loved ones on a daily basis. There are shortages of supplies and personal protective equipment (PPE), and HCPs are often expected to take emotionally and ethically challenging decisions around resource allocation.
The COVID-19 healthcare challenges loom large over the under resourced & already stretched Indian healthcare system. In 2012, India had 3.3 qualified allopathic doctors and 3.1 nurses and midwives for every 10,000 of her population. This number is less than 25% of the World Health Organization’s benchmark of 22.8 doctors, nurses and midwives per 10,000 population.4 Additionally, healthcare workers have been the targets of violence during the COVID-19 pandemic.5 Consequently, it is no surprise that the Indian HCPs suffer from anxiety, depression, burnout, insomnia and stress-related disorders6 similar to what is seen in other countries.7
There have been numerous studies that have looked at reducing stress and burnout in HCPs using programs incorporating mind-body practices, cognitive skills, community building, and connecting with meaning and purpose in work.8–11 In that vein, yoga and meditation-based interventions hold a significant promise and potential to boost well-being of HCPs. Recent studies that have examined the effects of various yoga based interventions on different HCPs populations have demonstrated similar improvements.12–15
Although yoga practices have gained in popularity, there still exist barriers to its adoption and implementation among the healthcare community. The common ones include skepticism, cost, lack of time & access to high quality yoga classes and teachers, and stereotypes related to flexibility and athleticism.16,17 In addition, to our knowledge, there haven’t been any yoga-based interventions that have specifically targeted HCPs during the COVID-19 pandemic. One approach that has been posited to address these challenges is Sudarshan Kriya Yoga (SKY). SKY is a cyclical controlled breathing practice with its roots in traditional yoga practices. In previous studies, SKY has been shown to help individuals with stress and mood disorders, including clinical depression and anxiety.18–20 The aim of our study is to evaluate the effect of SKY on the well-being of HCPs during the current COVID-19 pandemic in India.
Methods
Study Design
We conducted a pilot feasibility study with a single arm pre-post design. The data was collected between the months of April-June 2020 from participants who attended an online workshop that taught yogic breathing exercises. The mental states of depression, anxiety, stress, quality of sleep, resilience, and satisfaction with life for each individual were assessed using a standardized set of questionnaires at three different time points during the study: pre-intervention, immediately post-intervention (day 4, last day of the workshop), and after 40 days of practice. Data was collected via online questionnaires created on Google Forms. All participants were contacted for the assessment on day 40 through email and personal phone numbers. The Institutional Review Board of the Sri Sri Institute for Advanced Research in India approved this study bearing registration number SSIAR/IEC/02/2020.
Participants
A “health care provider” was defined as: a doctor of medicine, podiatrist, dentist, chiropractor, clinical psychologist, optometrist, nurse practitioner, nurse-midwife, or a clinical social worker who is authorized to practice by the state. Forty-five online SKY workshops for HCPs were organized in India between April to June 2020. A total of 7597 HCPs participated in these workshops. The organizers of these workshops were informed regarding the research study and were invited to participate. HCPs were enrolled in the online SKY workshops through word of mouth publicity, social media platforms and doctor & hospital networks.
On the first day of the SKY workshop, the participants were informed about the research study. Those who agreed to participate were included in the study after signing an informed consent form online. The study enrollment was stopped once 100 people were enrolled. The participants filled in the questionnaire which included questions regarding their exposure and treatment of COVID-19 patients.
Intervention
Sudarshan Kriya Yoga (SKY) is a method of cyclical controlled breathing and meditation practice. A typical SKY session is 30 minutes long and consists of four distinct yogic breathing stages (Ujjayi, Bhastrika, Om, and Sudarshan Kriya). Ujjayi involves experiencing the conscious sensation of the breath touching the throat. This slow breath technique is performed at a rate of 2–4 breaths per minute (bpm). During Bhastrika, the air is rapidly inhaled and forcefully exhaled at a rate of 20 bpm. Three one-minute rounds of Bhastrika are followed by a few minutes of normal breathing. Next, Om is chanted three times with very prolonged expiration. Lastly, Sudarshan Kriya rhythmic breathing is done with slow (20 bpm), medium (40–50 bpm), and fast (60–80 bpm). A SKY session is done in a seated posture, with eyes closed.
Sudarshan Kriya Yoga was taught to participants in a 4-day online breath and meditation workshop. The workshop was 8 hours long (2-hour session each day), and taught over a video conference. Experienced SKY instructors trained by the Art of Living Foundation facilitated the workshops.
The participants also learnt the 35-minute-long home practice, which included Pranayama, Bhastrika and the SKY breathing. They were encouraged to practice SKY breathing at home daily.
Measures
Depression, Anxiety and Stress Scale
The Depression, Anxiety and Stress Scale (DASS-21) is a set of three 7-item self-report scales designed to measure the emotional states of depression, anxiety, and stress. Each item is answered on a 0–3 Likert scale, based upon subject’s reflection over the past week. The summative scores for each domain range from 0–21. DASS-21 has been found to have high internal consistency and is used in a variety of settings to measure the current state or changes in emotional states over time. Higher scores correlate with stronger negative emotional states.21
Pittsburgh Sleep Quality Index
The Pittsburgh Sleep Quality Index (PSQI) is a standardized sleep questionnaire that has been used with multiple populations in many languages. It’s a broad subjective measure consisting of 19 questions, that assesses 7 components of sleep including quality, latency, duration, habitual sleep efficiency, sleep disturbances, the use of sleep medication, and daytime dysfunction. Each component is answered using a 0–3 Likert scale. The component scores are subsequently aggregated to get a global PSQI score. A global PSQI score of 5 or more indicates poor sleep quality.22
Connor-Davidson Resilience Scale
The Connor-Davidson Resilience Scale (CD-RISC) is a 25-item self-rated validated research measure of resilience. Each item is answered on a 0-4 Likert scale by the subject based on how they felt over the past month. The total score ranges from 0–100, and higher scores reflect greater resilience.23
Satisfaction With Life Scale
The Satisfaction with Life Scale (SWLS) is a 5-item scale that measures global cognitive judgments of satisfaction with life. It consists of five statements that participants agree or disagree with on a 1–7 Likert scale. The total score ranges from 5–35, and higher scores reflect greater satisfaction.24
Data Analysis
A paired-sample t-test was used to compare the differences between scores obtained at pre-intervention, post-intervention, and day 40 time points. The Pearson correlation coefficient was calculated to measure the linear correlation between the two variables for all domains in all scales.25 Apart from the descriptive statistical tools, a general linear model involving repeated measure ANOVA was used to elicit the effect of time, and other grouping variables of gender, and covariates of age, and years of medical practice on the dependent variables. A F test was also performed for the assumptions of normality. Levene's test of equality of error variances and Mauchly's test of sphericity were also carried out. Effect size was calculated via Cohen’s d value. Reliability and internal consistency of the questionnaire set was tested by calculating Cronbach’s alpha.
Results
100 participants were enrolled in the study. Of the total participants, ninety-two subjects completed the survey before and after the intervention. Table 1 describes the baseline characteristics of the study population. Overall, the study group had more women than men. Although HCPs from all streams were invited to be a part of the study, only one Ayurvedic doctor and three homeopaths participated. The rest of study participants were HCPs practicing modern medicine. They ranged in their clinical experience, and a large percentage were already treating COVID-19 patients at the baseline assessment in April 2020. Thirty-two healthcare professionals completed the day 40 assessment. By day 40, the percentage of HCPs treating COVID-19 patients, and those who had exposure to COVID-19 had increased, based on the self-reported questionnaires. Information was also gathered on day 40 regarding the frequency of home practice. The study participants reported the following: 46.7% had been practicing SKY daily, 20% were practicing 4–5 times a day, 13.3% were practicing 2–3 days a week and 20% reported practicing at least once a week. None of the participants were noncompliant.
Table 1.
Demographic Data.
|
Participants Characteristics (N = 92) n (%) | ||
|---|---|---|
| Characteristics | Type | All Participants |
| Gender n (%) | M | 38 (41.3) |
| F | 54 (58.7) | |
| Age (years) | Mean (SD) | 43.1 (11.1) |
| Min | 19 | |
| Max | 72 | |
| Marital Status n (%) | Single | 11 (11.9) |
| Married | 68 (73.9) | |
| Divorced | 2 (2.2) | |
| Widowed | 1 (1.1) | |
| Years of Medical Practice | Mean (SD) | 17.4 (10.7) |
| Min | 0 | |
| Max | 50 | |
| Specialty of HCP n (%) | Physicians | 56 (60.8) |
| Non physician clinicians | 17 (18.6) | |
| Non clinicians | 8 (8.7) | |
| Smoking n (%) | No | 80 (86.9) |
| Yes | 2 (2.2) | |
| Alcohol Use n (%) | No | 62 (67.4) |
| Yes | 20 (21.7) | |
| Exposed to COVID–19 n (%) | No | 48 (52.2) |
| Yes | 34 (47.8) | |
| Treated COVID-19 Patients n (%) | No | 64 (69.6) |
| Yes | 18 (19.6) | |
| Last Exposure to COVID-19 n (%) | Less than 15 Days ago | 11 (11.9) |
| More than 15 Days ago | 13 (14.1) | |
| Not Exposed | 58 (63.0) | |
Table 2 describes changes in outcomes pre- and post-intervention, and at day 40.
Table 2.
Mean Scores, Standard Deviation and P Values for All the Measures on Three Time Points.
| Scale | Pre (Mean and SD) | Post (Mean and SD) | Day 40 (Mean and SD) | P Value (Pre-post) | P Value (Pre-day40) |
|---|---|---|---|---|---|
| DASS | |||||
| Stress | 11.4 (7.3) | 7.2 (6.4) | 7.2 (6.4) | p < 0.001** | p = 0.49 |
| Anxiety | 7.3 (6.6) | 5.3 (5.4) | 5.9 (6.4) | p = 0.001** | p = 0.613 |
| Depression | 7.7 (6.7) | 4.1 (5.3) | 4.7 (6.4) | p < 0.001** | p = 0.563 |
| Global PSQI | 6.1 (2.9) | 4.7 (2.7) | 3.9 (2.9) | p < 0.001** | p = 0.154 |
| CD-RISC | 21.2 (7.3) | 24.3 (8.4) | 26.9 (12.3) | p < 0.001** | p = 0.015* |
| SWLS | 24.6 (6.1) | 26.9 (5.5) | 31.7 (3.9) | p < 0.001** | p < 0.001** |
Abbreviation: SD: Standard deviation.
*Significance p < 0.05.
**Significant p < 0.001.
Depression, Anxiety and Stress Scale-21
Over the course of the intervention, there was a statistically significant reduction in the scores reported for all the three states of stress, anxiety and depression (p < 0.001) immediately after the SKY program. Cohen’s d was 0.57 for the pre and post analysis.
Pittsburgh Sleep Quality Index
Over the course of the intervention, there was a statistically significant reduction in the scores (p < 0.001) immediately after the program, but not at 40 days (p = 0.154). The percentage of the population with PSQI scores below 5 increased from 36.9% before the intervention to 54.3% after the intervention, and to 68.75% at day 40. Cohen's d was 0.499 for the pre and post analysis.
Connor-Davidson Resilience Scale
Over the course of the intervention, there was a statistically significant improvement in resilience immediately after the program (p < 0.001); and it continued to increase on day 40 (p = 0.015).
Satisfaction With Life Scale
Over the course of the intervention, there was a statistically significant improvement in life satisfaction immediately after the program (p < 0.001); and it continued to increase on day 40 (p < 0.001).
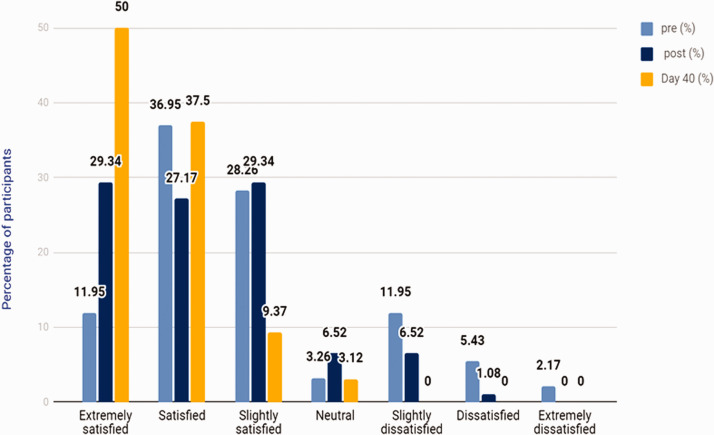
The subjects were categorized in seven degrees of satisfaction ranging from extremely satisfied to extremely dissatisfied. An increase in the overall average score of SWLS was noted after SKY. The percentage of population in the extremely satisfied category also increased post intervention and continued to rise with the practice of SKY. This trend was supported by the simultaneous reduction in the percentage of population with slightly dissatisfied and dissatisfied scores, post SKY. There were none who were dissatisfied on day 40 of the study (Figure 1).
Figure 1.
Satisfaction With Life Score—Percentage of Participants in the Seven Categories at Three Time Points Viz Pre, Post and Day 40.
Pearson correlation coefficient was calculated for stress, anxiety, depression, resilience, life satisfaction and sleep. It was found that stress, anxiety and depression have a moderate negative correlation with resilience (noted at all-time points), and relatively strong negative correlation with life satisfaction (noted at pre and post time points). Poor sleep quality, as demonstrated by high sleep scores, showed a strong negative correlation with stress, anxiety and depression (refer Table 3). Tests for normality of the data confirmed normal distribution.
Table 3.
Pearson Correlation Coefficient.
|
Pre |
Post |
Day 40 |
||||
|---|---|---|---|---|---|---|
| r | p value | r | p value | r | p value | |
| Stress and CD-RISC | −0.297 | 0.004* | −0.345 | 0.001** | −0.382 | 0.031* |
| Anxiety with CD-RISC | −0.298 | 0.004* | −0.279 | 0.007* | −0.464 | 0.007* |
| Depression with CD-RISC | −0.282 | 0.006* | −0.32 | 0.002* | −0.475 | 0.006* |
| Stress and SWLS | −0.479 | <0.001** | −0.367 | <0.001** | −0.402 | 0.022* |
| Anxiety with SWLS | −0.428 | <0.002* | −0.325 | 0.002* | −0.339 | 0.057 |
| Depression with SWLS | −0.46 | <0.003* | −0.399 | <0.001** | −0.292 | 0.105 |
| Stress and PSQI | 0.451 | <0.001** | 0.52 | <0.001** | 0.441 | 0.011* |
| Anxiety with PSQI | 0.393 | <0.001** | 0.427 | <0.001** | 0.457 | 0.009* |
| Depression with PSQI | 0.465 | <0.001** | 0.55 | <0.001** | 0.365 | 0.04* |
*Significant p <0.05.
**Significant p <0.001.
Discussion
To our knowledge, this is the first study that examines the effect of a mind body intervention on HCPs treating COVID-19 patients. Although there are several reviews that promote use of yoga, meditation and Ayurveda to mitigate the negative effects of COVID-19, there are no studies that investigate the direct effects of a yogic breathing technique on the mental wellbeing of HCPs during the current pandemic. By delivering the SKY intervention online, conducting the assessments online, and limiting the time of assessment to 10 minutes, we were able to elicit participation from HCPs, despite their busy schedules during the COVID-19 pandemic.
Immediately after the intervention, we observed significant reductions in stress, anxiety and depression amongst HCPs. In addition, quality of sleep improved immediately post intervention and continued to improve at day 40. The participants expressed greater satisfaction with life after the program and on day 40 after the practice, suggesting a sustained beneficial effect of SKY practice. The same was true for resilience in HCPs who practiced SKY. These results suggest a positive effect of SKY on their well-being during the COVID-19 pandemic.
Similar effects have been observed in previous studies on the benefits of yoga in HCPs. A single arm clinical trial on health care workers in Rome showed that yoga and mindfulness are effective in reducing stress and anxiety, and provide the ability to manage work’s stressful demands.13 Another pilot study of HCPs from the United States demonstrated the positive effect of group mindfulness-based yoga activities on personal accomplishment, depression, anxiety, stress, perceived resilience, and compassion.14 In a recent pilot study on ICU nurses, the nurses who received yoga instruction did better on the measures of quality of life after the intervention.15
Rooted in traditional yoga, the SKY technique has been studied for its impact on various medical conditions including depression, anxiety, PTSD and addiction disorders.18–20,26–30 It has been shown to benefit emotional regulation, autonomic modulation and immune function.31–33 A randomized controlled trial among university students found that with the practice of SKY, participants experienced significantly lowered levels of stress & depression, and betterment of mental health, social connectedness, positive emotion and mindfulness.34 Another study of university students showed reduced stress, anxiety, depression, and distress in those practicing SKY. SKY improved sleep, social connectedness, self-esteem, life satisfaction and conscientiousness and protection against anticipating stress.35
A study was done on 62 medical students (healthy volunteers of 18–27 years of age) in India. The students practiced SKY for 6 months. A morning blood sample taken before their final exams showed significantly lower levels of serum cortisol in the study group compared to the control group (p < 0.001).36 Amongst business executives, the SKY intervention significantly reduced the participants’ stress levels, blood cortisol levels, and increased their life satisfaction, emotional intelligence and emotional stability.37 Our study findings in HCPs are consistent with the stress-reducing effects of SKY in previous studies. It is also evident from our study that reduction in stress, anxiety and depression are correlated with enhanced resilience and satisfaction with life, and these observations are also consistent with previous studies. These correlations provide pilot data for future studies, especially in understanding mechanisms.
A recent review and meta-analysis of the prevention and management of the psychological effects of stress on healthcare care workers during epidemics, recognizes that the risk factors for psychological distress include being younger, more junior, parent of a dependent child, being in quarantine, infection in a family member, and lack of practical support and stigma.38 Though many of these factors are not in our control, the SKY breathing technique, which is taught online and hence can be learnt even during quarantine, offers practical support to the HCPs during this stressful time. This SKY technique has been delivered in multiple countries, in multiple languages to a wide variety of populations globally for over 39 years and can be easily made available to Healthcare providers to help boost their mental well-being and increase satisfaction with life.19,30,34,39
There are several important limitations to acknowledge in this study. The first limitation is the lack of a control group and randomization of study subjects. Causality cannot be determined in a non-controlled, pre-post study design. Selection bias cannot be ruled out as only individuals who wanted to participate in SKY workshops were enrolled for the study. The study was conducted in a single geographic area. There was a large drop-off rate in data collection on day 40.
Having said that, these results serve as important pilot data. The SKY intervention is shown to be feasible and reproducible. SKY has also been delivered in different clinical contexts as demonstrated by prior research studies.
Conclusion
This is a unique study demonstrating the impact of SKY – a yogic breathing technique on the wellbeing and resilience of HCPs. To our knowledge, this is the first study to investigate the effects of a mind-body intervention on HCPs during the COVID-19 pandemic. Importantly, this study took place in India, where there are significant numbers of reported COVID-19 cases. This pilot study demonstrated a positive impact of SKY on reducing stress, anxiety and depression in HCPs during the pandemic. In addition, results suggest sustained improvements in HCP quality of sleep, satisfaction with life, and resilience among those who practiced SKY. These attributes are essential for a healthcare worker to continue caring for their patients in extenuating circumstances with professionalism and passion. Interventions like SKY may serve as prudent options for stress management in HCPs. Future long-term and multi-site randomized controlled studies with larger sample size are necessary to further these benefits on HCPs.
Acknowledgments
We would like to acknowledge The Art of Living Trust, trainers and volunteers who have helped with organizing the online programs.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Divya Kanchibhotla https://orcid.org/0000-0002-0760-630X
Darshan H Mehta https://orcid.org/0000-0003-0457-4717
Conflict of Interest
All the authors declare that there is no financial conflict of interest. DK and SR are SKY trainers but were not involved in subject enrollment or providing the intervention.
References
- 1.World Health Organization: Coronavirus disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update. Accessed August 19, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/
- 2.Pfefferbaum B, North CS. Mental health and the COVID-19 pandemic. N Engl J Med. 2020; 383(6):510–512. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen LH, Drew DA, Joshi AD, et al. Risk of COVID-19 among frontline healthcare workers and the general community: a prospective cohort study. Preprint. medRxiv. Published May 25, 2020. doi:10.1101/2020.04.29.20084111
- 4.Rao KD, Shahrawat R, Bhatnagar A. Composition and distribution of the health workforce in India: estimates based on data from the National Sample Survey. WHO South East Asia J Public Health. 2016; 5(2):133–140. [DOI] [PubMed] [Google Scholar]
- 5.McKay D, Heisler M, Mishori R, Catton H, Kloiber O. Attacks against health-care personnel must stop, especially as the world fights COVID-19. Lancet. 2020; 395(10239):1743–1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta S, Sahoo S. Pandemic and mental health of the front-line healthcare workers: a review and implications in the Indian context amidst COVID-19. Gen Psychiatr. 2020; 33(5):e100284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020; 87:11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shanafelt TD, Dyrbye LN, West CP. Addressing physician burnout: the way forward. JAMA. 2017; 317(9):901–902. [DOI] [PubMed] [Google Scholar]
- 9.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016; 388(10057):2272–2281. [DOI] [PubMed] [Google Scholar]
- 10.Lee HF, Kuo CC, Chien TW, Wang YR. A meta-analysis of the effects of coping strategies on reducing nurse burnout. Appl Nurs Res. 2016; 31:100–110. [DOI] [PubMed] [Google Scholar]
- 11.Scheepers RA, Emke H, Epstein RM, Lombarts KMJMH. The impact of mindfulness-based interventions on doctors’ well-being and performance: a systematic review. Med Educ. 2020; 54(2):138–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cocchiara RA, Peruzzo M, Mannocci A, et al. The use of yoga to manage stress and burnout in healthcare workers: a systematic review. J Clin Med. 2019; 8(3):284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.La Torre G, Raffone A, Peruzzo M, et al. Yoga and mindfulness as a tool for influencing affectivity, anxiety, mental health, and stress among healthcare workers: results of a single-arm clinical trial. J Clin Med. 2020; 9(4):1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ofei-Dodoo S, Cleland-Leighton A, Nilsen K, Cloward JL, Casey E. Impact of a mindfulness-based, workplace group yoga intervention on burnout, self-care, and compassion in health care professionals: a pilot study. J Occup Environ Med. 2020; 62(8):581–587. [DOI] [PubMed] [Google Scholar]
- 15.Rostami K, Ghodsbin F. Effect of yoga on the quality of life of nurses working in intensive care units. Randomized controlled clinical trial . Invest EducEnferm. 2019; 37(3):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramamoorthy A, Jeevakarunyam SJ, Janardhanan S, et al. Survey on utility of yoga as an alternative therapy for occupational hazards among dental practioners. J Nat Sci Biol Med. 2015; 6(1):149–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brems C, Justice L, Sulenes K, et al. Improving access to yoga: barriers to and motivators for practice among health professions students. Adv Mind Body Med. 2015; 29(3):6–13. [PubMed] [Google Scholar]
- 18.Doria S, de Vuono A, Sanlorenzo R, Irtelli F, Mencacci C. Anti-anxiety efficacy of Sudarshan Kriya Yoga in general anxiety disorder: a multicomponent yoga based, breath intervention program for patients suffering from generalized anxiety disorder with or without comorbidities. J Affect Disord. 2015; 184:310–317. [DOI] [PubMed] [Google Scholar]
- 19.Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, Harish MG, Subbakrishna DK, Vedamurthachar A. Antidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: a randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord. 2000; 57(1–3):255–259. [DOI] [PubMed] [Google Scholar]
- 20.Toschi-Dias E, Tobaldini E, Solbiati M, et al. Sudarshan Kriya Yoga improves cardiac autonomic control in patients with anxiety-depression disorders. J Affect Disord. 2017; 214:74–80. [DOI] [PubMed] [Google Scholar]
- 21.Lovibond S, Lovibond PF. Manual for the Depression Anxiety Stress Scales. Sydney, Australia: Psychology Foundation of Australia Inc.; 1996. [Google Scholar]
- 22.Buysse DJ, Reynolds III, Monk CF, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28(2), 193–213. [DOI] [PubMed] [Google Scholar]
- 23.Connor KM, Davidson JR. Development of a new resilience scale: The Connor‐Davidson resilience scale (CD‐RISC). Depress Anxiety. 2003; 18(2):76–82. [DOI] [PubMed] [Google Scholar]
- 24.Diener ED, Emmons RA, Larsen RJ, et al. (1985). The satisfaction with life scale. J Pers Assess. 1985; 49(1): 71–75. [DOI] [PubMed] [Google Scholar]
- 25.Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analag. 2018; 126(5): 1763–1768. [DOI] [PubMed] [Google Scholar]
- 26.Sharma A, Barrett MS, Cucchiara AJ, Gooneratne NS, Thase ME. A breathing-based meditation intervention for patients with major depressive disorder following inadequate response to antidepressants: a randomized pilot study. J Clin Psychiatry. 2017; 78(1):e59–e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Seppälä EM, Nitschke JB, Tudorascu DL, et al. Breathing-based meditation decreases posttraumatic stress disorder symptoms in U.S. military veterans: a randomized controlled longitudinal study. J Trauma Stress. 2014; 27(4):397–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chandra S, Jaiswal AK, Singh R, et al. Mental stress: neurophysiology and its regulation by Sudarshan Kriya Yoga. Int J Yoga. 2017; 10(2):67–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vedamurthachar A, Janakiramaiah N, Hegde JM, et al. Antidepressant efficacy and hormonal effects of Sudarshana Kriya Yoga (SKY) in alcohol dependent individuals. J Affect Disord. 2006; 94(1–3):249–253. [DOI] [PubMed] [Google Scholar]
- 30.Kjellgren A, Bood SA, Axelsson K, et al. Wellness through a comprehensive yogic breathing program—a controlled pilot trial. BMC Complement Altern Med. 2007; 7:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ghahremani DG, Oh EY, Dean AC, et al. Effects of the youth empowerment seminar on impulsive behavior in adolescents. J Adolesc Health. 2013; 53(1):139–141. [DOI] [PubMed] [Google Scholar]
- 32.Zope SA, Zope RA. Sudarshan Kriya Yoga: breathing for health. Int J Yoga. 2013; 6(1):4–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kochupillai V, Kumar P, Singh D, et al. Effect of rhythmic breathing (Sudarshan Kriya and Pranayam) on immune functions and tobacco addiction. Ann N Y Acad Sci. 2005; 1056:242–252. [DOI] [PubMed] [Google Scholar]
- 34.Seppälä EM, Bradley C, Moeller J, et al. Promoting mental health and psychological thriving in university students: a randomized controlled trial of three well-being interventions. Front Psychiatry. 2020; 11:590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goldstein MR, Lewin RK, Allen JJB. Improvements in well-being and cardiac metrics of stress following a yogic breathing workshop: randomized controlled trial with active comparison. J Am Coll Health. 2020;1–11. doi: 10.1080/07448481.2020.1781867. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 36.Kumar S. Effect of “Sudarshan Kriya” on serum cortisol level before terminal examination in undergraduate medical students. IJAR. 2017; 3(7):533–535. [Google Scholar]
- 37.Mulla ZR, Vedamuthachar. Impact of a Sudarshan Kriya-based occupational stress management intervention on physiological and psychological outcomes. Manag Labour Stud. 2014; 39(4):381–395. [Google Scholar]
- 38.Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020; 369:m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kanchibhotla D, Kulkarni S, Singh S. Effectiveness of a comprehensive yoga program on convicted extremist offenders. Int J Yoga. 2020; 13(1):50–54. [DOI] [PMC free article] [PubMed] [Google Scholar]