Abstract
Best medical therapy for peripheral artery disease (PAD) includes statin and anti-platelet agents, a combination shown to decrease rates of major cardiovascular events. Despite these findings, many patients remain undertreated and the objective of this project was to investigate the rate of initiating anti-platelet and statin therapy for inpatients newly diagnosed with PAD with a focus on disparities by race and sex.
A retrospective chart review of inpatients with newly diagnosed PAD was performed between January 1, 2016 to December 31, 2016 at a single institution. Demographics and comorbid conditions were collected. Primary outcomes included antiplatelet and statin prescription at discharge.
The 44 patients included in this study were predominantly male (59% vs. 41%) and African American (61% vs. 39%). Between admission and discharge, prescriptions rose from 70% to 82% for statin and 82% to 91% for anti-platelet agents. Vascular specialists were more successful than non-vascular specialists at initiating medical therapy, with statin prescriptions increasing 22% and anti-platelet prescriptions climbing 23% for those admitted to a vascular specialist. Interestingly, when the ABI was reported in the normal range, rates of statin initiation were particularly compromised at only 40%. For the total patient sample, those discharged without a statin were more commonly African American (63%) and the majority were female (67%). All patients discharged without an antiplatelet were African American and 50% were females.
Despite national guidelines, patients with PAD continue to be discharged without optimal medical therapy. This study suggests that obstacles to initiation may include race, sex, admitting service, or presence of a normal ABI. Further investigation is warranted to determine effective avenues for provider education and system-wide initiatives.
Keywords: Antiplatelet, Statin, Peripheral artery disease
INTRODUCTION
Peripheral arterial disease (PAD), a condition in which blood flow to the limbs is reduced due to narrowing of the blood vessel lumen, develops through the formation of atherosclerotic plaques. Risk factor modification is important in the care of patients with PAD to help reduce morbidity and mortality. Patients with lifestyle-limiting symptoms (claudication, rest pain, or tissue loss) are typically in the care of a vascular specialist and are more likely to receive intense medical therapy with or without peripheral revascularization compared to patients who are asymptomatic. While it is widely quoted that patients with symptomatic PAD have a 70% increased risk of cardiovascular events and 80% increased risk of cardiovascular mortality, both symptomatic and asymptomatic populations have equivalent cardiovascular risks, therefore a lack of symptoms is not protective [1,2]. Specifically, myocardial infarction (MI) occurs 2.5-times more often in all patients with ABI <0.9 when compared to patients without PAD [1].
The Heart Protection Study confirmed the protective effects of statin therapy in patients with PAD, establishing an 18% reduction in coronary death rate in patients with arterial disease treated with statins [3]. As a result, in 2014, the Society for Vascular Surgery (SVS) released guidelines recommending the application of statin therapy in all patients with a 10-year Atherosclerotic Cardiovascular Disease (ASCVD) risk of >7.5%, thus including all patients with PAD [4]. Likewise, the American College of Cardiology recommends treating all patients with clinical ASCVD, encompassing patients with PAD and those age 40–75 with diabetes mellitus or a 10-year ASCVD of >7.5% and LDL > 70mg/dL [5]. Statin therapy has been effective through stabilization of atherosclerotic plaques, improving endothelial function, and enhancing blood flow in the microcirculation [6,7]. The pleiotropic effects of these cholesterol-lowering agents have included decreased recruitment of inflammatory markers to plaque sites and shifting the coagulation pathway toward thrombolysis, thereby decreasing clinical risk for adverse vascular events [7]. In patients with intermittent claudication and on statin therapy, significant improvement in the total walking distance and pain free walking time was observed [8,9]. Additionally, PAD patients on statin therapy require less interventions and experience an increase in amputation free survival [3,10]. The cardio protective effects delivered by statin therapy make initiation a crucial secondary prevention method in patients with atherosclerotic disease.
Optimal medical therapy for patients with PAD also includes daily aspirin. Aspirin acts by irreversibly inhibiting platelet function and pro-inflammatory enzymes, thereby interrupting the clotting cascade and reducing inflammatory markers. Although low-dose aspirin for primary prevention has been controversial, when used to slow disease progression it results in a decrease in serious vascular events (6.7% per year) when compared to the control group (8.2% per year) [11]. Likewise, numerous studies have shown reduction in cardiovascular mortality with administration of aspirin in patients with lower extremity atherosclerotic disease, therefore the American Heart Association (AHA) promotes doses of 75 to 325 mg per day as a Class IA recommendation [4]. Despite a tradeoff between increased risk for bleeding and thrombotic prevention, aspirin’s durable anti-platelet properties have made it a dependable staple in the modern physician’s toolbox.
The strong evidence for increased survival in PAD patients who receive optimal medical therapy has been validated through the Vascular Quality Initiative, which has acknowledged that discharge ought to include maintaining or initiating prescriptions for both antiplatelet agents and statins [12]. The SVS guidelines recommend more direct standards for prescribing, calling for the consideration of statin and antiplatelet adjunct therapy in patients undergoing exercise regimens for intermittent claudication [4]. The guidelines also dictate the use of statins in patients who undergo interventions for lower extremity vascular disease, noting that aggressive medical therapy is encouraged to combat already-present systemic atherosclerotic disease [4]. Despite these initiatives, it is clear that patients with PAD continue to leave the hospital without statin or antiplatelet therapy.
In addition to provider awareness and patient compliance, race and sex play a notable role in access to care as well as quality of care. Current studies suggest the PAD burden in African American patients is higher than that of Caucasian patients (15.6% vs. 11.4% prevalence) and African American females have the highest prevalence of any racial group at 16.9% [13]. A recent study using the Healthcare Cost and Utilization Project (HCUP) database showed an increased amputation rate in African Americans compared to that of Caucasians, suggesting greater disease on presentation and a lower rate of early intervention [14]. The population of South Carolina has been approximated at 28% African American and this state has also been documented to carry a high rate of limb loss [15]. In a retrospective study performed at the Medical University of South Carolina, Brothers et al. found that African American women were 7.6 times more likely to undergo lower extremity amputation than women of other races [16]. These women were also 1.3 times more likely to undergo this operation than African American men. Because of the influence of racial disparities on healthcare, remedying inequality through preventative prescriptions can have significant benefits for the PAD population.
Since antiplatelet and statin medications have been established as optimal medical therapy for PAD patients, and a cornerstone of early intervention, this study was performed to evaluate sex and race-related compliance with discharge prescriptions for antiplatelet and statin therapy in PAD patients treated at a tertiary care center in South Carolina. It is hypothesized that despite a new diagnosis of PAD and assessment with ankle-brachial index (ABI) during the inpatient stay, patients will continue to be discharged from the hospital without aspirin and statin medications, with disparate rates based on race and sex. These results will allow for the institution of local change and improved PAD care for our community.
MATERIALS AND METHODS
In this single center study, an IRB-approved retrospective chart review of all patients who were admitted as inpatient to Medical University of South Carolina (MUSC) between January 1, 2016 and December 31, 2016 was conducted. Inclusion criteria included patients at least 18 year of age who were receiving inpatient care with a new diagnosis of PAD and completed an ABI study during the admission. A comprehensive chart review was completed to extract patient demographics, comorbidities, admission medications, discharge medications, admitting service, allergy, and smoking status. The primary outcomes of the study were antiplatelet and statin prescriptions at the time of discharge.
RESULTS AND DISCUSSION
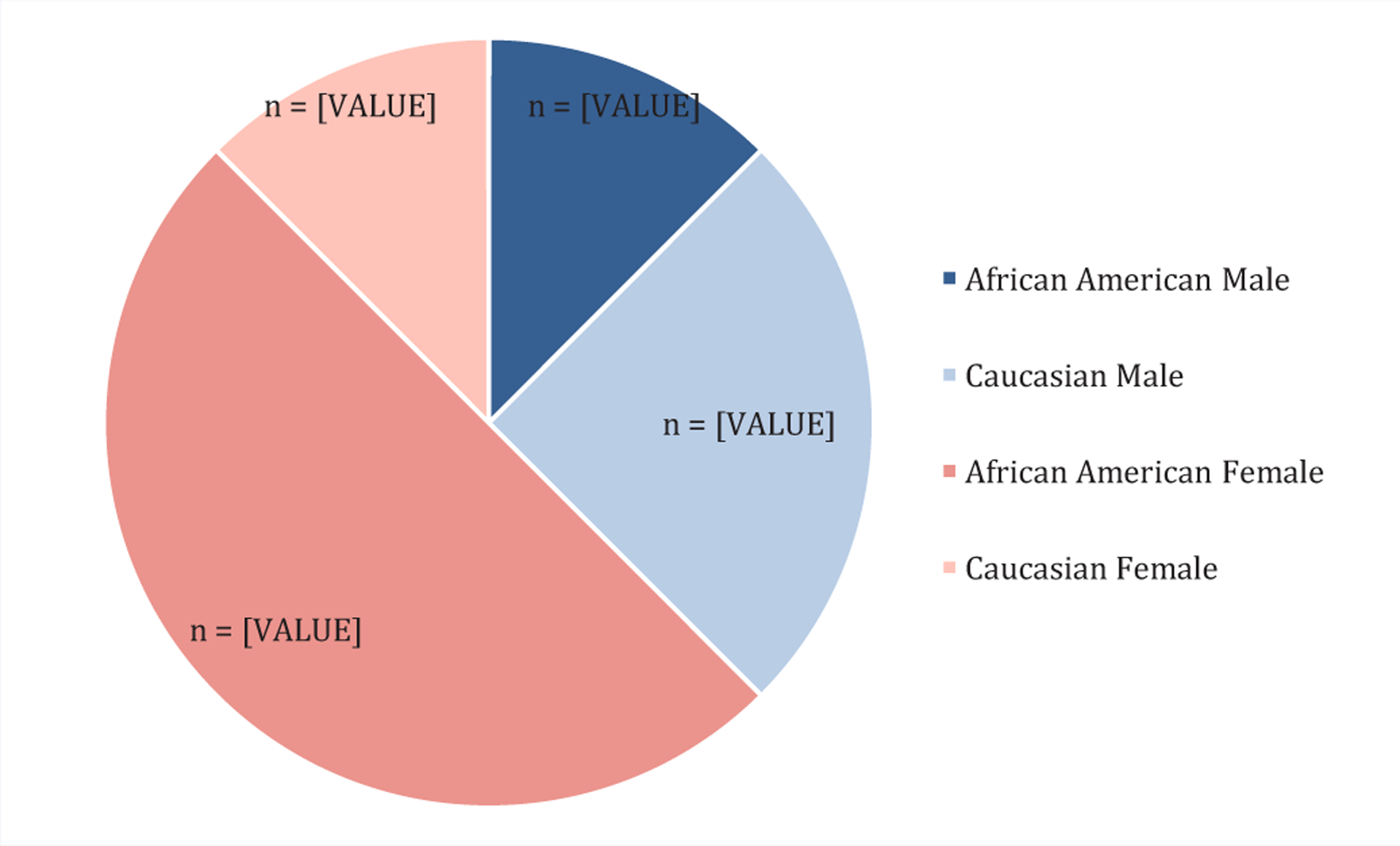
A total of 44 patients met the inclusion criteria for this retrospective review and the average age was 65 +/−22 years. Pertinent medical comorbidities included hypertension, hyperlipidemia, diabetes and chronic kidney disease (Figure 1). Interestingly, less than 50% of this population had been previously diagnosed with coronary artery disease (CAD), a condition which would also warrant optimal medical therapy with aspirin and statin. As demonstrated in Figure 2, the majority of the population was male (59% vs. 41%) and African American (61% vs. 39%). Since cigarette smoking is a known risk factor for atherosclerosis, it was expected that a majority of patients would be current or former smokers (80%).
Figure 1.
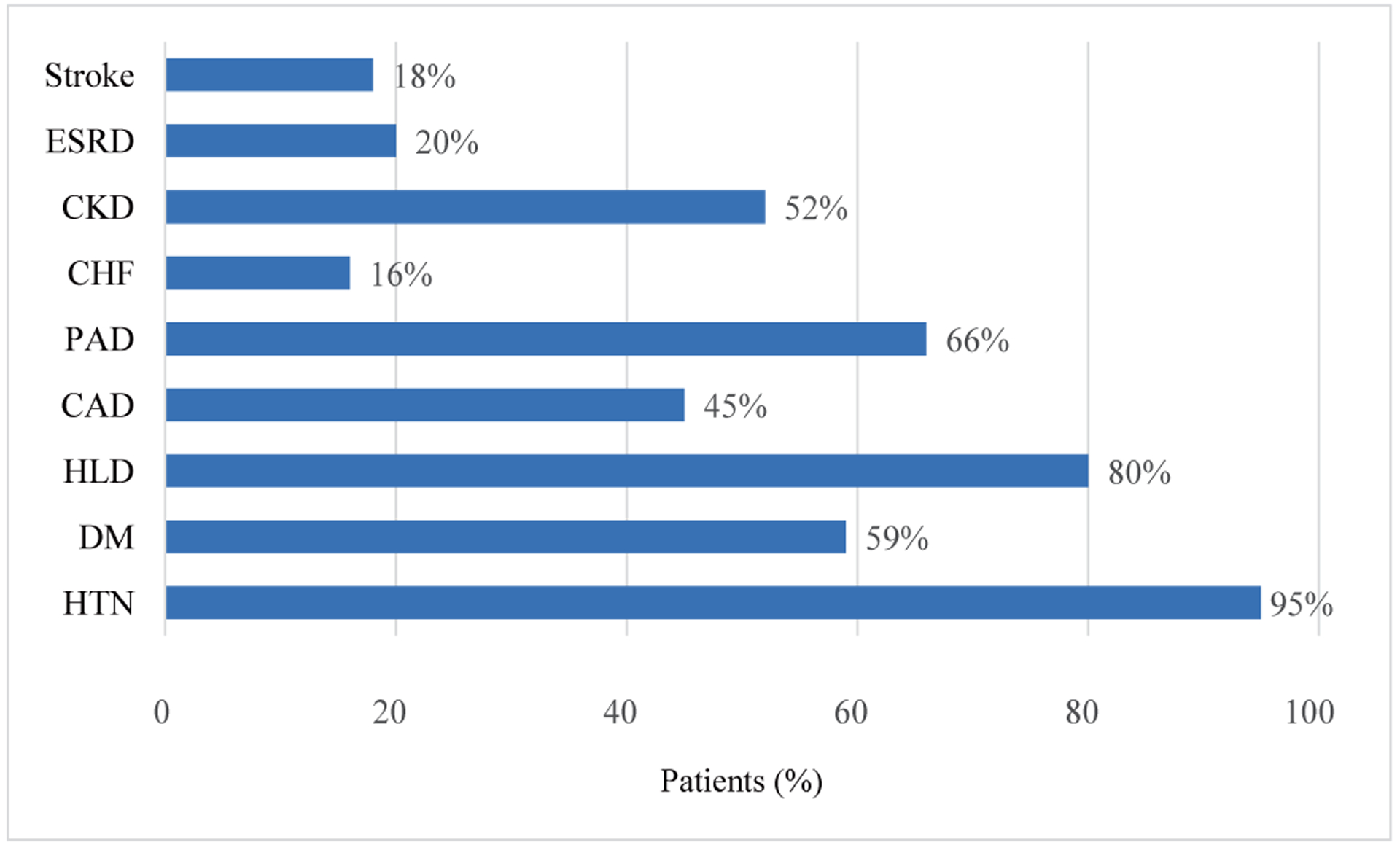
Comorbidities of patients included in this study (n=44).
Figure 2.
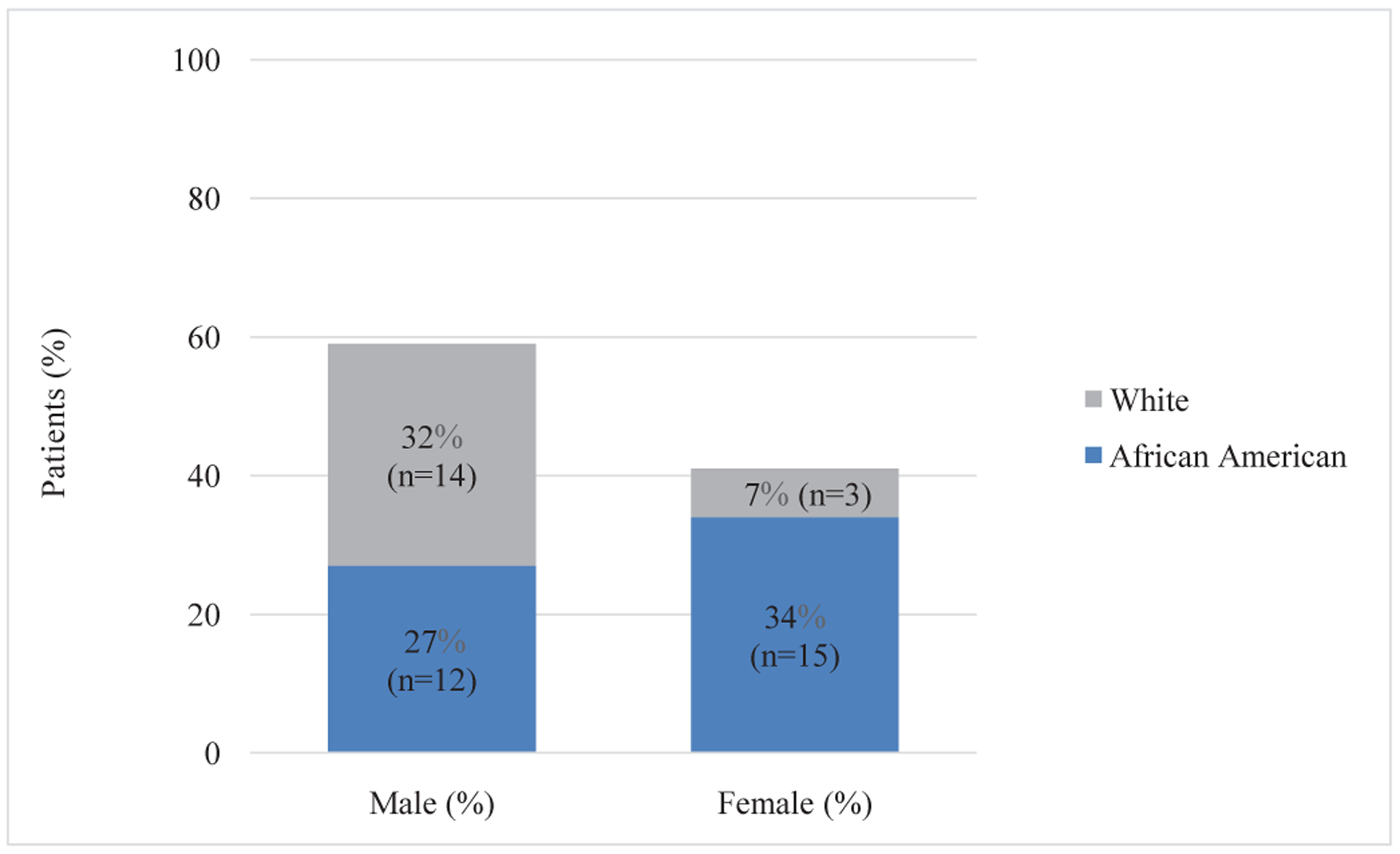
Race and sex distribution of patients in this study (n=44).
An ABI was used to quantify the extent of PAD in our patient population and the results are summarized in Table 1. In the studied population, 38% of males and 78% of females had an ABI that measured <0.9. Prior major amputations were seen in 27% of males in our cohort with no females affected. A noncompressible artery or not reliable reading was found in 23% of males and 11% of females. In the overall study population, 70% of patients were on a statin and 82% were on an antiplatelet agent at the time of admission, but by discharge, these percentages rose to 82% and 91%, respectively (Figure 3). Though a notable increase, our institution failed to reach the recommended goal of 100%, thus confirming that efforts ought to be directed toward this initiative.
Table 1:
Ankle Brachial Index.
| Males (n = 26) | Females (n = 18) | |
|---|---|---|
| ABI >0.9 | 12% (n = 3) | 11% (n = 2) |
| ABI <0.9 | 38% (n = 10) | 78% (n = 14) |
| Major Amputation | 27% (n =7) | 0 |
| Noncompressible, not reliable | 23% (n = 6) | 11% (n = 2) |
Abbreviations: ABI: Ankle-brachial index
Figure 3.
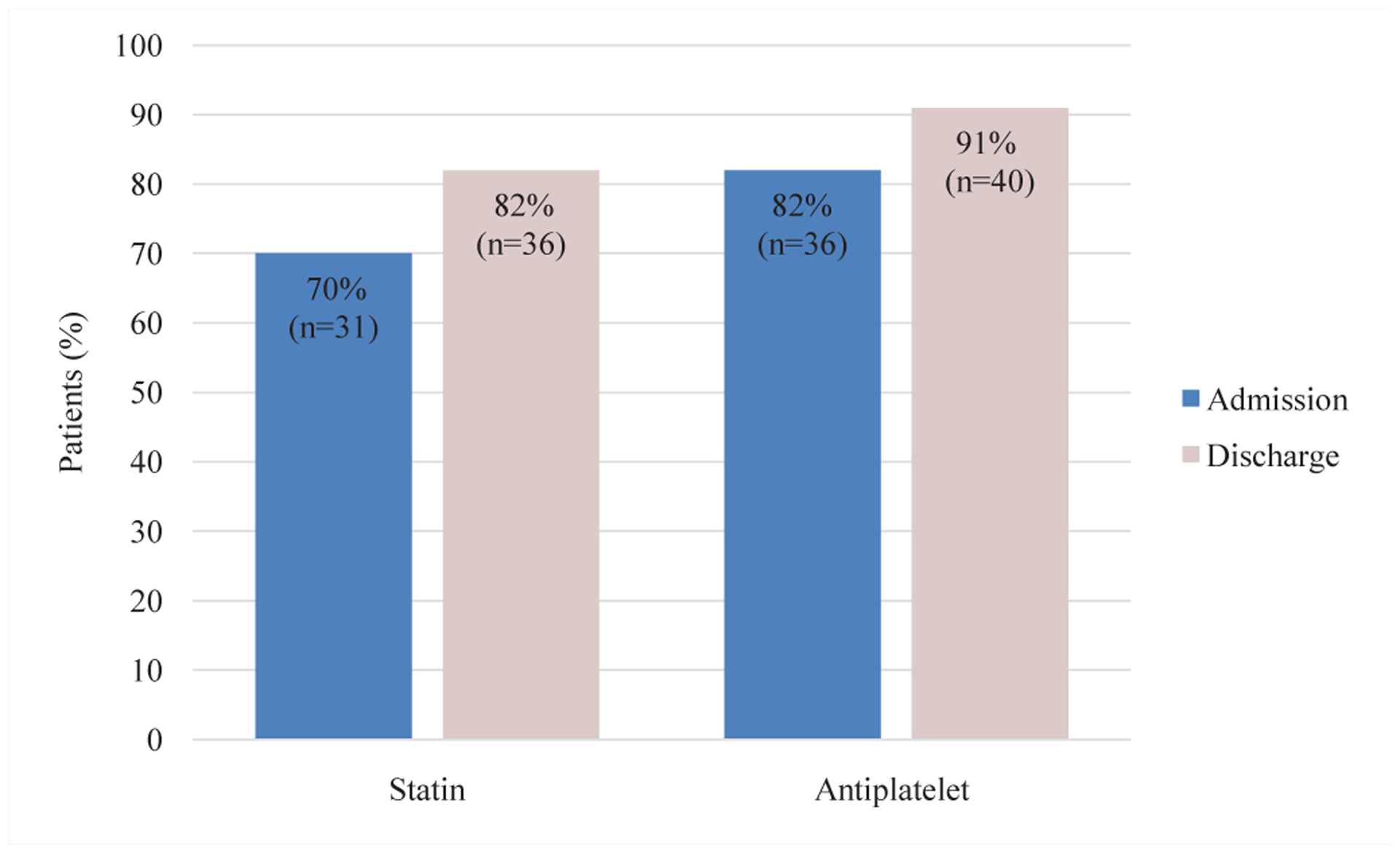
Percentage of patients with PAD (n=44) who were admitted and discharged with statin and antiplatelet therapy.
Admitting services were separated into vascular vs. non-vascular specialties and prescription outcomes were found to vary between the two. On the vascular services (Cardiology and Vascular Surgery), statin prescriptions rose 22%, from 65% to 87% between admission and discharge. On this same service, 74% of patients were admitted on an antiplatelet and 97% were discharged with a prescription, representing a 23% increase (Figure 4a). Unfortunately, on the non-vascular services, discharge medications trended downward. From admission to discharge, statin prescriptions fell from 85% to 69% and antiplatelet prescriptions decreased from 85% to 77% (Figure 4b).
Figure 4.
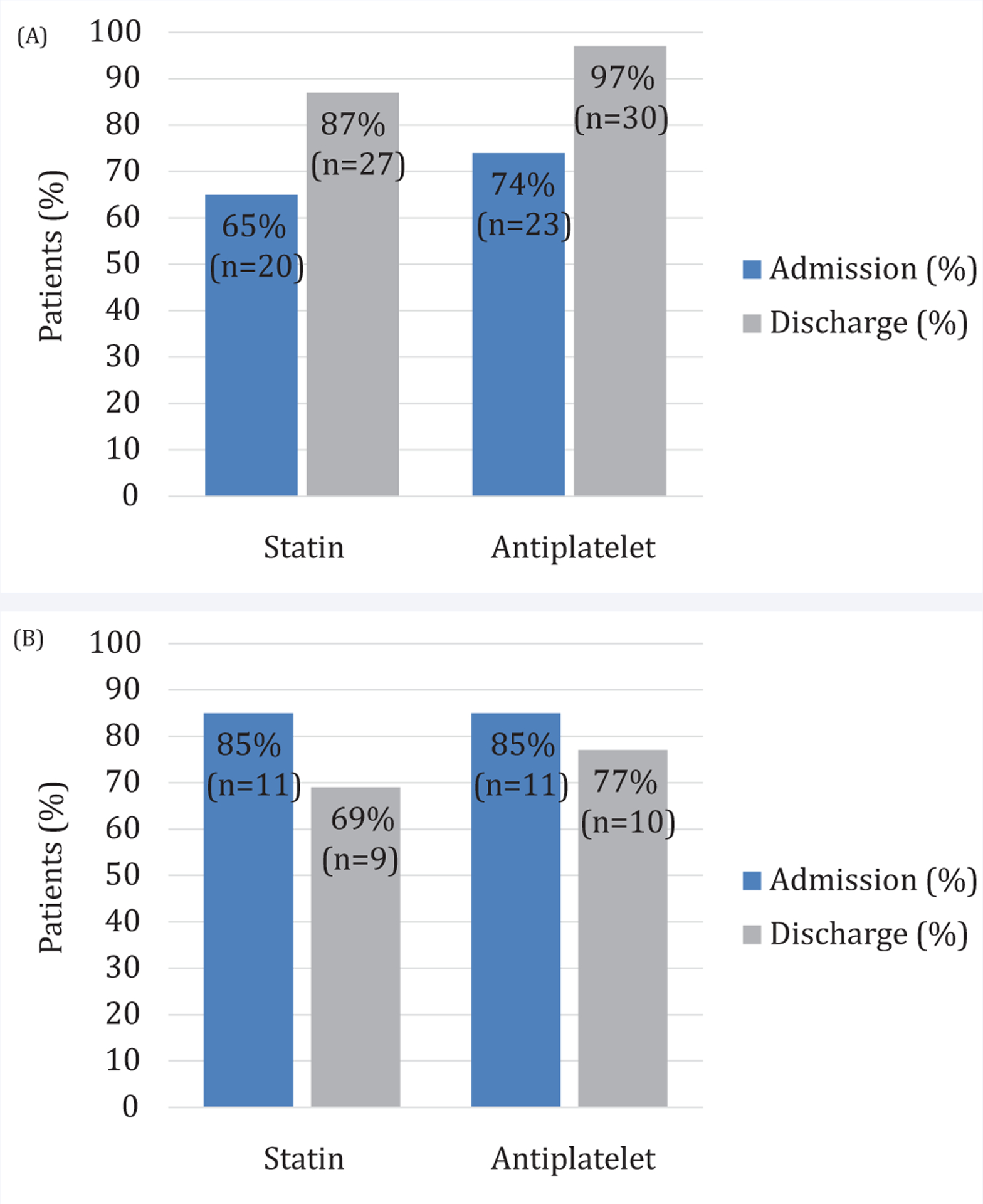
(A) - Distribution of success in vascular specialties at statin and anti-platelet prescriptions between admission and discharge. (B) - Distribution of success in non-vascular specialties at statin and anti-platelet prescriptions between admission and discharge.
Since ABI can be considered as an indication of PAD severity, patients with worse ABIs often demonstrate more obvious need for adjunctive medical therapy, but all PAD patients benefit from optimal medical therapy. In patients with normal ABI reading and a new diagnosis of PAD, 40% were discharged from the hospital with a statin (Figure 5a) and 80% with an antiplatelet prescription (Figure 5b), suggesting that normal ABI may dissuade providers from administering best medical therapy, particularly statin. In patients with ABI measurements <0.9, statin and antiplatelet were prescribed to 87% and 96% respectively (Figure 5a,b). Noncompressible or not reliable ABIs are concerning, and often a marker of advanced atherosclerosis or diabetes. Of the patients with these abnormal ABI readings, 75% were discharged on a statin and 75% on an antiplatelet (Figure 5a,b). Another potential indicator of PAD severity is evidence of prior amputation. Interestingly in this population, all patients with prior above-knee amputations (AKA) or below-knee amputations (BKA) were discharged on statin and antiplatelet agents even though those medications were always not present on admission (Figure 6).
Figure 5.
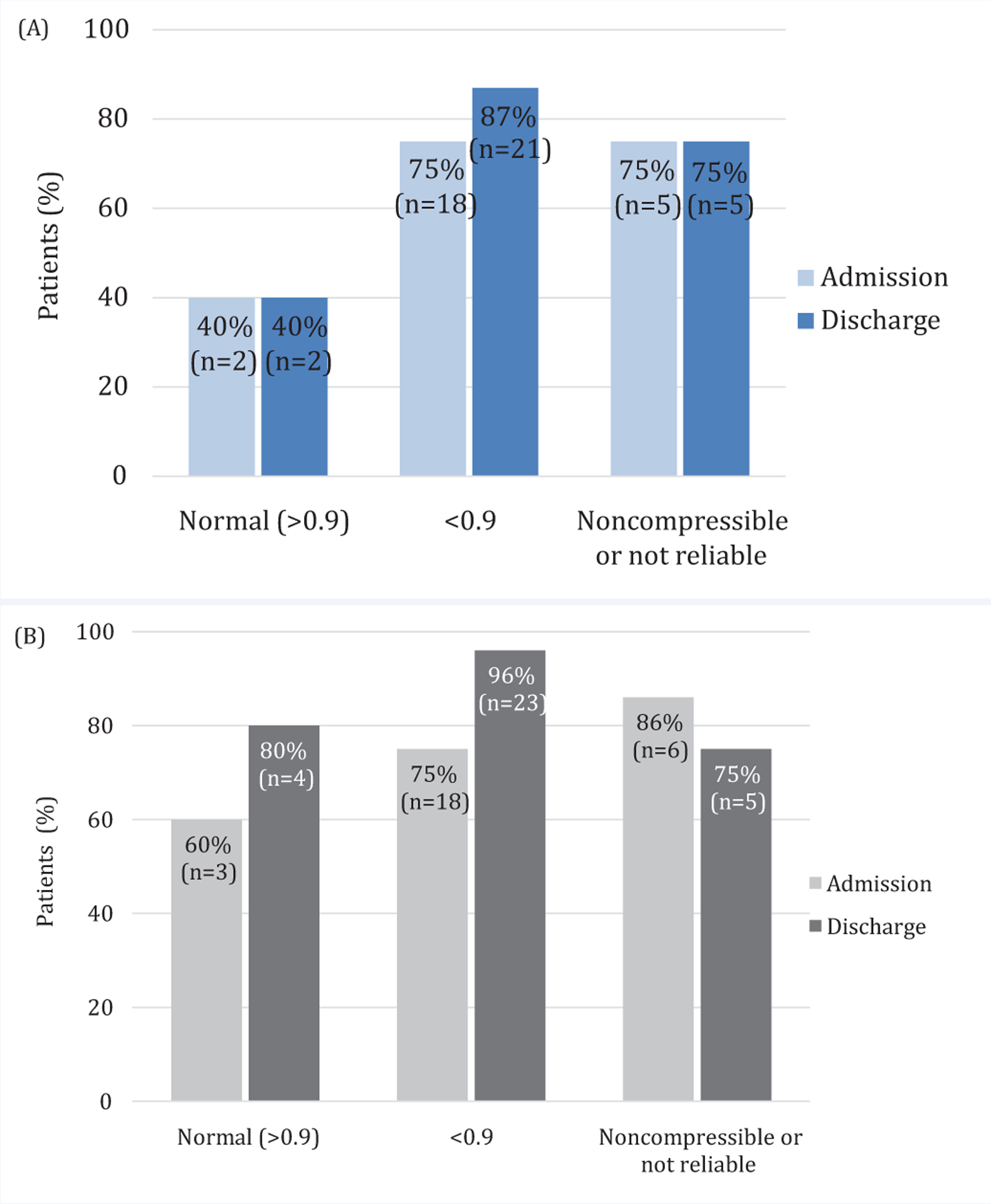
(A) - Distribution of success in prescribing statin agents at discharge based upon ABI. (B) - Distribution of success in prescribing antiplatelet agents at discharge based upon ABI.
Figure 6.
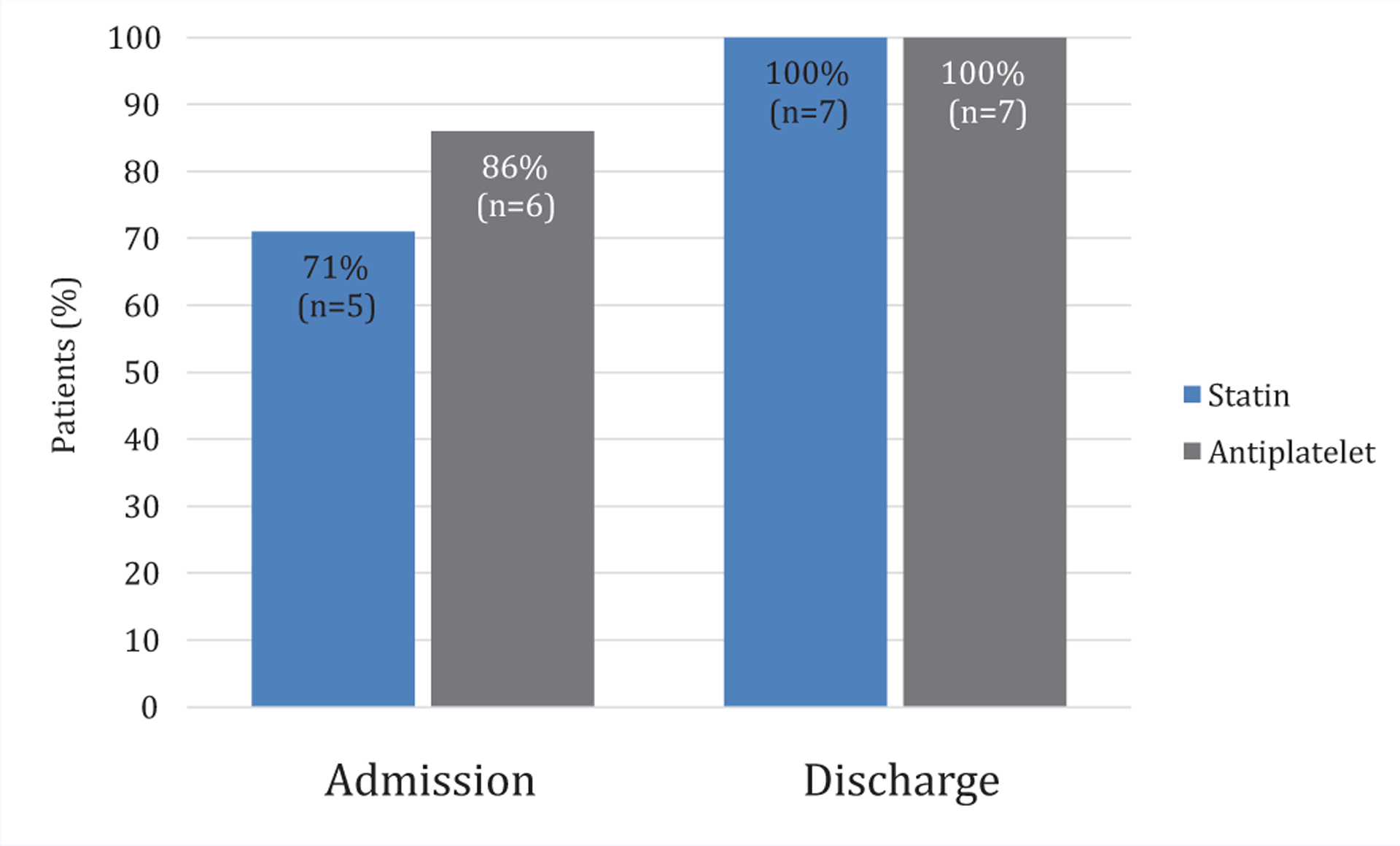
Distribution of success in prescribing statin and anti-platelet agents at discharge in patients with major amputations.
In order to better understand the populations of patients discharged without best medical therapy, a subset analysis was completed only on those patients discharged without a statin and those discharged without an antiplatelet. Of the patients discharged without a statin, 62% of the patients were African Americans (20% male vs. 80% female) and 38% were Caucasian (67% male, 33% female). Females were disproportionately affected, making up 62% of the non-statin population (80% African American, 20% Caucasian) (Figure 7). A look at comorbidities demonstrated that 100% of these patients had a prior diagnosis of hypertension, 50% had diabetes mellitus and 50% had hyperlipidemia, but none of these had a prior history of stroke. In these patients, 38% had normal ABIs and 25% had allergy, intolerance, or refusal documented in the medical record. In the patients discharged without an antiplatelet, 100% were African American (50% Male, 50% Female). All patients lacked a prior history of stroke, PAD or CAD, however all patients also had a prior diagnosis of hypertension. Notably, 50% of these patients were discharged on an anticoagulant (Coumadin) and 25% had normal ABIs.
Figure 7.
Racial and gender profile of patients discharged without a statin (n = 8).
CONCLUSION
Even at a tertiary care medical center, patients with confirmed PAD continue to be discharged without optimal medical management, indicating that further awareness and education are needed. Appropriate introduction of these therapies may be influenced by race, sex, admitting service, or presence of a normal ABI. In this study, we observed a 22% increase in statin and a 23% increase in antiplatelet prescriptions for patients on a vascular service at the time of discharge. For patients admitted under non-vascular services, there was a decrease in discharge prescriptions for these treatments. All patients discharged without an antiplatelet and most of those discharged without a statin were African American (63%), and African American females were disproportionately discharged on suboptimal medical therapy. Interestingly, the rate of prescribing anti-platelet agents was greater than for statins, suggesting that potential side effects may continue to influence physician practice.
These findings are consistent with prior investigations suggesting that best medical therapy implementation was disproportionately affected by race, age and underlying diagnoses [17–19]. Reasons for the suboptimal implementation of secondary prevention measures in patients with PAD may be attributed to three factors: (1) patient-related, including patient education and adherence; (2) physician-related, involving appropriate diagnoses and knowledge of risk factor modifications; and (3) healthcare-related, due to the diversity of specialties that care for these patients [20].
Patient education and adherence is pivotal to controlling PAD, a silent and systemically threatening disease. Every opportunity to involve the patient in the healthcare process should be made - from understanding the severity of the disease process to recognizing treatment options. Low compliance can also lead to low use of secondary prevention in PAD patients, especially in women and African Americans who are at highest risk for nonadherence to statin medications [21]. Not only are these populations receiving suboptimal medical therapy, they are also at highest risk for amputation [13,22,23]. Notably, most of the patients in this study that left the hospital without a statin were African American women. Additionally, African Americans and older women are more likely to be affected by polypharmacy, an issue strongly affiliated with medication error and harmful drug interactions [24,25]. Patient adherence is a constant battle for many physicians, however, providers’ perceived nonadherence should not result in missing an opportunity to intervene.
Physician-related factors which contributed to lack of statin or antiplatelet implementation can involve underdiagnosis due to normal ABI measures and an inadequate understanding of risk factors. Traditionally, an ABI <0.9 is indicative of hemodynamically significant arterial stenosis. Alternatively, elevated ABI is believed to be due to pathophysiological “propping open” of the vessel lumen, which may be evident in the waveforms of the pulse volume recording, but these are not always readily available. Therefore, providers may interpret a falsely elevated, normal ABI reading in a patient with significant PAD. Less than half of patients in this study with normal ABI measurements were discharged on a statin despite a new diagnosis of PAD, suggesting these normal values may deter providers from initiating proper medical therapy. Additionally, a patient without a history of vascular events might lead a provider to consider them low risk for symptomatic disease. In patients discharged without a statin, none had a history of stoke, 38% had history of CAD and 50% were diagnosed with hyperlipidemia. In line with physician-related factors hindering secondary PAD prevention, a group at Baylor College of Medicine and the Department of Veterans Affairs recently published results similar to those found at this institution, with 76% of patients with PAD alone receiving a statin prescription after undergoing in-house percutaneous vascular intervention [26]. This study also found a large variation in evidence-based statin prescribing in Veterans Affairs facilities across the country. Additionally, a separate study of primary care providers concluded that fears of hepatotoxicity drove physicians away from prescribing statin medications, even if medical indications were present [27]. Similarly, patients discharged without an antiplatelet had not experienced prior cardiovascular events such as myocardial infarction or stroke. No patients discharged without an antiplatelet prescription had history of CAD or stroke. This lack of debilitating vascular events may reduce the use of preventative medication in patient populations. Medications, like statins and antiplatelet agents, originally outlined for secondary prevention instead become a form of damage control and tertiary prevention.
Despite widespread integration of electronic medical record systems, physicians continue to struggle to communicate effectively to optimize patient care. For instance, a variety of specialties care for patients with PAD, including primary care physicians, cardiologists, vascular surgeons and neurologists, and each specialty plays a specific and important role in the battle against the disease. However, without a clear outline for coordination, information is frequently lost, repeated or mistranslated [28]. These healthcare-related factors are deeply systemic and require coordination across fields to properly implement preventative measures.
Complicated race and sex-based factors can contribute to inadequate prescribing during hospitalizations. For instance, guidelines for statin initiation in African Americans have changed since the United States Preventative Services Task Force (USPSTF) altered recommendations in 2017, which would exclude 25% of African American patients who would previously be recommended for statin initiation. The revised USPSTF guidelines no longer defined a low-density lipoprotein (LDL) range that suggests initiation of statin therapy [29]. Prior studies have also demonstrated cultural influence in compliance with medical therapy, particularly in this population [30,31]. Females are at additional risk for discharge without PAD optimal medical therapy because physicians perceive male patients as being at higher risk for adverse cardiovascular events, leading to an increase in secondary prevention being directed at males over females with equivalent risk factors [18]. Women are twice as likely to have atypical claudication and a normal ABI measurement, leading to delayed diagnosis and treatment [32,33]. Women with PAD are older on presentation and have increased rest pain, lower walking distances on treadmill tests, and slower walking speeds [34]. These symptoms can be attributed to a longer latent phase, leading to an increased risk of presentation with critical limb ischemia (CLI) when compared to men. A historically high gender gap in revascularization means women are less likely to undergo surgical procedures for PAD and a large number remain undiagnosed until critical presentation [35]. These gender differences demonstrate the continued need for targeted healthcare for women, with a focus on risk factor modification and diagnosis.
For many PAD patients, diagnosis during hospitalization is a pivotal moment to intervene. Patients are more likely to be adherent to statin prescription if they receive one while in the hospital for a peripheral vascular intervention (PVI) [36]. Identifying medically undertreated patient populations; especially those admitted to the hospital with a new vascular diagnosis, is an important goal for providers that ultimately increases their ability to impact the vulnerable patients. Previous findings demonstrate that educational outreach visits (EOV) have been successful in increasing statin prescriptions, while others were largely ineffective [37,38]. At Massachusetts General Hospital, a visit-independent disease management tool was able to increase the prescribing of statins in patients with hyperlipidemia by sending the provider an email outlining high-risk patients along with best-practice decision support [39]. This intervention was not only easily adopted by providers but also highlighted how an asynchronous reminder can shorten the delay between identifying and acting clinically to resolve a medical issue. One thing is certain from prior interventional studies, academic detailing and disease management emails are only a portion of the more complicated answer. Guidelines, increased quality studies with defined metrics, and coordination of care across specialties need to be maximized systemically in order to optimize prescribing of best medical therapy.
There are several limitations of this single-hospital study worth discussing. First, our retrospective study population was limited to patients who were admitted to a regional referral medical center. The sample size was relatively small and may not represent large-scale demographics. Additionally, a patient’s race may not fully account for multiple important socioeconomic and cultural factors; therefore future studies may utilize zip codes to further characterize regional aspects of financial resources and access to care. Second, this retrospective study evaluated real-world clinical outcomes, but since the majority of patients were not admitted with vascular indications, we were unable to assess the influence of consultation with vascular providers. We were also unable to determine whether outpatient follows up with a vascular provider was scheduled; a factor which may have impacted the inpatient physician’s prescribing practices. Third, acquiring a statin medication may depend on the status of the patients’ health insurance and our study was not structured to account for this variable. Lastly, the retrospective nature of this chart review prohibited investigation into individual reasons that aspirin or statin prescriptions were withheld from these PAD patients, therefore further studies are needed to explore these concepts.
These findings suggest that provider education is essential to avoiding events where patients are sent home from inpatient hospitalization with a new diagnosis of PAD but inadequate medical therapies. Initiation of a standardized provider protocol for inpatient statin and antiplatelet therapy may improve compliance and warrants further investigation.
ABBREVIATIONS
- PAD
Peripheral Artery Disease
- ABI
Ankle-Brachial Index
- SVS
Society for Vascular Surgery
- ASCVD
Atherosclerotic Cardiovascular Disease
- AHA
American Heart Association
- HCUP
Healthcare Cost and Utilization Project
- AKA
Above-Knee Amputation
- BKA
Below-Knee Amputation
- CAD
Coronary Artery Disease
- USPSTF
United States Preventative Services Task Force
- LDL
Low-Density Lipoprotein
- PVI
Peripheral Vascular Intervention
- EOV
Educational Outreach Visit
REFERENCES
- 1.Grenon SM, Vittinghoff Eric, Owens Christopher D, Conte Michael S, Whooley Mary, Cohen Beth E. Peripheral artery disease and risk of cardiovascular events in patients with coronary artery disease: insights from the Heart and Soul Study. Vasc Med. 2013; 18: 176–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diehm C, Allenberg Jens Rainer, Pittrow David, Mahn Matthias, Tepohl Gerhart, Haberl Roman L et al. Mortality and vascular morbidity in older adults with asymptomatic versus symptomatic peripheral artery disease. Circulation. 2009; 120: 2053–2061. [DOI] [PubMed] [Google Scholar]
- 3.Heart Protection Study Collaborative Group. Randomized trial of the effects of cholesterol-lowering with simvastatin on peripheral vascular and other major vascular outcomes in 20,536 people with peripheral arterial disease and other high-risk conditions. J Vasc Surg. 2007; 45: 645–654. [DOI] [PubMed] [Google Scholar]
- 4.Society for Vascular Surgery Lower Extremity Guidelines Writing Group; Conte Michael S 1, Pomposelli Frank B, Clair Daniel G, Geraghty Patrick J, McKinsey James F, Mills Joseph L, et al. Society for Vascular Surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: management of asymptomatic disease and claudication. J Vasc Surg. 2015; 61: 2S–41S. [DOI] [PubMed] [Google Scholar]
- 5.Arnett Donna K, Blumenthal Roger S, Albert Michelle A, Buroker Andrew B, Goldberger Zachary D, Hahn Ellen J, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019; 74: e177–e232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kinlay S, Plutzky J. Effect of lipid-lowering therapy on vasomotion and endothelial function. Curr Cardiol Rep. 1999; 1: 238–243. [DOI] [PubMed] [Google Scholar]
- 7.Coppola G, Novo S. Statins and peripheral arterial disease: effects on claudication, disease progression, and prevention of cardiovascular events. Arch Med Res. 2007; 38: 479–488. [DOI] [PubMed] [Google Scholar]
- 8.Aung PP, Maxwell HG, Jepson RG, Price JF, Leng GC. Lipid-lowering for peripheral arterial disease of the lower limb. Cochrane Database Syst Rev. 2007; 2007: CD000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohler ER, Hiatt WR, Creager MA. Cholesterol reduction with atorvastatin improves walking distance in patients with peripheral arterial disease. Circulation. 2003; 108: 1481–1486. [DOI] [PubMed] [Google Scholar]
- 10.Stavroulakis K, Borowski M, Torsello G, Bisdas T, Collaborators C. Association between statin therapy and amputation-free survival in patients with critical limb ischemia in the CRITISCH registry. J Vasc Surg. 2017; 66: 1534–1542. [DOI] [PubMed] [Google Scholar]
- 11.Antithrombotic Trialists’ (ATT) Collaboration; Baigent Colin, Blackwell Lisa, Collins Rory, Emberson Jonathan, Godwin Jon, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009; 373: 1849–1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Initiative VQ. Optimal Discharge Medications for Vascular Patients. 2020.
- 13.Mustapha JA, Fisher Bryan T Sr, Rizzo John A, Chen Jie, Martinsen Brad J, Kotlarz Harry, et al. Explaining Racial Disparities in Amputation Rates for the Treatment of Peripheral Artery Disease (PAD) Using Decomposition Methods. J Racial Ethn Health Disparities. 2017; 4: 784–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Epidemiology, et al. The Burden of Diabetes in South Carolina. (South Carolina Department of Health and Environmental Control. 2012. [Google Scholar]
- 15.Bureau USC. South Carolina Quick Facts. 2020.
- 16.TE Brothers JG Robison, SE Sutherland, BM Elliott. Racial differences in operation for peripheral vascular disease: results of a population-based study. Cardiovasc Surg. 1997; 5: 26–31. [DOI] [PubMed] [Google Scholar]
- 17.Bosco LA, Gerstman BB, Tomita DK. Variations in the use of medication for the treatment of childhood asthma in the Michigan Medicaid population, 1980 to 1986. Chest. 1993; 104: 1727–1732. [DOI] [PubMed] [Google Scholar]
- 18.Abuful A, Gidron Y, Henkin Y. Physicians’ attitudes toward preventive therapy for coronary artery disease: is there a gender bias? Clin Cardiol. 2005; 28: 389–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams D, Bennett K, Feely J. Evidence for an age and gender bias in the secondary prevention of ischaemic heart disease in primary care. Br J Clin Pharmacol. 2003; 55: 604–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flu HC, Tamsma JT, Lindeman JH, Hamming JF, Lardenoye JH. A systematic review of implementation of established recommended secondary prevention measures in patients with PAOD. Eur J Vasc Endovasc Surg. 2010; 39: 70–86. [DOI] [PubMed] [Google Scholar]
- 21.Lewey Jennifer, Shrank William H, Bowry Ashna D K, Kilabuk Elaine, Brennan Troyen A, Choudhry Niteesh K. Gender and racial disparities in adherence to statin therapy: a meta-analysis. Am Heart J. 2013; 165: 665–678. [DOI] [PubMed] [Google Scholar]
- 22.Rucker-Whitaker Cheryl, Feinglass Joe, Pearce William H. Explaining racial variation in lower extremity amputation: a 5-year retrospective claims data and medical record review at an urban teaching hospital. Arch Surg. 2003; 138: 1347–1351. [DOI] [PubMed] [Google Scholar]
- 23.De Martino Randall R, Hoel Andrew W, Beck Adam W, Eldrup-Jorgensen Jens, Hallett John W, Upchurch Gilbert R. et al. Participation in the Vascular Quality Initiative is associated with improved perioperative medication use, which is associated with longer patient survival. J Vasc Surg. 2015; 61: 1010–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perry BA, Turner LW. A prediction model for polypharmacy: are older, educated women more susceptible to an adverse drug event? J Women Aging. 2001; 13: 39–51. [DOI] [PubMed] [Google Scholar]
- 25.Assari S, Helmi H, Bazargan M. Polypharmacy in African American Adults: A National Epidemiological Study. Pharmacy (Basel). 2019; 7: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McBride Cameron L, Akeroyd Julia M, Ramsey David J, Nambi Vijay, Nasir Khurram, Michos Erin D, et al. Statin prescription rates and their facility-level variation in patients with peripheral artery disease and ischemic cerebrovascular disease: Insights from the Department of Veterans Affairs. Vasc Med. 2018; 23: 232–240. [DOI] [PubMed] [Google Scholar]
- 27.Fadi SR, Michael LV, Hilana HH, Siva KT, Rajasekhara RM, Gagan KS. Hepatotoxicity fears contribute to underutilization of statin medications by primary care physicians. Am J Med Sci. 2010; 340: 89–93. [DOI] [PubMed] [Google Scholar]
- 28.Sittig DF, Belmont E, Singh H. Improving the safety of health information technology requires shared responsibility: It is time we all step up. Healthc (Amst). 2018; 6: 7–12. [DOI] [PubMed] [Google Scholar]
- 29.Shah RV, Spahillari Aferdita, Mwasongwe Stanford, Carr J Jeffrey, Terry James G, Mentz Robert J, et al. Subclinical Atherosclerosis, Statin Eligibility, and Outcomes in African American Individuals: The Jackson Heart Study. JAMA Cardiol. 2017; 2: 644–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hammond WP. Psychosocial correlates of medical mistrust among African American men. Am J Community Psychol. 2010; 45: 87–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gamble VN. Under the shadow of Tuskegee: African Americans and health care. Am J Public Health. 1997; 87: 1773–1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schramm K, Rochon PJ. Gender Differences in Peripheral Vascular Disease. Semin Intervent Radiol. 2018; 35: 9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McDermott MM, Greenland Philip, Liu Kiang, Criqui Michael H, Guralnik Jack M, Celic Lillian, et al. Sex differences in peripheral arterial disease: leg symptoms and physical functioning. J Am Geriatr Soc. 2003; 51: 222–228. [DOI] [PubMed] [Google Scholar]
- 34.McDermott MM, Greenland Philip, Liu Kiang, Guralnik Jack M, Celic Lillian, Criqui Michael H, et al. The ankle brachial index is associated with leg function and physical activity: the Walking and Leg Circulation Study. Ann Intern Med. 2002; 136: 873–883. [DOI] [PubMed] [Google Scholar]
- 35.Feinglass J, McDermott MM, Foroohar M, Pearce WH. Gender differences in interventional management of peripheral vascular disease: evidence from a blood flow laboratory population. Ann Vasc Surg. 1994; 8: 343–349. [DOI] [PubMed] [Google Scholar]
- 36.Renard Brian M, Seth Milan, Share David, Aronow Herb D, Laveroni Eugene W, Gregorio Michele De, et al. If not now, when? Prescription of evidence-based medical therapy prior to hospital discharge increases utilization at 6 months in patients with symptomatic peripheral artery disease. Vasc Med. 2015; 20: 544–550. [DOI] [PubMed] [Google Scholar]
- 37.Zillich Alan J, Ackermann Ronald T, Stump Timothy E, Ambuehl Roberta J, Downs Steven M, Holmes Ann M, et al. An evaluation of educational outreach to improve evidence-based prescribing in Medicaid: a cautionary tale. J Eval Clin Pract. 2008; 14: 854–860. [DOI] [PubMed] [Google Scholar]
- 38.O’Brien MA, Rogers S, Jamtvedt G, Oxman AD, Odgaard-Jensen J, Kristoffersen DT, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2007; 2007: CD000409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lester WT, Grant RW, Barnett GO, Chueh HC. Randomized controlled trial of an informatics-based intervention to increase statin prescription for secondary prevention of coronary disease. J Gen Intern Med. 2006; 21: 22–29. [DOI] [PMC free article] [PubMed] [Google Scholar]


