Abstract
Objectives:
The study objective was to test the effectiveness of a photoaging software (APRILAGE©) intervention based on personalized, vivid illustrations of “smoker's face” among smokers aged 18–24 years of age in Bhubaneswar city through a self-structured questionnaire.
Materials and Methods:
A total of 204 engineering college students were randomized into two groups: intervention and control. A self-structured questionnaire in the form of Google Form was distributed among the participants. The study group participants were photographed using Aprilage® Software. Follow-up data were collected using the same questionnaire at 1-month and 3-month intervals. Statistical Analysis was done using STATA 15 software. Descriptive statistics and the relation between the dependent and independent variables were done using the nonparametric tests of significance. The probability value was kept at 0.05.
Results:
Significant reduction in nicotine dependency, was seen in 64.36% of the study population (P < 0.0001). There was a shift from severely dependent group to moderately or low dependence group in 33% of the study occupants.
Conclusion:
Aging software intervention is contemporary, congenial, and admissible and can be espoused to educate youngsters along with the conventional motivational methods. This method successfully delivers smoking cessation advice to young adults. This novel approach can be implemented in motivating young smokers to quit smoking.
Keywords: Cessation, intervention, tobacco
INTRODUCTION
The tobacco epidemic is one of the monumental public health threats, killing more than 7 million people annually, accounting for 25% of the death among adult men and 5% of the death amongst adult women.[1] Approximately 1.3 billion people are into smoking; and 80% of them or 1.1 billion people are residents of both low- and middle-income developing countries.[2] The World Bank reckons over 82,000–99,000 adolescents and young adults' for smoking regularly. This trend speculates over 250 million tobacco-related deaths among young adults in the following years. While the prevalence of tobacco usage has reportedly declined (29.4%) in various developed countries, it has been discerned to increase (13%) in developing countries such as India.[2] The prevalence of smoking is 8 of every 100 adults (7.8%) aged 18–24 years of age.[3]
The paradigm of smoking has shifted with an increase in the number of women symposiasts and has encouraged researchers to promote tobacco cessation by visualizing the esthetic alterations of smoking tobacco.[2] The artificially aged images evoked a “shocking” response from the participants and were successful in motivating participants to both reduce and quit smoking.[4] Women were seen to be more conscious about their physical appearance compared to male counterparts,[4,5,6] hence it was easier to educate them.
The present study tested the effectiveness of a photo aging software (APRILAGE®) intervention based on personalized, vivid illustrations of the “smoker's face” among smokers belonging to 18–24 years of age in Bhubaneswar city through a self-structured questionnaire. The study hypothesized that software intervention is not effective in motivating the participants to quit smoking. The study assessed the degree of addiction and the magnitude of exposure of the individual to the smoke form of tobacco and whether these two factors are associated with a reduction in tobacco usage.
MATERIALS AND METHODS
A longitudinal, interventional, questionnaire-based, parallel-arm, randomized controlled trial was conducted in the School of Engineering, KIIT University, Bhubaneswar, Odisha, India. The study population included all the four professional Bachelor of Technology (B. Tech) Course who were either established smokers or regular smokers (defined by a total of 100 cigarettes smoked till the day of data collection).[6,7] The variability of the population was attained as students belonged to different states. A total of 250 students both males and females were shortlisted using a survey questionnaire comprehending questions pertaining to sociodemographic variables and the numerical count of cigarettes smoked [Figure 1]. Randomization of the study population was done using the table of random numbers, and the participants were randomly allocated (1:1 ratio) in two groups by an attendant. Participants available up till 3 months from the commencement of the study were included. The students who had body dysmorphia or were on nicotine replacement therapy (NRT) or consuming drugs for nicotine dependence were excluded. A total of 204 participants (160 males and 44 females) consented for the study. Clinical trial Registry: CTRI/2018/12/016703; registered on December 18, 2018. A written informed consent was taken from individual subjects before the commencement of the main study.
Figure 1.
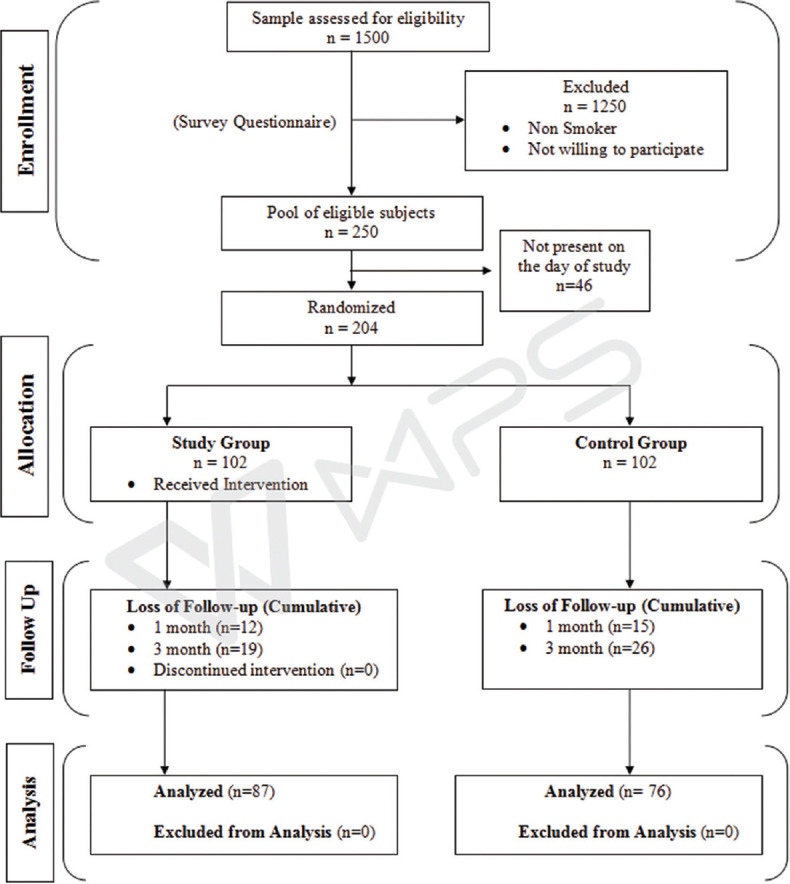
Consort flowchart for randomized controlled trial
The participants were given a validated self-structured questionnaire in the form of Google Form; shared through e-mail. The associates were randomly allocated (1:1 ratio) in two groups. The study group received software intervention along with the questionnaire, whereas the control group completed the questionnaire solely. The questionnaire comprised of thirty questions divided into five sections: measure of the smoking count; with options ranging from 1 to 15. Fagerstrom Test for nicotine dependence;[8] questions related to the appearance of the person; a 5-point Likert scale with options such as highly, moderately a little, not at all, and I don't know. Opinions on the effect on health; with dichotomous options yes or no. Perceived barriers to quit smoking included a 5-point Likert scale with options such as strongly agree, agree, don't know, disagree, and strongly disagree. The reliability coefficient (Cronbach's alpha α) value was 0.837 which indicated good internal consistency.
Software details
The APRIL® Face Aging software[9] is an internet-based three-dimensional age progression software package that creates a stream of aged images of faces from a standard digital photograph The validity of the software has been proved in various Brazilian studies conducted using this software.[8,9,10,11,12,13,14,15] The authors had been permitted to use the software only for research purposes.
A pilot study was conducted with n = 40 among the engineering students to analyze the face validity and the feasibility of the study. The content validation was done by a panel of 5 experts. Participation was voluntary and written informed consent was taken. Electronically consent was obtained. The Google Forms had options for consent. Once the participants clicked the option “Yes, I want to continue,” the questionnaire opened. The study was approved by the Institute Ethics Committee (KIMS/KIIT/IEC/33/2018). The study is in accordance with the Helsinki guidelines (1975). This was registered under the Clinical Trial Registry of India (CTRI/2018/12/016703).
formula:
Ho: P1= P2; H1: P1≠P2
N = {Z1-a/2 √ [2 P¯ (1 − P¯) + Z1- β √ P1 (1 − P1) + P2 (1 − P2)}2/(P1− P2)2
P1- Proportion of moderately dependent subjects in the intervention group: 0.138
P2- Proportion of moderately dependent subjects in the control group: 0.013
α - Significance level = Alpha error = 5%; 1 – β = Power = 80%
Minimum sample size required for each group: 69.
The final sample size was rounded off to 102 in each group. This excluded the participants of the pilot study.
The study was conducted from December 2018–March 2019. The study group members were asked to congregate at an open-air-theater in the college premises where under adequate natural light pictures were taken using the APRIL Age® Software. The images were digitally aged for both smoker and nonsmoker [Figure 2]. After the intervention, 2-min motivational advice was given to the conventioneer about the health effects of tobacco consumption. The digitally aged photograph was e-mailed to them within 24 h of the intervention. Follow-up surveys were undertaken using the same questionnaire via e-mail conversations at 1 and 3 months with a reminder if they failed to respond within 5 days of the due response date.
Figure 2.

The illustrations of age change by the software
Those who stated to have either reduced the frequency of smoking (from severely dependency to moderate or low; or from moderate dependency to low) or have quit smoking were required within 48 h to undertake a carbon monoxide (CO) breath test to validate their transit.
Data were entered using Microsoft Excel (version 2016) and then checked for any missing entries. It was analyzed using STATA version 15 (College Station, Texas: Stata Press. StataCorp. 2015). Descriptive statistics were presented with mean ± standard deviation or median (interquartile range) for continuous variables depending on their distribution. Categorical variables were described using frequency and percentages. A Chi-square test was used for measuring the association between two independent groups. Stuart Maxwell or trend analysis was used to find the association of categorical variables over time. To compare the continuous factors between the study group t-test or Wilcoxon rank-sum test was used depending on the distribution. Kruskal–Wallis test was used to analyze the continuous nonparametric data of the population at one point in time. Intragroup comparison of various domain scores was done using the Friedman test. Intergroup comparison of various domain scores at different follow up points was done using the Mann–Whitney U-test. The confidence interval was kept at 95%. The level of statistical significance was set at 0.05.
RESULTS
The mean age of the participants was 21 ± 0.86 years. Figure 2 shows the facial changes due to smoking. It was stated that the aging images were shocking by 13.7% of the population at baseline, which changed to 12.2% at 1st follow up and 21.7% at 2nd follow up. At baseline, 34.3% of the study population didn't find the images shocking which reduced to 21.7% at 2nd follow-up. A very high statistical significant relation was found in the study group from baseline to 3rd follow up (P < 0.0001). The differences in the mean scores at three points of time were statistically highly significant (P < 0.0001). Table 1 denotes the change in the nicotine dependence scores over 3 months' time.
Table 1.
The Fagerstrom Nicotine Dependence score comparisons
| Study group | Control group | χ2 | P | |||||
|---|---|---|---|---|---|---|---|---|
| Low | Moderate | Severe | Low | Moderate | Severe | |||
| Baseline, n (%) | 43 (42.2) | 48 (47.1) | 11 (10.8) | 50 (49.0) | 41 (40.2) | 11 (10.8) | 1.1 | 0.58 |
| At 1st follow up, n (%) | 51 (56.7) | 30 (33.3) | 9 (10.0) | 50 (57.5) | 28 (32.2) | 9 (10.4) | 0.1 | 0.98 |
| At 2nd follow up, n (%) | 63 (75.9) | 20 (24.1) | 0 (0.0) | 48 (63.2) | 22 (28.9) | 6 (7.9) | 7.8 | 0.02* |
*Statistically significant (Kruskal–Wallis Test)
The mean scores of the opinions of the effects of smoking on health and oral health were recorded at baseline (4.57 ± 1.35) for the study group and (4.57 ± 1.35) for the control group. There was mild improvement in the mean scores at 1st follow-up in the study group (4.57 ± 1.39) while there was a reduction in mean scores in the control group (4.59 ± 1.41). The difference between both groups was not statistically significant (P = 0.901). The mean scores were refined in the 3rd follow up; study group (4.33 ± 0.94) and control group (4.28 ± 1.29). The intra-group comparison at baseline and follow-ups was found to be significant in both the study group (P = 0.002) and the control group (P < 0.0001). The perceived barrier domain scores were noted to be improved at the end of the 3 months' follow-up, and it was seen that feeling tense and irritable was the most common predicted barrier in quitting smoking.
DISCUSSION
The present study investigates the effectiveness of Aprilage® Photo aging software (Ontario Science Centre (OSC), Toronto, Canada) in motivating 18–24-year-old adult smokers for smoking cessation. Although there was only one subject with the established cessation of smoking, other participants manifested a significant reduction in smoking dependency (34%). A bio-chemical confirmatory test using a CO breath analyzer was performed to validate smoking dependency. The digitally aging software intervention successfully demonstrated that the photo-aging intervention had larger leverage on participants belonging to 18–24 years.[16] The prevalence of male smokers in the present study was higher as compared to other studies conducted by various authors.[2,13,14] Hyset[4] proposed aging images to be a promising approach for educating women aged 18–24 years about the aesthetic alterations of smoking. This study is similar to a study by Weiss et al.[16] where 21.7% of the population believed the aging images were “shocking.” Grogan et al.[6] reported that 100% of the participants in his study intercepted the aging images to be shocking and 67% of them were willing to quit smoking. A statistically significant (P < 0.0001) reduction in the Fagerstrom score[17] was seen over a period of 3 months in the study group indicating an improvement in the dependence on smoking. The audio-visual presentation of ill effects of smoking on health and oral health might be a reason for a reduction in the Fagerstrom scores among control group participants. Studies hence revealed that young people are more reluctant to give up smoking, possibly due to greater addiction to nicotine.[18] The most common reason for failure of smoking prevention and cessation programs among young adult smokers is that they are less likely to be concerned about the health risks of smoking than older smokers.[19] In the present study, 54.2% of the study population made multiple quit attempts and 41% at least one and was in conformity with Reddy et al. (34.4%)[20] and Susan (54%).[21] The Fagerstrom Nicotine dependence scale is a validated reliable measure of nicotine dependence.[22,23,24] Gravitates of smoking behavior were found to ameliorate from severely dependent group to low dependent group (31%) after the 2nd follow-up. Copious studies have been conducted for determining perceived barriers in quitting smoking.[9,24,25,26] The present study identifies “feeling tense and irritable” as the most delineated barrier among 18–24-year-old engineering students to quit smoking with an Odds ratio of 3.2. The second most common barrier was “fear of gaining weight.” These two barriers are established symptoms of nicotine withdrawal according to previous studies.[24]
At 3 months' follow-up, of all who stated to have reduced the number of cigarettes or had reportedly quit smoking were required to take a CO breath-test for chemical-clinical validation. Only six of them gave consent. Fewer subjects were amenable for CO breath analysis probably because they continued to smoke in a similar pattern or they were absent at the time of confirmatory analysis. Nevertheless, the self-reported smoking status data are interesting and although likely to be prone to socially desirable responses, the effect size (0.002) is still substantial and on par with other interventional trials. The study can be extrapolated to a similar high risk group (young smokers of 18–24 years). The intervention used has already been proven to be effective in motivating the participants to quit smoking. The biological gradient of the intervention is mentioned in Table 1. The intervention cohers with both the epidemiological and clinical findings. There exists a causal relationship between the exposure i.e., the photographic imaging intervention and the outcome i.e., the advantage gained in reducing the clinical nicotine dependency of the participants. Technologies including internet, social networking sites, and smartphones have the potential to reach large young populations.[24]
This method of smoking cessation can be incorporated in the traditional method of 5As – Ask, Assess, Advice, Assist and Arrange. Visualizing age changes would help to improve the level of motivation of the patient in smoking cessation. Adjuncts with NRT including nicotine gum, nasal spray, oral inhaler, and pharmacological alternatives could improve the outcome of smoking cessation. The clinical relevance of this smoking cessation method includes a long term and efficient results as it works through the contemplation stage of behavior modification.
Limitations
The attrition (14.7%) among the study population could be because of a lack of interest to continue the study, lack of time and casual attitude of the participants towards quitting smoking. There was a substantial increase in the risk of contamination between study and control group participants due to the long duration of the study and the open recruitment of the participants from the same boarding house. This could have led to similar reporting of the answers and generalized response to the questionnaire. The participants and researcher could not be blinded to the study group because of the nature of the study. An improved multi-centric trial could be conducted for a better generalizability of the results.
CONCLUSION
This study presents a novel approach to integrating photo-aging software APRILAGE® in smoking prevention among young individuals. This method is new-fangled, amusing and admissible by the smokers in delivering smoking cessation advice compared to other methods. The association between the attitude towards quitting smoking and knowledge regarding the effects of health has been clearly established. Thus, it can be deduced that this method of delivering smoking cessation advice to the age group of 18–24 years is one of its kind and can be implemented in tobacco cessation cells.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank Mr. Ron Ester, Manager, Aprilage Face ageing Software, for giving permission to conduct an interventional study using the software.
REFERENCES
- 1.Janeswar A, Kumar G, Kanungo S, Singh A, Subramanya GB, Jha K. Prevalence patterns and profile of adolescent tobacco users findings from a youth survey: A cross-sectional study. J Family Med Prim Care. 2019;8:2017–22. doi: 10.4103/jfmpc.jfmpc_219_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roy P, Goel S. Is female smoking rising or declining in India? South Asian J Cancer. 2015;4:99–100. doi: 10.4103/2278-330X.155702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. [Last accessed on 2020 Jan 27]. Available from: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm#anchor_1549902047693 .
- 4.Treloar Padovano H, Merrill JE, Colby SM, Kahler CW, Gwaltney CJ. Affective and situational precipitants of smoking lapses among adolescents. Nicotine Tob Res. 2020;22:492–7. doi: 10.1093/ntr/ntz002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hysert PE, Mirand AL, Giovino GA, Cummings KM, Kuo CL. At face value: Age progression software provides personalised demonstration of the effects of smoking on appearance. Tob Control. 2003;12:238. doi: 10.1136/tc.12.2.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grogan S, Fry G, Gough B, Conner M. Smoking to stay thin or giving up to save face? Young men and women talk about appearance concerns and smoking. Br J Health Psychol. 2009;14:175–86. doi: 10.1348/135910708X327617. [DOI] [PubMed] [Google Scholar]
- 7.Brinker TJ, Brieske CM, Esser S, Klode J, Mons U, Batra A, et al. A face-aging app for smoking cessation in a waiting room setting: Pilot study in an HIV outpatient clinic. J Med Internet Res. 2018;20:e10976. doi: 10.2196/10976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burford O, Kindarji S, Parsons R, Falcoff H. Using visual demonstrations in young adults to promote smoking cessation: Preliminary findings from a French pilot study. Res Social Adm Pharm. 2018;14:398–400. doi: 10.1016/j.sapharm.2017.04.050. [DOI] [PubMed] [Google Scholar]
- 9.Aprilage Face Ageing Software. [Last accessed on 2018 Jan 05]. Available from: https://aprilagecom/
- 10.Brougham R, John R, Sparks R, Cogan L, Breit C, Dietch K, et al. Photo aging, future time perspective and social smoking Conference: Association for Psychological SciencesAt. Boston, MA: 2010. [Last accessed on 2020 Sep 10]. Available from https://wwwresearchgatenet/publication/263467356_Photo_aging_future_time_perspective_and_social_smoking . [Google Scholar]
- 11.Cheetham I, Ogden J. Enhancing sun safety in young women: The relative impact of format and temporal framing on beliefs and behaviour. Cogent Psychology. 2016;3:1210069. [Google Scholar]
- 12.Flett K, Grogan S, Clark-Carter D, Gough B, Conner M. Male smokers' experiences of an appearance-focused facial-ageing intervention. J Health Psychol. 2017;22:422–33. doi: 10.1177/1359105315603477. [DOI] [PubMed] [Google Scholar]
- 13.Burford O, Jiwa M, Carter O, Parsons R, Hendrie D. Internet-based photoaging within Australian pharmacies to promote smoking cessation: Randomized controlled trial. J Med Internet Res. 2013;15:e64. doi: 10.2196/jmir.2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grogan S, Flett K, Clark-Carter D, Conner M, Davey R, Richardson D, et al. A randomized controlled trial of an appearance-related smoking intervention. Health Psychol. 2011;30:805–9. doi: 10.1037/a0024745. [DOI] [PubMed] [Google Scholar]
- 15.At Face Value: A Survey of Self-Image and Health Behavior. Department of Health Behavior Division of Cancer Prevention and Population Sciences. 2008 [Google Scholar]
- 16.Weiss C, Hanebuth D, Coda P, Dratva J, Heintz M, Stutz EZ. Aging images as a motivational trigger for smoking cessation in young women. Int J Environ Res Public Health. 2010;7:3499–512. doi: 10.3390/ijerph7093499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fagerström K. Time to first cigarette; the best single indicator of tobacco dependence? Monaldi Arch Chest Dis. 2003;59:91–4. [PubMed] [Google Scholar]
- 18. [Last assessed on 2020 Jan 27]. Available from: https://www.who.int/tobacco/publications/gender/women_tob_epidemic/en/
- 19.Xu X, Liu L, Sharma M, Zhao Y. Smoking-related knowledge, attitudes, behaviors, smoking cessation idea and education level among young adult male smokers in Chongqing, China. Int J Environ Res Public Health. 2015;12:2135–49. doi: 10.3390/ijerph120202135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reddy KS, Yadav A, Arora M, Nazar GP. Integrating tobacco control into health and development agendas. Tob Control. 2012;21:281–6. doi: 10.1136/tobaccocontrol-2011-050419. [DOI] [PubMed] [Google Scholar]
- 21.Chaiton M, Diemert L, Cohen JE, Bondy SJ, Selby P, Philipneri A, et al. Estimating the number of quit attempts it takes to quit smoking successfully in a longitudinal cohort of smokers. BMJ Open. 2016;6:e011045. doi: 10.1136/bmjopen-2016-011045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. [Last accessed on 2018 Jun 15]. Available from: https://www.who.int/employment/FAQs_smoking_English.pdf .
- 23.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The fagerström test for nicotine dependence: A revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 24.Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: A systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4:e006414. doi: 10.1136/bmjopen-2014-006414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Falomir-Pichastor JM, Blondé J, Desrichard O, Felder M, Riedo G, Folly L, et al. Tobacco dependence and smoking cessation: The mediating role of smoker and ex-smoker self-concepts. Addictive Behaviors. 2020 Mar;102:106200. doi: 10.1016/j.addbeh.2019.106200. DOI: 101016/jaddbeh2019106200. [DOI] [PubMed] [Google Scholar]
- 26.Joveini H, Rohban A, Eftekhar Ardebili H, Dehdari T, Maheri M, Hashemian M. The effects of an education program on hookah smoking cessation in university students: An application of the Health Action Process Approach (HAPA) J Sub Use. 2020;25:62–9. [Google Scholar]


