Abstract
The increasing ubiquity of health sensing technology holds promise to enable patients and health care providers to make more informed decisions based on continuously-captured data. The use of sensor-captured patient-generated data (sPGD) has been gaining greater prominence in the assessment of physical health, but we have little understanding of the role that sPGD can play in mental health. To better understand the use of sPGD in mental health, we interviewed care providers in an intensive treatment program (ITP) for veterans with post-traumatic stress disorder. In this program, patients were given Fitbits for their own voluntary use. Providers identified a number of potential benefits from patients’ Fitbit use, such as patient empowerment and opportunities to reinforce therapeutic progress through collaborative data review and interpretation. However, despite the promise of sensor data as offering an “objective” view into patients’ health behavior and symptoms, the relationships between sPGD and therapeutic progress are often ambiguous. Given substantial subjectivity involved in interpreting data from commercial wearables in the context of mental health treatment, providers emphasized potential risks to their patients and were uncertain how to adjust their practice to effectively guide collaborative use of the FitBit and its sPGD. We discuss the implications of these findings for designing systems to leverage sPGD in mental health care.
Keywords: mental health, wearables, post-traumatic stress disorder, sensors, patient-generated data, Applied Computing~Consumer health, Applied Computing~Health care information systems, Human-centered computing~Empirical studies in HCI
1. INTRODUCTION
Mental health disorders are prevalent in the US and around the world, posing an enormous burden to individuals and society. At an individual level, mental health disorders can cause social and cognitive limitations and lower quality of life, while at a societal level, they can reduce productivity and increase health care expenditures [23, 31, 32, 63]. Veterans experience elevated rates of mental health issues, especially post-traumatic stress disorder (PTSD). An estimated 23% of veterans returning from Operation Enduring Freedom/Operation Iraqi Freedom receive a diagnosis of combat-related PTSD [42]. Patients with PTSD tend to have high rates of comorbid mental and physical health conditions, such as depression, suicidality, and musculoskeletal and respiratory disorders [17, 40, 113]. Given the complexity of both PTSD and its frequently cooccurring disorders, individuals with PTSD often require ongoing management by health care providers.
One promising avenue for managing complex health conditions involves leveraging behavioral and physiological signals via wearable activity monitors like Fitbits. These devices have become increasingly ubiquitous since their debut a decade ago. A 2014 national survey found that one in ten American adults uses a wearable activity monitoring device on a daily basis [87], and that number is growing. Through sensors in the devices, activity monitors automatically track signals such as step count, heart rate, and sleep, on a continuous basis. Sensor-captured data from wearable devices is one form of patient-generated data (PGD) which has been increasingly considered for integration into different clinical practice settings to inform care. A growing number of studies have started to address the potential of sensor-captured PGD (sPGD) as a tool to increase physical activity, for instance applying wearables as an intervention for overweight or sedentary patients [1, 7, 20, 45, 102].
Applications of wearables to mental health have proceeded more slowly, reflecting the less straightforward mapping of available data streams to psychological states and symptoms. Yet, there are strong connections between physical and mental health [108], and signals detectable through sensors can also correlate with psychiatric symptoms. Early work exploring the application of wearables to mental health has suggested that wearables may support behavioral activation among patients with depression [20] and motivate exercise among women with comorbid alcohol-dependence and depression, leading to reductions in anxiety and depressive symptoms [1]. In addition, studies of students and their college mental health providers suggest interest from both groups in applying sPGD to set personalized behavioral goals, assess therapeutic progress, and prompt reflection and discussion about the role of patients’ behavior in mental health [59, 74]. While this represents a fledgling area of research, early findings suggest potential value of self-tracking for mental health.
Opportunities to integrate sPGD into mental health care also potentially align with recent calls for measurement-based care of mental health conditions [38, 47, 71]. In measurement-based care, treatment decisions are made through systematic tracking of patients’ symptoms and responses to treatment. The guidelines that currently exist in relation to measurement-based care focus on self-reported assessments of symptom severity such as the Patient Health Questionnaire (PHQ-9) for depression [67], Generalized Anxiety Disorder Scale (GAD-7) for anxiety [101], PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (PCL-5) for PTSD [11], and Brief Alcohol Monitor (BAM) for substance abuse [15]. However, these self-report measures are subject to biases due to factors such as memory and social desirability. These biases do not affect sPGD. By using sPGD collaboratively with patients, providers may gain access to another stream of data to inform and adjust treatment.
Within CSCW there is growing interest in the collaboration required to leverage PGD generally in clinical environments [22, 75, 77, 94, 96]. We are still in the early adoption phase for sPGD, particularly in mental health care where providers are often slow to adopt health information technology [14], and where existing wearable devices have not been designed with mental health in mind. At present, we have little understanding of how mental health providers envision the role of sPGD in patient care and its potential impacts on their therapeutic role. To address this gap, we conducted semi-structured interviews with 17 mental health care providers who treat veterans with PTSD and who represent a variety of specializations from individual psychotherapy to yoga instruction. These providers offered care in a three-week intensive PTSD treatment program in which veterans were given a complementary Fitbit. Although not required, members of the care team had the opportunity to engage with patients regarding the use of the Fitbit and its data. This study seeks to clarify how mental health care providers perceive applications of sPGD in this therapeutic context, as well as the barriers they perceive to realizing use of sPGD.
In this paper, we address two research questions:
What opportunities and barriers do mental health care providers perceive in applying sPGD among populations with PTSD within routine care settings?
How can providers’ perspectives inform the design of sensor-captured tracking systems and strategies to implement these technologies and their data in treatment?
Our findings suggest that providers view patients’ self-tracking with Fitbit as a means to promote empowerment and positive behavior change. They also envision using sPGD collaboratively, for instance in clinical conversations where data is situated in relation to both their clinical expertise and the patient’s beliefs and experiences. However, given the climate of uncertainty around appropriate application of this novel type of health data, providers had enacted few of these envisioned collaborative uses. We discuss the challenge that mental health contexts may present to the “objective” nature of sPGD, the ways that perceived risks and uncertainty may drive treatment decisions in mental health care, and implications for designing systems to better leverage sPGD in mental health care.
2. BACKGROUND AND RELATED WORK
In this section, we provide an overview of prior work related to integrating sPGD into the clinic, emphasizing collaborative processes afforded by these data. Although most of these studies pertain to the physical health domain, we also review the few studies examining use of sPGD in mental health, an area in which measurement-based care is gaining prominence.
2.1. The Promise of sPGD in the Clinic
Reflecting the increased availability of commercial wearable devices, consumers have been at the forefront of adopting self-tracking technologies to advance health, with 172 million wearable devices shipped in 2018 alone [53]. Consumer wearables, built by companies including Apple, Samsung, Fitbit, and Garmin, have been advertised to “improve overall health” [54], and to facilitate self-management of health through collecting information that was previously accessible only in clinical settings, using specialized equipment, or through analog methods such as journaling. With relatively little effort, consumers can now create continuous logs of physiological and behavioral data such as number of steps, resting heart rate, and time asleep.
On its face, the growth of consumer wearables should contribute to the efficiency and quality of health care, reducing the need for health services through facilitating patients’ self-management, and – if data is made accessible to providers – allowing for remote monitoring and personalized treatment [8, 104]. Patient-provider collaboration using PGD collected through analog methods have been promising. Chung et al. [21] examined how health care providers used log data from patients with obesity and irritable bowel syndrome (e.g., manually compiled logs of sleep, stress, mood, and food), and showed that PGD aided in developing personalized treatment plans, building the patient-provider relationship, and supporting patients in behavior change. Early research on automated tracking with devices such as continuous blood glucose monitors and smartphone accelerometers likewise suggested that making these data available to providers enhanced patient motivation and facilitated decision-making around health behavior change [19, 69, 89].
Despite these potential benefits, studies on the diffusion of PGD into routine clinical practice have also uncovered a number of barriers faced by clinicians [2]. For instance, Zhu et al. [116] identified technical, social, and organizational challenges related to sharing and utilizing PGD in clinical practice. Technical challenges included the inability to transfer PGD into electronic health records. Social challenges included negotiating differing expectations around use of data in clinical discussions given the limited time during visits. Organizationally, while many patients desired to make their care more collaborative, clinicians often had not adjusted their culture or workflows to accommodate desired levels of patient involvement. In a review of the literature on PGD in the clinic, West et al. [112] revealed additional barriers to integration including: misalignment of patient and provider perspectives, such as when patients shared detailed activity logs that providers deemed clinically irrelevant, issues with data quality, incompatible data formatting, ambiguity in data interpretation, and challenges deciding what actions to take based on the data. Notably, most studies on the use of PGD in clinical settings centered on its application on physical health conditions; only two clinicians in the studies reviewed by West et al. were mental health care providers.
Our study begins to fill this gap by providing early insights into how mental health care providers perceive PGD, specifically sPGD. This question is timely given the paradigm shift occurring in mental health care over the past two decades towards measurement-based care, as described in the next section.
2.2. Measurement-Based Care in Mental Health
In clinical contexts, measurement-based care involves repeated and systematic appraisal of a patient’s condition to inform treatment delivery, including adjusting treatment based on the patient’s response. While measurement-based approaches have been longstanding in care of physical health conditions [50], the push toward measurement-based care in mental health has been more recent and has distinct challenges [38, 47, 71]. Measurement-based care of physical health can involve administration of laboratory tests to diagnose conditions or monitor progress over time [103], but gold standards for assessing mental health rely on patients reporting their own psychological symptoms. Typically, patients rate the extent to which they experience symptoms outlined in the Diagnostic and Statistical Manual of Mental Disorders [4]. To reflect the dynamic nature of these symptoms, measures must be completed regularly, which imposes a burden on patients and providers. In addition, patient-reported data are subject to fallible memory, as well as social desirability bias wherein patients over-report positive behaviors and experiences and under-report negative ones in an attempt to meet providers’ expectations [98, 107]. Furthermore, patients and clinicians may lack the tools, motivation, or ability to take regular, systematic measurements.
Sensor-captured measurement holds promise to easily extract a range of health-related signals while avoiding the various pitfalls of self-report. While current consumer wearables do not provide a direct view into psychological states like anxiety or mood, a number of signals captured by wearables, including physical activity, resting heart rate, and sleep, have relevance for both physical and mental health [56, 114]. As mentioned above, Fitbit reduced relapse risk among women with depression and alcoholism by motivating use of physical activity to manage alcohol cravings and mood [1]. Another study found that participants with depression perceived benefit from using a Fitbit in terms of increased self-awareness and physical activity motivation [20]. Yet, in these studies, sPGD were not integrated into clinical workflows and did not inform treatment decisions. Wearables were applied primarily as a way to enhance mental health via the benefits of physical activity, rather than to extract insight into specific mental states or symptoms.
The ability to gain insight into mental states and symptoms via sPGD may be improving. An emerging area of research on “digital phenotypes” suggests that combining signals extracted from wearable devices and additional sensors (e.g., sensors in the mobile phone) can serve as a basis for identifying and predicting mental health states, often through machine learning models [78, 83, 106]. For example, Madan et al. [73] used location and communication data from mobile phones in order to detect stress. Mobile phone sensors have also been used to monitor mental health-related signals in conditions including bipolar disorder, schizophrenia, and depression, and to predict events like relapse [9, 30, 78, 92], although less work to date has examined how patients and care providers might effectively intervene on the basis of such predictive models [94].
As sPGD becomes more accurately linked to mental health states, these data are likely to become increasingly relevant to measurement-based mental health care, suggesting a need to better understand clinical perspectives and experiences related to using sPGD in a mental health treatment environment.
2.3. Integrating sPGD in Mental Health Treatment
There are few studies in CSCW that specifically address clinical integration of sPGD in mental health care. One by Meng et al. [74] investigated how collaborative use of sPGD by students and their university mental health counselors could support management of depression. This study examined reactions to a prototype of iSee, a mobile sensing platform that collected data on heart rate, physical activity, phone use, location, and other physiological and environmental factors, processed data into personalized targets for behavior change, and shared this data with students and their counselors. Similar to previous findings on self-tracking, students and counselors valued the potential to track progress and to discuss data during counseling sessions. Providers and patients also saw potential to use PGD to enhance therapeutic feedback and to find new correlations between behaviors and symptoms. Similarly, a study by Kelley et al. [59] on college students and student mental health professionals found that both groups viewed behavioral data as providing useful proxies for mental health states. For example, stress is difficult to track directly, but students felt they could approximate their stress levels by observing their patterns of sleep.
Our study extends this avenue of research, examining the potential for delivering mental health care that integrates sensor data from a widely-available consumer wearable, Fitbit, in a different therapeutic population and setting: veterans completing an intensive PTSD treatment program. It might be especially useful to examine sPGD in relation to PTSD given that PTSD symptoms and treatments have behavioral and physiological elements that wearables like Fitbit may detect. For instance, stress and panic attacks are associated with elevations in heart rate, while disruptions to sleep schedules and daily routines may correspond to sleep hours and step counts. Thus, various streams of sPGD available from commercial wearables have promise to facilitate “objective assessments” of behaviors and states relevant to symptoms, coping, and therapeutic progress in this population [70].
sPGD can offer detailed, ongoing, and multifaceted information about patients’ status outside the clinic, providing an alternative to error-prone and burdensome self-report measures common in mental health treatment. However, commercial wearable devices are designed with wearers as primary stakeholders and adopters rather than care providers. Such devices have not been designed or optimized for clinical settings, particularly mental health care settings. This is both a limitation of the current exploration as well as an opportunity to inform future work. Our contribution to this area of research includes a provider perspective of the use of Fitbit in a routine care setting for veterans with PTSD.
3. SUMMARY
Studies have shown that sPGD have potential to improve health care by providing access to extensive information about patients’ health and daily behaviors, thereby facilitating evidence-based treatment decisions. To date, there have been few studies of sPGD in mental health. It therefore remains unclear what opportunities providers see in using sPGD in a routine care setting and in relation to the physiological and behavioral manifestations of PTSD. Our investigation seeks to expand our understanding of the potential role that sPGD might play in mental health care from the perspective of providers who are on the front lines of adopting these data into a new setting and navigating uncertainties around their interpretation and use.
4. SETTING
4.1. Prevalence, Characteristics, and Treatment of PTSD
Lifetime prevalence of PTSD is estimated to be around 7% among American adults [62]. A diagnosis of PTSD requires both exposure to a trauma and a combination of symptoms clustering around intrusion, avoidance, changes in mood and cognition, and changes in arousal and reactivity [4]. Not everyone who experiences a traumatic event develops PTSD, and the development of PTSD is more common in women than men (20.4% to 8.1% respectively) and varies in response to the type of trauma experienced (1.8% for physical attack to 65.0% for rape) [61] Military personnel with exposure to combat stressors are at an elevated risk of developing PTSD, with an estimated 38.8% receiving a PTSD diagnosis. Especially when severe, PTSD can have negative consequences for life, work, and relationships [6, 61].
PTSD is often addressed in outpatient settings with evidence-based treatments including cognitive processing therapy (CPT). CPT focuses on discovering “stuck points,” irrational beliefs about traumatic events. For example, a veteran suffering from combat-related trauma could believe they were the cause of others’ untimely death through their commands. Dispelling stuck points involves Socratic dialogue and worksheets. In Socratic dialogue, the clinician asks the patient a series of questions to facilitate healthier reappraisal of traumatic events. In this process, the patient contributes their life experiences and interpretations while the clinician contributes their expertise on trauma and interventions. Clinicians may also assign worksheets for patients to complete outside of session. These may prompt patients to write and dissect narratives about the traumatic event [41, 90].
The uptake of evidence-based treatment for PTSD is poor due in part to patients’ avoidance as well as difficulties accessing treatment [52, 57, 97, 111]. Some individuals with more severe or persistent symptoms also require a high level of care. One form of more intensive care is intensive outpatient treatment which condenses comprehensive therapeutic interventions into a short time period. Increasing the frequency of visits can lead to lower dropout rates and minimize between-session distractions that disrupt treatment [57, 58]. Intensive treatments are beginning to gain significant traction and yield positive results for a variety of mental health conditions [49, 95].
4.2. Routine Care Setting: Intensive Treatment Program
The Road Home Program: National Center of Excellence for Veterans and Their Families at Rush, funded in part by Wounded Warrior Project, created an intensive treatment program (ITP) in order to improve the accessibility, quality, and frequency of care for veterans living with the invisible wounds of war. This outpatient ITP lasts for three weeks and provides over 120 hours of comprehensive mental health care [115]. Each cohort consists of 10-13 veterans diagnosed with PTSD. To measure progress over the three weeks, veterans regularly complete four clinical survey assessments. These surveys track symptoms of PTSD (PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, PCL-5) [11, 12], depression (Patient Health Questionnaire-9) [67], negative cognitions (Post-traumatic Cognitions Inventory) [36], and guilt (Trauma-Related Guilt Inventory) [68].
During the ITP, each veteran receives 13 sessions of group CPT, 14 sessions of individual CPT, 12 sessions of group mindfulness-based resilience training, and 13 sessions of group yoga. Each patient is assigned an individual provider, consistent across all individual sessions. Group providers are consistent across all sessions for each cohort. CPT providers include counselors, social workers, and psychologists. Mindfulness-based resiliency training and yoga groups are led by nurse practitioners, mindfulness instructors, and yoga teachers. In addition, the comprehensive team includes nurses, psychiatrists, neurologists, neuropsychologists, and psychology and social work trainees. In this study, we refer to this group as the “care team” and individuals as “care providers” as opposed to “clinicians” to encapsulate the diversity of expertise represented.
As part of wellness programming, Fitbits were incorporated into the fitness and nutrition courses to promote a healthy physical activity level and to facilitate self-awareness of the body’s physiological responses to triggering events. On the day of the veteran’s arrival, the staff provides the veteran with their own Fitbit and explains how to program it, use it, and interact with it, answering questions as the veteran sets up the device. Throughout the program, nutrition and fitness care team members incorporated the Fitbit into the curriculum through training and reviewing heart rate during sessions.
A prior study investigated how veterans in the ITP made use of Fitbit and its PGD [82], but it did not assess the care team’s uses or perceptions of sPGD, as examined here. Prior to the application of Fitbit in the ITP, providers did not report extensive past engagement with PGD beyond soliciting patient completion of clinical symptom surveys; few reported engaging with behavioral or physiological data collected by patients outside the clinic. When the Fitbits were first introduced to the ITP, care team members received minimal (<1 hour) training on the data generated by the Fitbit. Team members that joined after the initial deployment of Fitbit devices were not trained, and most participants reported not being able to recall this training. Care team members did not have access to the Fitbit data unless the patient showed it to them through the Fitbit mobile application on their smartphone or through the Fitbit device itself. At the end of their three-week stay, Fitbit data for each consenting patient was downloaded in spreadsheet format to store for potential future research (Fig. 1). Care team members’ largely undirected use of sPGD allows us to understand how routine mental health care processes may or may not be conducive to integration of these data.
Fig. 1.
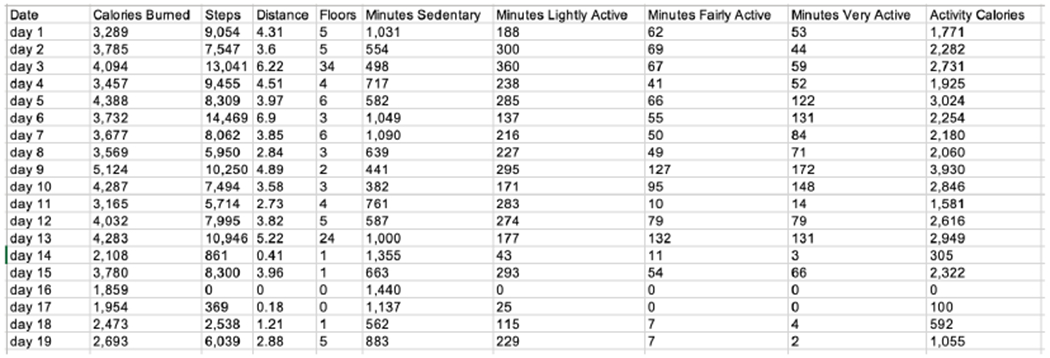
De-identified Fitbit data from a patient that completed the program
5. DATA COLLECTION AND ANALYSIS
5.1. Recruitment and Participants
Interviews were conducted in person except for one conducted by phone due to a scheduling conflict. All care team members in the ITP received an invitation to participate via e-mail from the research director (AKZ) and the clinical director (MB). Participants were not compensated for their participation. Table 1 provides summary information for all participants.
Table 1.
Participant Care Roles
| Participant | Role |
|---|---|
| C1 | Group therapist |
| C2 | Individual therapist |
| C3 | Non-therapistb |
| C4 | Group therapist |
| C5 | Group and Individual therapist |
| C6 | Non-therapistb |
| C7 | Individual therapist |
| C8 | Individual therapist |
| C9 | Individual therapist |
| C10 | Non-therapistb |
| C11 | Individual therapist |
| C12 | Individual therapist |
| C13 | Group and Individual therapist |
| C14 | Individual therapist |
| C15 | Non-therapista,b |
| C16 | Group therapista |
| C17 | Group therapista |
Participant is also an organization administrator
To anonymize participants who are the sole providers in their role, an administrator, nurse, nutritionist, and yoga instructor are listed as “non-therapist”
5.2. Data Collection
In order to examine how health care providers in the ITP envisioned using Fitbit data, we conducted semi-structured interviews with 17 members of the program’s care team. Three members of this group also served as administrators.
The interviews with the care team covered their: 1) role within the ITP, 2) experiences with PGD outside of the ITP, 3) perspectives on PGD, and 4) experiences with the Fitbit during the ITP. In order to gain a deeper understanding of possible uses of data outside of the current constraints of the Fitbit interface, care team members were also shown a list of broad categories of data Fitbit captures: heart rate, sleep, physical activity, consumption (food, drink), height, and weight. They were asked how they envisioned data of these types could be used within the context of the ITP.
Next, to constrain their envisioned uses to current technical capabilities and processes at the ITP, participants were shown a Microsoft Excel spreadsheet containing deidentified Fitbit data from a single patient who had previously completed the 3-week ITP (Fig. 1). The patient data was chosen for its completeness over the three-weeks of the program in order to gather more reactions to the various types of available data. Care team members talked through their initial impressions of the data, the value they envisioned the data could bring, and how they imagined incorporating sPGD into their daily workflow. Participants were also prompted to envision having access to the data in real-time as the three-weeks elapsed, with completeness of the data depending on when the data is accessed. For example, if they were to check the Fitbit data on the third day of the program, the spreadsheet would only contain the first three rows of data. Finally, given that the care team can currently only access a patient’s Fitbit data via the patient sharing data on their mobile app, we asked participants to explore a version of the Fitbit application shown on an iOS device. Care team members with administrative roles in the organization were asked additional questions about their observations of the care team’s use of the Fitbits and their perspective on the role of the Fitbit within the goals of the ITP and within its parent program.
The Institutional Review Boards at Northwestern University and Rush University Medical Center approved this research.
5.3. Data Analysis
A third-party service transcribed audio recordings from all interviews. The resulting transcripts were analyzed by the first author through a process of open coding, which captured current and proposed uses of data trackable by the Fitbit and barriers to such uses. Open codes were condensed into axial codes to create a code book, and all transcripts were coded using the resulting code book. The other authors peer-checked codes throughout. Taking a thematic analysis approach, the emerging patterns were sorted into themes that were derived from the data itself as opposed to existing theories [13]. This allowed us to identify patterns of use embedded in this specific context of care. Less prominent themes were disregarded, and the resultant themes were used to reanalyze the data set.
6. FINDINGS
In this section, we present our findings on care providers’ perceptions of the applications of Fitbit and its sensor-captured data to managing their patients’ mental health. Providers were generally aware that their patients in the ITP were using Fitbits, and some reported specific interactions related to the Fitbit data. Providers also reflected broadly on the ways they envisioned sPGD being leveraged in the future, ranging from patient-driven Fitbit uses to active collaboration around the Fitbit and attempts to incorporate its data into routine delivery of mental health care. We organize our findings to reflect this distinction between uses that minimally or indirectly involve the provider and collaborative uses of sPGD.
6.1. Patient-Driven Uses of Fitbit and its Data
While providers lacked extensive knowledge of how their patients were using the Fitbit during or after the ITP, they envisioned a number of ways in which patients could monitor and reflect on patterns in their Fitbit-captured data, leading to improved understanding and management of their own health. Several had examples of discussing these data in care when initiated by the patient. However, providers also noted potential challenges of interpretation that could arise in patient-driven use.
6.1.1. Self-Monitoring and Validation.
Providers largely agreed that patients’ uses of Fitbit might involve monitoring of and reflecting on patterns in their data (e.g., step count, heart rate, sleep logs) as objective records of their activity. This monitoring was generally viewed as a source of patient empowerment, and some had seen evidence of such benefit in practice. For example, C16 described the sense of validation a patient had experienced by reviewing patterns in her data. This patient had believed her feelings of exhaustion were inexplicable, given their persistence despite efforts to get reasonable hours of sleep, but she discovered that the Fitbit tracked not just hours in bed but also the quality of sleep. This metric yielded a new insight, providing a better account of her troubling symptoms. C16 described:
“It’s almost like getting an outside opinion… from the Fitbit that helps them see, that helps them better understand their symptoms… That’s really validating.” (C16)
Providers also speculated that patients might be motivated through accessing a record of their accomplishments, such as meeting step count goals. As C16 continued:
“I think that the benefit for the step challenge, for example, is obviously getting physical exercise, likely more than they have in the past because they are kind of prompted to do more. It also helps them feel a sense of accomplishment.” (C16)
This validation might be particularly valuable to patients with PTSD whose sense of self-worth is often impoverished:
“A lot of the thoughts you have are that you are incapable, inadequate, cannot accomplish things. So, that [data] kind of directly speaks against that, right? ‘I am able to accomplish something, like reaching 10,000 steps a day.’” (C16)
C4 described seeing these benefits in practice, with patients reporting that they had used sPGD to counter some components of PTSD, such as negative beliefs. In particular, some patients who had been isolated and inactive because of PTSD expressed their delight when increases in activity became apparent through reviewing sPGD. C4 reports that, in response, “I just try to provide affirmations for the change in their behavior.”
In addition, some providers hypothesized that sPGD might even surface benefits obtained through therapy, such as a change in symptoms after completing a written narrative of their trauma. For example, C4 described that accessing Fitbit’s graphs of symptoms could hypothetically provide a patient with:
“…a visual of progress, or how things are changing over time for them. It can connect. For example, if somebody writes their trauma account… and then, they notice a change in how they slept.” (C4)
In these examples, the data from Fitbit have value in allowing patients to self-monitor. They also have potential to provide an outside perspective for patients, which might yield new insight or validate a patient’s effort and therapeutic progress. Indeed, some of these benefits had already been reported by patients in clinical conversations.
6.1.2. Reinforcing Negative Views and Agitating Symptoms.
Providers also recognized situations where patients’ use of the Fitbit could lead to negative consequences. For instance, PTSD can be characterized by the tendency to catastrophize or become hyperfocused on negative occurrences. Several providers reported concerns that, upon reflecting on their data, patients could become discouraged by apparent lack of progress, or might focus on negative trends:
“Sometimes it can have an alternative effect like, ‘Yeah, look how shitty I’m sleeping, no wonder I feel so bad’ and then it can create a focus on negative things as opposed to not being aware that you’re sleeping so bad. It creates something else like, ‘Oh, look at me, I’m not even sleeping well. It’s just one more thing like life sucks’ kind of a thing. So, I wouldn’t say that that’s typical but that’s also a way that it can actually have a negative impact… if somebody is overly negatively bleak about their life and everything around them then it could just be one more thing to reinforce how bad they have it.” (C14)
Providers also reported that overuse of Fitbit might provoke anxiety in patients. This had already occurred with at least one of C9’s patients, such that C9 had to shift focus away from the data to a more productive task. He described:
“People get a little obsessed about sort of tracking symptoms. I had a client that I can remember that wore his Fitbit and every time he would get anxious he’d be like, ‘My heart rate’s at this, my heart rate’s at this,’ and that would just get him really amped up and he would obsess about this and it was like this instant biofeedback which just really elevated his anxiety because he was just so fixated on his heart rate and so we actually had to say, ‘Let’s dial back on you monitoring every few minutes. It’s useful information to have but let’s refocus on what we’re doing here.’” (C9)
In C9’s view, not only did the patient’s use of sPGD reinforce anxiety, but conversations about the sPGD led to loss of time that might have been spent on evidence-based practices like CPT.
These examples suggest that, from the provider’s perspective, the same data from the Fitbit might either support empowerment or induce fixation and anxiety depending on context, suggesting an ambiguous relationship of Fitbit data to patient wellbeing. C11 provided an example of how productive or unproductive application of Fitbit data may reflect a particular patient’s approach to coping:
“I think physical activity can go both ways. Iťs a coping skill for a lot of people, but it can also be a form of avoidance…. So, ‘Oh, you were distressed today and then you went and ran so hard that you made yourself puke? … Is this healthy exercise or is this you not wanting to feel your feelings?’ I know that that’s come up with a couple of my veterans as far as limiting their physical activity to, ‘Okay you’re going to go work out for an hour, but you’re not gonna push yourself to a point of pain because that’s avoidance.’ So, depending on the person, sometimes that’s real useful information. Other veterans will be like, ‘Oh, I’ve been walking to and from group today. It feels really good. I’ve been getting my steps in and it’s been really helpful. I’ve noticed a difference.’ That’s helpful.” (C11)
This situation highlights the importance of re-contextualizing physiological data within a clinical process where a provider may intervene to suggest an alternate way to frame or interact with the data. The provider may choose to de-emphasize negative patterns or to steer a patient away from data fixation or avoidant behaviors that have potential to be exacerbated by self-tracking, such as over-exercise. In the next section, we describe how providers recognized potential benefits of engaging with sPGD as a routine aspect of treatment.
6.2. Integrating Fitbit Data into Treatment Protocols
While providers reported that patients occasionally discussed their Fitbit data in clinic visits, providers largely had not pursued integration of the Fitbit and its data into their routine mental health care. However, providers envisioned that the Fitbit and its data could support their work by capturing additional information outside of the treatment setting, even providing a new means of systematically testing effectiveness of treatment options in order to improve care. When assessing a patient’s condition, therapists currently rely on three streams of data: (1) observation of the patient’s behaviors and interactions, (2) the patient’s self-report, and (3) the patient’s scores on various survey measures. Analyzed together, providers can identify areas of consensus or discrepancy between the different data streams, sometimes highlighting a need for discussion and clarification. For example, if the patient’s PHQ-9 scores decrease (i.e. patient’s depression is decreasing) yet the patient appears to be withdrawn during group therapy sessions, there is a conflict between the two points of data that needs to be reconciled. Some providers imagined that the Fitbit data could serve as a fourth stream of data that could offer triangulation with other available data streams and also provide ongoing insight into the patient’s status and behaviors outside of the clinic.
6.2.1. Understanding the Relationship Between sPGD and Standard Measures.
In order to make this new stream of data useful, providers stated that sPGD should ultimately connect back to survey measurements. C17 speculated that it might be possible to identify a relationship between PTSD symptoms as measured by surveys and behaviors tracked by the Fitbit, potentially even allowing a view into therapeutic progress across the ITP:
“What I think we could do more of with the Fitbit is seeing [patterns of sleep]…what was their baseline for the first week and then going into the second week what’s the average there and then the third week and seeing if that mimics the scores that we see on their self-report measures. Usually people will be very distressed in the first week, experience significant hypervigilance, an increase sometimes in frequency and intensity of their symptoms and then it will hit a peak and then will decrease into week three so I would be curious as to whether the Fitbit would show that.” (C17)
Having observed a common trajectory of symptom scores among patients undergoing three weeks of treatment, C17 was curious about whether the Fitbit could also surface these patterns.
6.2.2. Integrating sPGD with Therapy.
Beyond triangulating patterns observed in other data streams, care team members envisioned that the Fitbit could be used to aid in treatment, such as through facilitating “reality testing” to help patients overcome false or dysfunctional beliefs. C1 envisioned a situation in which the step count feature could be applied to identify negative cognitions and dispel them during individual therapy sessions:
“If somebody’s steps are really low for the entire ITP, it might lead to a discussion about ‘What’s that about?’ and then it might elicit a belief or cognition of, ‘The world is not safe’ or, ‘If I leave my room something terrible might happen.’ That could result in a homework assignment being given about, ‘Why don’t you go out with the group tonight and just see how it goes? Experiment.’” (C1)
Thus, accessing the Fitbit and its data could prompt dialogue around a stuck point centering on the consequences of being out in the world. The Fitbit could then be used to quantify or track progress toward an increased activity goal as the participant challenges the stuck point.
The Fitbit data was also viewed to have the potential to guide more productive discussions during treatment. For instance, C2 described how discovering correlations might open up a conversation about causes of stress:
“It could be beneficial [to] have that information and say, ‘Oh, wow, as your scores have gone down, your sleep is gotten better’ [or] ‘As your scores have gone down, your heart rate seems a little more even’ [or] ‘Your heart rate is always up during the group, what’s going on with that?’” (C2)
While these uses were hypothetical, providers were optimistic that the signals tracked by Fitbit might offer new opportunities to engage in therapeutic dialogue. In particular, observing correlations between symptoms and behaviors was envisioned as a potential way to spark conversations about progress and changes throughout therapy.
6.3. Challenges to the Use of sPGD in Treatment
Providers also anticipated potential negative consequences of collaborative activities involving sPGD, such as diverting time from evidence-based practices. They highlighted that displacement of standard care could negatively affect the patient’s treatment and cost the organization valuable time and resources.
6.3.1. Connecting to Clinical Practice.
Especially given the present context wherein patients decide whether and how to use the Fitbit and which data to share with providers, providers questioned whether they would have opportunities to connect data with their domain expertise: evidence-based care, which in this program was CPT. Providers wanted not only evidence that use of the Fitbit would significantly help patients, as measured by self-report surveys, but also training to help them connect Fitbit data to their established clinical practices. C8 outlined these concerns about not adhering strictly to CPT:
“It’s noticeable if a clinician is not sticking to protocol because, a) the patient’s scores aren’t changing and they’re not as engaged in the program and the client lags behind and, b) If I were like, ‘We went into the app and talked about sleep data’ we would be asked ‘Why aren’t you sticking to the protocol?’ not in a mean way or not in a punishing way but in a way that’s just like everyone needs to be a united front and consistent.” (C8)
Given that patients’ health is at stake, providers in the ITP highly value providing care that is effective and cohesive. It was not yet clear that the Fitbit and its sPGD would help in this effort.
Questions about the validity of the sensors were also cause for concern. C1 hypothesized that inaccurate readings from the Fitbit could cause unnecessary alarm and waste time in “non-productive conversations,” derailing clinical practices and undermining protocol. For example, this was imagined to occur if the Fitbit indicated poor sleep in a patient who in reality slept well:
“The Fitbit sleep data is not as solid as other sources of data so I could see it backfiring somewhat…that if a person is actually sleeping fine their Fitbit could say that they’re not or vice versa it might just confuse things.” (C1)
Thus, measurement errors might be counterproductive to treatment, even potentially leading to an exacerbation of patients’ issues.
6.3.2. Time and Resources.
Another concern regarding integrating Fitbit into care was the time and the resources needed to incorporate new streams of data. As C7 described:
“There’s always so much to do… You’re already kind of preparing for sessions, and at a certain point it’s like, ‘How much am I treating or assessing what I’m seeing on a screen or on paper compared to just talking to someone and figuring stuff out together?’” (C7)
In this quote, C7 highlights the potential that time needed to understand sPGD might negatively impact a meaningful interaction with the patient.
Furthermore, if Fitbit data were to be integrated into the clinical data repository (as opposed to the patient approaching the provider to share data), participants noted that additional individual preparation work might be required in order for patient-provider collaboration to occur. To prevent wasting time in sessions, the care team members envisioned reviewing the data before the patient comes in in order to decide whether there is something notable to discuss. However, as C5 notes, therapists may be unclear on how to recognize what is worth discussing and, furthermore, how to act on it.
“You’re going to need [to] train them on how to balance all of these different pieces of data they have access to and how to prioritize the data. I think it would be especially important for new therapists coming on. It would probably be pretty overwhelming for some to have access to that much data and I think we would need to do like a standard operating procedure of how to [deal with] the information.” (C5)
Providers felt they had relatively little flexibility in adopting new practices given the organization’s emphasis on protocols to ensure standardization and cohesion. Administration of specific symptoms survey measures was directly tied to grants and funding sources for the organization. As one provider and program leader (C16) stated:
“If our main funders want to see you doing a program for veterans with PTSD, what we want to see is reduction in PTSD symptoms and obviously that’s what we want to focus on. If we had another funder that said, ‘Hey, we’ll give you this much money to make sure that all the veterans with PTSD see an improvement in their sleep or their exercise’ or any of that, then our program would be structured very differently and maybe would incorporate more of these types of information… I don’t think the goals will change simply because they are pretty set on what they’re looking for, but if they were to change, I think that would directly impact what we do in here because we specifically chose CPT because it’s an evidence-based treatment for PTSD because that’s our goal.” (C16)
At present, there are no specific evidence-based practices for the treatment of PTSD that involve data the Fitbit can track. Consequently, providers noted a lack of organizational incentive to use the data, especially given its unknown value in treatment and the time and resources that would be required for training and integration.
7. DISCUSSION
Our study examined providers’ perceptions of the application of sPGD to delivering mental health care. In current practice, Fitbit and sPGD use were self-directed by patients, and providers recognized a number of ways that sPGD could help patients to generate new insights about symptoms, provide external validation, and reinforce therapeutic gains. At the same time, providers also expressed concern that patients might interpret data in unproductive ways or fixate on negative patterns. Clinical interactions were viewed as potentially fruitful settings within which to contextualize sPGD in relation to the patient’s experience and goals, while also drawing on the provider’s therapeutic expertise to interpret data and extract insights relevant to treatment. Nonetheless, given the limited validation of sPGD as clinically-relevant measures in mental health and the lack of protocols to accommodate collaboration around these data into clinical workflows, providers had done little to apply Fitbit as a mental health tool beyond offering consultation when initiated by patients. These findings echo our prior work with veterans completing the ITP, which found that the Fitbit was primarily used for self-monitoring and supporting social interactions with peers, rather than collaborating with the care team [82].
The gap we describe between providers’ envisioned and actual collaborative uses of Fitbit and its data reflects a number of challenges these providers face in adopting novel technologies within a mental health care environment. In our discussion, we describe that despite the promise of sPGD as a means of bringing “objectivity” into mental health care, applying sensor-captured data involves a complex and uncertain interpretive process that, from the provider’s perspective, is imbued with potential risk. In the sections that follow, we situate our findings in relation to prior work highlighting the subjectivity inherent in extracting meaning from technology-based measurements and we discuss organizational factors relevant to negotiating risks emerging from this interpretive process. Finally, given the unique constraints of sensor-based data within this mental health space, we identify design opportunities for patient-provider collaboration around sPGD.
7.1. Shifting Fitbit Data from “Objective” to “Situated Objectivity”
Our data highlight a tension between the perceived authority of sPGD as a source of “objective” measurement and the subjectivity inherent in extracting insights from these data. Below we describe how a process to appropriately situate data is necessary in order to establish meaning so that sPGD can be effectively used in mental health services.
7.1.1. Situating Objective Data in Mental Health.
Pantzar and Ruckenstein have observed that there are prevailing perceptions of tracking devices as a source of “mechanical objectivity” [28] where, due to their automated and standardized collection of data, their measurements are perceived as essentially objective [85]. Yet, they argue, the meaning of sensor-captured data is in fact deeply tied to the particular contexts in which data are collected, and data must therefore be appropriately situated to offer reliable insight. For example, sensor-captured data might indicate a user’s elevated heart rate over their baseline in a certain timeframe. There could be multiple possible reasons for this pattern; elevated heart rate might reflect stress and motivation as an individual strives to achieve a meaningful goal, but it could also reveal anxiety that impairs that individual’s ability to function. In this example, contextualizing sensor-based data within an individual’s larger experience is central to interpretation. Pantzar and Ruckenstein therefore propose the concept of “situated objectivity” to describe the epistemological status of sensor-tracked data, combining the authority of mechanical objectivity with the important role of context in knowledge formation.
Our findings suggest that providers view clinical interactions as a promising site for developing situated objectivity, with both patients and providers contributing valuable context. Specifically, clinical conversations may facilitate elaboration by the patient on her subjective experiences during data collection and on her initial assessment of the meaning of these experiences. In turn, the provider might suggest an alternative framework through which to view these experiences, drawing on a therapeutic perspective. For instance, Fitbit data might show the patient’s elevated heart rate whenever she is in a particular location. The patient might identify that this physiological reaction reflects an experience of anxiety. Without guidance from the provider, the patient might take this as a sign to avoid that location to prevent this response. However, from a therapeutic perspective, such avoidance might be unproductive, failing to address the cause of the anxiety. The provider might recommend against avoidance, instead suggesting continued visits to the site while employing coping methods learned in therapy, allowing the patient to ultimately overcome the anxious response. In this example, despite the application of non-traditional data to spark the conversation, the therapist operates within his or her therapeutic expertise by proposing a new possible lens through which the patient might view her experience in order to facilitate the development of mastery and resilience [39].
7.1.2. Overcoming Interpretive Challenges.
Our findings also suggest that providers see a potential role they could play in helping patients overcome specific interpretive biases that might manifest in relation to sPGD. One challenge among patients with PTSD is a tendency to focus on negative aspects of experience at the expense of positive ones [60]. In this context, the perceived “objectivity” of sensor-based data can play a dual role. On the one hand, providers hoped that sPGD could reduce the bias involved when patients monitor their symptoms and health behaviors in daily life, speculating that these data could offer an “outside” perspective, potentially more tethered to reality, and more valid and reliable than patients’ perceptions. This authoritative perspective from sPGD was viewed to have beneficial effects when it allowed patients to recognize their efforts and accomplishments (e.g. achieving step count goals). By the same token, however, sPGD could authoritatively reveal negative patterns of behavior or lack of progress in ways that might be demotivating. Thus, perceptions of sPGD as an unbiased signal could enhance or diminish motivation, largely reflecting the particular patterns the patient extracts from the data. Given the numerous potential patterns that patients could focus on within the Fitbit data, the input of the provider may become especially valuable to counteract negative biases, including by highlighting positive trends and accomplishments, or recommending against over-tracking in those who become fixated.
Our findings suggest that mental health providers may have an important role to play in situating sPGD, including reframing and refocusing data interpretation. These findings echo those of West et al. [112], who found that mental health providers perceived their patients to need help overcoming the substantial ambiguity of self-tracked mood ratings. It is worth noting that providers’ perspectives offer value in contexts beyond mental health, with work in physical health also suggesting the value of collaboration to overcome data ambiguity [75–77]. For instance, similar to our findings, Mentis et al. [76] describe “co-interpretation” that occurs as a negotiation between perspectives of patients and providers in clinic visits. Yet, as the next section describes, despite value of multiple perspectives for interpreting sPGD, providers in this setting faced barriers to taking on this role in routine practice.
7.2. Uncertainty and Risk of Non-Traditional Mental Health Data
In this section, we describe the barriers to integrating sPGD into mental health care, focusing on the ways providers are inhibited by uncertainty in deciding which measures to examine, lack of clarity on what sPGD-driven actions to take, and concerns that emphasis on sPGD might displace validated measures and better-established therapeutic activities.
7.2.1. PGD as an Unvalidated Measure.
In a commercial context, wearables provide data that may sometimes lack precision and accuracy, but that still generally fall within an acceptable “uncertainty tolerance” for consumers [65]. Providers using such devices, including those in mental health settings, may have substantially lower tolerance for risk. Indeed, managing risks and benefits for their patients is a large part of providers’ jobs, and prior work suggests that providers are often slow at adopting new technology because of concerns about liability and risk [48, 66]. To manage risk, providers typically rely on evidence-based practices, which include using validated measures and assessments. Commercial devices that passively capture PGD, such as Fitbits, have yet to be empirically validated for many of their potential uses in health care, particularly in mental health care. In physical health, many self-tracking technologies at least mirror “gold standard” analog tracking practices, such as blood glucose monitoring, calorie counting, and heart rate variability. In contrast, in mental health, sensors currently map onto symptoms like stress and depression in ambiguous ways, with “gold standard” measures generally coming from validated self-report instruments [38]. While a body of evidence is emerging to support correlations between sensed data and self-reported symptoms, such models generally combine an array of signals [78]. This work has also relied heavily on “black box” algorithms that people cannot easily understand [10]. At present, there is limited evidence that care team members can manually extract clinically meaningful information from self-tracked data from commercial wearables.
In medicine, risks of a new measure or approach can be justified at times based on potential clinical benefits. In this study, benefits were viewed as uncertain. While providers suggested possible therapeutic uses for sPGD, they also emphasized that benefits could be inconsistent across patients. With clinical relevance of sPGD to mental health still unclear, especially in contrast with evidence-based practices, it is unsurprising that providers were hesitant to engage with sPGD.
7.2.2. Organizational Fit & PGD.
While the providers described in this paper are on the front lines of this novel application of PGD to mental health, a number of organizational factors make them unlikely evangelists for new technologies.
First, these providers operated in an organizational context in which their workflows and incentives were closely tied to self-report measures of mental health symptoms that were not associated with Fitbit. In this context, if a provider dedicates time during a clinical interaction to interpreting sPGD, they risk disrupting the organization’s established practices. Such disruption could even come at the cost of patient health, since focusing on sPGD takes time and attention that might otherwise be applied to evidence-based treatment. Second, if a patient’s health does not improve per symptom questionnaires, the provider’s care process could even come under scrutiny, a possibility mentioned by at least one provider in this study. In general, providers wondered whether there was organizational buy-in for their role in supporting patient use of the Fitbit such that they would be appropriately trained and accommodated in taking on the substantial work and risk involved. Finally, when we consider health information technology, it is often important to evaluate innovations post-implementation to understand how workflows and other organizational features affect adoption [25]. However, sPGD creates an additional challenge because of the potential use of the collected data in the care process itself. With the growing emphasis on evidence-based practices in health care [37], administrators and policymakers will need to ensure that there is a strong evidence base supporting safety and effectiveness prior to even implementing sPGD technologies. Otherwise, providers may be reluctant to use these tools. Other studies have also highlighted unmalleable policies, introduction of new risks, and lack of incentives for adopting new work practices as major barriers to implementation [79, 84, 86, 109].
While these challenges to adoption are significant, CSCW and Implementation Science researchers highlight how we could begin to navigate organizational barriers [24, 35, 44]. For example, the CSCW community has highlighted the importance of understanding organization members’ interpretive frames for making sense of emerging technology [84] and the Implementation Science community has emphasized how willingness to adopt an innovation can reflect positive characteristics such as trialability, which may involve providing low-risk situations within which to experiment and become comfortable with new technologies [29, 34, 46]. This may also include the provision of training, a social climate where key stakeholders support social influence [27, 64], and where organization members can learn from other’s experience [18]. The success of sPGD in healthcare organizations will depend on ensuring the organizational readiness to adopt these tools.
7.3. Design Considerations for sPGD in Mental Health
In this section, we describe challenges designers face in supporting use of sPGD in mental health, including in facilitating data interpretation by both providers and patients. We also discuss considerations that may emerge as mental health states become more reliably linked to sensor-based data.
7.3.1. Designing for Multiple Perspectives.
Our findings suggest that providers and patients have different interpretive approaches and priorities for sPGD, with providers emphasizing opportunities to inform therapeutic activities, and patients looking to validate their experiences, enhance self-understanding, or motivate themselves outside the clinic. These differing patterns of interacting with the data suggest a need for different types of interfaces for different stakeholders to access, review, and interpret sPGD.
In considering possibilities of using sPGD in their work, mental health providers emphasized their need to constrain the application of sPGD to data considered more relevant and familiar, and for which the organization holds them accountable. Similarly, other studies have found that clinicians want patients to track data considered “clinically relevant” [112, 116]. Yet, in the present context, Fitbit use by patients is voluntary and self-directed, and providers have little control over what data patients track or share. To support extracting relevant information, providers will likely require more comprehensive, reliable, and timely access to data. While fundamental, this step is not simple. Prior work from a physical health context suggests barriers to data sharing including privacy concerns as well as incompatible formatting and challenges incorporating data within electronic health records [22, 112, 116]. Furthermore, having accessed data, providers likely need support to extract meaningful signals. This could be facilitated by automatic pattern recognition. For instance, prior work has generated alerts based on changes in physical activity as captured by wearable sensors [16], and changes in health status as captured through passive sensing in a housing facility [99]. Pattern recognition and interpretation can also be facilitated through automated data annotations, such as natural language captions for correlations between different self-tracked measures (e.g., sleep and stress) [10]. In past work, the presence of captions increased users’ understanding of behavioral patterns and of these patterns’ potential consequences. Visualizations may also help to make correlations between various signals salient (e.g., through bubble and bar charts) [96]. Finally, as Raj et al. [88] note, providers’ appropriate response to changes in patient status may require access to contextual information. For instance, providers may benefit from labels that specify whether data were collected when patients were at home, at work, or in the clinic.
Considering the needs of patients suggests additional design considerations. In particular, providers suggested negative consequences when patients over rely on quantified metrics in monitoring their health status, expressing concern that patients might use data in ways that manifest PTSD and its related symptoms by becoming fixated on the data or using it to harshly evaluate themselves. Such considerations could be addressed, in part, through the ways data is visualized. Researchers and designers in the HCI space have previously explored departures from numeric presentation of tracked data towards visual representations that allow for subjective interpretation and that prompt reflection and mindfulness. This has included imprinting physiological data on artifacts, such as when Howell et al. [51] created a shirt with a colorful display corresponding to emotion as detected by changes in the wearer’s skin conductance, and when Thieme et al. [105] created spheres with lights that fade in and out based on the holder’s heart rate. As for non-digital data representation, Snyder et al. [100] worked with individuals with bipolar disorder to create speculative visual representations of their lived experience. Although these examples might not translate into a clinical environment, they highlight a shift from quantified PGD to instead emphasize multiple possible meanings of data, potentially reducing fixation with quantified self-monitoring, as observed in this and other studies [59, 72, 96]. These potential benefits should be weighed against the usefulness of numeric representations in identifying trends and anomalies.
Design may also facilitate collaboration and integration of multiple perspectives. For example, Chung et al. [22] show that patients and providers rely on data artifacts to facilitate sharing and contextualizing self-tracking data. Through these data artifacts, patients and providers can prioritize topics of discussion to cover during clinic visits [96]. Each party also can draw attention to patterns that they find important, offering tentative accounts of the data’s meaning, perhaps through highlights or annotations [75]. Options to annotate data may be especially desirable in mental health, where patterns in sPGD cannot be interpreted without understanding the wearer’s subjective mental state. Additional considerations should be taken to constrain the annotation process given the numerous possible correlations to draw from the data. For instance, automated pattern recognition could be applied to identify a subset of patterns and anomalies from sPGD which the patient might then annotate, situating them in subjective experiences such as motivational states and occurrence of symptoms.
7.3.2. Leveraging Sensor Data in the Future.
This study investigated the ad-hoc use of a commercial wearable in a routine care setting, expanding a body of research on the clinical use of passively generated data in mental health. While our findings suggest a high level of ambiguity perceived in the signals from a commercial wearable in this care setting, this in part reflects that Fitbit and similar wearables focus on physical rather than mental health sensing. This will likely change in the future as research and development advance to better detect and predict mental health states through passively collected data, sometimes in combination with self-reported data [78, 106]. Much of the work in this area has leveraged smartphones rather than wearable devices, including smartphone-based sensing of geolocation, vocal quality, accelerometry, communication logs, and social interactions as based on co-presence of other devices and sampling of ambient noise [5, 33, 55, 78]. Other work has explored using physiological measurements not routinely available in commercial wearables, such as electrodermal activity [43]. In addition, digital trace data, such as social media posting content has been applied to predict mental health states [93]. As these advancements involve the collection of private and personal data, it is important to highlight recent work on passive tracking that has identified ethical concerns with privacy and monitoring of populations [91].
This work is still at an early stage and largely outside the awareness of the providers interviewed in this study. However, integration of these emerging methods into treatment and management of mental health must ultimately be informed by collaboration with the stakeholder communities these tools will impact, including patients, who will be asked to allow these devices to collect and transmit their personal data, and clinicians, who will be required to use this data to inform and adjust their clinical care.
8. FUTURE WORK
Our findings suggest some areas of further research. First, although a few collaborative uses of sPGD were being actively carried out in this care setting such as consulting with patients, most uses envisioned by providers were hypothetical. Other research methods may be needed to understand what collaborative uses of sPGD would look like on the ground. For example, research in this area might introduce prototypes to providers to elicit specific reactions that may inform how to design sPGD technologies and integrate them into workflows. Second, findings suggest that providers are concerned that patients’ PTSD might lead them to a biased and even dangerous interpretation of sPGD. Future work might seek to understand with greater specificity the nature of interpretive patterns among those with mental health conditions. For instance, some mental health conditions affect processes of social comparison (e.g., a tendency toward upward social comparisons that reinforce feelings of inadequacy), and this could manifest when using social features of self-tracking [3, 80]. In addition, future research might address how such interpretive biases can be addressed in collaborative processes outside the clinic. Work in both the physical and mental health domains acknowledges that self-tracking practices are shaped through input from others, including not just providers, but also friends, family, peers, and acquaintances [81, 110]. Applying the lens of situated objectivity, future work may ask what distinct perspectives individuals in these social roles can provide to better extract meaning from data and plan action. Third, a prior study investigated how veterans in the same ITP made use of Fitbit and its sPGD [82], and future research will involve comparing the perspectives of these two groups of stakeholders to understand where their perspectives do and do not align.
Finally, we noted a gap between providers’ envisioned uses of sPGD and their day-to-day practices, with perceived risks emerging as a major barrier to applying sPGD to therapy. While there are many variations of models explaining adoption of innovation in health care [26], future work might seek to understand whether different care settings and specializations place greater or lesser emphasis on risk. For example, mental health care providers may be particularly sensitive to risk given the perceived vulnerability of their patients. Understanding the role of risk may be crucial to facilitating further adoption of novel technologies in mental health care treatment.
9. LIMITATIONS
Our study had several limitations. First, our study was limited to one care setting, an intensive treatment program for PTSD. While such settings are common for PTSD treatment among returning veterans, it is unclear to what extent the use of sPGD would proceed similarly in other care settings, such as those that feature less time with patients, fewer providers, or different areas of specialty. Second, in this care setting, the specific wearables provided to patients were Fitbit brand. While we cannot generalize our findings to other sources of sPGD, Fitbit leads in the consumer market for wrist-worn wearables and has features common across many other such devices. Third, it is worth noting that the Fitbit is not designed for mental health specifically or for a clinical setting. Yet, as discussed throughout this paper, the type of information derived from the Fitbit may nonetheless include behavioral and physiological signals pertinent to mental health and its treatment.
10. CONCLUSIONS
In this intensive treatment program, mental health care providers identified opportunities for sPGD to empower their patients in managing PTSD, as well as potential to situate data in therapeutic expertise to guide data interpretation. However, while patients may have increasing interest in bringing these data into mental health treatment settings, providers had thus far not taken an active role in integrating sPGD into their practice. Provider perspectives highlight a number of challenges in adopting consumer-focused technologies in routine mental health care. Their hesitation reflects, in part, the lack of clear clinical relevance of the data. Furthermore, providers anticipated that substantial time and effort would be needed to appropriately understand and apply these new, complex data streams. Without organizational support, applying sPGD in therapy might compromise their ability to meet present professional objectives and standards based around established self-report metrics. These findings suggest areas of consideration when bringing self-tracked data into mental health care and highlight the importance of facilitating data interpretation, establishing clinical relevance, and managing risk. These issues will likely play an important role as wearables and their data further diffuse into mental health care.
ACKNOWLEDGEMENTS
We thank the clinical care team members for their participation. The Road Home Program: National Center of Excellence for Veterans and Their Families at Rush is supported by Wounded Warrior Project. We would also like to acknowledge the Robert Wood Johnson Foundation and Reos Partners for the authors’ involvement in a series of workshops on “Useful Cases for Co-Producing Health: Patient Generated Data in the Clinical Encounter” that featured this work. Rachel Kornfield is supported by a postdoctoral training grant from the National Institute of Mental Health (T32 MH115882). Alyson K. Zalta is supported by a career development award from the National Institute of Mental Health (K23 MH103394). REDCap Web application for managing surveys was made available through the Northwestern University Clinical and Translational Science Institute, which was funded in part by the National Institutes of Health’s (NIH) National Center for Advancing Translational Sciences (UL1TR001422). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Contributor Information
ADA NG, Northwestern University, USA.
RACHEL KORNFIELD, Northwestern University, USA.
STEPHEN M. SCHUELLER, University of California, Irvine, USA
ALYSON K. ZALTA, University of California, Irvine; Rush University Medical Center, USA
MICHAEL BRENNAN, Rush University Medical Center, USA.
MADHU REDDY, Northwestern University, USA.
REFERENCES
- [1].Abrantes Ana M, Blevins Claire E, Battle Cynthia L, Read Jennifer P, Gordon Alan L and Stein Michael D. 2017. Developing a Fitbit-supported lifestyle physical activity intervention for depressed alcohol dependent women. Journal of substance abuse treatment, 80 88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Ahuja Neera, Ozdalga Errol and Aaronson Alistair. 2017. Integrating mobile fitness trackers into the practice of medicine. American journal of lifestyle medicine, 11 (1). 77–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Appel Helmut, Crusius Jan and Gerlach Alexander L. 2015. Social comparison, envy, and depression on Facebook: A study looking at the effects of high comparison standards on depressed individuals. Journal of Social and Clinical Psychology, 34 (4). 277–289. [Google Scholar]
- [4].American Psychiatric Association. 2013. Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub. [Google Scholar]
- [5].Barnett Ian, Torous John, Staples Patrick, Sandoval Luis, Keshavan Matcheri and Onnela Jukka-Pekka. 2018. Relapse prediction in schizophrenia through digital phenotyping: a pilot study. Neuropsychopharmacology. 43 1660–1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Barrett Drue H, Doebbeling Caroline Carney, Schwartz David A, Voelker Margaret D, Falter Kenneth H, Woolson Robert F and Doebbeling Bradley N. 2002. Posttraumatic stress disorder and self-reported physical health status among US Military personnel serving during the Gulf War period: a population-based study. Psychosomatics, 43 (3). 195–205. [DOI] [PubMed] [Google Scholar]
- [7].Batsis John A, Naslund John A, Gill Lydia E, Masutani Rebecca K, Agarwal Nayan and Bartels Stephen J. 2016. Use of a wearable activity device in rural older obese adults: A pilot study. Gerontology and geriatric medicine, 2 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Bauer Amy M, Thielke Stephen M, Katon Wayne, Unutzer Jurgen and Arean Patricia. 2014. Aligning health information technologies with effective service delivery models to improve chronic disease care. Preventive medicine, 66 167–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Ben-Zeev Dror, Scherer Emily A, Wang Rui, Xie Haiyi and Campbell Andrew T. 2015. Next-generation psychiatric assessment: Using smartphone sensors to monitor behavior and mental health. Psychiatric rehabilitation journal, 38 (3). 218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bentley Frank, Tollmar Konrad, Stephenson Peter, Levy Laura, Jones Brian, Robertson Scott, Price Ed, Catrambone Richard and Wilson Jeff. 2013. Health Mashups: Presenting statistical patterns between wellbeing data and context in natural language to promote behavior change. ACM Transactions on Computer-Human Interaction (TOCHI), 20 (5). 30. [Google Scholar]
- [11].Blevins Christy A, Weathers Frank W, Davis Margaret T, Witte Tracy K and Domino Jessica L. 2015. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28 (6). 489–498. [DOI] [PubMed] [Google Scholar]
- [12].Bovin Michelle J, Marx Brian P, Weathers Frank W, Gallagher Matthew W, Rodriguez Paola, Schnurr Paula P and Keane Terence M. 2016. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28 (11). 1379. [DOI] [PubMed] [Google Scholar]
- [13].Braun Virginia and Clarke Victoria. 2006. Using thematic analysis in psychology. Qualitative research in psychology, 3 (2). 77–101. [Google Scholar]
- [14].Byrnes Elizabeth and Johnson James H. 1981. Change technology and the implementation of automation in mental health care settings. Behavior Research Methods & Instrumentation, 13 (4). 573–580. [Google Scholar]
- [15].Cacciola John S, Alterman Arthur I, DePhilippis Dominick, Drapkin Michelle L, Valadez Charles Jr, Fala Natalie C, Oslin David and McKay James R. 2013. Development and initial evaluation of the Brief Addiction Monitor (BAM). Journal of Substance Abuse Treatment, 44 (3). 256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Candás Juan Luis Carús, Peláez Víctor, López Gloria, Fernández Miguel Ángel, Álvarez Eduardo and Díaz Gabriel. 2014. An automatic data mining method to detect abnormal human behaviour using physical activity measurements. Pervasive and Mobile Computing, 15 228–241. [Google Scholar]
- [17].Chan Domin, Cheadle Allen D, Reiber Gayle, Unutzer Jürgen and Chaney Edmund F. 2009. Health care utilization and its costs for depressed veterans with and without comorbid PTSD symptoms. Psychiatric Services, 60 (12). 1612–1617. [DOI] [PubMed] [Google Scholar]
- [18].Choe Eun Kyoung, Lee Nicole B, Lee Bongshin, Pratt Wanda and Kientz Julie A. 2014. Understanding quantified-selfers’ practices in collecting and exploring personal data. In Proceedings of the 32nd annual ACM conference on Human factors in computing systems, ACM, 1143–1152. [Google Scholar]
- [19].Choo Seryung, Kim Ju Young, Jung Se Young, Kim Sarah, Kim Jeong Eun, Han Jong Soo, Kim Sohye, Kim Jeong Hyun, Kim Jeehye and Kim Yongseok. 2016. Development of a weight loss mobile app linked with an accelerometer for use in the clinic: usability, acceptability, and early testing of its impact on the patient-doctor relationship. JMIR mHealth and uHealth, 4 (1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Chum Jenny, Kim Min Suk, Zielinski Laura, Bhatt Meha, Chung Douglas, Yeung Sharon, Litke Kathryn, McCabe Kathleen, Whattam Jeff and Garrick Laura. 2017. Acceptability of the Fitbit in behavioural activation therapy for depression: a qualitative study. Evidence-based mental health. 20(4), 128–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Chung Chia-Fang, Cook Jonathan, Bales Elizabeth, Zia Jasmine and Munson Sean A. 2015. More than telemonitoring: health provider use and nonuse of life-log data in irritable bowel syndrome and weight management. Journal of medical Internet research, 17 (8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Chung Chia-Fang, Dew Kristin, Cole Allison, Zia Jasmine, Fogarty James, Kientz Julie A and Munson Sean A. 2016. Boundary negotiating artifacts in personal informatics: Patient-provider collaboration with patient-generated data. In Proceedings of the 19th ACM Conference on Computer-Supported Cooperative Work & Social Computing, ACM, 770–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Collins Pamela Y, Patel Vikram, Joestl Sarah S, March Dana, Insel Thomas R, Daar Abdallah S, Bordin Isabel A, Costello E Jane, Durkin Maureen and Fairburn Christopher. 2011. Grand challenges in global mental health. Nature, 475 (7354). 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Colusso Lucas, Bennett Cynthia L, Hsieh Gary and Munson Sean A. 2017. Translational resources: Reducing the gap between academic research and HCI practice. In Proceedings of the 2017 Conference on Designing Interactive Systems, ACM, 957–968. [Google Scholar]
- [25].Cresswell Kathrin M, Blandford Ann and Sheikh Aziz. 2017. Drawing on human factors engineering to evaluate the effectiveness of health information technology. Journal of the Royal Society of Medicine, 110 (8). 309–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Cresswell Kathrin and Sheikh Aziz. 2013. Organizational issues in the implementation and adoption of health information technology innovations: an interpretative review. International journal of medical informatics, 82 (5). e73–e86. [DOI] [PubMed] [Google Scholar]
- [27].Damschroder Laura J, Aron David C, Keith Rosalind E, Kirsh Susan R, Alexander Jeffery A and Lowery Julie C. 2009. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation science, 4 (1). 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Daston Lorraine and Galison Peter. 2007. Objectivity Zone, Brooklyn, NY. [Google Scholar]
- [29].Denis Jean-Louis, Hebert Yann, Langley Ann, Lozeau Daniel and Trottier Louise-Helene. 2002. Explaining diffusion patterns for complex health care innovations. Health care management review, 27 (3). 60–73. [DOI] [PubMed] [Google Scholar]
- [30].Depp Colin, Torous John and Thompson Wesley. 2016. Technology-based early warning systems for bipolar disorder: a conceptual framework. JMIR mental health, 3 (3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Druss Benjamin G, Hwang Irving, Petukhova Masha, Sampson Nancy A, Wang Philip S and Kessler Ronald C. 2009. Impairment in role functioning in mental and chronic medical disorders in the United States: results from the National Comorbidity Survey Replication. Molecular psychiatry, 14 (7). 728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Druss Benjamin G, Marcus Steven C, Rosenheck Robert A, Olfson Mark, Tanielian Terri and Pincus Harold A. 2000. Understanding disability in mental and general medical conditions. American Journal of Psychiatry, 157 (9). 1485–1491. [DOI] [PubMed] [Google Scholar]
- [33].Faurholt-Jepsen Maria, Busk Jonas, Frost Mads, Vinberg Maj, Christensen Ellen M, Winther Ole, Bardram Jakob Eyvind and Kessing Lars V. 2016. Voice analysis as an objective state marker in bipolar disorder. Translational psychiatry, 6 (7). e856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Ferlie Ewan, Gabbay John, Fitzgerald Louise, Locock Louise and Dopson Sue. 2001. Evidence-based medicine and organisational change: an overview of some recent qualitative research. 18–42. [Google Scholar]
- [35].Fitzpatrick Geraldine and Ellingsen Gunnar. 2013. A review of 25 years of CSCW research in healthcare: contributions, challenges and future agendas. Computer Supported Cooperative Work (CSCW), 22 (4–6). 609–665. [Google Scholar]
- [36].Foa Edna B, Ehlers Anke, Clark David M, Tolin David F and Orsillo Susan M. 1999. The posttraumatic cognitions inventory (PTCI): Development and validation. Psychological assessment, 11 (3). 303. [Google Scholar]
- [37].APA Task Force. 2006. APA presidential task force on evidence based practice. American Psychologist, 61 271–285. [DOI] [PubMed] [Google Scholar]
- [38].Fortney John C, Unutzer Jurgen, Wrenn Glenda, Pyne Jeffrey M, Smith G Richard, Michael Schoenbaum and Henry T Harbin. 2016. A tipping point for measurement-based care. Psychiatric Services, 68 (2). 179–188. [DOI] [PubMed] [Google Scholar]
- [39].Frank Jerome D and Frank Julia B. 1993. Persuasion and healing: A comparative study of psychotherapy. JHU Press. [Google Scholar]
- [40].Frayne Susan M, Chiu Victor Y, Iqbal Samina, Berg Eric A, Laungani Kaajal J, Cronkite Ruth C, Pavao Joanne and Kimerling Rachel. 2011. Medical care needs of returning veterans with PTSD: their other burden. Journal of general internal medicine, 26 (1). 33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Friedman Matthew J, Keane Terence M and Resick Patricia A. 2007. Handbook of PTSD: Science and practice. Guilford Press; New York, NY. [Google Scholar]
- [42].Fulton Jessica J, Calhoun Patrick S, Wagner H Ryan, Schry Amie R, Hair Lauren P, Feeling Nicole, Elbogen Eric and Beckham Jean C. 2015. The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans: a meta-analysis. Journal of anxiety disorders, 31 98–107. [DOI] [PubMed] [Google Scholar]
- [43].Ghandeharioun Asma, Fedor Szymon, Sangermano Lisa, Ionescu Dawn, Alpert Jonathan, Dale Chelsea, Sontag David and Picard Rosalind. 2017. Objective assessment of depressive symptoms with machine learning and wearable sensors data. In 2017 Seventh International Conference on Affective Computing and Intelligent Interaction (ACE), IEEE, 325–332. [Google Scholar]
- [44].Glasgow Russell E, Vinson Cynthia, Chambers David, Khoury Muin J, Kaplan Robert M and Hunter Christine. 2012. National Institutes of Health approaches to dissemination and implementation science: current and future directions. American journal of public health, 102 (7). 1274–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Granado-Font Esther, Flores-Mateo Gemma, Sorlí-Aguilar Mar, Montaña-Carreras Xavier, Ferre-Grau Carme, Barrera-Uriarte Maria-Luisa, Oriol-Colominas Eulàlia, Rey-Reñones Cristina, Caules Iolanda and Satué-Gracia Eva-María. 2015. Effectiveness of a Smartphone application and wearable device for weight loss in overweight or obese primary care patients: protocol for a randomised controlled trial. BMC Public Health, 15 (1). 531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Greenhalgh Trisha, Robert Glenn, Macfarlane Fraser, Bate Paul and Kyriakidou Olivia. 2004. Diffusion of innovations in service organizations: systematic review and recommendations. The Milbank Quarterly, 82 (4). 581–629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Harding Kelli Jane K, Rush A John, Arbuckle Melissa, Trivedi Madhukar H and Pincus Harold Alan. 2011. Measurement-based care in psychiatric practice: a policy framework for implementation. The Journal of clinical psychiatry. 72(8):1136–1143. [DOI] [PubMed] [Google Scholar]
- [48].Harrison Michael I, Koppel Ross and Bar-Lev Shirly. 2007. Unintended consequences of information technologies in health care—an interactive sociotechnical analysis. Journal of the American medical informatics Association, 14 (5). 542–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Harvey Margaret M, Rauch Sheila AM, Zalta Alyson K, Sornborger Jo, Pollack Mark H, Rothbaum Barbara O, Laifer Lauren M and Simon Naomi M. 2017. Intensive Treatment Models to Address Posttraumatic Stress Among Post-9/11 Warriors: The Warrior Care Network. Focus, 15 (4). 378–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Institute of Medicine. 2005. Committee On Crossing The Quality Chasm: Adaptation To Mental Health And Addictive Disorders: Improving The Quality Of Health Care For Mental And Substance-Use Conditions. National Academy Press; Washington, D.C. [Google Scholar]
- [51].Howell Noura, Devendorf Laura, Galvez Tomas Alfonso Vega, Tian Rundong and Ryokai Kimiko. 2018. Tensions of data-driven reflection: A case study of real-time emotional biosensing. In Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems, ACM, 431. [Google Scholar]
- [52].Hundt Natalie E, Mott Juliette M, Miles Shannon R, Arney Jennifer, Cully Jeffrey A and Stanley Melinda A. 2015. Veterans’ perspectives on initiating evidence-based psychotherapy for posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 7 (6). 539. [DOI] [PubMed] [Google Scholar]
- [53].IDC. 2019. IDC Reports Strong Growth in the Worldwide Wearables Market, Led by Holiday Shipments of Smartwatches, Wrist Bands, and Ear-Worn Devices. Retrieved from https://www.idc.com/getdoc.jsp?containerId=prUS44901819.
- [54].Apple Inc. 2019. Retrieved March 28, 2019 from https://www.apple.com/apple-watch-series-4.
- [55].Jarden Aaron. 2017. An Interview with Victor J. Strecher. International Journal of Wellbeing, 7 (2). [Google Scholar]
- [56].Jayakody Kaushadh, Gunadasa Shalmini and Hosker Christian. 2014. Exercise for anxiety disorders: systematic review. Br J Sports Med, 48 (3). 187–196. [DOI] [PubMed] [Google Scholar]
- [57].Kehle Shannon M, Greer Nancy, Rutks Indulis and Wilt Timothy. 2011. Interventions to improve veterans’ access to care: a systematic review of the literature. Journal of general internal medicine, 26 (2). 689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Kehle-Forbes Shannon M, Meis Laura A, Spoont Michele R and Polusny Melissa A. 2016. Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a VA outpatient clinic. Psychological Trauma: Theory, Research, Practice, and Policy, 8 (1). 107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Kelley Christina, Lee Bongshin and Wilcox Lauren. 2017. Self-tracking for mental wellness: understanding expert perspectives and student experiences. In Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems, ACM, 629–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Keogh Edmund and Asmundson Gordon JG. 2004. Negative affectivity, catastrophizing, and anxiety sensitivity. Understanding and treating fear of pain. 91–115. [Google Scholar]
- [61].Kessler Ronald C. 2000. Posttraumatic stress disorder: the burden to the individual and to society. The Journal of clinical psychiatry. 61(5). 4–12. [PubMed] [Google Scholar]
- [62].Kessler Ronald C, Berglund Patricia, Demler Olga, Jin Robert, Merikangas Kathleen R and Walters Ellen E. 2005. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. [DOI] [PubMed] [Google Scholar]
- [63].Kessler Ronald C, Chiu Wai Tat, Demler Olga and Walters Ellen E. 2005. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry, 62 (6). 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Kilbourne Amy M, Neumann Mary S, Pincus Harold A, Bauer Mark S and Stall Ronald. 2007. Implementing evidence-based interventions in health care: application of the replicating effective programs framework. Implementation Science, 2 (1). 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Knowles Bran, Smith-Renner Alison, Poursabzi-Sangdeh Forough, Lu Di and Alabi Halimat. 2018. Uncertainty in current and future health wearables. Communications of the ACM, 61 (12). 62–67. [Google Scholar]
- [66].Koppel Ross and Kreda David. 2009. Health care information technology vendors'“hold harmless" clause: implications for patients and clinicians. JAMA, 301 (12). 1276–1278. [DOI] [PubMed] [Google Scholar]
- [67].Kroenke Kurt and Spitzer Robert L. 2002. The PHQ-9: a new depression diagnostic and severity measure. Psychiatric annals, 32 (9). 509–515. [Google Scholar]
- [68].Kubany Edward S, Haynes Stephen N, Abueg Francis R, Manke Frederic P, Brennan Jerry M and Stahura Catherine. 1996. Development and validation of the Trauma-Related Guilt Inventory (TRGI). Psychological Assessment, 8 (4). 428. [Google Scholar]
- [69].Kumar Rajiv B, Goren Nira D, Stark David E, Wall Dennis P and Longhurst Christopher A. 2016. Automated integration of continuous glucose monitor data in the electronic health record using consumer technology. Journal of the American Medical Informatics Association, 23 (3). 532–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Landry Brian M, Kyoung Choe Eun, McCutcheon Stephen and Kientz Julie A. 2010. Post-traumatic stress disorder: opportunities & challenges for computing technology. In Proceedings of the 1st ACM International Health Informatics Symposium, ACM, 780–789. [Google Scholar]
- [71].Lewis Cara C, Boyd Meredith, Puspitasari Ajeng, Navarro Elena, Howard Jacqueline, Kassab Hannah, Hoffman Mira, Scott Kelli, Lyon Aaron and Douglas Susan. 2019. Implementing Measurement-Based Care in Behavioral Health: A Review. JAMA psychiatry, 76 (3). 324–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Lupton Deborah. 2013. Quantifying the body: monitoring and measuring health in the age of mHealth technologies. Critical Public Health, 23 (4). 393–403. [Google Scholar]
- [73].Madan Anmol, Cebrian Manuel, Lazer David and Pentland Alex. 2010. Social sensing for epidemiological behavior change. In Proceedings of the 12th ACM international conference on Ubiquitous computing, ACM, 291–300. [Google Scholar]
- [74].Meng Jingbo, Hussain Syed Ali, Mohr David C, Czerwinski Mary and Zhang Mi. 2018. Exploring User Needs for a Mobile Behavioral-Sensing Technology for Depression Management: Qualitative Study. Journal of medical Internet research, 20 (7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Mentis Helena M, Komlodi Anita, Schrader Katrina, Phipps Michael, Gruber-Baldini Ann, Yarbrough Karen and Shulman Lisa. 2017. Crafting a view of self-tracking data in the clinical visit. In Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems, ACM, 5800–5812. [Google Scholar]
- [76].Mentis Helena M, Shewbridge Rita, Powell Sharon, Armstrong Melissa, Fishman Paul and Shulman Lisa. 2016. Co-interpreting movement with sensors: assessing Parkinson’s patients’ deep brain stimulation programming. Human-Computer Interaction, 31 (3–4). 227–260. [Google Scholar]
- [77].Mishra Sonali R, Miller Andrew D, Haldar Shefali, Khelifi Maher, Eschler Jordan, Elera Rashmi G, Pollack Ari H and Pratt Wanda. 2018. Supporting Collaborative Health Tracking in the Hospital: Patients’ Perspectives. In Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems, ACM, 650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Mohr David C, Zhang Mi and Schueller Stephen M. 2017. Personal sensing: understanding mental health using ubiquitous sensors and machine learning. Annual review of clinical psychology, 13 23–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Munkvold Bjorn E. 1999. Challenges of IT implementation for supporting collaboration in distributed organizations. European Journal of Information Systems, 8 (4). 260–272. [Google Scholar]
- [80].Munson Sean A and Consolvo Sunny. 2012. Exploring goal-setting, rewards, self-monitoring, and sharing to motivate physical activity. In 2012 6th International Conference On Pervasive Computing Technologies For Healthcare (PervasiveHealth) And Workshops, IEEE, 25–32. [Google Scholar]
- [81].Murnane Elizabeth L, Walker Tara G, Tench Beck, Voida Stephen and Snyder Jaime. 2018. Personal Informatics in Interpersonal Contexts: Towards the Design of Technology that Supports the Social Ecologies of Long-Term Mental Health Management. In Proceedings of the ACM on Human-Computer Interaction, 2 (CSCW; ). 127. [Google Scholar]
- [82].Ng Ada, Reddy Madhu, Zalta Alyson K and Schueller Stephen M. 2018. Veterans’ Perspectives on Fitbit Use in Treatment for Post-Traumatic Stress Disorder: An Interview Study. JMIR mental health, 5 (2). e10415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Onnela Jukka-Pekka and Rauch Scott L. 2016. Harnessing smartphone-based digital phenotyping to enhance behavioral and mental health. Neuropsychopharmacology, 41 (7). 1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Orlikowski Wanda J. 1993. Learning from notes: Organizational issues in groupware implementation. 237–250. [Google Scholar]
- [85].Pantzar Mika and Ruckenstein Minna. 2017. Living the metrics: Self-tracking and situated objectivity. Digital health, 3 2055207617712590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Pratt Wanda, Reddy Madhu C, McDonald David W, Tarczy-Hornoch Peter and Gennari John H. 2004. Incorporating ideas from computer-supported cooperative work. Journal of biomedical informatics, 37 (2). 128–137. [DOI] [PubMed] [Google Scholar]
- [87].BV PricewaterhouseCoopers. 2014. Consumer intelligence series the wearable future. Retreived from https://www.pwc.com/us/en/industries/technology/library/wearable-technology.html.
- [88].Raj Shriti, Toporski Kelsey, Garrity Ashley, Lee Joyce M and Newman Mark W. 2019. My blood sugar is higher on the weekends: Finding a Role for Context and Context-Awareness in the Design of Health Self-Management Technology. In Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems, ACM, 119. [Google Scholar]
- [89].Ravichandran Ruth, Sien Sang-Wha, Patel Shwetak N, Kientz Julie A and Pina Laura R. 2017. Making sense of sleep sensors: How sleep sensing technologies support and undermine sleep health. In Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems, ACM, 6864–6875. [Google Scholar]
- [90].Resick Patricia A, Monson Candice M and Chard Kathleen M. 2016. Cognitive processing therapy for PTSD: A comprehensive manual. Guilford Publications; New York, NY. [Google Scholar]
- [91].Rooksby John, Morrison Alistair and Murray-Rust Dave. 2019. Student Perspectives on Digital Phenotyping: The Acceptability of Using Smartphone Data to Assess Mental Health. In Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems, ACM, 425. [Google Scholar]
- [92].Saeb Sohrab, Lattie Emily G, Schueller Stephen M, Kording Konrad P and Mohr David C. 2016. The relationship between mobile phone location sensor data and depressive symptom severity. PeerJ, 4 e2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Saha Koustuv, Bayraktaroglu Ayse E, Campbell Andrew T, Chawla Nitesh V, De Choudhury Munmun, D’Mello Sidney K, Dey Anind K, Gao Ge, Gregg Julie M and Jagannath Krithika. 2019. Social media as a passive sensor in longitudinal studies of human behavior and wellbeing. In Extended Abstracts of the 2019 CHI Conference on Human Factors in Computing Systems, ACM, CS12. [Google Scholar]
- [94].Sanches Pedro, Janson Axel, Karpashevich Pavel, Nadal Camille, Qu Chengcheng, Roquet Claudia Daudén, Umair Muhammad, Windlin Charles, Doherty Gavin and Höök Kristina. 2019. HCI and Affective Health: Taking stock of a decade of studies and charting future research directions. In Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems, ACM, 245. [Google Scholar]
- [95].Schramm Elisabeth, van Calker Dietrich, Dykierek Petra, Lieb Klaus, Psych Sabine Kech D Clin, Psych Ingo Zobel D Clin, Psych Rainer Leonhart D Clin and Berger Mathias. 2007. An intensive treatment program of interpersonal psychotherapy plus pharmacotherapy for depressed inpatients: acute and long-term results. American Journal of Psychiatry, 164 (5). 768–777. [DOI] [PubMed] [Google Scholar]
- [96].Schroeder Jessica, Hoffswell Jane, Chung Chia-Fang, Fogarty James, Munson Sean and Zia Jasmine. 2017. Supporting patient-provider collaboration to identify individual triggers using food and symptom journals. In CSCW: proceedings of the Conference on Computer-Supported Cooperative Work. Conference on Computer-Supported Cooperative Work, NIH Public Access, 1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97].Seal Karen H, Maguen Shira, Cohen Beth, Gima Kristian S, Metzler Thomas J, Ren Li, Bertenthal Daniel and Marmar Charles R. 2010. VA mental health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses. Journal of traumatic stress, 23 (1). 5–16. [DOI] [PubMed] [Google Scholar]
- [98].Shiffman Saul, Stone Arthur A and Hufford Michael R. 2008. Ecological momentary assessment. Annu. Rev. Clin. Psychol, 4 1–32. [DOI] [PubMed] [Google Scholar]
- [99].Skubic Marjorie, Guevara Rainer Dane and Rantz Marilyn. 2015. Automated health alerts using in-home sensor data for embedded health assessment. IEEE journal of translational engineering in health and medicine, 3 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Snyder Jaime, Murnane Elizabeth, Lustig Caitie and Voida Stephen. 2019. Visually Encoding the Lived Experience of Bipolar Disorder. In Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems, ACM, 133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Spitzer Robert L, Kroenke Kurt, Williams Janet BW and Lowe Bernd. 2006. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of internal medicine, 166 (10). 1092–1097. [DOI] [PubMed] [Google Scholar]
- [102].Stephenson Aoife, McDonough Suzanne M, Murphy Marie H, Nugent Chris D and Mair Jacqueline L. 2017. Using computer, mobile and wearable technology enhanced interventions to reduce sedentary behaviour: a systematic review and meta-analysis. International Journal of Behavioral Nutrition and Physical Activity, 14 (1). 105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Stricker George and Widiger Thomas A. 2003. Handbook of psychology. Psychopathology, 1 1. [Google Scholar]
- [104].Swan Melanie. 2009. Emerging patient-driven health care models: an examination of health social networks, consumer personalized medicine and quantified self-tracking. International journal of environmental research and public health, 6 (2). 492–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [105].Thieme Anja, Wallace Jayne, Johnson Paula, John McCarthy Sian Lindley, Wright Peter, Olivier Patrick and Meyer Thomas D. 2013. Design to promote mindfulness practice and sense of self for vulnerable women in secure hospital services. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, ACM, 2647–2656. [Google Scholar]
- [106].Torous John, Onnela J-P and Keshavan Matcheri. 2017. New dimensions and new tools to realize the potential of RDoC: digital phenotyping via smartphones and connected devices. Translational psychiatry, 7 (3). e1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [107].Tversky Amos and Kahneman Daniel. 1973. Availability: A heuristic for judging frequency and probability. Cognitive psychology, 5 (2). 207–232. [Google Scholar]
- [108].van der Kolk Bessel A, Stone Laura, West Jennifer, Rhodes Alison, Emerson David, Suvak Michael and Spinazzola Joseph. 2014. Original research yoga as an adjunctive treatment for posttraumatic stress disorder: A randomized controlled trial. J Clin Psychiatry, 75 (6). e559–e565. [DOI] [PubMed] [Google Scholar]
- [109].Vikkelsø Signe. 2005. Subtle redistribution of work, attention and risks: Electronic patient records and organisational consequences. Scandinavian Journal of Information Systems, 17 (1). 10. [Google Scholar]
- [110].Vizer Lisa M, Eschler Jordan, Koo Bon Mi, Ralston James, Pratt Wanda and Munson Sean. 2019. “It’s Not Just Technology, It’s People”: Constructing a Conceptual Model of Shared Health Informatics for Tracking in Chronic Illness Management. Journal of medical Internet research, 21 (4). e10830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111].Watts Bradley V, Shiner Brian, Zubkoff Lisa, Carpenter-Song Elizabeth, Ronconi Julia M and Coldwell Craig M. 2014. Implementation of evidence-based psychotherapies for posttraumatic stress disorder in VA specialty clinics. Psychiatric Services, 65 (5). 648–653. [DOI] [PubMed] [Google Scholar]
- [112].West Peter, Van Kleek Max, Giordano Richard, Weal Mark J and Shadbolt Nigel. 2018. Common Barriers to the Use of Patient-Generated Data Across Clinical Settings. In Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems, ACM, 484. [Google Scholar]
- [113].Whealin Julia M, Jenchura Emily C, Wong Ava C and Zulman Donna M. 2016. How Veterans with post-traumatic stress disorder and comorbid health conditions utilize ehealth to manage their health care needs: a mixed-methods analysis. Journal of medical Internet research, 18 (10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [114].Wipfli Bradley M, Rethorst Chad D and Landers Daniel M. 2008. The anxiolytic effects of exercise: a meta-analysis of randomized trials and dose-response analysis. Journal of Sport and Exercise Psychology, 30 (4). 392–410. [DOI] [PubMed] [Google Scholar]
- [115].Zalta Alyson K, Held Philip, Smith Dale L, Klassen Brian J, Lofgreen Ashton M, Normand Patricia S, Brennan Michael B, Rydberg Thad S, Boley Randy A and Pollack Mark H. 2018. Evaluating patterns and predictors of symptom change during a three-week intensive outpatient treatment for veterans with PTSD. BMC psychiatry, 18 (1). 242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Zhu Haining, Colgan Joanna, Reddy Madhu and Choe Eun Kyoung. 2016. Sharing patient-generated data in clinical practices: an interview study. In AMIA Annual Symposium Proceedings, American Medical Informatics Association, 1303. [PMC free article] [PubMed] [Google Scholar]


