Abstract
Aim
To test the feasibility, acceptability and preliminary efficacy of using an integrated approach combined online and in‐person delivery to support colorectal cancer (CRC) patients and their spousal caregivers coping positively with cancer together.
Design
A single‐arm pre–post‐feasibility design was used.
Methods
Chinese CRC patient‐partner dyads (N = 24) accessed the blended intervention combined online platform and face‐to‐face sessions for six weeks between October 2019 to January 2020. Feasibility was measured through recruitment and retention and acceptability was examined by intervention engagement and post‐treatment programme evaluation. Effect sizes were calculated using the complete data (N = 20 couple dyads) to evaluate preliminary treatment effect.
Results
Recruitment (70.6%) and retention rates (83.3%) supported programme feasibility. Participants’ positive intervention engagements and evaluations indicated acceptability. The overall small‐to‐medium improvements in most outcome measures verified preliminary efficacy of the integrated couples‐based supportive programme. The findings support its feasible and acceptable for couples coping with CRC and show potential efficacy.
Keywords: blended intervention, cancer, colorectal cancer, couples‐based intervention, oncology, spousal caregiver
1. INTRODUCTION
As one of the most prevalent cancers worldwide, colorectal cancer (CRC) ranks third and second in terms of incidence and mortality, with incidence and mortality rates varying widely in different regions (Bray et al., 2018). According to cancer statistics, the burden of CRC is expected to increase in China in the near future, with nearly 642,300 new CRC cases and 221,100 deaths estimated to occur in 2025 (Zhang et al., 2019).
Cancer diagnosis and treatment affect both patients and spousal caregivers, leading to a growing recognition of couples‐based interventions (Badr & Krebs, 2013; Regan et al., 2012). Reviews have reported that couples‐based interventions had small‐to‐medium beneficial effects on psychological distress, communication, relationship and quality of life (QOL) (Badr & Krebs, 2013; Regan et al., 2012). Our previous “Caring for Couples Coping with Cancer (4Cs)” programme, a single group/uncontrolled study delivered via traditional in‐person dyadic sessions, also showed promising effects on Chinese couples dealing with mixed cancer (Li et al., 2015).
2. BACKGROUND
In the context of CRC, evidence has shown that both CRC patients and their partners are affected during the cancer journey (Traa et al., 2015a) and associations and an interdependent nature exist between CRC patients and their partners in several areas, for example, fatigue (Traa et al., 2016), sexual function and marital function (Traa et al., 2015b). A study also reported that relationship quality within patient‐partner dyads affected a couple's adjustment to CRC, specifically, good relationship functioning benefits psychosocial adjustment (Kayser et al., 2018).
The complex mutual impacts between couples resulted from cancer also existed among Chinese CRC patients and their spousal caregivers. Recently, we conducted a qualitative study and found that CRC presents various challenges for Chinese couples and mutual support played a significant role in couples’ journey coping with CRC together (Li et al., 2018). Although a telephone‐based intimacy enhancement intervention targeting American CRC couples has shown promise (Barsky Reese et al., 2014), it only centred on addressing sexual concerns of couples, rather than focusing on a comprehensive dyadic level, for example dyadic mediator, dyadic appraisal and dyadic coping to help CRC couples coping with cancer. No specific interventions focusing on couples coping with CRC on a dyadic level in China were identified. Given the critical need described above, based on the previous 4Cs programme, to satisfy Chinses CRC couples’ unmet needs (Li et al., 2018), a new 4Cs: CRC dyadic programme was developed, with the intention of better supporting CRC couples coping with cancer on multiple dyadic levels.
Web‐based intervention delivery showed unique advantages over in‐person interventions, including diverse format and content, fewer space‐time restrictions and anonymity (Luo et al., 2020). However, possible disadvantages included a lack of personal interaction(Luo et al., 2020). To best make use of the advantages of both the Internet and traditional delivery formats, we combined an online platform with face‐to‐face sessions into one integrated programme, in a blended intervention. This study aimed to examine the feasibility, acceptability and preliminary efficacy of the 4Cs: CRC programme for CRC patients and their spousal caregivers.
3. METHODS
3.1. Study design and participants
This was a pre–post‐single‐arm intervention study design targeting Chinese CRC patients and spousal caregivers. Eligibility criteria were as follows: adult married couples with one partner diagnosed with CRC (any stage); the patient was cared for by his/her spouse; couples had daily access to a smartphone; and both patient and partner could communicate in Mandarin and were willing to participate in the programme. Participants were recruited in the oncology wards of a cancer hospital in Wuxi City, China, from October 2019 to January 2020. Basic CRC couple demographic and health‐related information was collected pre‐intervention (Table S1).
3.2. Guiding theory
The design of the dyadic intervention was guided by a preliminary Live with Love Conceptual Framework (P‐LLCF) (Figure 1), which was specifically focused on patients‐partners coping with cancer as a unit during the cancer period(Li & Loke, 2015). The P‐LLCF encompassed the following dyadic level domains in a couple's cancer journey: Event Situation, Dyadic Mediators, Dyadic Coping, Dyadic Appraisal and Dyadic Adjustment/Outcomes. In the P‐LLCF, particular events or situations will have an impact on dyadic outcomes directly or indirectly through Dyadic Mediators, which situated above the action wheel, act as ‘‘leverage’’ to balance or offset the stressors, leading to the dyadic appraisal, coping and adjustment of the cancer couple dyads. The dyadic mediators, dyadic appraisal and dyadic coping are interrelated and work together to achieve positive dyadic outcomes, which are the goal and the P‐LLCF’s central focus. These domains were the foundation for the entire intervention design and dyadic learning sessions.
FIGURE 1.
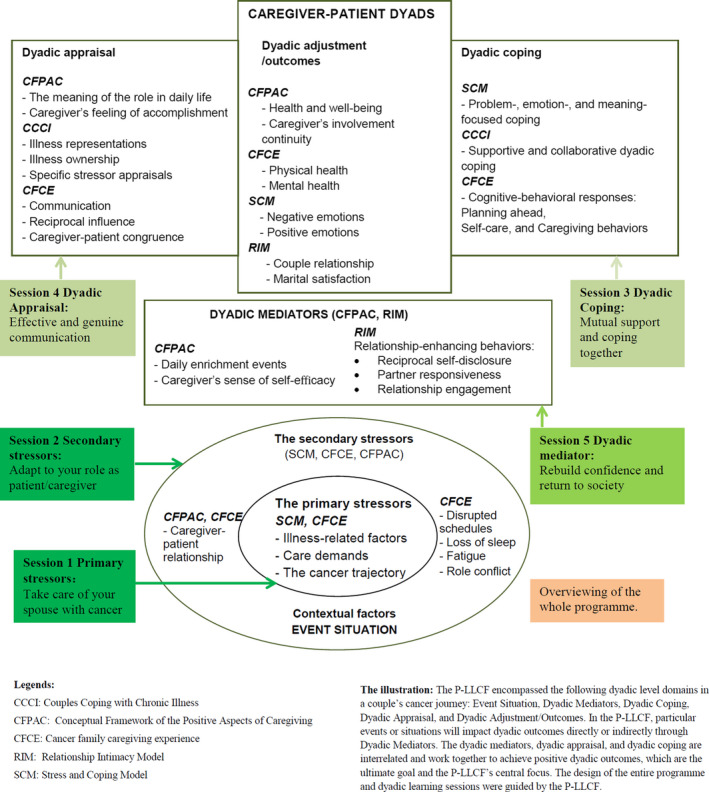
A preliminary Live with Love Conceptual Framework (P‐LLCF) for Cancer Couple Dyads
3.3. Intervention development and content
To satisfy CRC couples’ unmet information needs (Li et al., 2018) and because translating the dyadic CRC psychoeducation sessions into a web‐based format could increase intervention accessibility, an online platform (4Cs: CRC programme) was developed, following the recommendations proposed by a review of dyadic web‐based interventions (Luo et al., 2020) and providing information support, psychoeducation sessions, online communication and skills‐building to support couples coping with CRC. The development of the 4Cs: CRC programme was guided by the P‐LLCF (Li & Loke, 2015).
The online platform consisted of six modules: Dyadic Learning Sessions, Health Information, Cancer News, Online Support, Sharing Circle and Personal Centre. Dyadic Learning Sessions was the central module and included five psychoeducational sessions: Take care of your spouse with cancer; Adapt to your role as patient/caregiver; Mutual support and coping together; Effective and genuine communication; and Rebuild confidence and return to society.
3.4. Measures
Feasibility was evaluated by calculating recruitment and retention rates. Acceptability was determined by face‐to‐face session completion rates, online intervention engagement and postintervention programme evaluation. Multiple instruments were used to measure CRC couples’ outcome domains pre‐ and postintervention (Table S2). All measures were demonstrated to be reliable in the previous 4Cs programme (Li et al., 2015). Considering the “leverage” effect of Dyadic Mediators in the P‐LLCF (Figure 1), self‐efficacy (dyadic mediator) was identified as a primary outcome, measured by the 12‐item Cancer Behavior Inventory (CBI‐B), which evaluates self‐efficacy in people coping with cancer. The CBI‐B Cronbach's α coefficient ranged from 0.84 to 0.88 (Heitzmann et al., 2011).
Secondary outcome measures consisted of the 37‐item Dyadic Coping Inventory (dyadic coping), 15‐item Cancer‐Related Communication Problems within Couples Scale (dyadic appraisal) and four measures for dyadic outcomes, including the medical outcomes study 12‐item short form (QOL), 14‐item hospital anxiety and depression scale (negative emotions), 17‐item benefit‐finding scale (positive emotions) and 14‐item revised dyadic adjustments scale (marital satisfaction). Other measures included a basic demographic and health‐related information sheet (pre‐intervention) and postintervention programme evaluation questionnaire (Table S2).
3.5. Ethics and procedures
All study procedures were approved by the Jiangnan University research ethics committee (JNU20200312IRB09). Once eligible couples gave written informed consent, the dyads independently completed baseline survey measures. They were instructed on how to access the online platform and create a login account prior to study commencement. During the six‐week period, the programme was delivered in a combined format. Weekly reminders were sent to participants asking them to complete each dyadic session. Three couples‐based biweekly (two‐, four‐ and six‐week, respectively) face‐to‐face sessions (each 60–90 min) were held to revisit the online learning sessions and provide additional support if required. The postintervention assessment was administered immediately after intervention completion (at six weeks).
3.6. Data Analyses
Descriptive analyses were used to measure feasibility and acceptability. Due to the small sample size, which limited our power to make inferential statistics as to study variables, we calculated the effect size for patients and their partners separately (using mean pre–post‐change scores/pooled standard deviation). The effect sizes were estimated using Cohen's d, and the effect was classified as large (d = 0.8), medium (d = 0.5) and small (d ≤ 0.2), respectively (Portney & Watkins, 2009). Participants’ pre–post‐intervention improvement was also assessed using minimally clinically important differences (MCID). Analyses were conducted using SPSS version 25.0.
4. RESULTS
Figure 2 illustrates the flow of participants into the study, indicating 70.6% and 83.3% for the recruitment and retention rates, respectively. In terms of face‐to‐face dyadic session engagement, there was an 85% completion rate. Regarding online intervention engagement acceptability, with total approximately 609 views (mean = 21 views per page) for the dyadic learning session module by all included dyads. And the mean view times of each session's pages by per dyad ranged from 3 to 7 views. In addition, participants rated the programme highly in terms of its usefulness, ease of use, as well as satisfaction, with all mean acceptability ratings greater than 5.2 on a 7‐point scale. Open‐ended responses were generally favourable in the postintervention programme evaluation (Table 1).
FIGURE 2.
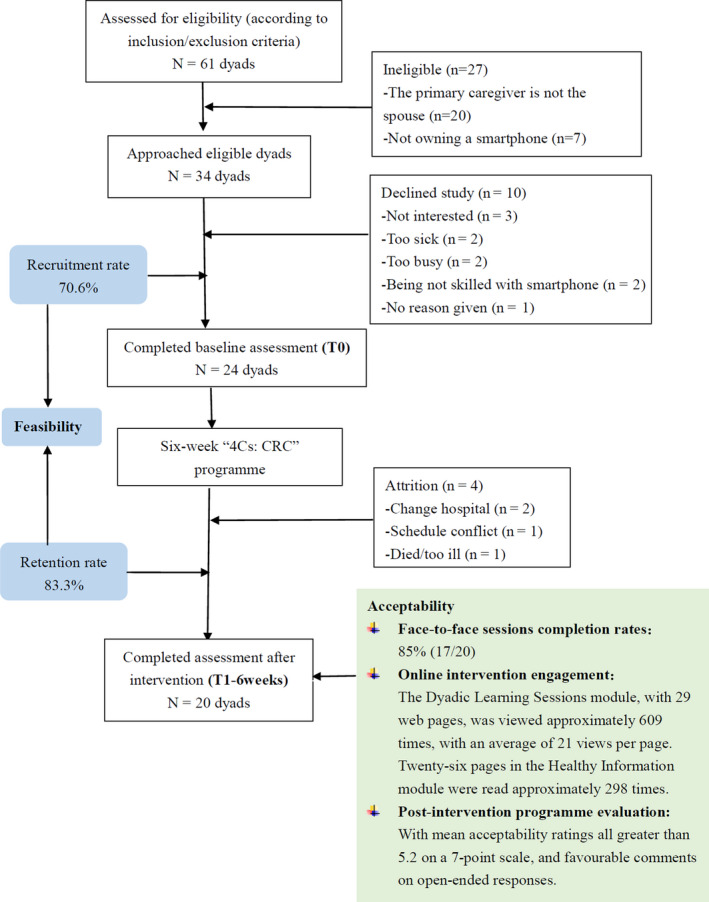
Study consort diagram
TABLE 1.
Feasibility and acceptability outcomes
| Feasibility | |
| Recruitment rates | 70.6% consented and enrolled |
| Retention rates | 83.3% completed both pre‐post study assessments |
| Acceptability | |
| Face‐to‐face sessions completion rates | Of the 20 dyads that completed post‐intervention assessment, 17 dyads completed all three sessions, yielding an 85% completion rate. |
| Online intervention engagement | The Dyadic Learning Sessions module, with 29 web pages, was viewed approximately 609 times, with an average of 21 views per page. Twenty‐six pages in the Healthy Information module were read approximately 298 times. |
| Post‐intervention programme evaluation questionnaire† | With mean acceptability ratings all greater than 5.2 on a 7‐point scale and favourable comments (see Table 1a and b, below, for detailed information) |
| 1a: Post‐intervention acceptability items among patients and their spousal caregivers (n = 20 patient‐spousal dyads) | ||
|---|---|---|
| Category |
Patient M (SD) |
Spousal caregiver M (SD) |
| Usefulness | ||
| The programme content is useful | 5.5 (1.2) | 5.8 (0.8) |
| The online platform is convenient for me and saves me time when I use it | 5.2 (1.0) | 5.4 (0.8) |
| The online platform includes important information that I want | 6.0 (0.7) | 5.9 (0.7) |
| Ease of use | ||
| The online platform is easy to use | 5.6 (0.9) | 5.8 (0.8) |
| I found what I was looking for quickly and easily | 5.5 (0.8) | 5.7 (0.5) |
| The online content is easy to understand and follow | 5.6 (0.9) | 5.6 (0.7) |
| Satisfaction | ||
| I am satisfied with the intervention content | 5.3 (0.6) | 5.7 (0.6) |
| I am satisfied with the delivery format (combination of online and in‐person delivery) | 5.4 (0.7) | 5.6 (0.7) |
| I would recommend it to someone else | 5.6 (0.6) | 6.0 (0.6) |
| The programme has | ||
| Increased my knowledge of colorectal cancer | 6.0 (0.7) | 6.0 (0.7) |
| Improved my ability to cope with cancer with my partner together | 5.7 (0.8) | 6.1 (0.8) |
| 1b: Detailed responses to the open‐ended question | ||
| There were a total of 11 CRC patients and 12 spousal caregivers who responded to the question. Most of the responses were positive (11/11 and 11/12 respectively). Their favourable comments and suggestions for further improvement of the programme are summarised below: | ||
|
Favourable comments:
| ||
|
Suggestions for improvement:
| ||
Note: Postintervention programme evaluation questionnaire†: the questionnaire was adapted from the existing USE scale (AM. L. Measuring usability with the USE questionnaire. Usability Interface. 2001;8(2):3–6). It evaluated the programme in terms of usefulness, ease of use, and satisfaction on a 7‐point Likert scale ranging from “1” (“Strongly disagree”) to “7” (“Strongly agree”). In addition, an open‐ended question was added to collect any thoughts or feelings regarding use of the programme or intervention improvement suggestions.
Further programme refinement: The present report supported the programme's feasibility and acceptability, but some limitations remain, and should be addressed in future research. Apart from further refining the related content according to participant suggestions, for example updating information more frequently, and preparing more pictures or videos for greater ease of use, we may try to improve the study design, for example using RCT, recruiting adequate numbers of participants and extending the follow‐up period.
Abbreviations: M, mean; SD, standard deviation.
In terms of primary outcomes, small‐to‐medium improvements in self‐efficacy were found in CRC patients (d = 0.36) and spousal caregivers alike (d = 0.37). Additionally, improvements were found in self‐efficacy, with 55% of patients and 60% of partners showing a clinically important difference postintervention. Overall small‐to‐medium improvements were also found across all other outcome measures for CRC patients (d = 0.12–0.65) and spousal caregivers (d = 0.004–0.37) (Table S3). Approximately 30%‐55% of patients and 20%–60% of spouses reported clinically important differences across other outcome measures postintervention (Table S4).
5. DISCUSSION
The findings largely supported the feasibility of the hybrid approach. The recruitment rate (70.6%) was excellent, higher than typical rates for most cancer couples‐based interventions, but somewhat lower than that of the 4Cs programme (86.7%). Retention and completion rates were good (83.3% and 85%, respectively), slightly higher than the 4Cs programme retention rate (78.6%) (Li et al., 2015), which could be attributed to the shortened number of face‐to‐face sessions (three vs. six) and the attraction of the online intervention (e.g. flexible and diverse presentation form). Nevertheless, the somewhat lower recruitment rate and higher retention rate of the 4Cs: CRC programme may indicate the potential of blended delivery to enhance intervention adherence, supporting the programme's feasibility and acceptability. This may also point to a need for more publicity, to increase the recruitment rate.
Further, patients and their partners praised the programme for its usefulness and ease of use. Their comments also indicated that the programme delivery mode might be acceptable, but cannot be generalized to a controlled trial, since this is a single‐arm design, and all participants received the study intervention.
The intervention's preliminary effect showed generally small‐to‐medium effect sizes for CRC patients and their spousal caregivers in multiple dyadic domains, similar to our prior 4Cs programme(Li et al., 2015). However, preliminary efficacy is necessarily viewed with caution due to the small sample size.
Although testing in a larger‐scale study is warranted, our study findings might indicate that integrated intervention as a novel delivery approach offers the following potential advantages. First, it combines the advantages of online and in‐person delivery and requires less in‐person contact than single face‐to‐face sessions, making more comprehensive, accessible, minimally intensive psychological interventions possible. Second, the comprehensive strategy adjusts to the unique preferences of each couple, which may to a certain extent enhance intervention adherence.
5.1. Limitations
First, this study lacked a control group, so we cannot conclusively attribute the improved results to the intervention. In addition, the small sample size limits the potential to make inferences about study variables. The pre–post‐study design, with no follow‐up, restricts exploration of the long‐term programme's efficacy. Finally, the study was implemented in China and its findings may not be generalizable to a broader population.
5.2. Implications for practice
Our findings not only encourage other researchers to best integrate the advantages of the Internet and traditional delivery to support CRC couples, but also to faciliate clinicians in transforming the 4Cs: CRC programme into standard clinical service for CRC couples, allowing them to better adjust to living with cancer.
6. CONCLUSION
The 4Cs: CRC programme is a unique, important and promising new approach that appears to be feasible, acceptable and preliminarily effective among Chinese CRC couples. Following participants’ suggestions for improvement (Table 1), testing in a larger‐scale study is warranted.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
Supporting information
Table S1‐S4
ACKNOWLEDGEMENTS
The authors thank all patient‐partner dyads who participated in this study and share their experience.
Luo X, Li J, Cao Q, et al. A feasibility study of an integrated couples‐based supportive programme for Chinese couples living with colorectal cancer. Nurs Open.2021;8:920–926. 10.1002/nop2.700
Xingjuan LUO and Jieyu LI contributed equally to this work.
Center for Open Science ‐ https://osf.io/rfxz3/
Funding information
Financial support of this study was provided by the National Natural Science Foundation of China (No. 81773297) and General Project of Wuxi Health Commission (MS201832, MS201916).
Contributor Information
Xingjuan Luo, Email: 1014857395@qq.com, Email: liqp@163.com.
Jie Zhao, Email: 1014857395@qq.com, Email: liqp@163.com.
DATA AVAILABILITY STATEMENT
The dataset(s) supporting the conclusions of this article is (are) available and will be provided on request.
REFERENCES
- Badr, H. , & Krebs, P. (2013). A systematic review and meta‐analysis of psychosocial interventions for couples coping with cancer. Psychooncology, 22(8), 1688–1704. 10.1002/pon.3200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray, F. , Ferlay, J. , Soerjomataram, I. , Siegel, R. L. , Torre, L. A. , & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 68(6), 394–424. 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- Heitzmann, C. A. , Merluzzi, T. V. , Jean‐Pierre, P. , Roscoe, J. A. , Kirsh, K. L. , & Passik, S. D. (2011). Assessing self‐efficacy for coping with cancer: Development and psychometric analysis of the brief version of the Cancer Behavior Inventory (CBI‐B). Psychooncology, 20(3), 302–312. 10.1002/pon.1735 [DOI] [PubMed] [Google Scholar]
- Kayser, K. , Acquati, C. , Reese, J. B. , Mark, K. , Wittmann, D. , & Karam, E. (2018). A systematic review of dyadic studies examining relationship quality in couples facing colorectal cancer together. Psychooncology, 27(1), 13–21. 10.1002/pon.4339 [DOI] [PubMed] [Google Scholar]
- Li, Q. , Lin, Y. , Chen, Y. , & Loke, A. Y. (2018). Mutual support and challenges among Chinese couples living with colorectal cancer: A qualitative study. Cancer Nursing, 41(5), E50–E60. 10.1097/ncc.0000000000000553 [DOI] [PubMed] [Google Scholar]
- Li, Q. , & Loke, A. Y. (2015). A preliminary conceptual framework for cancer couple dyads: Live with love. Cancer Nursing, 38(2), E27–E36. 10.1097/ncc.0000000000000148 [DOI] [PubMed] [Google Scholar]
- Li, Q. , Xu, Y. , Zhou, H. , & Loke, A. Y. (2015). A couple‐based complex intervention for Chinese spousal caregivers and their partners with advanced cancer: An intervention study. Psychooncology, 24(11), 1423–1431. 10.1002/pon.3809 [DOI] [PubMed] [Google Scholar]
- Luo, X. , Gao, L. , Li, J. , Lin, Y. , Zhao, J. , & Li, Q. (2020). A critical literature review of dyadic web‐based interventions to support cancer patients and their caregivers and directions for future research. Psychooncology, 29(1), 38–48. 10.1002/pon.5278 [DOI] [PubMed] [Google Scholar]
- Portney, L. G. & Watkins, M. P. (2009). Foundations of clinical research: Applications to practice, Vol. 892 Upper Saddle River, NJ: Pearson/Prentice Hall. [Google Scholar]
- Reese, J. B. , Porter, L. S. , Regan, K. R. , Keefe, F. J. , Azad, N. S. , Diaz, L. A. , Herman, J. M. , & Haythornthwaite, J. A. (2014). A randomized pilot trial of a telephone‐based couples intervention for physical intimacy and sexual concerns in colorectal cancer. Psychooncology, 23(9), 1005–1013. 10.1002/pon.3508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regan, T. W. , Lambert, S. D. , Girgis, A. , Kelly, B. , Kayser, K. , & Turner, J. (2012). Do couple‐based interventions make a difference for couples affected by cancer?: A systematic review. BMC Cancer, 12, 279 10.1186/1471-2407-12-279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traa, M. J. , Braeken, J. , De Vries, J. , Roukema, J. A. , Orsini, R. G. , & Den Oudsten, B. L. (2015). Evaluating quality of life and response shift from a couple‐based perspective: A study among patients with colorectal cancer and their partners. Quality of Life Research, 24(6), 1431–1441. 10.1007/s11136-014-0872-8 [DOI] [PubMed] [Google Scholar]
- Traa, M. J. , Braeken, J. , De Vries, J. , Roukema, J. A. , Slooter, G. D. , Crolla, R. M. P. H. , Borremans, M. P. M. , & Den Oudsten, B. L. (2015). Sexual, marital and general life functioning in couples coping with colorectal cancer: A dyadic study across time. Psychooncology, 24(9), 1181–1188. 10.1002/pon.3801 [DOI] [PubMed] [Google Scholar]
- Traa, M. J. , De Vries, J. , Roukema, J. A. , & Den Oudsten, B. L. (2016). The association between patient's and partner's fatigue in couples coping with colorectal cancer: A longitudinal study. Supportive Care in Cancer, 24(10), 4113–4121. 10.1007/s00520-016-3226-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, L. , Cao, F. , Zhang, G. , Shi, L. , Chen, S. , Zhang, Z. , Zhi, W. , & Ma, T. (2019). Trends in and Predictions of Colorectal Cancer Incidence and Mortality in China From 1990 to 2025. Frontiers in Oncology, 9, 98 10.3389/fonc.2019.00098 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1‐S4
Data Availability Statement
The dataset(s) supporting the conclusions of this article is (are) available and will be provided on request.


