A brief, primary care-based web intervention shows potential to help adults with obesity take a first step in engaging in evidence-based behavioral weight loss treatment.
Keywords: Core functions, Form, Complex health intervention, Core components, Program adaptation, Qualitative research, Theory-based research, Planned Adaptation Model
Abstract
Adaptation of existing evidence-based interventions (EBIs) to improve their fit in new contexts is common. A critical first step in adaptation is to identify core functions (purposes) and forms (activities) of EBIs. Core functions should not be adapted as they are what account for the efficacy of EBIs. Despite their importance, core functions are rarely identified by EBI developers; methods for identifying them post hoc are lacking.
We present a case study of theory-based methods for identifying core functions and forms post hoc. We developed these methods as the first step in a larger effort to adapt an existing EBI to improve the timeliness of referrals to hospice to a new patient population and care setting. Our methods were rooted in the Planned Adaptation Model (PAM). Through our case study, we developed six steps for identifying core functions and forms, as well as accompanying tools and methods. Our case study further operationalized PAM in several ways. Where PAM offered guiding tenets for identifying core functions and forms (review existing EBI materials, conduct primary data collection, and identify the theory of change), we produced specific tools (interview guides and codebooks) and methods (sampling approaches and analytic methods). Our case study extended PAM with the addition of two steps in the process of identifying core functions and forms: (a) identifying the usual care pathway, including barriers to the outcome of interest encountered in usual care, and (b) mapping EBI core functions onto an extant theory. Identifying core functions and forms is a critical first step in the adaptation process to ensure adaptations do not inadvertently compromise the efficacy or effectiveness of the EBI by compromising core functions. Our case study presents step-by-step methods that could be used by researchers or practitioners to identify core functions and forms post hoc.
Implications.
Practice: These methods and tools can be used in the field to identify core functions and forms of existing evidence-based interventions (EBIs) to promote adaptation that preserves the effectiveness of EBIs.
Policy: Policymakers who want to ensure that adaptation efforts preserve interventions’ effectiveness and programs could consider further testing and refinement of these methods to identify core functions and forms.
Research: Future research is needed to thoroughly test and expand upon these methods for use in broad contexts.
BACKGROUND
Reproducing the level of effectiveness demonstrated in trials is critical when moving an evidence-based intervention (EBI) into practice. Historically, fidelity to EBI protocol was considered paramount for reproducing effectiveness; adaptations were viewed as threats to effectiveness [1–5]. Increasingly, researchers and practitioners recognize that adaptations can promote effectiveness by improving fit between the EBI and new contexts (e.g., new organizations and patient populations) [6–8]. In this view, attention shifts from preserving perfect fidelity to making adaptations that improve fit between EBIs and context [1, 7, 9–13]. To achieve this goal, specification of an EBI’s core functions and forms is critical as core functions are the underlying principles that make the EBI effective and, thus, should not be adapted. Despite their importance, core functions are rarely specified by intervention developers as part of intervention testing [14]. Moreover, methods for identifying core functions post hoc are lacking. Thus, in this paper, we identified core functions and forms of an existing EBI and present a case study of the methods we used to identify core functions and forms of the EBI post hoc.
In the Background, we describe the intervention and the concepts of core functions and forms. In the Methods section, we describe the tools that we developed to identify core functions and forms so that others can use and refine them. Given that most EBI developers and evaluators do not clearly identify core functions and forms in publications or EBI materials [14], the Results section presents the core functions and forms along with other related outputs (usual care pathway and theory of change) for our EBI. Although specific to our case study, our results can serve as a model for how researchers and practitioners could report core functions and forms. In the Discussion, we offer recommendations for future use based on lessons learned from this case study, explore in more detail the applications of core functions and forms in practice, and discuss how we used core functions and forms identified in this research to adapt our EBI.
Intervention
Hospice care offers proven benefits to terminally ill patients, including improved quality of life and decreased physical and psychosocial symptom burden [15, 16]. Despite this evidence, fewer than half of Medicare decedents die on hospice services [17]. Furthermore, the median length of stay for those who do use hospice is 24 days, falling short of the expert-recommended 3 months [17–19]. A primary reason for underutilization is delayed referrals from the physician who makes the terminal diagnosis; physicians may be hesitant to refer seriously ill patients to hospice for fear of bringing up hospice “too early,” lack of training in compassionate discussion of bad news, and/or difficulty in accurately predicting a prognosis of 6 months or less [20–23].
Some evidence, however, demonstrates effective methods for overcoming these barriers. Casarett et al. developed an intervention for nursing home residents to improve physician referrals to hospice [24]. The Casarett et al. intervention (herein “Casarett EBI”) used a three-question screening tool to elicit nursing home residents’ care goals, preferences, and needs; responses to these questions were used to identify patients potentially appropriate for hospice. If a patient screened positive, a referral to hospice was initiated. The intervention improved hospice referral and election rates by 19 percentage points in a randomized controlled trial (RCT) [24]. Although the intervention was found to be efficacious, it was limited in reach because it was developed and tested only for nursing home residents. Nursing home residents comprise 19% of U.S. hospice patients compared to the 51% of hospice patients who receive hospice services in home- and community-based settings [25]. Thus, to improve its reach and impact, we adapted the Casarett EBI for use in home health.
Core functions and forms
As a first step in adapting the Casarett EBI, we sought to identify the core functions and forms of the intervention. As noted in the Patient-Centered Outcomes Research Institute’s (PCORI’s) standards for the study of complex interventions [26] and elsewhere [27, 28], core functions relate to the underlying mechanisms of change that make an intervention effective. They articulate the purpose intervention activities serve and how the intervention’s activities work to produce desired outcomes. As they describe how changes in outcomes are being achieved, core functions are closely related to an intervention’s theory of change [14, 29, 30].
Core functions are distinguished from forms, which are the specific intervention activities that carry out core functions. In short, core functions explain the purpose of intervention components (why it matters and how it produces change), while form denotes activities (who is doing what, when, where, and how; note that although other research in the field uses the term “core components” [the essential EBI components that make an EBI effective and should not be adapted] and “adaptable periphery” [components that can be adapted without compromising effectiveness because they are not necessary to produce desired outcomes] [15–17], we have used the terms “core functions” and “forms” to align with recent PCORI methodology standards for the study complex interventions [12], as well as recent publications which advocate for use of core functions and forms instead of core components and adaptable periphery [13]). For example, in considering an intervention that is a reminder to a clinician to complete a specific care process, one core function of the intervention could be that the reminder is not easily dismissable/ignorable, the purpose of which is to ensure that the reminder is seen and acknowledged by the clinician. To fulfill this core function, a form could be that the electronic health record requires the clinician to acknowledge the reminder and enter meaningful data before the reminder can be closed and the clinician can move on to the next step in the clinical workflow.
Clearly defining core functions and forms is a critical first step in the adaptation process as core functions should not be adapted since changing or removing them challenges the integrity of the intervention. On the other hand, forms can be adapted to an individual setting or context as multiple forms may serve a single function [27]. In the example above, “not easily dismissable/ignorable” may take any number of forms given a specific organization’s context. For example, an organization that uses paper-based medical records will have a different form to fulfill the function of “not easily dismissable/ignorable” than an organization using an electronic health record. For a paper-based organization, the form chosen could be brightly colored insert sheets at the front of each paper medical record; although different than the electronic health record form, it still fulfills the same core function.
Adaptation at the form level allows flexibility for organizations to tailor an intervention to their context and, as long as the adapted form still fulfills the core function, such adaptations should improve intervention-context fit while minimizing the risk of compromising the effectiveness of the intervention. In this sense, knowing core functions and forms is necessary but insufficient for adaptation. One must also map forms to core functions to know which forms are related to which core functions [27]. This allows researchers and practitioners to ensure that any adaptations to form are still fulfilling the related core function and ensures that there are forms to fulfill every core function.
In research, forms are often clearly defined through intervention protocols and manuals. Less often specified are core functions of interventions [14]. Less common still is explicit mapping of forms to core functions to show which intervention forms (activities) are related to which core functions. This gap in the literature has resulted in unclear guidance on how best to identify core functions and forms and how to report and use them in adaptation.
METHODS
Theoretical framework
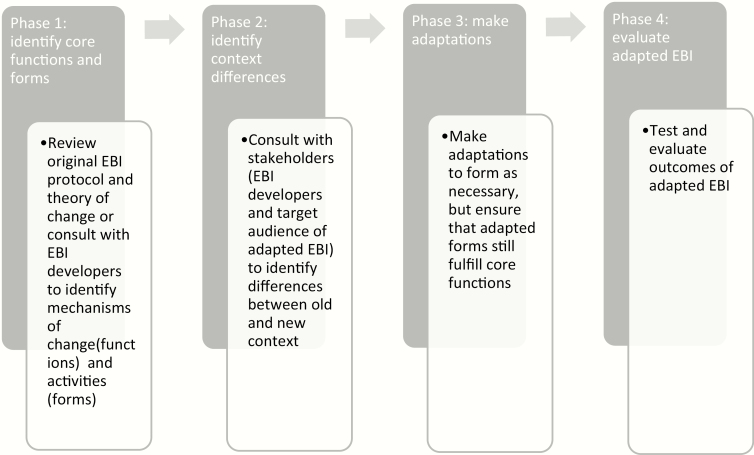
Our overall approach was based on the Planned Adaptation Model (PAM) [31]. We selected PAM because of its high level of specificity regarding the adaptation process. PAM includes four phases in the adaptation process (Fig. 1); Phase 1 focuses on identifying core forms and functions by specifying the theory of change, which is closely related to core functions and specifying all activities of the EBI (i.e., forms). We used the guiding principles from PAM to identify the theory of change and activities; we then used data on the theory of change and activities to identify core functions and forms. Finally, we engaged in a mapping process to map forms to core functions.
Fig 1.
Planned adaptation model.
Procedures
The six steps below comprise the approach we took to identify core functions and forms of the Casarett EBI. Researchers and practitioners may find these methods from our case study helpful in identifying core functions and forms of other interventions.
Step 1: review existing materials
The first step was to review existing EBI materials to determine whether core functions and forms or the theory of change had already been specified. To complete this step, we searched for available published and gray literature on the Casarett EBI. We identified one existing public data source: the publication of the RCT that originally tested the Casarett EBI [24]. This publication did not include a clear description of the core functions or the theory of change. We contacted the research team for a copy of the intervention protocol, which was not publicly available. The intervention protocol listed all forms (activities) but did not map them back to core functions as the core functions had not been specified. We reviewed existing materials (publication and protocol) to guide the development of the semistructured interview guide that we used in Step 2.
Step 2: develop semistructured interview guide
Because existing materials for the Casarett EBI did not specify the core functions and their related forms, we conducted semistructured interviews with those involved in the development and initial testing of the Casarett EBI to identify its core functions and forms. Our interview guide covered four main topics: (a) usual care pathway, including barriers to the outcome of interest, (b) EBI theory of change, (c) forms (activities) of the EBI, and (d) core functions of the EBI. Topics 2–4 were recommended by PAM; we included Topic 1 as an icebreaker to help participants feel comfortable and jog their memory about the context for the intervention. That said, Topic 1 ultimately proved crucial to analysis (see Results).
Across all topics, we phrased questions in layperson’s terms within the context of the EBI. For example, instead of asking “what are the moderators in this intervention’s causal pathway?” we asked, “was there anything about the nursing home setting that may have boosted (or limited) the success of the intervention?” We employed this strategy because our interview participants were primarily clinical researchers and practitioners who were unfamiliar with theory-specific terminology. We also included frequent probes throughout the interview guide to elicit the principles underlying the theory of change and core functions. For example, if a respondent stated, “the intervention made clinicians feel more comfortable discussing hospice,” we probed for reasons why to better understand the theory and purpose behind the EBI. Example interview questions for each interview topic are listed in Table 1. Supplementary Additional File 1 contains an updated interview guide, which we refined after conducting our interviews. Because the RCT of the Casarett EBI occurred ~10 years earlier, we sent a one-page description of the intervention based on the publication [24] to interview participants prior to interviews to refresh their memory.
Table 1.
Example interview questions for each major topic area
| Topic | Selected example interview questions |
|---|---|
| Topic 1: usual care pathway, including barriers to outcome of interest | • Irrespective of the intervention, based on your experience, can you describe barriers to hospice referral you often see or encounter in practice? |
| Topic 2: evidence-based intervention (EBI) theory of change | • How does the intervention help fix the barriers you described (if at all)? • What was driving the success of the intervention? |
| Topic 3: EBI activities (forms) | • Who were the study staff that carried out the intervention activities? Did they have any qualifications required to perform these activities (e.g., prior experience with nursing home patients or hospice)? • Where were the screening conversations held? (via phone? In person at the nursing home?) • What was the physician’s role beyond certifying the prognosis of 6 months or less and authorizing a hospice referral, if anything? |
| Topic 4: core functions | • Which EBI activities contributed most to the success of the intervention? Probe: what about it was essential—e.g., who is conducting the activity; mode of activity (in person vs. written)? • In an adapted intervention, which activities/principles would you maintain at all costs and why? |
Step 3: recruit interview participants
Our sampling frame included all six authors on the Casarett EBI RCT publication [10]. These authors represented a variety of roles, including the lead developer of the intervention, members of the RCT study team (e.g., research assistant and statistician), and staff from the clinical sites who participated in the RCT.
Step 4: conduct interviews
We conducted interviews during a 3 month period between April and June 2017. Interviews were conducted by the lead author (A.K.) via telephone or in person. All interviews were between 20 and 60 min.
Step 5: analyze interview data
Interviews were audio-recorded, transcribed verbatim, and analyzed using template analysis, which allowed us to identify a priori and emergent themes [32]. We developed the initial codebook based on a priori themes, which included the key topics and subtopics from the interview guide (Table 1). We used the literature [30, 31, 33] to develop the definitions of key constructs in our codebook. Using interview data, we developed coding rules to further operationalize and distinguish among each code. Select coding definitions and examples are presented in Table 2; the final codebook is presented in Supplementary Additional File 2. Two authors (A.K. and E.H.) coded all interviews; following our initial independent coding, A.K. and E.H. reviewed coding results and discussed discrepancies until consensus was reached. After coding, three authors (A.K., S.B., and E.H.) interpreted coded data to develop themes and final outputs.
Table 2.
Theory of change for Casarett evidence-based intervention (EBI)
| Component of theory of change | Results |
|---|---|
| Primary causal pathway | • “Don’t lead the conversation by mentioning the “h” word [hospice], end the conversation by talking about hospice as a solution to self-identified needs”*: Reframing of the conversation from one about death and hospice to be about patient’s needs, goals, and preferences. For patients who “screened positive,” hospice was presented as a solution to the patient’s specific needs, goals, and preferences that they had expressed during the screening. |
| Secondary causal pathway | • “It allows for the potential to identify people who need hospice sooner…by…having these conversations about care goals, preferences, and needs without there being a precipitating event”*: Integrating the reframed conversation into usual care via standardized patient eligibility criteria for having the conversation and standardized timing of the conversation lessens the tendency to wait for a precipitating event (e.g., decline in clinical status and change in prognosis) to identify someone as needing hospice, improving timeliness of referrals to hospice. |
*Quote from semistructured interviews.
Overall, we conducted our analysis in phases—we coded data for each topic in the interview (i.e., usual care pathway, EBI theory of change, EBI activities, and core functions and forms). We then interpreted coded data to develop several outputs. We coded data for the usual care pathway first, followed by the theory of change, forms (activities), and core functions. Once all data were coded, we interpreted coded data to identify the usual care pathway, EBI theory of change, and core functions. The final step in our interpretation process was to map forms to core functions.
Our strategy for identifying core functions was to review the data coded as the theory of change and core functions to look for the mechanisms of change behind the intervention and the purpose intervention activities served. With core functions specified, we then reviewed the data coded as EBI forms (activities) and engaged in group discussion to map forms to the core functions they fulfilled. To complete this mapping process, three authors (A.K., E.H., and S.B.) discussed as a group the following question: Does this form (activity) operationalize one of the core functions? If so, the form (activity) was considered related to a core function; if not, it was considered unrelated to a core function.
Step 6: map core functions onto extant theory from the literature
Because the Casarett EBI was not developed using a theory-based approach, we developed our own theory of change based on a qualitative approach described in Steps 1–5. From this theory of change, we were able to identify core functions and forms of the Casarett EBI. However, given that the Casarett EBI was not theory based and the core functions we identified were identified post hoc via a qualitative approach and not verified empirically, we added an additional step to PAM to help validate the theory of change and core functions we identified. To help validate the core functions, we searched for an existing theory that aligned with the Casarett EBI core functions. If our core functions were supported by an existing theory, this could improve our confidence in the core functions as valid mechanisms of change. This additional step extends the utility of PAM for interventions that lack a theory base; for EBIs that are theory based, this additional step may be unnecessary.
To identify a related theory of change, we used the following process: first, we considered the level of change of the intervention (e.g., individual, group and team, or organizational level) and the type of change (e.g., change in habit, cognitive perception, or health behavior) to narrow down a field for the theory search. Based on our EBI (individual-level intervention designed to change the cognitive perception of a health-related conversation), we chose to search for theories within psychology, a field that seeks to understand cognitive phenomena at the individual level. Within the selected general field, we then searched for theories with similar constructs and levers of change to the core functions we had identified.
RESULTS
We interviewed five of the six original research team members; we analyzed interview data using the process described above, and the main outputs from our analysis were: (a) usual care pathway, including barriers to change, (b) EBI theory of change, (c) description of the core functions and forms, and (d) mapping little-t theory of change onto extant Big-T theory of change. We present each of these outputs for our case example to serve as a model for how these types of results could be presented.
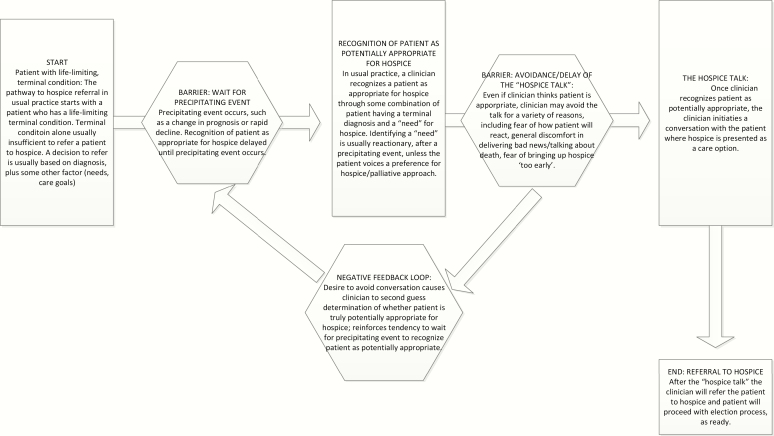
Output 1: usual care pathway, including barriers
For the usual care pathway, we developed a visual (Fig. 2) and a text description. By outlining the barriers to change that a well-designed intervention should address, the usual care pathway provided a clear foil for the EBI theory of change and core functions and forms. In this sense, for EBIs that are not theory based, outlining the usual care pathway can help in developing a theory of change as they show the barriers in usual care/practice that the intervention should be working to address. For our context, we identified two main barriers to hospice referral that lie on the usual care pathway: (a) waiting for a precipitating event before discussing hospice and (b) discomfort with the “hospice talk” (broaching hospice as a potential care option with the patient). These two barriers (represented by hexagons in Fig. 2) were interrelated, causing a negative feedback loop (also represented by a hexagon in Fig. 2) that further exacerbates delays in hospice referral. In our theory of change, we were able to show how the EBI addressed these barriers and negative feedback loop.
Fig 2.
Usual care pathway visualization.
Output 2: EBI theory of change
For the theory of change, we developed a text description for the primary and secondary causal pathways in the theory of change (Table 2). In short, the Casarett EBI’s causal pathways removed the barriers identified in the usual care pathway by reframing the conversation about hospice entirely. The Casarett EBI shifted the conversation from one about hospice to one about care goals, needs, and preferences more generally. Clinicians felt equipped and comfortable discussing care goals, needs, and preferences and, thus, no longer avoided or delayed these conversations. Additionally, the Casarett EBI screening questions were built into regular clinical workflows and asked of all eligible patients. This standardized the timing of the conversation, eliminating the second barrier encountered in usual care—reliance on a precipitating event to recognize a patient as potentially appropriate for hospice.
Output 3: description of core functions and forms
Ultimately, we found that the causal pathways from the theory of change formed core functions of the Casarett EBI. With the core functions outlined, we then delineated which EBI forms (activities) fulfilled which core functions (Table 3). Three authors (A.K., E.H., and S.B.) made this determination by engaging in group discussion to evaluate each activity to determine whether it fulfilled a core function.
Table 3.
Detailed description of core functions and forms
| Core function (purpose) | Related forms (activities) | Notes for future adaptation |
|---|---|---|
| Core Function 1: Do not lead the conversation by mentioning the “h” word [hospice], start the conversation by discussing care goals, needs, and preferences. End the conversation by talking about hospice as a solution to self-identified needs and goals. Purpose this serves: Per the Casarett evidence-based intervention (EBI) theory of change, the driving causal mechanism is the reframing of the conversation. Thus, the purpose this core function serves is that the reframing shifts the conversation to a topic the clinician feels comfortable discussing and will be less likely to delay/avoid. | Activities related to the framing of the conversation: In the Casarett EBI, the conversation was introduced as one about patient care goals, needs, and preferences and the exact form (script/wording) was detailed in the intervention protocol. | Because the core function is the reframing of the conversation, the exact script introducing the screening conversation could be adapted as long as the adaptations still preserve the related core function, which was the fact that you are starting by discussing a “neutral” topic, other than hospice/end-of-life care. Other aspects of form that were unrelated to this core function include the screening questions themselves, as well as who is asking the questions. As unrelated forms, these activities could also be adapted without the need to ensure that any adaptations to form are fulfilling a core function. |
| Core Function 2: Standardize the timing of the conversation, as well as the eligible patient population for the conversation. Purpose this serves: Per the Casarett EBI theory of change, standardizing the timing and target population for the conversation eliminates the need to rely on clinical judgment and a precipitating event, thus improving the timing of the conversation and subsequent referrals to hospice. Thus, this core function serves the purpose of removing the need to rely on clinical judgment alone, decreasing the risk for delaying the conversation. | In the Casarett EBI intervention, eligible patients included all nursing home residents assigned to the treatment group who were not already on hospice. Timing of the conversation was to happen after the mailer was sent to the patient’s surrogate. | The form (exact timing and exact patient eligibility criteria) can be adapted, provided the core function is still met (that there are some clearly defined parameters around who is eligible and when the conversations should occur so that you are not relying entirely on clinical judgment to decide when to initiate the screening conversation and with whom). Unrelated forms include how eligible patients were identified and how follow-up and referrals to hospice were initiated. |
As noted in Table 3, we identified two core functions of the Casarett EBI. These core functions were directly derived from the causal pathways in the theory of change and included how the conversation is introduced/framed (framed as a conversation about care goals, needs, and preferences, not a conversation about hospice, which made the conversation something clinicians felt comfortable discussing and would not delay) and standardizing the conversation in some way (i.e., clearly specifying an eligible patient population and timeframe for initiating the conversation to avoid reliance on clinical judgment and a precipitating event, which delays the conversation). Because the Core Function 1 was about the frame of the conversation (not who was asking the questions or whether questions were asked in person or via phone), we determined that the forms (activities) related to Core Function 1 were those related to how the conversation was introduced, which was detailed in the script of the intervention protocol. Because Core Function 2 was about the act of standardizing the timing of the conversation and patient eligibility criteria, we determined that the related forms (activities) were how the conversation was standardized (i.e., patient eligibility criteria, which for the Casarett EBI was all nursing home residents randomized to the treatment group who met all other study inclusion criteria) and the timing of the screening conversation (which for the Casarett EBI was after letters were sent to each resident’s surrogate notifying them of eligibility for the study). All other forms (activities) detailed in the Casarett EBI protocol were considered forms unrelated to any of the two core functions (e.g., who asked the screening questions and how, the exact wording of the screening questions, and internal workflow for how physicians were contacted to authorize referral to hospice).
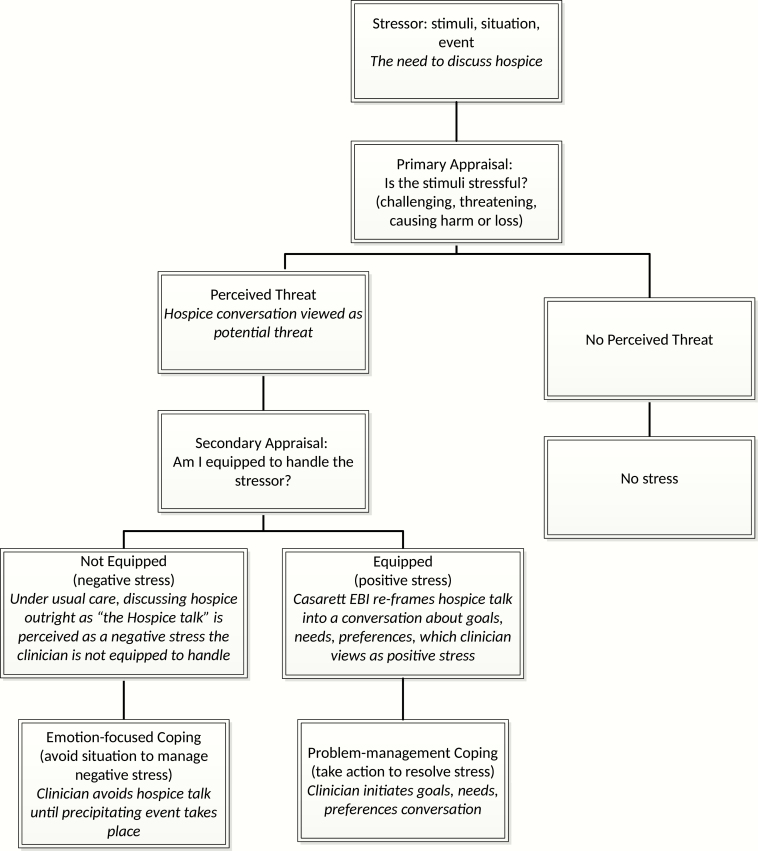
Output 4: mapping EBI core functions onto existing theory
We were able to successfully map constructs from our core functions onto an existing theory: Lazarus’ Transactional Model of Stress and Coping [34–36] (see Fig. 3). Ultimately, the notion that the primary causal pathway/core function behind the intervention was that it reframed the conversation as something clinicians felt comfortable discussing was supported by Lazarus’s theory, which states that when individuals feel they are equipped to handle a stressor, they take action instead of avoiding the stressor. We considered a range of other individual psychology theories [37–39] and ultimately selected Lazarus’s theory because of its congruence with our core functions. Moreover, Lazarus’ theory has been validated in several studies, increasing our confidence that our core functions are legitimate [35, 36, 40–43]. Although outputs from the mapping exercise are not used in the adaptation process, we believe that they are important outputs for EBIs that are not theory based as they help validate core functions by aligning them with existing theory.
Fig 3.
Mapping evidence-based intervention core functions onto existing theory.
DISCUSSION
Methods for identifying core components
This paper fills an important gap in the current literature by providing as a case study a step-by-step guide—including methods, tools, and recommendations—for identifying core functions and forms post hoc. Although PAM provided a general checklist of what is needed to identify core functions and forms (e.g., develop the theory of change and establish intervention activities) and suggested some overall methodological approaches (e.g., primary data collection from intervention developers), specific tools were lacking. The methods we developed comprise six concrete steps for identifying core functions and forms, and each step is accompanied by specific tools (e.g., interview guides and codebooks). Although our methods may not address nuances of all situations (e.g., situations where an EBI has been tested multiple times and researchers gather conflicting information on what might comprise core functions and forms), we believe they offer a starting point to contribute to a growing field of research on identifying core functions and forms of interventions. Through our case study, we were able to develop several preliminary recommendations for applying these methods and tools, both relating to data collection and analysis (see Table 4). As researchers and practitioners apply these methods in the field in the context of other interventions, we welcome refinement of both the methods and our preliminary recommendations.
Table 4.
Preliminary recommendations for identifying core functions and forms
| Steps | Recommendations |
|---|---|
| Step 1—search for and review existing materials | • Cast a wide net when searching for existing materials—do not limit your search to peer-reviewed literature. Relevant materials may be available as gray literature on program or funder websites. Personal communications with members of the evidence-based intervention (EBI) team are also potential sources of existing materials. • Even if core functions and theory of change are not specified in existing materials, existing materials can prove useful in other ways (i.e., to provide context for the intervention or guide development of primary data collection materials). |
| Step 2—develop semistructured interview guide | • Review existing materials to inform development of primary data collection materials. • Make sure questions are “participant friendly”: avoid jargon in questions, instead, provide definitions of terms and phrase questions in the context of your specific intervention. ◯ For example: Instead of “ what are the moderators of your intervention?” ask “were there aspects of xxx intervention (or xxx context) that boosted its effectiveness?” • Ask about barriers to the outcome of interest encountered in usual care: this can serve as a jumping off point for the rest of the interview, making it easier for participants to think about the theory of change and primary causal pathway. Information on barriers to change was critical in the analysis phase for specifying the theory of change. • Theory of change: make sure to probe on responses about theory of change. For example, if a participant says “I think the intervention works because it makes clinicians feel comfortable” probe as to why/how it makes clinicians feel comfortable. This will help clearly define the causal pathways. • Core functions: ask about core functions directly, after asking about EBI activities and the theory of change. As a lead-in to the questions focusing on core functions, provide an explanation of what core functions are and why identifying them is important. Again, our explanation avoided jargon and framed core functions as the “active ingredients” or “secret sauce” that drove the success of the intervention. We also found it helpful to ask several questions about core functions and probe often to ensure respondents were drilling down to “the core” of core functions. • Probe often to ensure you are drilling down to the underlying principles of why certain activities were important to the overall success of the intervention. • Consider developing supplemental materials (e.g., short descriptions of the intervention’s activities) to distribute to interview participants. |
| Step 3—recruit interview participants | • Try to maximize heterogeneity in your sampling frame and final sample by recruiting a variety of roles (research assistant, statistician, and lead developer) from a variety of perspectives (researcher vs. clinician). • Employ snowball sampling to maximize variation in perspectives, especially when one perspective (e.g., researcher and clinician) is overrepresented in the sampling frame. |
| Step 4—conduct interviews | • Use interviews or other bidirectional methods (e.g., focus groups) to allow for probing and follow-up questions |
| Step 5—analyze interview data | • Complete analysis in the following order: ◯ Usual care pathway (focusing on barriers to your outcome of interest encountered in usual care) ◯ Theory of change (primary and secondary causal pathways) ◯ Forms (activities) of the intervention ◯ Core functions ◯ Mapping forms (activities) to core functions • Identifying the barriers to outcome of interest encountered in usual care is critical to clearly elucidating the causal pathways in the theory of change. The barriers to change provide a clear “gap” that the primary and secondary causal pathways should (ideally) address • The primary/secondary causal pathways in your theory of change will likely form each core function. With each core function identified, then review all data coded as forms (activities) and discuss whether the activity is related to/operationalizes core function. If so, the activity is related to a core function. If not, it is unrelated. |
| Step 6—map theory of change onto extant theory from the literature | • Helpful in “validating” the “little-t” theory of change and resulting core functions • To identify a relevant Big-T theory, first consider the type of change your EBI is affecting (e.g., individual level and system level). You may have to explore extant, Big-T theories from other fields outside of implementation science based on the level of change and type of change. For example, person-level change in behavior may point to theories from health behavior or psychology; organizational-level change may point to theories from sociology or organizational theory. |
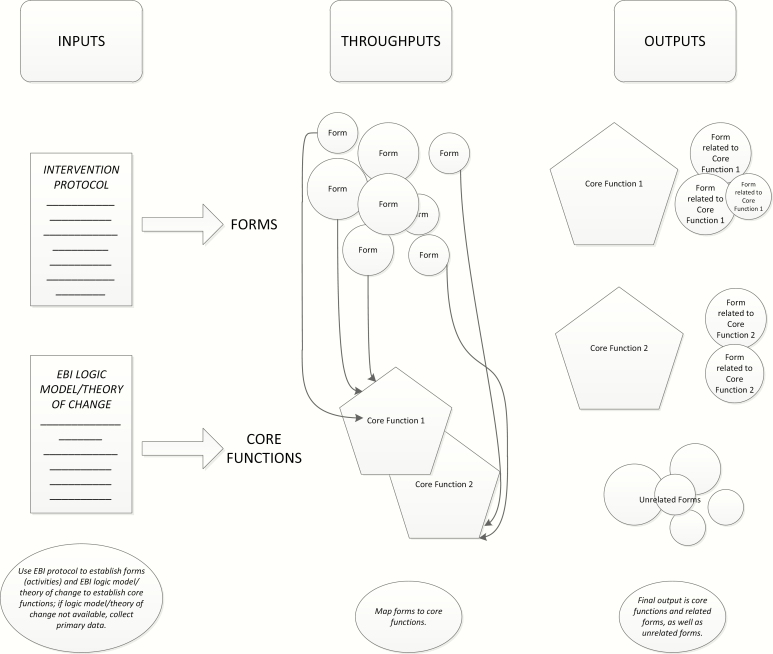
This paper explored the concept of core functions and forms, which is a recent departure in the field from “core components” (and related terms, such as “active ingredients”) and “adaptable periphery” [13, 14, 26, 27, 29, 30]. This paper is one of the first to explore and apply this new terminology in depth, including how to identify core functions and forms and apply them in adaptation process. Based on our case study, we developed a figure to conceptualize the inputs, throughputs, and outputs of identifying and reporting core functions and forms (Fig. 4). As detailed in Fig. 4, there were several important inputs we sought out to identify core functions and forms, including EBI protocols and EBI logic models and/or theories of change. These inputs fed directly into the specification of core functions and forms of EBIs. Once core functions and forms had been specified, we used a mapping process described elsewhere [27] to map forms to core functions to denote related and unrelated forms. Ultimately, this mapping process produced an output of core functions and related forms, as well as unrelated forms (other activities of the intervention that contribute to its functioning but are unrelated to any specific core function). In our example, related forms included the script in the Casarett EBI protocol that introduced/framed the conversation, as well as how the timing and eligible patient population were standardized (all nursing home residents not already on hospice; screening conversations should take place after mailers were sent). Unrelated forms included who was initiating the conversation, the mode of the conversation (in person vs. telephone), etc.
Fig 4.
Process for identifying and mapping core functions and forms.
More research is needed on related and unrelated forms to discern the reason behind unrelated forms, as well as whether unrelated forms are necessary activities for organizations to invest in as part of EBI implementation. For example, it could be that most interventions will have related and unrelated forms and that unrelated forms are activities that are needed for the intervention but do not fulfill a core function (similar to how pharmaceutical drugs contain active and inactive ingredients, both of which are necessary but only active ingredients have a therapeutic effect). On the other hand, unrelated forms may signal potential issues with the specification of core functions in that unrelated forms could point to “missing” core functions.
Relevance for adaptation
As noted in Fig. 1, clear specification of core functions and forms is a critical first step in the larger adaptation process. Clear specification of core functions and forms gives those who are adapting a clear sense of what is driving the success of the EBI. In this sense, clearly specified core functions serve as a checkpoint for adapting forms by allowing those adapting EBIs to answer the following question: does the proposed adapted form still fulfill its related core function? In our adaptation of the Casarett EBI, clear specification and mapping of core functions and forms were crucial in fulfilling subsequent steps in the adaptation process. After identifying core functions and forms as described here, our team then engaged in a stakeholder-driven process for identifying potential adaptations that would be needed to carry the intervention from the nursing home to the home health setting. Specifying core functions and delineating which forms fulfilled which functions allowed us flexibility in adapting forms without compromising core functions of the Casarett EBI. For example, major adaptations we made to the Casarett EBI included changing eligibility criteria to make the intervention more appropriate for the home health patient population (screened only high-risk or frail patients instead of all patients). Because the original Casarett EBI protocol was for an RCT where research study staff carried out all activities, we also had to adapt who was delivering the intervention so that it could be delivered by home health staff as part of usual care instead of research staff.
In deciding which adaptations to make, mapping of core functions and forms was crucial in our decision-making process. For each potential adaptation, we first discussed whether the adaptation was to a form that was related or unrelated to a core function. If we were adapting a related form, we then had to discuss whether the adapted form still fulfilled the related core function. If it did not, we had to rethink the adaptation to see if there was a way we could adapt form to improve fit but still maintain the fulfillment of the core function. Had we not outlined and mapped core functions and their related forms, we would not have had an in-depth understanding of our boundaries for what could be adapted without risk to the efficacy of the Casarett EBI.
Mapping core functions to forms also allowed us to leave our adapted EBI protocol flexible so that individual organizations wishing to implement the adapted Casarett EBI could further tailor the intervention to their contexts. We used core functions to set boundaries in the EBI protocol (see Supplementary Additional File 3). For example, in the adapted EBI protocol, we left patient eligibility criteria flexible in that we left it to individual home health organizations to decide exactly how they would define “frail or high-risk” patients that would be eligible for the screening. However, because we had identified core functions, we were able to set boundaries around adaptation to note that although home health organizations could choose how they would define frail or high risk (diagnosis, age, and EHR alerts), they should choose a standard definition for eligibility and not rely on clinical judgment alone to identify eligible patients.
Limitations
The primary limitation of our research is that our methods and tools were developed and tested in our single case study, potentially limiting the generalizability of our methods and resulting recommendations. However, given the paucity of specific methods and tools for identifying core components in the literature, we believe this paper can serve as the foundation for developing a compendium of tools for identifying core functions and forms. Another limitation was that our data collection was based on an intervention that was developed and tested over 10 years ago. To mitigate potential recall bias, we provided the one-page summary document of the Casarett EBI to all interview participants prior to the interview. If the participant had not read the one-page summary, we provided time at the start of each interview to review the material. Without prompting, participants stated this one-page document was a useful refresher and helped “jog their memory” about the intervention. Finally, we did not empirically verify the Casarett EBI core components we identified. We did, however, map the little-t EBI theory of change onto an extant Big-T theory of change; this may be a practical core function “check” that other researchers could use. Given the fact that most intervention developers do not identify core components as part of their research, it is likely unfeasible for those wishing to adapt interventions to first identify and empirically verify core components. Thus, our method of theory mapping may present a more feasible alternative.
Future directions
More work is needed to refine and strengthen the methods that we have developed for identifying core functions and forms post hoc. As these methods are applied and refined by other researchers, a compendium of methods for identifying core functions and forms—and methods for adaptation on a larger scale—could be disseminated through adaptation platforms or toolkits [44]. We also believe that more research under the core functions and forms schema would move the field forward in helping to define what about interventions is “core” and how we can conceptualize and apply core functions and forms in adapting EBIs.
Supplementary Material
Acknowledgments:
We would like to thank the members of the Casarett et al. research team for their contributions to this research, which include participation in interviews. We would also like to thank Dr. Mónica Pérez Jolles for her contributions in conceptualizing core functions and forms.
Funding: This research was partially funded using internal funds from RTI International; the funding body did not have any role in the design of the study, data collection, analysis, interpretation of the data, or writing of the manuscript. This manuscript represents the views of the authors alone. This research was also supported in part by the National Center for Advancing Translational Sciences and the National Institutes of Health (NIH; KL2TR001109, K01MH113806, L30MH108060, R25MH080916, R01MH106510, UL1TR001111, and P30AI050410). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Compliance with Ethical Standards
Conflicts of Interest: All authors declare that they have no conflicts of interest.
Authors’ Contributions: A.K. led data collection and analysis and writing of manuscript. S.B. and E.H. participated in data analysis. F.R., B.P., M.W., L.H., S.B., and A.K. contributed to research design and writing of the manuscript.
Ethical Approval: This study was reviewed by the institutional review boards at the University of North Carolina at Chapel Hill and RTI International and determined to be nonhuman subjects research. This article does not contain any studies with animals performed by any of the authors.
Informed Consent: This study does not involve human participants and informed consent was, therefore, not required.
References
- 1. Bopp M, Saunders RP, Lattimore D. The tug-of-war: Fidelity versus adaptation throughout the health promotion program life cycle. J Prim Prev. 2013;34(3):193–207. [DOI] [PubMed] [Google Scholar]
- 2. Elliott DS, Mihalic S. Issues in disseminating and replicating effective prevention programs. Prev Sci. 2004;5(1):47–53. [DOI] [PubMed] [Google Scholar]
- 3. Mowbray CT, Holter MC, Teague GB, Bybee D. Fidelity criteria: Development, measurement, and validation. Am J Eval. 2003;24:315–340. [Google Scholar]
- 4. Schoenwald SK, Hoagwood K. Effectiveness, transportability, and dissemination of interventions: What matters when? Psychiatr Serv. 2001;52(9):1190–1197. [DOI] [PubMed] [Google Scholar]
- 5. Rabin B. Fidelity and Adaptation for Implementation Science: How Can We Reconcile the Tension? Center for Research in Implementation Science and Prevention (CRISP) Seminar Series; University of Colorado Anschutz Medical Campus.2016. [Google Scholar]
- 6. Botvin GJ. Advancing prevention science and practice: Challenges, critical issues, and future directions. Prev Sci. 2004;5(1):69–72. [DOI] [PubMed] [Google Scholar]
- 7. Castro FG, Barrera M Jr, Martinez CR Jr. The cultural adaptation of prevention interventions: Resolving tensions between fidelity and fit. Prev Sci. 2004;5(1):41–45. [DOI] [PubMed] [Google Scholar]
- 8. Morrison DM, Hoppe MJ, Gillmore MR, Kluver C, Higa D, Wells EA. Replicating an intervention: The tension between fidelity and adaptation. AIDS Educ Prev. 2009;21(2):128–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cohen DJ, Crabtree BF, Etz RS, et al. Fidelity versus flexibility: Translating evidence-based research into practice. Am J Prev Med. 2008;35(5 suppl):S381–S389. [DOI] [PubMed] [Google Scholar]
- 10. van Daele T, van Audenhove C, Hermans D, van den Bergh O, van den Broucke S. Empowerment implementation: Enhancing fidelity and adaptation in a psycho-educational intervention. Health Promot Int. 2014;29(2):212–222. [DOI] [PubMed] [Google Scholar]
- 11. Carvalho ML, Honeycutt S, Escoffery C, Glanz K, Sabbs D, Kegler MC. Balancing fidelity and adaptation: Implementing evidence-based chronic disease prevention programs. J Public Health Manag Pract. 2013;19(4):348–356. [DOI] [PubMed] [Google Scholar]
- 12. Chambers D, Simpson L, Neta G, et al. Proceedings from the 9th annual conference on the science of dissemination and implementation. Implement Sci. 2017;12:48. [Google Scholar]
- 13. Backer TE. Finding the Balance: Program Fidelity and Adaptation in Substance Abuse Prevention: A State-of-the-Art Review. Rockville, MD: Center for Substance Abuse Prevention; 2001. [Google Scholar]
- 14. Blase K, Fixsen D. Core Intervention Components: Identifying and Operationalizing What Makes Programs Work. ASPE Research Brief. US Department of Health and Human Services; 2013. [Google Scholar]
- 15. Teno JM, Gozalo PL, Lee IC, et al. Does hospice improve quality of care for persons dying from dementia? J Am Geriatr Soc. 2011;59(8):1531–1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Miller SC, Mor V, Wu N, Gozalo P, Lapane K. Does receipt of hospice care in nursing homes improve the management of pain at the end of life? J Am Geriatr Soc. 2002;50(3):507–515. [DOI] [PubMed] [Google Scholar]
- 17. National Hospice and Palliative Care Organization. NHPCO Facts and Figures: Hospice Care in America. Alexandria, VA: NHPCO; 2018. [Google Scholar]
- 18. Christakis NA, Iwashyna TJ. Impact of individual and market factors on the timing of initiation of hospice terminal care. Med Care. 2000;38(5):528–541. [DOI] [PubMed] [Google Scholar]
- 19. Rickerson E, Harrold J, Kapo J, Carroll JT, Casarett D. Timing of hospice referral and families’ perceptions of services: are earlier hospice referrals better? J Am Geriatr Soc. 2005;53(5):819–823. [DOI] [PubMed] [Google Scholar]
- 20. Friedman BT, Harwood MK, Shields M. Barriers and enablers to hospice referrals: An expert overview. J Palliat Med. 2002;5(1):73–84. [DOI] [PubMed] [Google Scholar]
- 21. Cherlin E, Fried T, Prigerson HG, Schulman-Green D, Johnson-Hurzeler R, Bradley EH. Communication between physicians and family caregivers about care at the end of life: When do discussions occur and what is said? J Palliat Med. 2005;8(6):1176–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Vig EK, Starks H, Taylor JS, Hopley EK, Fryer-Edwards K. Why don’t patients enroll in hospice? Can we do anything about it? J Gen Intern Med. 2010;25(10):1009–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jenkins TM, Chapman KL, Ritchie CS, et al. Barriers to hospice care in Alabama: Provider-based perceptions. Am J Hosp Palliat Care. 2011;28(3):153–160. [DOI] [PubMed] [Google Scholar]
- 24. Casarett D, Karlawish J, Morales K, Crowley R, Mirsch T, Asch DA. Improving the use of hospice services in nursing homes: a randomized controlled trial. Jama. 2005;294(2):211–217. [DOI] [PubMed] [Google Scholar]
- 25. RTI International. Hospice Quality Reporting Program: HIS-Based Quality Measures Annual Testing Executive Summary. 2016. Available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Hospice-Quality-Reporting/Downloads/HQRP-HIS-Based-QMs-Annual-Testing-Executive-Summary-October-2016.pdf. [Google Scholar]
- 26. Patient-Centered Outcomes Research Institute. Standards for Studies of Complex Interventions. 2019. Available at https://www.pcori.org/research-results/about-our-research/research-methodology/pcori-methodology-standards#Complex [Google Scholar]
- 27. Pérez MJ, Jara C, Quintanilla RA. Contribution of tau pathology to mitochondrial impairment in neurodegeneration. Front Neurosci. 2018;12:441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655. [DOI] [PMC free article] [PubMed]
- 29. Jordanova T, Gerlach B, Faulkner M. Developing Strategies for Child Maltreatment Prevention A Guide for Adapting Evidence-Based Programs. Austin, TX: The University of Texas at Austin; 2015. [Google Scholar]
- 30. Fixsen DL, Naoom SF, Blase KA, Friedman RM.Wallace F. Implementation Research: A Synthesis of the Literature. Tampa, FL: University of South Florida, Louis de la Parte Florida Mental Health Institute, The National Implementation Research Network (FMHI Publication #231); 2005. [Google Scholar]
- 31. Lee SJ, Altschul I, Mowbray CT. Using planned adaptation to implement evidence-based programs with new populations. Am J Community Psychol. 2008;41(3-4):290–303. [DOI] [PubMed] [Google Scholar]
- 32. Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Huberman AM, Miles MB, eds. The Qualitative Researcher’s Companion. London and New York: Routledge; 2002:305–329. [Google Scholar]
- 33. Fixsen DL, Blase KA, Naoom SF, Wallace F. Core implementation components. Res Soc Work Pract. 2009, 19:531–540. [Google Scholar]
- 34. Lazarus RS. Psychological Stress and the Coping Process. New York: McGraw-Hill; 1966. [Google Scholar]
- 35. Lazarus RS, Cohen JB. Environmental stress. In: Altman I, Wohlwill JF, eds. Human Behavior and Environment. Boston, MA: Springer; 1977: 89–127. [Google Scholar]
- 36. Lazarus RS, Folkman S. Transactional theory and research on emotions and coping. Eur J Pers. 1987;1:141–169. [Google Scholar]
- 37. Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behav Ther. 2004;35:639–665. [DOI] [PubMed] [Google Scholar]
- 38. Sweeny K, Melnyk D, Miller W, Shepperd JA. Information avoidance: Who, what, when, and why. Rev Gen Psychol. 2010;14:340. [Google Scholar]
- 39. Afifi WA, Weiner JL. Toward a theory of motivated information management. Commun Theory. 2004;14:167–190. [Google Scholar]
- 40. Laubmeier KK, Zakowski SG, Bair JP. The role of spirituality in the psychological adjustment to cancer: A test of the transactional model of stress and coping. Int J Behav Med. 2004;11(1):48–55. [DOI] [PubMed] [Google Scholar]
- 41. Pottie CG, Ingram KM. Daily stress, coping, and well-being in parents of children with autism: A multilevel modeling approach. J Fam Psychol. 2008;22(6):855–864. [DOI] [PubMed] [Google Scholar]
- 42. Miller TA, McCool SF. Coping with stress in outdoor recreational settings: An application of transactional stress theory. Leis Sci. 2003;25:257–275. [Google Scholar]
- 43. Honey K, Morgan M, Bennett P. A stress-coping transactional model of low mood following childbirth. J Reprod Infant Psychol. 2003;21:129–143. [Google Scholar]
- 44. Chambers DA, Norton WE. The Adaptome: Advancing the science of intervention adaptation. Am J Prev Med. 2016;51(4 suppl 2):S124–S131. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.