Abstract
Purpose of Review
The impact of the coronavirus disease 2019 (COVID-19) pandemic is profound, with distressing consequences on many individuals, especially those with co-morbidities. Pregnant women are one such group of individuals who are at in increased risk of contracting COVID-19, due to their immunocompromised state. In South Africa, HIV infection and pre-eclampsia are the leading causes of maternal morbidity and mortality, with South Africa being the HIV epicentre of the world. The relationship between COVID-19 superimposed on HIV infection and preeclampsia is complex and uncertain due to their different immune responses, and therefore requires further research.
Recent Findings
Notably evidence suggests that pregnant women with chronic comorbidities (HIV and pre-eclampsia) may be at a greater risk of contracting or encountering complications from COVID-19. Maternal stress, during a pandemic, as well as home delivery have become potential options for pregnant woman. Nonetheless there is currently a paucity of information on the combined effect of COVID-19 in HIV-associated preeclampsia.
Summary
Understanding the pathogenesis of COVID-19 could potentially aid in developing effective treatment strategies for COVID-19 in HIV associated preeclampsia. This review article presents a comprehensive analysis of the current data in relation to COVID-19 and its effect on pregnant women, including symptoms, pathogenesis and the possible risk of vertical transmission. This paper also reviews its’ interactions and effects on preeclamptic and HIV positive pregnant women with suspected or confirmed COVID-19.
Keywords: COVID-19, Pre-eclampsia, HIV, Pregnancy
Introduction
In Wuhan City, China, numerous cases of pneumonia with unknown aetiology were reported by the Chinese Health Authority in late November /December 2019 [1•]. This epidemic of coronavirus disease 2019 (COVID-19) was caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The World Health Organization (WHO) declared the outbreak a global pandemic on March 11, 2020 [2–4].
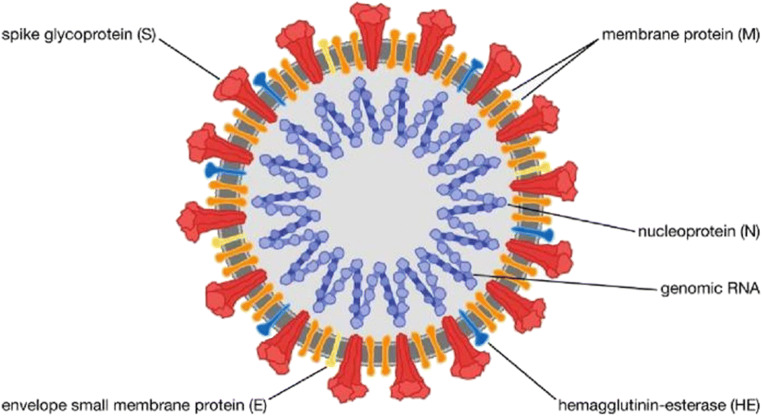
Coronaviruses are single-stranded viruses with an encapsulated RNA (Fig. 1) [7]. The term corona loosely means “halo” or “crown” in Latin, and refers to the structure of the capsid and RNA (Fig. 1) [8••]. The majority of the circulating coronaviruses cause mild upper respiratory infections, typically with fever, dry cough and fatigue, with sporadic severe illness in immunocompromised individuals [9••]. Although people of all ages are vulnerable to this virus, the elderly and those with pre-existing medical conditions such as tuberculosis, Human Immunodeficiency Virus (HIV), diabetes and asthma, are more susceptible to severe illness and fatalities [10•]. In addition, pregnant women are at a higher risk than non-pregnant women, as their altered immune state renders them more susceptible to viral infections and adverse pregnancy outcomes [11]. Previous evidence suggests that pregnant women with viral infections similar to that of SARS-CoV-2, such as severe acute respiratory syndrome (SARS), and Middle East respiratory syndrome (MERS) have a greater risk of maternal and neonatal morbidity and mortality [12••].
Fig. 1.
Structure of SARS-CoV-2 [Adapted from Encyclopedia Britannica, 2020] [5].The spike protein (S) enables binding to the trans-membrane ACE2 host receptor; the envelope (E) protein and the membrane (M) protein together form the viral envelope and determine its shape; the hemagglutinin esterase (HE) protein may look like another cell entry mechanism of novel CoVs; the nucleocapsid (N) protein in bound to the RNA genome of the virus to form the nucleocapsid [6]. For SARS-CoV-1 and SARS-CoV-2, the S protein is the key determinant for host tropism and pathogenicity. It is the focal target for neutralizing antibodies and thus of great concern with regard to immunological response and vaccine development [6]
During pregnancy, women develop an immunological adaptation which is essential for maintaining tolerance of the foetal semi-allograft [13]. This phase of a temporary suppressed immunity is modified by repression of T cell activity, which thus predisposes pregnant women to viral infections [14, 15]. Furthermore, the physiological changes in the circulatory and respiratory systems during pregnancy together with any inflammatory responses, as a result of a viral infection, is likely to aggravate clinical outcomes [16••]. Pregnant woman hospitalized for pneumonia are known to be at a higher risk of preterm birth, miscarriage, caesarean delivery and pre-eclampsia development [16••].
Pre-eclampsia (PE) is a pregnancy specific disorder characterized by new onset hypertension at or after 20 weeks’ gestation [17]. Moreover, women with bacterial or viral infections have a two-fold higher risk of developing PE [18]. SARS-CoV-2 is believed to attack the host and invade via angiotensin-converting enzyme 2 (ACE2), a cell entry receptor [19••]. The signs and symptoms produced by the SARS-CoV-2 infection are assumed to be a result of vasoconstriction due to a dysfunction of the renin-angiotensin system [20••]. On the other hand, the pathognomonic feature of PE involves widespread endothelial damage emanating from oxidative stress and anti-angiogenesis with dysregulation of the immune response [21•]. Furthermore, in the immunocompromised state of HIV infection, the tat protein has a powerful anti-angiogenic effect. Thus HIV-infected individuals have an increased risk of SARS-CoV-2 infection or severe illness [22]. The administration of anti-retroviral therapy (protease inhibitors, nucleoside reverse transfer inhibitors, or non-nucleoside reverse transfer inhibitors) may alter an individual’s predisposition to SARS-CoV-2 infection [22].
There is a paucity of data investigating the status of COVID-19 in pregnant women due to its high risk of human-to-human transmission. Thus a review is urgent and necessary to fill in current voids in the literature on COVID-19 infection concomitant with HIV infection in pregnant women with PE. This is of particular importance in countries such as South Africa in which the frequencies of both HIV infection and PE are high [23]. Moreover, this type of clinical setting will enable the development of efficacious treatment strategies.
COVID-19 Infection
Molecular Alterations by SARS-CoV-2
An understanding of the molecular basis of SARS-CoV-2 and its’ interaction with host cells, is crucial in designing effective therapeutic strategies against COVID-19. Despite the fact that COVID-19 results in severe pulmonary disease and its complications which may result in death, there is as yet no effective cure, drug treatment or vaccine [24]. Treatment remains supportive care with nasal oxygen or assisted ventilation although the use of low doses of the steroid, dexamethasone has been shown to improve survival rates [25].
Numerous molecular events are possibly involved in the pathogenesis of SARS-CoV-2 infection and its subsequent pulmonary and systemic complications. An accumulation of hyaluronan (a glycosaminoglycan component of the extracellular matrix found in the lung) and the potential role of polysaccharides for the interstitial oedema of the lungs, have been recognized [26]. Hyaluronan can absorb water 1000 times its molecular weight [27]. Andonegui-Elguera et al., (2020) revealed that an upregulation of genes encoding proteins that are required in hyaluronan, glycosaminoglycan, aminoglycan and mucopolysaccharide metabolism, in bronchoalveolar cells, are vital precursors in interstitial pulmonary oedema [28]. Additionally, several inflammatory cytokines produced in SARS-CoV-2 infection are robust inducers of hyaluronan metabolism, thus the need to identify immune cells infiltrating lung tissue [29]. The inhibition of hyaluronan synthesis could thus contribute to the management of SARS-CoV-2 infection [28]. An increased infiltration of macrophage and neutrophils to sites of infection/s have been documented and could potentially fuel acute respiratory distress syndrome (ARDS) [30]. Alterations in the concentrations of myeloid, Natural Killer (NK) and B-cells in the SARS-CoV-2 infected patients have also been reported [31]. Additionally, significant lymphopenia has also been observed, particularly in young patients, indicative of an impairment of the immune system during the SARS-CoV-2 infection [32]. Alterations of mast cell concentrations in broncho-alveolar lavage fluid, has also been documented. These mast cells secrete certain interleukins and chemokines necessary for attracting white blood cells to the inflammatory sites [33]. Although a synchronized immune response from both the innate and adaptative systems could result in the rapid control of the virus, an unsuccessful immune response would cause viral spread, cytokine storm and ultimately death.
Molecular Mechanisms and Gender Differences
Similar to the 1918 influenza pandemic and the SARS outbreak in 2003, males are more susceptible to SARS-CoV-2 infections as compared to females [34, 35]. Currently, more males than females have succumbed to death as a result of SARS-CoV-2 infections [36]. The decreased morbidity of SARS-CoV-2 infected women may be attributed to genes encoded on X chromosomes, and sex hormones [37]. ACE2 is a major link in the pathogenesis of COVID-19 and also catalyses the conversion of angiotensin I and angiotensin II to Ang 1–9 and 1–7, which aids in organ protection [38]. ACE2 genes are located on X chromosomes and females contain two X chromosomes, which function in a coordinated manner [37]. Men, with one X chromosome, thus lack cellular protection necessary during the SARS-CoV-2 infection [39]. Furthermore, Toll-like receptors (TLRs), which recognize pathogen-associated molecular patterns (PAMPS’s) to initiate appropriate immune responses, are also encoded on the X chromosomes [40]. Thus, woman have an enhanced TLR-mediated response and stronger innate immune response due to their two X chromosomes, compared to males, with one X chromosome. Besides chromosomes, sex hormones also effect the selection of immune response in both males and females [37]. Oestrogen and oestrogen receptor-α have been identified to contribute to T cell activation and proliferation, with the subsequent induction of interferon gamma (IFN-γ) which inhibit SARS-CoV-1 replication in females [41].
Pathogenesis: Entry into Host
Notably, the clinical manifestations of COVID-19 are similar to two other human infecting coronaviruses viz., SARS-CoV-1 and MERS-CoV infections [42]. Whilst the exact pathogenesis of COVID-19 requires clarity, the mechanisms of SARS-CoV-1 and MERS-CoV action may assist in unravelling the mystique of this infection.
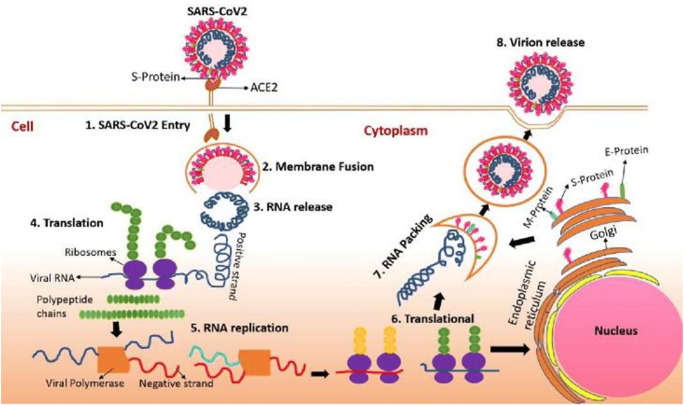
The coronavirus S protein serves as an important determinant of viral entry into host cells [43]. More specifically, these spike glycoproteins on the viral envelope bind to the ACE2 receptor, for SARS-CoV-1 and SARS-CoV-2, and N,N-diethyl-2-(4-phenylmethyl) ethanamine (DPPE) for MERS-CoV [44]. ACE2 is expressed in most organs in the body including ciliated and goblets cells in airways, as well on the placenta in pregnant woman, which serve as additional routes of entry into the host [45]. ACE2 has also been identified on intestinal epithelium, in high volumes, and also on cardiac cells and vascular endothelia, thus accounting for the cardiac problems endured by some patients [46]. A critical proteolytic cleavage at the SARS-CoV S proteins position, S2’ facilitates the viral and plasma membrane fusion, and viral infectivity [47]. Upon viral entry into the host (Fig. 2), the viral RNA genome that is released into the cytoplasm is then translated into two polyproteins and structural proteins, followed by the replication of the viral genome [48]. Envelope glycoproteins that are newly synthesized are inserted into either the golgi or endoplasmic reticulum (ER), and the nucleocapsid is synthesized through the combination of both nucleocapsid protein and genomic RNA [7]. Afterwards there is germination of the viral particles into the ER-golgi intermediate compartment (ERGIC), and ultimately there is fusion between the vesicle containing the virus particles and the plasma membrane to expel the virus [49••].
Fig. 2.
COVID-19 entry and viral replication and viral RNA packing in the human cell [Adapted from Boopathi et al., 2020] [48]
Antigen Presentation
Upon entry into the cell, viral antigens are presented to antigen presenting cells (APC) [50]. The three major histocompatibility complex (MHC) class I genes; human leukocyte antigens (HLA) A, B, and C, present these antigenic peptides to virus-specific cytotoxic T lymphocytes (CTLS) [51]. Although antigen presentation of SARS-CoV-1 primarily depends on MHC I molecules, MHC II also has a contributory role [51]. The diverse peptides present, and the antigen presentation procedure of the host, enables a better understanding of cellular immunity thereby contributing to vaccine development. Dendritic cells (DCs) also have an important role as an antigen presenting cell during viral infection, and further links innate and adaptive immunity [52]. The analogy between SARS-CoV-2 and its predecessor strain infection (SARS-CoV-1 & MERS-CoV), allow for its’ antigen presentation mechanisms to be understood using accessible data. Lau et.al., (2012) [53] elucidates that DCs are found to be a possible prospect in antigen presentation during SARS infection, as they are alleged to respond back whenever there is an inflammatory response in the respiratory tract. Evidence shows that SARS-CoV-2 infects human macrophages as a result of Immunoglobulin G (IgG) mediated antibody enhancement (ADE), and that infected macrophages do not illicit productive viral replication [54].
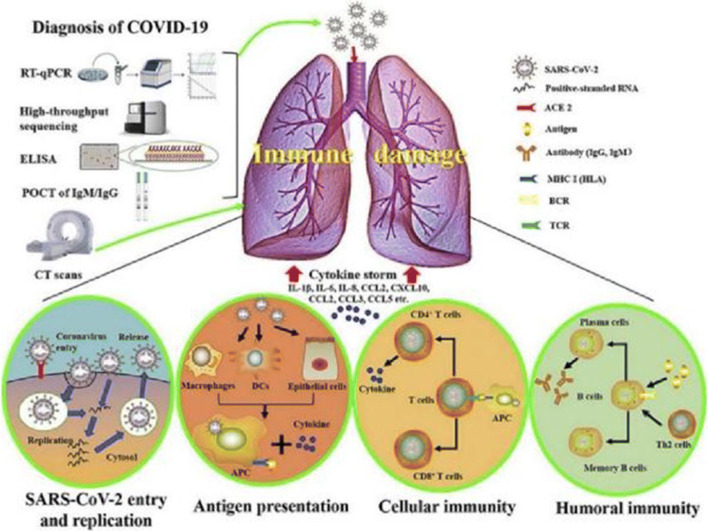
Humoral and Cellular Immunity
The humoral and cellular immunity are facilitated by virus-specific B and T cells, that are activated by antigen presentation [55]. The humoral immune response is an antibody-mediated immune response, where B cells are assisted by T helper cells to differentiate into plasma cells that can produce antibodies specific to a viral antigen (Fig. 3) [50]. Since SARS-CoV-1 virus has an antibody profile similar to that of common acute viral infections, IgM and IgG production form part of the primary and secondary immune responses, respectively [56]. Research has shown that the SARS-specific IgM antibodies disappear at the end of week 12, whilst the IgG antibodies last for a longer time [56] confirming that IgG is a potent protector antibody during infection. Furthermore, SARS-specific IgG antibodies are S-specific and N-specific antibodies that attach to either the spike or nucleocapsid, respectively [57]. In comparing the humoral immune response to the cellular immune response, the latter is a mechanism of adaptive immunity, mediated by T-lymphocytes (Fig. 3). Helper T cells and cytotoxic T cells are vital in cellular immunity, where they direct the overall adaptive immune response and kill of viral infected cells, respectively [58]. Yong et. al., (2019) [59] showed that T cells are imperative for cellular immunity on both the MERS-CoV and SARS-CoV-1, where a lack of T cells consequently resulted in no viral clearance.
Fig. 3.
The pathogenesis of COVID-19 [Adapted from Li et al.,2020] [50]
Furthermore, recent reports show that the number of CD4+ and CD8+ T cells in the peripheral blood of SARS-CoV-2 infected patients are reduced significantly, despite its excessive activation [60]. Likewise, the acute phase response in patients with SARS-CoV-1 is accompanied with severe reduction of both CD4+ T and CD8+ T cells [56]. With regard to the SARS-CoV-1 and MERS-CoV infections, it was reported that, CD4+ (TNFα, IL-2, and IFN) and CD8+ (TNFα, IFN-gamma) memory T cells can persist for four years in SARS-CoV-1 recovered individuals and can also undergo T cell proliferation, delayed-type hypersensitivity (DTH) response and production of IFN-gamma [61]. Investigations performed has revealed that 14 out 23 patients, 6 years after the SARS-CoV-1 infection, displayed distinct T cell memory when exposed to the S peptide library of SARS -CoV-1 [62]. Similarly, specific CD8+ T cells display a comparable effect on MERS-CoV clearance in mice [63].
Although these discoveries can assist in the rational design and development of effective vaccines against SARS-CoV-2, recent reports show that peripheral blood mononuclear cells in those SARS-CoV-2 infected patients, decline with concomitant reduction in CD8+ and CD4+ T cell counts [64]. SARS-CoV-2 may therefore persist in these survivors as they may have a compromised T memory cell generation.
Cytokine Storm
An over-reaction of one’s immune system in response to a foreign material or antigen gaining entry, produces an uncontrolled and generalized inflammatory response of cytokines known as the “cytokine storm” [65]. Consequently, enormous quantities of pro-inflammatory cytokines (IFN-α, IFN-γ, IL-13, IL-6, IL-12, IL-18, IL-33, TNF-α, TGF-3, etc.) and chemokines (CCL2, CCL3, CCL5, CXCL8, CXCL9, CXCL10, etc.) are secreted by immune effector cells as seen in SARS-CoV infected patients [66]. Acute respiratory distress syndrome and pulmonary inflammation are in fact a consequence of cytokine storm, and is thus one of the crucial determinants to assess the severity of COVID-19 [62, 66, 67]. Reports show that 40% of the earlier SARS-CoV-2 infected patients died as a result of ARDS [68].
Previous studies have reported that COVID-19 infected patients requiring ICU admission, have elevated concentrations of CXCL10, CCL2 and TNF-α, in contrast to those not requiring ICU admission [67]. Moreover, a distinguishing characteristic of SARS-Cov-2 infection compared to SARS-CoV infection, is the increase in Th2-cytokines (IL-4 and IL-10) that are primarily important in supressing inflammation [69]. The above data suggests that cytokine storms are therefore detrimental in that they attack the immune system, with resultant ARDS, multiple organ collapse and, in severe cases of SARS-CoV-2 infection, death [70].
Immune Evasion
Despite a lack of clarity on how SARS-CoV-2 evades the hosts immune system, an 80% and 50% RNA sequence homology of SARS-CoV-2 with SARS-CoV-1 and MERS-CoV respectively, allows for an extrapolation of knowledge until further evidence has been identified [71]. Nonetheless, Kikkert (2019) [72] hypothesised that SARS-CoV-1, MERS-CoV, and SARS-CoV-2 evades immune detection by supression of our immune response. As a result of the three aforementioned coronaviruses belonging to the same genera, Betacoronavirus, they share similar immune evasion methods [8]. Immune evasion could also highlight the reason for longer incubation periods (2–11 days) experienced in some patients, where the virus is able to escape detection by cellular pattern recognition receptors (PRR) during the initial phase of infection [73]. In the progression of a SARS-CoV infection, viral PAMPS’s are protected from cytosolic PRR’s detection as the isolation of viral dsRNA occurs within double membrane vesicles (DMV’s) [73]. Corona viruses implement strategies (e.g. type I IFN responses) against the human bodies innate immune responses to exist and expand within a host with an incorporated antiviral IFN immune response [74]. In 2003, during the SARS-CoV-1 outbreak in Toronto, Canada, IFN-α was used to treat hospitalized SARS patients, resulting in an enhanced resolution of lung abnormalities [75]. Interferons serve as an extremely effective cytokine that can control the viral infection [76]. Corona viruses escape the immune strategies by inhibiting IFN induction and signalling [77]. During the inhibition of IFN induction, the deferred induction of IFN by the coronavirus subsequently activates proinflammatory cytokines and macrophages in the lungs [78]. This activation causes leakage of vessels, and further damages responses in the adaptive immunity.
IFN signalling is inhibited by SARS-CoV-1 and MERS-CoV interacting with several proteins to interfere with the signal transduction chain [79].
Phenotypic Signs and Symptoms
The symptoms associated with COVID-19 infection manifests after an incubation period of approximately 5.2 days [80]. The time frame from the onset of the symptoms to death may extend this period from 6 to 41 days, with an average of 14 days [81••]. However, this range is dependent on various factors, such as the immunity and age of the patient. Evidence shows that patients >70-years old have a shorter number of days to death, compared to patients <70-years old. In terms of immunity, evidence shows that patients with underlying diseases have a compromised immunity that renders them more susceptible to a severe COVID-19 infection, and thus these individuals are more susceptible to severe illness than those with no underlying medical condition [81••]. Symptoms are mostly systemic and respiratory disorders (Fig. 4), that include at onset fatigue, fever, cough, headache, diarrhoea, sputum production and haemoptysis [82]. In addition, digestive symptoms such as nausea, loss of appetite and vomiting, are experienced by some individuals.
Fig. 4.
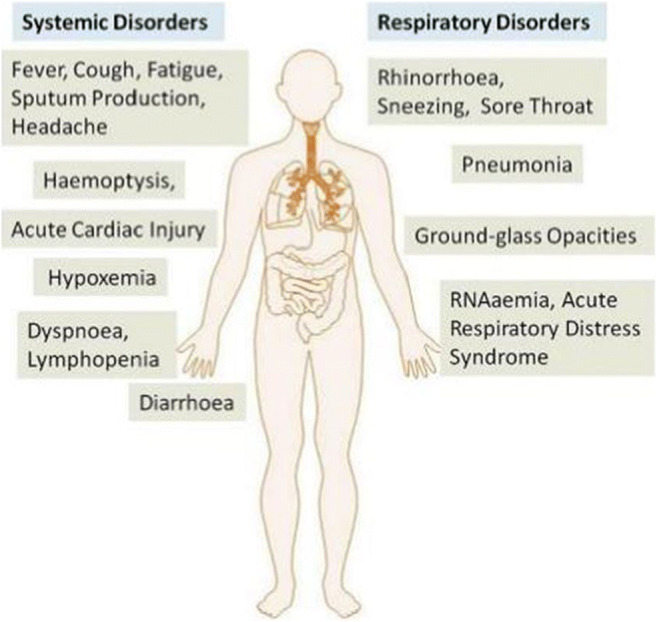
The systemic and respiratory disorders caused by COVID-19 infection [Adapted from Rothan and Byrareddy, 2020] [82]
Radiologic manifestations of COVID-19 have been primarily explored on chest CT scans and reveal clinical features, of pneumonia and ARDS, RNAaemia and acute cardiac injury [83]. The distinctive features include bilateral ground-glass opacities (GGO) with or without consolidation in the peripheral lungs, that culminates in death [84]. The use of CT scans has benefits in COVID-19 tested negative patients diagnosed by real-time reverse-transcription polymerase-chain-reaction (rt-PCR) assay [85].
COVID-19 during Pregnancy
The prevention, control and management of COVID-19 infection among pregnant women and the probable risk of vertical transmission is a major concern. The danger of vertical transmission of SARS-CoV-2 could be as low as that of SARS-CoV-1, where homology modelling revealed similar receptor binding domain structure between the two, suggesting similar pathogenesis [86]. While many recent studies only scrutinize and investigate a minimal number of COVID-19 infected pregnant woman, their findings are valuable under such emergent circumstances to aid effective preventative and clinical practices globally.
Pregnant women are at an increased risk of contracting additional severe diseases compared to non-pregnant women, due to the physiologic changes that they experience, including an increased heart rate and oxygen consumption, reduced lung capacity, and furthermore a shift away from cell-mediated immunity [87]. The symptoms experienced in COVID-19 infected pregnant woman, include a fever, cough, and shortness of breath, all of which are similar to those experienced in a MERS-CoV and SARS-CoV-1 infection [16]. Research has shown as association between severe COVID-19 in pregnancy with iatrogenic preterm delivery (75%), mainly in the third trimester, and for maternal indication [86]. Pregnant women are more vulnerable to respiratory pathogens and hence the development of severe pneumonia [88]. This sequentially renders them more vulnerable to COVID-19 infection as compared to the general population, specifically if they have chronic diseases or any maternal complications such as preeclampsia (PE). Pregnant women and their new-born babies should therefore be regarded as crucial at-risk populations in approaches focusing on the prevention and management of COVID-19 infection. Majority of neonates delivered from COVID-19 infected pregnant woman thus far, were asymptomatic and were also discharged to return to their homes in good health [89]. In contrast, a small number of neonates were symptomatic, requiring admission to neonatal specialist care [90]. It was very rare that neonates were positive for SARS-CoV-2 succeeding delivery, although a few cases did arise [91]. It was further observed that three asymptomatic infants who had tested negative for SARS-CoV-2, displayed elevated concentrations of serum IgM antibodies shortly after birth in umbilical blood [92]. However, the significance of vertical transmission remains unknown. The clinical characteristics reported in COVID-19 positive pregnant women are analogous to those reported for COVID-19 negative non-pregnant woman in the general population, and are reminiscent of a moderately optimistic clinical course and outcome for the COVID-19 infection [93]. Evidence also proposes that a risk of life-threatening infection occurs during the later stages of pregnancy, with current reports of severity of clinical illness ranging from asymptomatic infection/mild illness to extreme infection and fatal disease [94]. Case studies on a small cohort of COVID-19 infected pregnant women advocate that COVID-19 infection may increase ones’ risk of preterm delivery with minimal foetal effects. It is also important to consider that maternal stress is elevated during the pandemic, as proposed by numerous media publications [95]. Furthermore, isolation and an elevated stress or anxiety in pregnancy can result in adverse pregnancy outcomes, including low birth weight and preterm birth [96]. To help pregnant woman find coping mechanisms, a social support during pregnancy is vital and, in the interim, has been associated with less childhood adiposity at 18 months of age, and further protects the mother against postpartum depression [97]. With the amplified fear and concern about contracting this virus in a hospital, numerous women are now contemplating home delivery. However, although home birth can be safe in suitably selected pregnant woman with a trained, licenced birth assistant and close proximity to a hospital, it also involves mindful deliberation and discussion of risks, as some mothers are high-risk and would profit from a hospital delivery [98]. The necessary support from health care personnel may assist mothers to make an informed decision. Current administrative approaches of COVID-19 in pregnancy include advanced isolation stringencies, vigorous infection control mechanisms, fluid overload evasion, oxygen therapy, empiric antibiotics, SARS-CoV-2 and comorbidities testing, observation of uterine and foetal contraction, initial mechanical ventilation for progressive respiratory failure and individualized delivery planning [16].
Molecular Alterations from SARS-CoV-2 in Normal Pregnancy
Pregnancy encompasses inimitable immunological and suitable environmental alterations to protect the foetus from maternal rejection, and to allow suitable foetal development and safety against microorganisms [99]. Higher mortality rates and complications have been identified in pregnant woman with viral infections compared to the general population [100]. Notably during the SARS-CoV-1 epidemic in 2003, a prominent upsurge of mortalities and morbidities were identified in pregnant patients [101]. Although little is known about placental findings associated with viral infections, such as SARS-CoV-2, studies performed to date have identified foetal vascular malperfusion (FVM) with multiple thromboses [102]. Additionally, pathological features include placentas with increased perivillous or sub-chorionic fibrin, large zones of avascular villi, intravillous with an increase in local syncytial nodules, multiple villous infarcts, and chorangioma [93]. Moreover, studies have noted an increased rate of decidual arteriopathy including atherosis, fibrinoid necrosis, and mural hypertrophy of membrane arterioles, which ultimately result in maternal malperfusion (MVM) [103]. Off note, maternal hypertensive disorders, such as gestational hypertension and PE, are the main risk factors associated with MVM [104].
Pre-Eclampsia
COVID-19 and Maternal Pre-Eclampsia
During PE, the homeostasis of circulating helper T cells is shifted from the Th2 bias of normal pregnancy, towards Th1 and Th17, where Th17 promotes autoimmunity [105]. Agonistic autoantibodies produced against the angiotensin receptor-1 are a frequent but non-specific attribute of PE, which serve to intensify maternal vascular inflammation [106]. This subsequently causes an acute atherosis, which affects small uteroplacental spiral arteries and contributes to PE development [107].
PE is the leading cause of maternal and foetal morbidity and mortality, world-wide [23]. Currently the only cure for PE is delivery of the placenta as its exact aetiology remains unknown. Furthermore, overlapping and coexisting diseases (HIV infection and PE) with COVID-19 infection are a diagnostic predicament in obstetrics. In such situations, clinicians focus on the exclusive characteristics of these disease entities, such as significant hypertension in PE and elevated temperature in COVID-19 infection, to diagnose concurrent pathologies [108].
Shanes et al., (2020) identified that SAR-CoV-2 infected woman presented with elevated rates of maternal vascular malperfusion features [103], linked to the hypoxic injury of the placenta, and hence the development of PE. Preceding reports revealed that maternal infections, specifically viral, contribute to the development of PE via a deficient trophoblastic invasion and by subsequently inducing a maternal systematic inflammatory response [109]. Furthermore, ACE2 protein plays a vital role in regulating blood pressure and protecting the heart via hydrolysis of Angiotensin II to Angiotensin, to act as a receptor for coronavirus [109]. ACE2 protein is also expressed in surplus quantities in the syncytiotrophoblast, cytotrophoblast, endothelium and vascular smooth muscle of placental villi. It contributes primarily in regulating blood pressure and also in foetal development [110]. Any potential COVID-19 intrauterine infection may modify ACE2 expression and result in the development of a pre-eclamptic state through elevated Angiotensin II levels in the placental villi [111]. This will subsequently result in vasoconstriction and restricted foetal blood flow [111].
Furthermore, immune similarities occur between COVID-19 infection and pre-eclamptic women. During COVID-19, a cytokine profile resembling secondary haemophagocytic lymphohistiocytosis may be characterized by an upsurge of pro-inflammatory cytokines (IL-2, IL6, IL-7 and TNF-α) [67]. Screening of all COVID-19 severe patients are recommended to be performed using laboratory markers of hyper-inflammation as increased serum ferritin and low platelet count have been identified [67]. Research on maternal serum cytokines reveal a significant rise in maternal IL-6, IL-10 and TNF-α in pre-eclamptic pregnant women compared to normotensive pregnant women [112]. Additionally, a hyper-inflammatory state is reflected in pre-eclamptic compared to normotensive pregnant women, as their maternal serum ferritin is much greater. Lastly, thrombocytopenia (<100,000/mL), a condition of having low blood platelets, is an independent risk factor used to assess the severity in PE [113]. In terms of assessing the severity of COVID-19 patients, it is a defining criterion for cytopenia in H-score [67].
Preeclampsia-like Syndrome and COVID-19
The occurrence of a PE-like syndrome has been identified in six out of eight COVID-19 pregnant women who were admitted to the ICU with severe pneumonia [114]. Routine laboratory tests (uterine artery pulsatility index on Doppler ultrasound, serum soluble fms-like tyrosine kinase-1 [sFLT-1] and placental growth factor [PlGF]) measuring biophysical and biochemical markers, that are usually altered in PE, were within their normal levels [115]. The normal biomarker results advocate that severe coronavirus disease can produce symptoms that mimic those of PE in the absence of defective placentation. This is additionally validated by symptoms disappearance without the placental delivery when an overall clinical improvement transpires. It is plausible that such occurrences are due to cytokine storms, which as mentioned above, results in ubiquitous inflammation and endothelial damage, and is also the reason behind symptoms related to coronavirus-related organ injury [116]. This reaction incorporates the activation of inflammation pathways that convert arachidonic acid to prostaglandins, thromboxane and eicosanoids, to eventually aggravate the significant release of cytokines [114]. The concentration of specific PE angiogenic and anti-angiogenic markers (such as sFLT-1 and PlGF) appear to be unaffected by the cytokine storms cascade of events. Usually a normal sFLT-1: PlGF ratio in a woman with clinically assumed PE may be presumably used to speculate the short-term absence of disease [117].
COVID-19 and Placental Pathology
With the increase in COVID-19 infected cases, hospitals expect an influx of Covid-19 infected pregnant patients for labour and delivery. As expected, there is very scanty information on placental findings in COVID-19 infected pregnant woman. Although the risk of vertical transmission is rare, it has been documented [118]. However, the frequency and mechanisms behind this occurrence, is unknown. Fortunately, information concerning the health of both mother and foetus may be gleaned via histopathologic examination of placental tissue [119]. Placental findings have previously been associated with a variety of viral infections in pregnancy, including lymphoplasmacytic villitis with associated enlargement of villi and intra-villous hemosiderin deposition as a result of maternal cytomegalovirus infection [120]. Reports of inter-villositis as a result of Zika virus and Dengue virus, among others, have also been noted. Algarroba et al., (2020) [121] used electron microscopy (EM) to visualize and recognize coronavirus virions attacking syncytiotrophoblasts in the placental villi (Fig. 5), this being the first visualization of the SARS-CoV-2 virus in the human placenta. EM has identified numerous invading virions (e.g. HIV) in the syncytiotrophoblast of placental villi, as well as SARS-CoV-2 virions in placental villi within fibroblasts [121]. Fibroblasts are cells that may develop into myofibroblasts in response to injury or inflammation, and in this instance, it reacts to the SARS-CoV-2 virus [122]. Attention is now focussed on the ACE2 receptor as it is expressed in the placenta. Notwithstanding the fact that placental infection with SARS-CoV-2 has been demonstrated, there is no evidence to show foetal infection. The vertical transmission of SARS-CoV-2 is controversial [93], some have reported no evidence on it. Dong et al., (2020) [91] reported that although a neonate born to a COVID-19 infected mother with infection of at least 20 days duration, the neonate presented with positive IgM and IgG antibodies, along with elevated IL-6 and IL-10 cytokines two hours after birth. Surprisingly, the maternal vaginal secretions tested negative for COVID-19 [121]. Furthermore, the asymptomatic neonate had numerous nasopharyngeal swabs for SARS-CoV-2 which tested negative. As a result of the neonate mounting an innate immune response, an in utero infection was suspected as IgM antibodies do not cross the placenta [121].
Fig. 5.
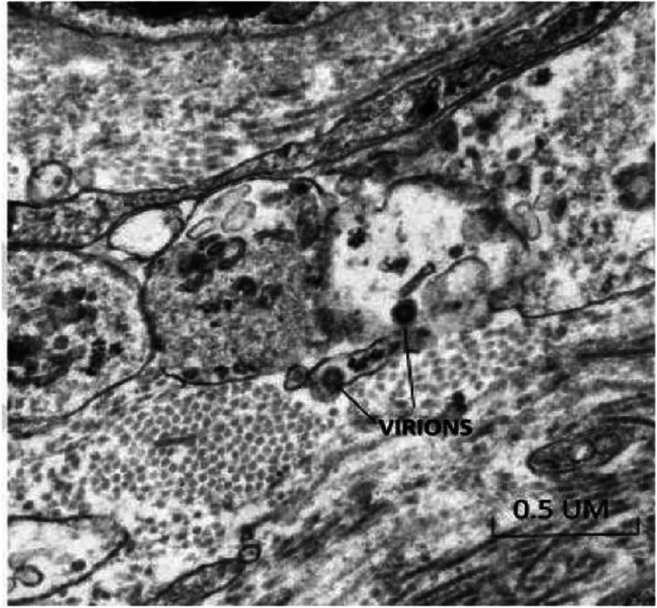
Transmission electron microscopy of the trophoblastic layer in the mesenchymal core of the terminal villus showing two virions, in the cell processes of fibroblasts (50,000X) [Adapted from Algarroba et al., 2020] [121]
HIV and COVID-19 Pandemic
In South Africa, more than half of all HIV infected individuals are female in their reproductive age (15–49 years old) [123]. Moreover, South Africa is the HIV epicentre in the world, with the highest active HIV cases [124] HIV infected individuals are more susceptible during the COVID-19 outbreak. Recent evidence suggests that the function of antiretroviral treatment (ART) could be the reason for the inconsistent infection rate of COVID-19 in HIV infected patients [125]. Notably HIV infected individuals whose disease is not well managed and who are not on ART have an amplified risk of contracting COVID-19. This susceptibility is attributed to their compromised immunity, which subsequently renders them at a heightened risk for death. Although HIV infected pregnant women are challenged by contracting COVID-19, they also are affected by the COVID-19 pandemic in restriction of movement, mental health and exposure to health care workers during antenatal visits [126•].
HIV and COVID-19 in Pregnancy
South Africa has the highest coronavirus prevalence in Africa, with over 603,338 cases across all nine provinces [4]. To-date, the South African Department of Health has reported 12,843 deaths of individuals infected with coronavirus [4]. Despite the devastating COVID-19 pandemic, South Africa is also home to the largest HIV epidemic in the world, with 7.7 million people living with HIV and 3 million people living with HIV (PLWH) yet not on treatment [127]. South Africa’s reaction to the HIV epidemic has functioned fairly well as 91% of PLHIV are aware of their HIV status, 68% are on ART, and 83% are attaining viral suppression [128]. HIV testing and the necessary treatment are standard of care at both antenatal clinics and hospitals. Moreover, South Africa has also seen a decrease in the vertical transmission of HIV from 3.5% in 2010 to 0.9% in 2018 [127].
The 21 day coronavirus lockdown in South Africa has increased PLWH based on probable connections between COVID-19 exposure, HIV infection, and other risk factors such as diabetes and hypertension in pregnancy (PE) [129]. Furthermore, potential disruptions with care and treatments, and increased rates of socially-derived burdens in the form of stigma, violence, discrimination, segregation, and hate encountered by PLWH, also contribute to this syndemic [130]. A syndemic is defined as two or more epidemics interacting synergistically to produce an increased burden of disease in a population [131]. In this scenario, SARS-CoV-2 is presumed to function in tandem with numerous health challenges faced by PLWH, including HIV infection itself, chronic non-communicable diseases, mental health burden, substance abuse, and other infections, all of which are catalysed by biological, behavioural, psychosocial and structural drivers of disease as posited by Halkitis et al., (2013) [132]. Although there is an increase in the number of COVID-19 positive and HIV positive pregnant woman entering antenatal clinics and hospitals, there is a lack of information regarding the effect of this syndemic on pregnant woman. Considering the elevated number of HIV infection and preeclamptic pregnant women in South Africa, and the fact that both disorders are related to alterations in the immune system, primarily a reduced cell mediated immunity and an inflated inflammatory response respectively [133], it seems judicious to presume that these conflicting immune responses maybe neutralized and have minimal contribution to the SARS-CoV-2 infection. However, there is a scarcity in information regarding this, and thus further research needs to be conducted to develop effective treatment methods that target both the viruses, with minimal effect on the mother and her offspring.
Comparisons between HIV and SARS-CoV-2
HIV belongs to the genus Lentivirus, and functions by destroying the immune system cells (macrophages and CD4+ cells), thus exposing one to opportunistic infections and rendering them more vulnerable [126•]. The HIV-1 subtype is accountable for most infections globally, and is transmitted through exposure to infected bodily fluids (e.g. semen, blood, breast milk, vaginal fluids) [134]. Common routes of transmission routes for HIV are through, intravenous drug use and occupational vulnerability, condom-less sexual intercourse, and vertical transmission from an infected mother-to-child during pregnancy, delivery, or breastfeeding [126•]. Comparatively yet dissimilar to HIV, SARS-CoV-2 is an acute respiratory infection and has a quick incubation period. Although evidence shows that the primary modes of transmission are through respiratory droplets and contact, evidence confirms a possibility for oral-faecal transmission [135]. Recent evidence suggests that the virus is airborne [136]. Unlike HIV, where an undetectable viral load denotes an un-transmissible virus, the occurrence of the viral RNA does not necessarily indicate a current infection for SARS-CoV-2 [137].
Despite differing modes of transmission, HIV and COVID-19 transmission both present with a stigma of fear and anxiety. Analogous to the initial years of the HIV epidemic, the fear associated with COVID-19 infection resides in the absence of a vaccine [138]. This anxiety creates implications for mental health and endorses disease-related stigma [138]. Those HIV infected individuals who do not have effective disease management, have an increased risk of contracting COVID-19 and subsequently experiencing complications. During the COVID-19 pandemic, HIV treatment orders may be interrupted and also, HIV infected individuals suffering from any additional illnesses may experience delayed treatment as a result of COVID-19 [139]. HIV infected individuals are thus more prone to contracting an opportunistic infection (e.g., pneumonia, tuberculosis, etc.,), compared to those without compromised immune systems [139].
Conclusion
There is currently a rapid increase in the number of COVID-19 cases, deaths, and countries affected. Multiple voids about this virus and its effects currently exist, with limited data being available on COVID-19 infected pregnant women. The relationship between COVID-19 superimposed on HIV infection and preeclampsia is complex and uncertain. Similarities in the homology of SARS-CoV-2 with SARS-CoV-1 and MERS-CoV validates the homologous clinical characteristics among pregnancies with COVID-19, SARS and MERS. COVID-19 infected pregnant women should be closely monitored, even after their etiological tests turn negative, as they are still at a great risk. Notably this research has provided some strategies for the obstetric management of pregnant women with COVID-19. Collectively, these findings advocate an urgent amplified antenatal surveillance for pregnant women diagnosed with SARS-CoV-2 and comorbidities (HIV and preeclampsia). An aggressive mandatory intervention to effectively manage a severe respiratory infection should be the basis of care for any pregnant woman with COVID-19. Future surveillance systems for COVID-19 cases need to include data on pregnancy status, as well as maternal and fetal outcomes.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Preeclampsia
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rowen Govender, Email: rowengovende@gmail.com.
Thajasvarie Naicker, Email: naickera@ukzn.ac.za.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Chen L, Jin Q, Zhou Y, Yang J, Wang Z, Ge K, Yang J, Wang H. Clinical characteristics of 2019 novel coronavirus pneumonia in Zhejiang province, China. Mol Med Rep. 2020;22(3):2583–2587. doi: 10.3892/mmr.2020.11329. [DOI] [PubMed] [Google Scholar]
- 2.Boelig R, Manuck T, Oliver E, Di Mascio D, Saccone G, Bellussi F, Berghella V. Labor and delivery guidance for COVID-19. American Journal of Obstetrics & Gynecology MFM. 2020;2(2):100110. doi: 10.1016/j.ajogmf.2020.100110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta bio-medica : Atenei Parmensis. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coronavirus Update (Live): 23,264,348 Cases and 805,834 Deaths from COVID-19 Virus Pandemic - Worldometer [Internet]. Worldometers.info. 2020 [cited 21 August 2020]. Available from: https://www.worldometers.info/coronavirus/
- 5.Coronavirus | Definition, Features, & Examples [Internet]. Encyclopedia Britannica. 2020 [cited 17 July 2020]. Available from: https://www.britannica.com/science/coronavirus-virus-group.
- 6.Samavati L. and Uhal B. ACE2, Much More Than Just a Receptor for SARS-COV-2. Front Cell Infect Microbiol. 2020;10(317). Published online 2020 June 5. doi: 10.3389/fcimb.2020.00317 [DOI] [PMC free article] [PubMed]
- 7.Perlman S, Netland J. Coronaviruses post-SARS: update on replication and pathogenesis. Nat Rev Microbiol. 2009;7(6):439–450. doi: 10.1038/nrmicro2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.•• Kumar S, Nyodu R, Maurya VK, Saxena SK. Host Immune Response and Immunobiology of Human SARS-CoV-2 Infection. Coronavirus Disease 2019 (COVID-19). 2020: 43–53. This article demonstrates the importance of immune responses during SARS-CoV-2 infection.
- 9.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu F, Cao Y, Xu S, Zhou M. Co-infection of SARS-CoV-2 and HIV in a patient in Wuhan city, China. J Med Virol. 2020;92(6):529–530. doi: 10.1002/jmv.25732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kourtis AP, Read JS, Jamieson DJ. Pregnancy and infection. N Engl J Med. 2014;370(23):2211–2218. doi: 10.1056/NEJMra1213566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ciobanu AM, Peltecu G, Panaitescu AM. Coronavirus in pregnancy. What we know so far? Maedica (Buchar) 2020;15(1):6–10. doi: 10.26574/maedica.2020.15.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weetman AP. Immunity, thyroid function and pregnancy: molecular mechanisms. Nat Rev Endocrinol. 2010;6(6):311–318. doi: 10.1038/nrendo.2010.46. [DOI] [PubMed] [Google Scholar]
- 14.Longman R, Johnson T. Viral respiratory disease in pregnancy. Postgrad Obstet Gynecol. 2007;27(22):1–6. doi: 10.1097/GCO.0b013e328028fdc7. [DOI] [PubMed] [Google Scholar]
- 15.Pazos M, Sperling RS, Moran TM, Kraus TA. The influence of pregnancy on systemic immunity. Immunol Res. 2012;54(1–3):254–261. doi: 10.1007/s12026-012-8303-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus Disease 2019 (COVID-19) and Pregnancy: What obstetricians need to know. Am J Obstet Gynecol. 2020;222(5):415–426. doi: 10.1016/j.ajog.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, Hall DR, Warren CE, Adoyi G, Ishaku S. Hypertensive disorders of pregnancy: ISSHP classifcation, diagnosis, and management recommendations for international practice. Hypertension. 2018;72(1):24–43. doi: 10.1161/HYPERTENSIONAHA.117.10803. [DOI] [PubMed] [Google Scholar]
- 18.Alshareef SA, Eltom AM, Nasr AM, Hamdan HZ, Adam I. Rubella, herpes simplex virus type 2 and preeclampsia. Virol J. 2017;14(1):142. doi: 10.1186/s12985-017-0813-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Astuti I, Ysrafil Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): An overview of viral structure and host response. Diabetes Metab Syndr Clin Res Rev. 2020;14(4):407–412. doi: 10.1016/j.dsx.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Groß S, Jahn C, Cushman S, Bär C, Thum T. SARS-CoV-2 receptor ACE2-dependent implications on the cardiovascular system: From basic science to clinical implications. J Mol Cell Cardiol. 2020;144:47–53. doi: 10.1016/j.yjmcc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Powe C, Levine R, Karumanchi S. Preeclampsia, a Disease of the Maternal Endothelium. Circulation. 2020;123(24):2856–2869. doi: 10.1161/CIRCULATIONAHA.109.853127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vizcarra P, Pérez-Elías M, Quereda C, Moreno A, Vivancos M, Dronda F and Casado J. COVID-19 in HIV-Infected Individuals: Preliminary Results of a Prospective Cohort. The lancet HIV,ONLINE FIRST. 2020 [Cited 30 June 2020]. Available from SSRN: https://ssrn.com/abstract=3588554 . [DOI] [PMC free article] [PubMed]
- 23.Department of Health. Saving mothers 2014–2016: (2017). Seventh triennial report on confidential enquiries into maternal deaths in South Africa: executive summary. Republic of South Africa: National Department of Health, 1–134.
- 24.Xiong Y, Liu Y, Cao L, Wang D, Guo M, Guo D, Hu W, Yang J, Tang Z, Zhang Q, Shi M, Liu Y, Zhou Y, Lan K, Chen Y. Transcriptomic characteristics of Bronchoalveolar lavage fluid and peripheral blood mononuclear cells in COVID-19 patients. SSRN Electron J. 2020;9(1):761–770. doi: 10.1080/22221751.2020.1747363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lammers T, Sofias A, van der Meel R, Schiffelers R, Storm G, Tacke F, Koschmieder S, Brümmendorf T, Kiessling F, Metselaar J. Dexamethasone nanomedicines for COVID-19. Nat Nanotechnol. 2020;15(8):622–624. doi: 10.1038/s41565-020-0752-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hällgren R, Samuelsson T, Laurent T, Modig J. Accumulation of Hyaluronan (hyaluronic acid) in the lung in adult respiratory distress syndrome. Am Rev Respir Dis. 1989;139(3):682–687. doi: 10.1164/ajrccm/139.3.682. [DOI] [PubMed] [Google Scholar]
- 27.Bell TJ, Brand OJ, Morgan DJ, Salek-Ardakani S, Jagger C, Fujimori T, Cholewa L, Tilakaratna V, Östling J, Thomas M, Day AJ, Snelgrove RJ, Hussell T. Defective lung function following influenza virus is due to prolonged, reversible hyaluronan synthesis. Matrix Biol. 2019;80:14–28. doi: 10.1016/j.matbio.2018.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Andonegui-Elguera S, Taniguchi-Ponciano K, Gonzalez-Bonilla C, Torres J, Mayani H, Herrera L, Peña-Martínez E, Silva-Román G, Vela-Patiño S, Ferreira-Hermosillo A, Ramirez-Renteria C, Carvente-Garcia R, Mata-Lozano C, Marrero-Rodríguez D and Mercado M. Molecular Alterations Prompted by SARS-CoV-2 Infection: Induction of Hyaluronan, Glycosaminoglycan and Mucopolysaccharide Metabolism. Arch Med Res. Published online 2020 June 18. Available from 10.1016/j.arcmed.2020.06.011 [DOI] [PMC free article] [PubMed]
- 29.Shi Y, Wang Y, Shao C, Huang J, Gan J, Huang X, Bucci E, Piacentini M, Ippolito G, Melino G. COVID-19 infection: the perspectives on immune responses. Cell Death Differ. 2020;27(5):1451–1454. doi: 10.1038/s41418-020-0530-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liao M, Liu Y, Yuan J, Wen Y, Xu G, Zhao J, Cheng L, Li J, Wang X, Wang F, Liu L, Amit I, Zhang S, Zhang Z. Single-cell landscape of bronchoalveolar immune cells in patients with COVID-19. Nat Med. 2020;26(6):842–844. doi: 10.1038/s41591-020-0901-9. [DOI] [PubMed] [Google Scholar]
- 31.Wen W, Su W, Tang H, Le W, Zhang X, Zheng Y, Liu X, Xie L, Li J, Ye J, Dong L, Cui X, Miao Y, Wang D, Dong J, Xiao C, Chen W and Wang H. Author correction: immune cell profiling of COVID-19 patients in the recovery stage by single-cell sequencing. Cell Discov. 2020;6(41). Available from 10.1038/s41421-020-00187-5. [DOI] [PMC free article] [PubMed]
- 32.Wang F, Nie J, Wang H, Zhao Q, Xiong Y, Deng L, Song S, Ma Z, Mo P, Zhang Y. Characteristics of peripheral lymphocyte subset alteration in COVID-19 pneumonia. J Infect Dis. 2020;221(11):1762–1769. doi: 10.1093/infdis/jiaa150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Theoharides T. COVID -19, pulmonary mast cells, cytokine storms, and beneficial actions of luteolin. BioFactors. 2020;46(3):306–308. doi: 10.1002/biof.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Karlberg J. Do men have a higher case fatality rate of severe acute respiratory syndrome than women do? Am J Epidemiol. 2004;159(3):229–231. doi: 10.1093/aje/kwh056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Klein S, Dhakal S, Ursin R, Deshpande S, Sandberg K, Mauvais-Jarvis F. Biological sex impacts COVID-19 outcomes. PLoS Pathog. 2020;16(6):e1008570. doi: 10.1371/journal.ppat.1008570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Klein SL, Pekosz A, Passaretti C, Anker M, Olukoya P. The impact of sex, gender and pregnancy on 2009 H1N1 disease. Biol Sex Differ. 2010;1(1):5. doi: 10.1186/2042-6410-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li Y, Jerkic M, Slutsky A and Zhang H. Molecular mechanisms of sex bias differences in COVID-19 mortality. Crit Care. 2020;24(1). Available from10.1186/s13054-020-03118-8 [DOI] [PMC free article] [PubMed]
- 38.Zhang H, Penninger J, Li Y, Zhong N, Slutsky A. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46(4):586–590. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lan J, Ge J, Yu J, Shan S, Zhou H, Fan S, Zhang Q, Shi X, Wang Q, Zhang L, Wang X. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581(7807):215–220. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 40.Libert C, Dejager L, Pinheiro I. The X chromosome in immune functions: when a chromosome makes the difference. Nat Rev Immunol. 2010;10(8):594–604. doi: 10.1038/nri2815. [DOI] [PubMed] [Google Scholar]
- 41.Sainz B, Mossel E, Peters C, Garry R. Interferon-beta and interferon-gamma synergistically inhibit the replication of severe acute respiratory syndrome-associated coronavirus (SARS-CoV) Virology. 2004;329(1):11–17. doi: 10.1016/j.virol.2004.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Petrosillo N, Viceconte G, Ergonul O, Ippolito G, Petersen E. COVID-19, SARS and MERS: are they closely related? Clin Microbiol Infect. 2020;26(6):729–734. doi: 10.1016/j.cmi.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shang J, Wan Y, Luo C, Ye G, Geng Q, Auerbach A, Li F. Cell entry mechanisms of SARS-CoV-2. Proc Natl Acad Sci. 2020;117(21):11727–11734. doi: 10.1073/pnas.2003138117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Woo H, Park S, Choi Y, Park T, Tanveer M, Cao Y, Kern N, Lee J, Yeom M, Croll T, Seok C, Im W. Developing a fully glycosylated full-length SARS-CoV-2 spike protein model in a viral membrane. J Phys Chem B. 2020;124(33):7128–7131. doi: 10.1021/acs.jpcb.0c04553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ziegler C, Allon S, Nyquist S, Mbano I, Miao V, Cao Y, Yousif A, Bals J, Hauser B, Feldman J, Muus C, Wadsworth M, II, Kazer S, Hughes T, Doran B, Gatter G, Vukovic M, Tzouanas C, Taliaferro F, Guo Z, Wang J, Dwyer D, Buchheit K, Boyce J, Barrett N, Laidlaw T, Carroll S, Colonna L, Tkachev V, Yu A, Zheng H, Gideon H, Winchell C, Lin P, Berger B, Leslie A, Flynn J, Fortune S, Finberg R, Kean L, Garber M, Schmidt A, Lingwood D, Shalek A, Ordovas-Montanes J. SARS-CoV-2 Receptor ACE2 is an Interferon-Stimulated Gene in Human Airway Epithelial Cells and Is Enriched in Specific Cell Subsets Across Tissues. Cell Press. 2020;181(5):1016–1035.e19. doi: 10.1016/j.cell.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong J, Turner A, Raizada M, Grant M, Oudit G. Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system. Circ Res. 2020;126(10):1456–1474. doi: 10.1161/CIRCRESAHA.120.317015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tang T, Bidon M, Jaimes J, Whittaker G, Daniel S. Coronavirus membrane fusion mechanism offers a potential target for antiviral development. Antivir Res. 2020;178:104792. doi: 10.1016/j.antiviral.2020.104792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Boopathi S, Poma A and Kolandaivel P. Novel 2019 coronavirus structure, mechanism of action, antiviral drug promises and rule out against its treatment. J Biomol Struct Dyn. 2020:1-10. Available from 10.1080/07391102.2020.1758788. [DOI] [PMC free article] [PubMed]
- 49.de Wit E, van Doremalen N, Falzarano D, Munster V. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol. 2016;14(8):523–534. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li X, Geng M, Peng Y, Meng L, Lu S. Molecular immune pathogenesis and diagnosis of COVID-19. J Pharm Anal. 2020;10(2):102–108. doi: 10.1016/j.jpha.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu J, Wu P, Gao F, Qi J, Kawana-Tachikawa A, Xie J, Vavricka C, Iwamoto A, Li T, Gao G. Novel Immunodominant peptide presentation strategy: a featured HLA-A*2402-restricted cytotoxic T-lymphocyte epitope stabilized by Intrachain hydrogen bonds from severe acute respiratory syndrome coronavirus Nucleocapsid protein. J Virol. 2010;84(22):11849–11857. doi: 10.1128/JVI.01464-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cook P, MacDonald A. Dendritic cells in lung immunopathology. Semin Immunopathol. 2016;38(4):449–460. doi: 10.1007/s00281-016-0571-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lau YL, Peiris JS, Law HK. Role of dendritic cells in SARS coronavirus infection. Hong Kong Med J. 2012;18(Suppl 3):28–30. [PubMed] [Google Scholar]
- 54.Eroshenko N, Gill T, Keaveney M, Church G, Trevejo J, Rajaniemi H. Implications of antibody-dependent enhancement of infection for SARS-CoV-2 countermeasures. Nat Biotechnol. 2020;38(7):789–791. doi: 10.1038/s41587-020-0577-1. [DOI] [PubMed] [Google Scholar]
- 55.Ni L, Ye F, Cheng M, Feng Y, Deng Y, Zhao H, et al. Detection of SARS-CoV-2-Specific Humoral and Cellular Immunity in COVID-19 Convalescent Individuals. Immunity. 2020;52(6):971–977.e3. doi: 10.1016/j.immuni.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Haveri A, Smura T, Kuivanen S, Österlund P, Hepojoki J, Ikonen N, Pitkäpaasi M, Blomqvist S, Rönkkö E, Kantele A, Strandin T, Kallio-Kokko H, Mannonen L, Lappalainen M, Broas M, Jiang M, Siira L, Salminen M, Puumalainen T, Sane J, Melin M, Vapalahti O, Savolainen-Kopra C. Serological and molecular findings during SARS-CoV-2 infection: the first case study in Finland, January to February 2020. Eurosurveillance. 2020;25(11):2000266. doi: 10.2807/1560-7917.ES.2020.25.11.2000266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Oh H, Gan S, Bertoletti A, Tan Y. Understanding the T cell immune response in SARS coronavirus infection. Emerg Microbes Infect. 2012;1(9):1–6. doi: 10.1038/emi.2012.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chowdhury M, Hossain N, Kashem M, Shahid M, Alam A. Immune Response in COVID-19: A Review. J Infect Public Health. 2020. Available from. 10.1016/j.jiph.2020.07.001. [DOI] [PMC free article] [PubMed]
- 59.Yong C, Ong H, Yeap S, Ho K, Tan W. Recent advances in the vaccine development against Middle East respiratory syndrome-coronavirus. Front Microbiol. 2019;10:1781. doi: 10.3389/fmicb.2019.01781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lin L, Lu L, Cao W, Li T. Hypothesis for potential pathogenesis of SARS-CoV-2 infection–a review of immune changes in patients with viral pneumonia. Emerg Microbes Infect. 2020;9(1):727–732. doi: 10.1080/22221751.2020.1746199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tay M, Poh C, Rénia L, MacAry P, Ng L. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20(6):363–374. doi: 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Channappanavar R, Zhao J, Perlman S. T cell-mediated immune response to respiratory coronaviruses. Immunol Res. 2014;59(1–3):118–128. doi: 10.1007/s12026-014-8534-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Coleman C, Sisk J, Halasz G, Zhong J, Beck S, Matthews K, Venkataraman T, Rajagopalan S, Kyratsous C, Frieman M. CD8+ T cells and macrophages regulate pathogenesis in a mouse model of Middle East respiratory syndrome. J Virol. 2016;91(1):e01825–e01816. doi: 10.1128/JVI.01825-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Diao B, Wang C, Tan Y, Chen X, Liu Y, Ning L, Chen L, Li M, Liu Y, Wang G, Yuan Z, Feng Z, Zhang Y, Wu Y and Chen Y. Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19). Front Immunol. 2020;11. Available from 10.1101/2020.02.18.20024364. [DOI] [PMC free article] [PubMed]
- 65.Ye Q, Wang B, Mao J. The pathogenesis and treatment of the ‘cytokine Storm’ in COVID-19. J Inf. 2020;80(6):607–613. doi: 10.1016/j.jinf.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zheng H, Zhang M, Yang C, Zhang N, Wang X, Yang X, Dong X, Zheng Y. Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID-19 patients. Cell Mol Immunol. 2020;17(5):541–543. doi: 10.1038/s41423-020-0401-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Coperchini F, Chiovato L, Croce L, Magri F, Rotondi M. The cytokine storm in COVID-19: an overview of the involvement of the chemokine/chemokine-receptor system. Cytokine Growth Factor Rev. 2020;53:25–32. doi: 10.1016/j.cytogfr.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhang C, Wu Z, Li J, Zhao H, Wang G. Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality. Int J Antimicrob Agents. 2020;55(5):105954. doi: 10.1016/j.ijantimicag.2020.105954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Song P, Li W, Xie J, Hou Y, You C. Cytokine storm induced by SARS-CoV-2. Clin Chim Acta. 2020;509:280–287. doi: 10.1016/j.cca.2020.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kim J, Chung Y, Jo H, Lee N, Kim M, Woo S, Park S, Kim J, Kim H, Han M. Identification of coronavirus isolated from a patient in Korea with COVID-19. Osong Public Health Res Perspect. 2020;11(1):3–7. doi: 10.24171/j.phrp.2020.11.1.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kikkert M. Innate immune evasion by human respiratory RNA viruses. J Innate Immun. 2019;12(1):4–20. doi: 10.1159/000503030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Snijder E, van der Meer Y, Zevenhoven-Dobbe J, Onderwater J, van der Meulen J, Koerten H, Mommaas A. Ultrastructure and origin of membrane vesicles associated with the severe acute respiratory syndrome coronavirus replication complex. J Virol. 2006;80(12):59275940. doi: 10.1128/JVI.02501-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Park A, Iwasaki A. Type I and type III Interferons – induction, signaling, evasion, and application to combat COVID-19. Cell Host Microbe. 2020;27(6):870–878. doi: 10.1016/j.chom.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Loutfy M, Blatt LM, Siminovitch KA, Ward S, Wolff B, Lho H, Pham DH, Deif H, LaMere EA, Chang M, Kain KC, Farcas GA, Ferguson P, Lathcford M, Levy G, Dennis JW, Lai EKY, Fish EN. Interferon alfacon-1plus corticosteroids in severe acute respiratory syndrome. JAMA. 2003;290(24):3222–3228. doi: 10.1001/jama.290.24.3222. [DOI] [PubMed] [Google Scholar]
- 76.Frieman M, Heise M, Baric R. SARS coronavirus and innate immunity. Virus Res. 2008;133(1):101–112. doi: 10.1016/j.virusres.2007.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Channappanavar R, Fehr A, Vijay R, Mack M, Zhao J, Meyerholz D, Perlman S. Dysregulated type I interferon and inflammatory monocyte-macrophage responses cause lethal pneumonia in SARS-CoV-infected mice. Cell Host Microbe. 2016;19(2):181–193. doi: 10.1016/j.chom.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Totura A, Whitmore A, Agnihothram S, Schäfer A, Katze M, Heise M, Baric R. Toll-Like Receptor 3 Signaling via TRIF Contributes to a Protective Innate Immune Response to Severe Acute Respiratory Syndrome Coronavirus Infection. mBio. 2015;6(3):e00638–e00615. doi: 10.1128/mBio.00638-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kopecky-Bromberg S, Martínez-Sobrido L, Frieman M, Baric R, Palese P. Severe acute respiratory syndrome coronavirus open Reading frame (ORF) 3b, ORF 6, and Nucleocapsid proteins function as interferon antagonists. J Virol. 2006;81(2):548–557. doi: 10.1128/JVI.01782-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tarafder S. Coronavirus Disease-2019 (COVID-19): a review of the literature. Acta Sci Microbiol. 2020;3(7):73–82. [Google Scholar]
- 81.Wang SX, Wang Y, Lu YB, Li JY, Song YJ, Nyamgerelt M, Wang XX. Diagnosis and treatment of novel coronavirus pneumonia based on the theory of traditional Chinese medicine. J Integr Med. 2020;18(4):275–283. doi: 10.1016/j.joim.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Li J, Gong X, Wang Z, Chen R, Li T, Zeng D, Li M. Clinical features of familial clustering in patients infected with 2019 novel coronavirus in Wuhan, China. Virus Res. 2020;286:198043. doi: 10.1016/j.virusres.2020.198043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Parekh M, Donuru A, Balasubramanya R and Kapur S. Review of the chest CT differential diagnosis of ground-glass opacities in the COVID era. Radiology. 2020:202504. Available from 10.1148/radiol.2020202504. [DOI] [PMC free article] [PubMed]
- 85.He J, Luo L, Luo Z, Lyu J, Ng M, Shen X, Wen Z. Diagnostic performance between CT and initial real-time RT-PCR for clinically suspected 2019 coronavirus disease (COVID-19) patients outside Wuhan, China. Respir Med. 2020;168:105980. doi: 10.1016/j.rmed.2020.105980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Karimi-Zarchi M, Neamatzadeh H, Dastgheib S, Abbasi H, Mirjalili S, Behforouz A, Ferdosian F, Bahrami R. Vertical transmission of coronavirus disease 19 (COVID-19) from infected pregnant mothers to neonates: a review. Fetal Pediatr Pathol. 2020;39(3):246–250. doi: 10.1080/15513815.2020.1747120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.López M, Gonce A, Meler E, Plaza A, Hernández S, Martinez-Portilla R, Cobo T, García F, Gómez Roig M, Gratacós E, Palacio M, Figueras F. Coronavirus disease 2019 in pregnancy: a clinical management protocol and considerations for practice. Fetal Diagn Ther. 2020;47(7):519–528. doi: 10.1159/000508487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Liu H, Wang L, Zhao S, Kwak-Kim J, Mor G, Liao A. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. J Reprod Immunol. 2020;139:103122. doi: 10.1016/j.jri.2020.103122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, Xia S, Zhou W. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Translat Pediatr. 2020;9(1):51–60. doi: 10.21037/tp.2020.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Breslin N, Baptiste C, Gyamfi-Bannerman C, Miller R, Martinez R, Bernstein K, Ring L, Landau R, Purisch S, Friedman A, Fuchs K, Sutton D, Andrikopoulou M, Rupley D, Sheen J, Aubey J, Zork N, Moroz L, Mourad M, Wapner R, Simpson L, D’Alton M, Goffman D. Coronavirus disease 2019 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol MFM. 2020;2(2):100118. doi: 10.1016/j.ajogmf.2020.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dong L, Tian J, He S, Zhu C, Wang J, Liu C, Yang J. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020;323(18):1846–1848. doi: 10.1001/jama.2020.4621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zeng H, Xu C, Fan J, Tang Y, Deng Q, Zhang W, Long X. Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA. 2020;323(18):1848–1849. doi: 10.1001/jama.2020.4861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chen S, Huang B, Luo DJ, Li X, Yang F, Zhao Y, Nie X, Huang BX. Pregnancy with new coronavirus infection: clinical characteristics and placental pathological analysis of three cases. Zhonghua Bing Li Xue Za Zhi. 2020;49(5):418–423. doi: 10.3760/cma.j.cn112151-20200225-00138. [DOI] [PubMed] [Google Scholar]
- 94.Alfaraj S, Al-Tawfiq J, Memish Z. Middle East respiratory syndrome coronavirus (MERS-CoV) infection during pregnancy: report of two cases & review of the literature. J Microbiol Immunol Infect. 2019;52(3):501–503. doi: 10.1016/j.jmii.2018.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Elsenbruch S, Benson S, Rücke M, Rose M, Dudenhausen J, Pincus-Knackstedt M, Klapp B, Arck P. Social support during pregnancy: effects on maternal depressive symptoms, smoking and pregnancy outcome. Hum Reprod. 2006;22(3):869–877. doi: 10.1093/humrep/del432. [DOI] [PubMed] [Google Scholar]
- 96.Mignacca FG. With maternity ward off-limits to partners, a mother-to-be struggles with fear and uncertainty. Available at: https://www.cbc.ca/news/canada/montreal/jgh-maternitycoronavirus-rule-1.5522380. Retrieved April 10, 2020.
- 97.MacMillan S. COVID-19 an added stress for Sudbury woman preparing to give birth. Available at: https://www.cbc.ca/news/Canada/sudbury/sudbury-covid-19-pregnancy-1.5519433. Retrieved April 10, 2020.
- 98.McMillan A. Pandemic pregnancies prove stressful as COVID-19 questions remain unanswered. Available at: https://globalnews.ca/news/6733471/covid19-pandemic-pregnancyquestions/.Retrieved April 10, 2020.
- 99.Mor G, Cardenas I. The immune system in pregnancy: a unique complexity. Am J Reprod Immunol. 2010;63(6):425–433. doi: 10.1111/j.1600-0897.2010.00836.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Neggers Y. The association between viral infections, maternal and fetal mortality/morbidity. Glob J Reprod Med. 2018;4(2):555638. [Google Scholar]
- 101.Lam C, Wong S, Leung T, Chow K, Yu W, Wong T, Lai S, Ho L. A case-controlled study comparing clinical course and outcomes of pregnant and non-pregnant women with severe acute respiratory syndrome. BJOG. 2004;111(8):771–774. doi: 10.1111/j.1471-0528.2004.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647–7. [DOI] [PubMed]
- 103.Shanes E, Mithal L, Otero S, Azad H, Miller E, Goldstein J. Placental pathology in COVID-19. Am J Clin Pathol. 2020;154(1):23–32. doi: 10.1093/ajcp/aqaa089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Weiner E, Feldstein O, Tamayev L, Grinstein E, Barber E, Bar J, Schreiber L, Kovo M. Placental histopathological lesions in correlation with neonatal outcome in preeclampsia with and without severe features. Pregnancy Hypertens. 2018;12:6–10. doi: 10.1016/j.preghy.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 105.Taylor R, Roberts J, Cunningham F and Lindheimer M. Immunology of Normal Pregnancy and Preeclampsia. Chesley"s Hypertensive Disorders In Pregnancy. 2014;4(8):161–179.
- 106.Xia Y, Kellems R. Angiotensin receptor agonistic autoantibodies and hypertension. Circ Res. 2013;113(1):78–87. doi: 10.1161/CIRCRESAHA.113.300752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kim J, Kim Y. Acute Atherosis of the uterine spiral arteries: Clinicopathologic implications. J Pathol Transl Med. 2015;49(6):462–471. doi: 10.4132/jptm.2015.10.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hansen J, Hine J, Strout T. COVID-19 and preeclampsia with severe features at 34-weeks gestation. Am J Emerg Med. 2020;39:252.e3–252.e5. doi: 10.1016/j.ajem.2020.06.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jing Y, Run-Qian L, Hao-Ran W, Hao-Ran C, Ya-Bin L, Yang G. And Fei Chen. Potential influence of COVID-19/ACE2 on the female reproductive system. Mol Hum Reprod. 2020;26(6):367–373. doi: 10.1093/molehr/gaaa030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Abbas AM, Ahmed OA, Shaltout AS. COVID-19 and maternal pre-eclampsia: a synopsis. Scand J Immunol. 2020;92(3):e12918. doi: 10.1111/sji.12918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yan R, Zhang Y, Li Y, Xia L, Guo Y, Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020;367(6485):1444–1448. doi: 10.1126/science.abb2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Lau S, Guild S, Barrett C, Chen Q, McCowan L, Jordan V, Chamley L. Tumor necrosis factor-alpha, Interleukin-6, and Interleukin-10 levels are altered in preeclampsia: a systematic review and meta-analysis. Am J Reprod Immunol. 2013;70(5):412–427. doi: 10.1111/aji.12138. [DOI] [PubMed] [Google Scholar]
- 113.Uludag SZ, Karasu AFG, Kutuk MS, Takmaz T. Incidence and outcomes of eclampsia: a single-center 30-year study. Hypertens Pregnancy. 2019;38(2):119–123. doi: 10.1080/10641955.2019.1590719. [DOI] [PubMed] [Google Scholar]
- 114.Rolnik D. Can COVID-19 in pregnancy cause preeclampsia? BJOG Int J Obstet Gynaecol. 2020. Available from. 10.1111/1471-0528.16339.
- 115.Mendoza M, Garcia-Ruiz I, Maiz N, Rodo C, Garcia-Manau P, Serrano B, et al. Pre-eclampsia-like syndrome induced by severe COVID-19: a prospective observational study. BJOG Int J Obstet Gynaecol. 2020. Available from. 10.1111/1471-0528.16339. [DOI] [PMC free article] [PubMed]
- 116.Turpin CA, Sakyi SA, Owiredu WKBA, Ephraim RKD, Anto EO. Association between adverse pregnancy outcome and imbalance in angiogenic regulators and oxidative stress biomarkers in gestational hypertension and preeclampsia. BMC Pregnancy Childbirth. 2015;15:189. doi: 10.1186/s12884-015-0624-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hung TH, Skepper JN, Burton GJ. In vitro ischemia-reperfusion injury in term human placenta as a model for oxidative stress in pathological pregnancies. Am J Pathol. 2001;159(3):1031–1043. doi: 10.1016/S0002-9440(10)61778-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Lamouroux A, Attie-Bitach T, Martinovic J, Leruez-Ville M, Ville Y. Evidence for and against vertical transmission for SARS-CoV-2 (COVID-19) Am J Obstet Gynecol. 2020;223(1):91.E1–91.E4. doi: 10.1016/j.ajog.2020.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Martines RB, Bhatnagar J, Keating MK, Silva-Flannery L, Muehlenbachs A, Gary J, Goldsmith C, Hale G, Ritter J, Rollin D, Shieh W, Luz KG, Ramos A, Davi HPF, de Oliveria WK, Lanciotti R, Lambert R, Zaki S. Notes from the field: evidence of Zika virus infection in brain and placental tissues from two congenitally infected newborns and two fetal losses–Brazil, 2015. MMWR Morb Mortal Wkly Rep. 2016;65(6):159–160. doi: 10.15585/mmwr.mm6506e1. [DOI] [PubMed] [Google Scholar]
- 120.Ribeiro CF, Silami VG, Brasil P, Nogueira RMR. Sickle-cell erythrocytes in the placentas of dengue-infected women. Int J Infect Dis. 2012;16(1):72. doi: 10.1016/j.ijid.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 121.Algarroba G, Rekawek P, Vahanian S, Khullar P, Palaia T, Peltier M, Chavez M, Vintzileos A. Visualization of SARS-CoV-2 virus invading the human placenta using electron microscopy. Am J Obstet Gynecol. 2020;223(2):275–278. doi: 10.1016/j.ajog.2020.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Baum J, Duffy HS. Fibroblasts and myofibroblasts: what are we talking about? J Cardiovasc Pharmacol. 2011;57(4):376–379. doi: 10.1097/FJC.0b013e3182116e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Maluleke R. Mid-year Population Estimates [Internet]. Statssa.gov.za. 2020 [cited 19 July 2020]. Available from: https://www.statssa.gov.za/publications/P0302/P03022018.pdf.
- 124.Maternal mortality [Internet]. Who.int. 2020 [cited 21 July 2020]. Available from: https://www.who.int/news-room/fact-sheets/detail/maternal-mortality.
- 125.Laurence J. Why aren’t people living with HIV at higher risk for developing severe coronavirus disease (COVID-19)? AIDS Patient Care STDs. 2020;34(6):247–248. doi: 10.1089/apc.2020.29005.com. [DOI] [PubMed] [Google Scholar]
- 126.Chenneville T, Gabbidon K, Hanson P, Holyfield C. The Impact of COVID-19 on HIV Treatment and Research: A Call to Action. Int J Environ Res Public Health. 2020;17(12):4548. doi: 10.3390/ijerph17124548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.UNAIDS. Global AIDS update 2019- communities at the centre. Geneva, Switzerland : UNAIDS;2019. Available from https://www.unaids.org/sites/default/files/media_asset/2019-global-AIDS-update_en.pdf
- 128.Council HSR | Incidence, Behaviour and Communication Survey, “South African National Prevalence, Incidence, Behaviour and Communication Survey" [Internet]. Hsrca.co.za. 2020 [cited 15 July 2020]. Available from: https://www.hsrca.co.za/en/media -briefs/hiv-aids-stis-and-tb/sabssm-launch-2018v2;2018.
- 129.Davey DJ, Bekker L, Coates TJ, Myer L. Contracting HIV or contracting SAR-CoV-2 (COVID-19) in pregnancy? Balancing the risks and benefits. AIDS Behav. 2020;24:2229–2231. doi: 10.1007/s10461-020-02861-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Singer M. Pathogen-pathogen interaction: a syndemic model of complex biosocial processes in disease. Virulence. 2010;1(1):10–18. doi: 10.4161/viru.1.1.9933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Halkitis PN, Moeller RW, Siconolfi DE, Storholm ED, Solomon TM, Bub KL. Measurement model exploring a syndemic in emerging adult gay and bisexual men. AIDS Behav. 2013;17(2):662–673. doi: 10.1007/s10461-012-0273-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kalumba VM, Moodley J, Naidoo TD. Is the prevalence of pre-eclampsia affected by HIV/AIDS? A retrospective case-control study. Cardiovasc J Afr. 2013;24(2):24–27. doi: 10.5830/CVJA-2012-078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Chinen J, Shearer WT. Molecular virology and immunology of HIV infection. J Allergy Clin Immunol. 2002;110(2):189–198. doi: 10.1067/mai.2002.126226. [DOI] [PubMed] [Google Scholar]
- 135.Wang W, Tang J, Wei F. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan, China. J Med Virol. 2020;92(4):441–447. doi: 10.1002/jmv.25689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Morawska L, Tang J, Bahnfleth W, Bluyssen P, Boerstra A, Buonanno G, Cao J, Dancer S, Floto A, Franchimon F, Haworth C, Hogeling J, Isaxon C, Jimenez J, Kurnitski J, Li Y, Loomans M, Marks G, Marr L, Mazzarella L, Melikov A, Miller S, Milton D, Nazaroff W, Nielsen P, Noakes C, Peccia J, Querol X, Sekhar C, Seppänen O, Tanabe S, Tellier R, Tham K, Wargocki P, Wierzbicka A, Yao M. How can airborne transmission of COVID-19 indoors be minimized? Environ Int. 2020;142:105832. doi: 10.1016/j.envint.2020.105832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Fauci A. 22nd International Aids Conference. International AIDS Conference, Amsterdam, The Netherlands [Internet]. Aids2018.org. 2020 [cited 23 August 2020]. Available from: https://www.aids2018.org/Programme/Conference-Programme/Pre-conferences
- 138.Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: How far have we come? J Int AIDS Soc. 2013;16(3Suppl 2):18734. doi: 10.7448/IAS.16.3.18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.VA.gov | Veterans Affairs [Internet]. Hiv.va.gov. 2020 [cited 23 August 2020]. Available from: https://www.hiv.va.gov/patient/diagnosis/OI-prevention.asp.