Abstract
Background:
The fourth wave of the opioid crisis is characterized by increased use and co-use of methamphetamine. How opioid and methamphetamine co-use is associated with health care use, housing instability, social service use, and criminal justice involvement has not been studied and could inform future interventions and partnerships.
Objectives:
To estimate service involvement across sectors among people who reported past year opioid and methamphetamine co-use, methamphetamine use, opioid use, or neither opioid nor methamphetamine use.
Research Design:
We examined 2015–2018 data from the National Survey on Drug Use and Health. We used multivariable negative binomial and logistic regression models and predictive margins, adjusted for sociodemographic and clinical characteristics.
Subjects:
Non-elderly US adults aged 18 or older.
Measures:
Hospital days, emergency department visits, housing instability, social service use, and criminal justice involvement in the past year.
Results:
In adjusted analyses, adults who reported opioid and methamphetamine co-use had 99% more overnight hospital days, 46% more emergency department visits, 2.1 times more housing instability, 1.4 times more social service use, and 3.3 times more criminal justice involvement compared to people with opioid use only. People who used any methamphetamine, with opioids or alone, were significantly more likely be involved with services in 2 or more sectors compared with those who used opioids only (Opioids only: 11.6%; methamphetamine only: 19.8%; opioids and methamphetamine: 27.6%).
Conclusions:
Multi-sector service involvement is highest among those who use both opioids and methamphetamine, suggesting that partnerships between health care, housing, social service, and criminal justice agencies are needed to develop, test, and implement interventions to reduce methamphetamine-related morbidity.
Keywords: methamphetamine use, opioid use, polysubstance use, cross-sector service use, criminal justice involvement
Background:
Opioid overdose deaths in the United States (US) remain at unprecedented levels and represent an ongoing public health crisis. Deaths related to methamphetamine and other psychostimulants have increased over six-fold during the last decade, further complicating the crisis.(1) Co-occurring opioid and methamphetamine use, and methamphetamine only, now represent the fourth wave of the overdose crisis.(2, 3) Co-use of opioids and methamphetamine in the US increased 86% among those seeking treatment for opioid use disorder (4–6) and hospitalizations involving both opioids and methamphetamine increased over 500% between 2003 and 2015.(7) Methamphetamine use alone is associated with significant morbidity, including increased psychiatric morbidity,(8–10) high-risk sexual behavior,(11, 12) HIV infection,(13–15) and heart disease,(9, 13) which further complicates opioid use and its health consequences.
To address the opioid overdose epidemic, there have been efforts to understand how interactions with health care and non-health care sectors influence overdose risk.(16) Cross-sector analysis examines how patients intersect with health care, housing, social service, and criminal justice systems to identify novel opportunities to engage people in treatment and develop collaborations across normally siloed sectors.(17–20) It is unknown whether service involvement across sectors among adults who use both opioids and methamphetamine, or methamphetamine only, differ from people who report opioid use only.(21, 22) While effective treatments for methamphetamine use are limited, cross-sector data could identify partnerships to develop novel programs and/or reduce methamphetamine-associated harms.(23)
Our objective was to use nationally representative data to describe hospital and emergency department use, housing instability, social service use, and criminal justice involvement among people who co-use opioids and methamphetamine or use methamphetamine only compared to the general population and to people who use opioids only. We hypothesized that methamphetamine use would be associated with higher utilization of services across multiple sectors compared with opioid use and that people who co-use methamphetamine and opioids would have the highest rates of service use.
Methods:
We used 2015–2018 data from the National Survey on Drug Use and Health (NSDUH), an annual survey of the non-institutionalized US population designed to estimate the prevalence of substance use and mental illness. The NSDUH uses a complex survey design in all 50 states and includes approximately 55,000 residents age 12 and older in each annual, de-identified public use data set.(24) We limited our analyses to respondents age 18 or older.
Independent variable: past year substance use
Our exposures of interest were any reported illicit opioid use in the past year but no methamphetamine use, methamphetamine use in the past year but no illicit opioid use, use of both illicit opioids and methamphetamine in the past year, or neither opioid nor methamphetamine use in the past year (herein no opioid/methamphetamine use). Illicit opioid use (herein opioid use) was defined as heroin use or any use of prescription opioids that were not taken as directed by a doctor in the past year.
Dependent variables: cross-sector service involvement
Our main outcomes were involvement in services in four domains and in multiple of these domains in the past year: acute health care use (i.e., number hospital days, number of emergency department visit), housing instability, social service use, and criminal justice involvement. For acute health care use, we created count variables of number of hospital days and emergency room visits in the past year. In line with other cross-sector service analysis(25–27), we included a variable for housing sector use, but were limited by NSDUH data. As a proxy for housing sector use, we dichotomized responses on housing instability similar to specifications used in previous work: moved zero or one time in the past year vs. moved two or more times in the past year.(28, 29) We identified respondents as using social services if they reported receiving social security income, food stamps, cash assistance, or non-cash assistance (e.g., childcare) through a government program in the past year. We identified a respondent as having criminal justice involvement in the past year if they reported an arrest in the past year or having been on probation or parole in the past year.
We created a multi-sector involvement variable that totaled the number of sectors in which an individual reported past year involvement: (zero sectors, one sector, or two or more sectors.)
Covariates
We included the following covariates in our adjusted analyses: age, race/ethnicity, gender, poverty, rurality, serious psychological distress, and self-reported health. These covariates were included to address potential confounding by demographic and clinical factors previously associated with higher service utilization.(23, 30, 31) For our analyses, we collapsed rural-urban continuum codes (RUCC) developed by the US Department of Agriculture into two categories: urban (RUCC 1–3) and rural (RUCC 4–9).(32) We coded presence of serious psychological distress using a score of greater than or equal to 13 on the Kessler Psychological Distress Scale (K6), a validated screening tool for detecting serious mental illness in the general population. (33)
Statistical Analysis
We first estimated and compared weighted proportion of demographic and clinical characteristics for adults who reported no opioid/methamphetamine use, opioid use only, methamphetamine use only, or opioid and methamphetamine use. We then described demographic and clinical factors of people who reported service involvement in individual sectors and service involvement in 2 or more sectors.
Next, we estimated weighted frequencies of inpatient hospital days, emergency department visits, housing instability, social service use, and criminal justice involvement and use of 0, 1, or 2 or more sectors in the past year. We then estimated multivariable regression models for each outcome and computed predictive margins to obtain adjusted probabilities of service involvement across multiple sectors for each substance use category.(34) For hospital days and emergency department visits, we used negative binomial regression and reported adjusted probabilities of events per 100 person-years. For housing instability, social service use, and criminal justice involvement, we used logistic regression models and presented probabilities as a percentage within each population. Finally, we used a multivariable logistic regression model to estimate associations between sociodemographic and clinical characteristics and involvement in services in 2 or more sectors compared to use of 0–1 sectors in the past year.
All analyses used person-level survey weights provided by NSDUH to generate estimates representative of the non-institutionalized US population. We used Stata’s svy command to account for primary sampling unit and strata variables, in addition to the person-level weights reported in the public use data file. All analyses were performed using Stata/SE version 15.1 (StataCorp, College Station, TX). Two-sided P values <.05 were considered statistically significant a priori. This study was considered exempt by the Yale University Human Investigations Committee.
Results:
Our study sample consisted of 171,766 adult respondents. The annualized proportion who reported opioid use only was 4.0% (95% Confidence Interval (CI):3.9%−4.2%; weighted N: 9,943,000), methamphetamine use only was 0.4% (95% CI:0.3%−0.4%; weighted N: 889,301), and both opioid and methamphetamine use was 0.3% (95% CI:0.2%−0.3%; weighted N: 738,856). Sociodemographic and clinical characteristics across the four substance use categories are reported in Table 1. Compared to people who reported opioid use only, those who reported methamphetamine use only, or both opioid and methamphetamine use were more likely to be American Indian/Alaskan Native, male, live in a rural county, live below 100% federal poverty line, report fair or poor health, and report serious psychological distress.
Table 1.
Sociodemographic and clinical characteristics of study population by reported substance use in the past year, United States, 2015–2018
| No Illicit Opioid or Methamphetamine Use in Past Year (N=161,558) | Illicit Opioid Use in Past Year (N=8,721) | Methamphetamine Use in Past Year (N=762) | Methamphetamine and Illicit Opioid Use in Past Year (N=725) | |
|---|---|---|---|---|
| % of total population | 95.3% (95.2%−95.4%) | 4.0% (3.9%−4.2%) | 0.4% (0.3%−0.4%) | 0.3% (0.2%−0.3%) |
| Female | 52.1% (51.7%−52.5%) | 45.9% (44.4%−47.3%) | 38.4% (33.9%−43.0%) | 34.9% (30.4%−39.7%) |
| Age Range, y | ||||
| 18–25 | 13.6% (13.3%−13.8%) | 23.2% (22.1%−24.3%) | 16.5% (13.7%−19.8%) | 23.5% (20.0%−27.4%) |
| 26–34 | 15.5% (15.2%−15.8%) | 24.8% (23.6%−26.0%) | 24.3% (20.8%−28.1%) | 29.3% (25.2%−33.7%) |
| 35–49 | 24.7% (24.3%−25.0%) | 25.5% (24.4%−26.7%) | 31.8% (28.1%−35.7%) | 30.6% (26.2%−35.3%) |
| 50+ | 46.3% (45.7%−46.8%) | 26.5% (24.8%−28.3%) | 27.5% (23.1%−32.3%) | 16.7% (12.0%−22.8%) |
| Race/Ethnicity | ||||
| White, non-Hispanic | 63.9% (63.3%−64.4%) | 67.0% (65.3%−68.7%) | 68.5% (63.8%−72.9%) | 77.5% (73.0%−81.4%) |
| Black, non-Hispanic | 11.9% (11.5%−12.3%) | 11.4% (10.3%−12.5%) | 5.3% (3.7%−7.5%) | 3.4% (2.2%−5.2%) |
| Hispanic | 16.3% (15.9%−16.7%) | 16.2% (15.1%−17.3%) | 19.4% (15.7%−23.6%) | 13.4% (10.3%−17.1%) |
| American Indian/Alaskan Native | 0.5% (0.5%−0.6%) | 0.7% (0.5%−0.9%) | 2.8% (1.5%−5.3%) | 1.7%(1.1%−2.8%) |
| Other | 7.4% (7.1%−7.6%) | 4.7% (4.1%−5.5%) | 4.0% (2.6%−6.1%) | 4.0% (2.6%−6.3%) |
| Income | ||||
| <100% FPL | 14.0% (13.7%−14.4%) | 19.3% (18.2–20.5%) | 32.8% (28.2%−37.7%) | 34.6% (29.7%−39.8%) |
| >100% & <200% FPL | 19.9% (19.6%−20.2%) | 21.4% (20.0–22.9%) | 24.6% (21.2%−28.3%) | 31.2% (26.7%−36.1%) |
| >200% FPL | 66.1% (65.6%−66.6%) | 59.3% (57.6%−60.9%) | 42.6% (38.2%−47.1%) | 34.2% (29.2%−39.5%) |
| Reside in Rural County | 14.6% (14.2%−15.1%) | 13.4% (12.4%−14.5%) | 19.4% (15.8%−23.7%) | 22.7% (18.4%−27.7%) |
| Self-Reported Fair or Poor Health | 13.6% (13.3%−14.0%) | 18.4% (16.9%−19.9%) | 28.6% (23.8%−33.8%) | 28.0% (23.8%−32.6%) |
| Serious Psychological Distress | 10.0% (9.7%−10.2%) | 30.1% (28.8%−31.5%) | 37.4% (32.9%−41.7%) | 52.4% (46.8%−58.0%) |
Note: Estimates reflect weighted proportions based on survey methodology. Range reflects 95% confidence interval.
Service Involvement in Individual Sectors
In unadjusted analyses, adults who reported any methamphetamine use, with or without opioid use, had significantly more hospital days (P≤.01, P=0.04) and more emergency department visits (P≤.001 for both) than people with opioid use only. In addition, adults with any methamphetamine use, with or without opioid use, were more likely to report housing instability (P≤.001 for both), social service use (P≤.001 for both), and criminal justice involvement (P≤.001 for both) in the past year than people with opioid use only (Figure 1; Table 2). Sociodemographic characteristics of each single sector category are included in the Table, Supplemental Digital Content 1.
Figure 1.
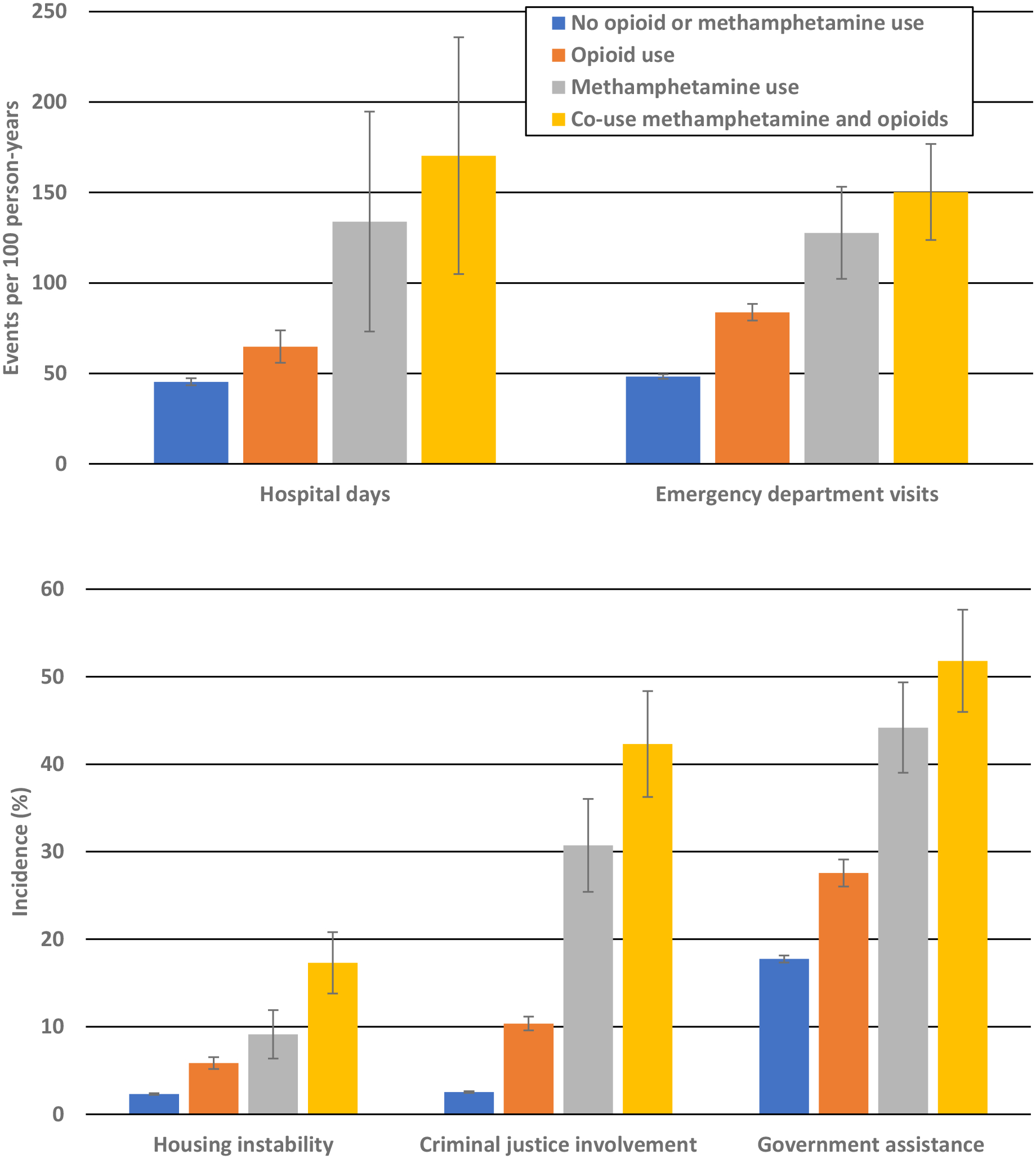
Unadjusted service use among people who reported use of opioids, methamphetamine, or both opioids and methamphetamine compared to people who reported no use, 2015–2018
Notes: Estimates reflect weighted proportions based on survey methodology. Error bars reflect 95% confidence interval.
Table 2.
Unadjusted and adjusted estimates of service use by substance use category, United States 2015–2018
| No illicit opioid or methamphetamine use in past year | Illicit Opioid Use in Past Year | Methamphetamine Use in Past Year | Methamphetamine and Illicit Opioid Use in Past Year | |
|---|---|---|---|---|
| Unadjusted | ||||
| Hospital days per 100 person-years (N, 95% CI) | 45 (43–47) | 65 (56–74)** | 134 (73–195)*,a | 170 (105–236)**,b |
| ED visits per 100 person-years (N, 95% CI) | 48 (47–49) | 84 (79–88)** | 128 (102–153)**,c | 150 (124–177)**,c |
| Housing instability (%, 95% CI) | 2.3% (2.2%−2.4%) | 5.8% (5.2%−6.5%)** | 9.1% (6.3%−11.9%)**,b | 17.3% (13.8%−20.8%)**,c |
| Social service use (%, 95% CI) | 17.7% (17.3%−18.1%) | 27.6% (26.0%−29.1%)** | 44.2% (39.0%−49.3%)**,c | 51.8% (46.0%−57.6%)*,c |
| Past year criminal justice involvement (%, 95% CI) | 2.5% (2.4%−2.6%) | 10.4% (9.6%−11.1%)** | 30.7% (25.4%−36.0%)**,c | 42.3% (36.3%−48.4%)**,c |
| Adjustedα | ||||
| Hospital days per 100 person-years (N, 95% CI) | 47 (45–49) | 70 (59–82)** | 120 (62–177)* | 139 (93–185)**,a |
| ED visits per 100 person-years (N, 95% CI) | 49 (48–50) | 70 (67–74)** | 91 (75–107)**,a | 102 (83–122)**,b |
| Housing instability (%, 95% CI) | 2.4% (2.3%−2.5%) | 3.9% (3.4–4.4%)** | 5.3% (3.7%−6.9%)** | 8.4% (6.5%−10.3%)**,b |
| Social service use (%, 95% CI) | 18.0% (17.6%−18.4%) | 23.4% (22.2%−24.6%)** | 29.4% (25.5%−33.4%)**,b | 33.1% (28.1%−38.0%)**,b |
| Past year criminal justice involvement (%, 95% CI) | 2.6% (2.5%−2.7%) | 7.1% (6.5%−7.6%)** | 19.1% (15.3%−22.8%)**,b | 23.4% (18.9%−27.8%)**,b |
Notes: Estimates reflect weighted proportions based on survey methodology.
- adjusted for age, race/ethnicity, gender, poverty, rurality, serious psychological distress, and self-reported health
P=.01 compared to no past year illicit opioid or methamphetamine use
P≤.001 compared to no past year illicit opioid or methamphetamine use
P=.04 compared to illicit opioid use
P≤.01 compared to illicit opioid use
P≤.001 compared to illicit opioid use
After adjusting for demographic and clinical factors, people with both methamphetamine and opioid use had nearly twice as many hospital days (P≤.01) and 46% more emergency department visits (P≤.001) compared with people with opioid use only (Table 2). In the adjusted analysis the proportion of adults with both opioid and methamphetamine use reported housing instability was 2.2 times higher (P≤.001), social service use was 1.3 times higher(P≤.001), and criminal justice involvement was 3.3 times higher (P≤.001) than people with opioid use only Table 2.
Multi-Sector Service Involvement
In unadjusted analyses, 6.4% of individuals with no opioid/methamphetamine use, 15.9% with opioid use only, 33.9% with methamphetamine use only, and 49.4% with both opioid and methamphetamine use reported involvement in 2 or more sectors in the past year (Figure 2; Table 3). After adjustment, the proportions of people with methamphetamine use only (P≤.001) or both opioid and methamphetamine use (P≤.001) who were involved with services from 2 or more sectors were 71% and 138% higher, respectively, compared with those with opioid use only (Table 3). Individuals reporting service involvement across 2 or more sectors, across all drug use categories, had higher proportions living below 200% the federal poverty level, in fair or poor health, and with serious psychological distress (Table, Supplemental Digital Content 2) compared with overall study population characteristics in Table 1.
Figure 2.
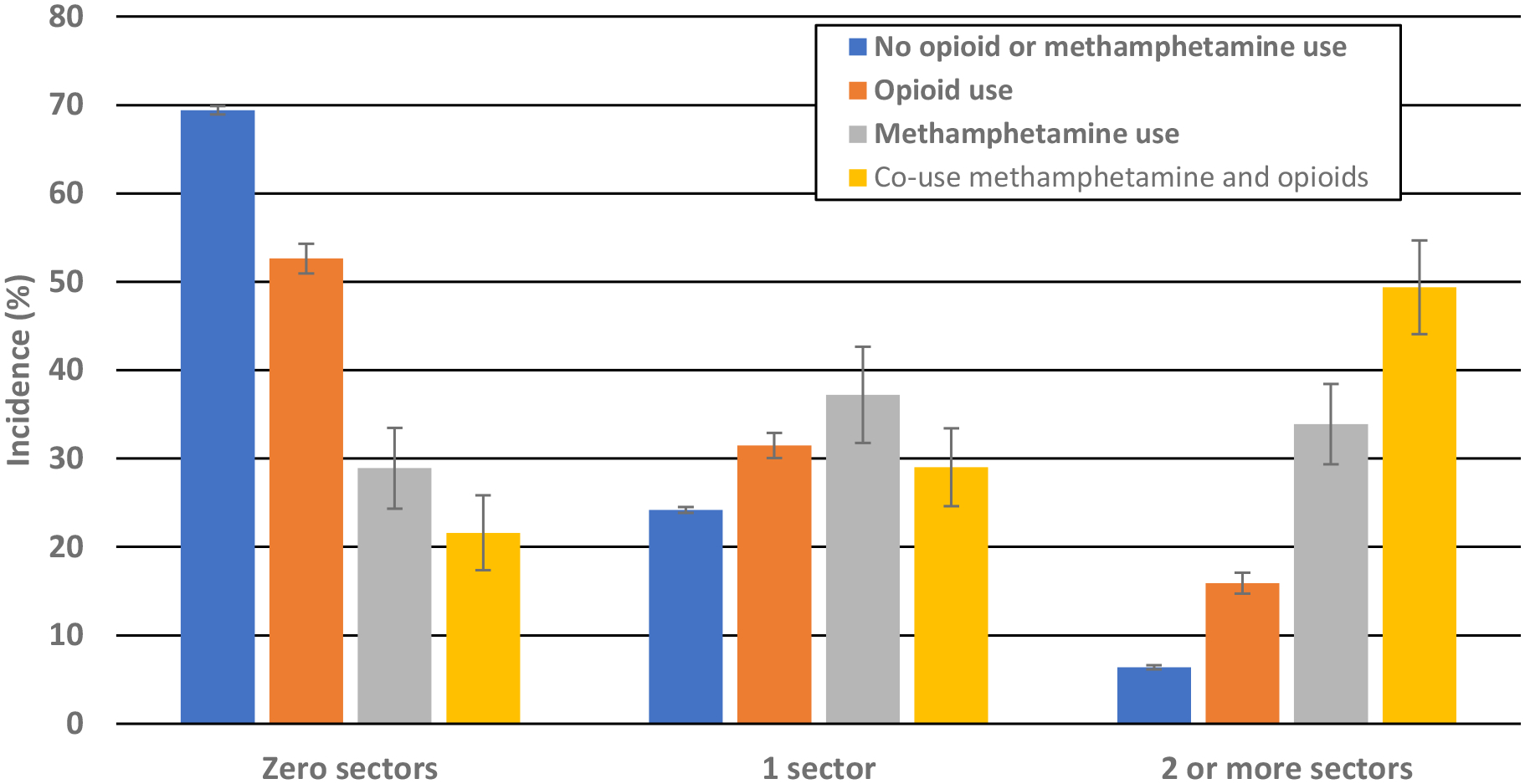
Unadjusted multi-sector service use among people who reported use of opioids, methamphetamine, or both opioids and methamphetamine compared to people who reported no use, 2015–2018
Notes: Estimates reflect weighted proportions based on survey methodology. Error bars reflect 95% confidence interval.
Table 3.
Unadjusted and adjusted estimates of multi-sector service use by substance use category, United States 2015–2018
| No illicit Opioid or Methamphetamine use in past year | Illicit Opioid Use in Past Year | Methamphetamine Use in Past Year | Methamphetamine and Illicit Opioid Use in Past Year | |
|---|---|---|---|---|
| Unadjusted (95% CI) | ||||
| 0 sectors | 69.4% (69.0%−69.8%) | 52.6% (50.9%−54.3%)** | 28.9% (24.4%−33.5%)**,b | 21.6% (17.4%−25.8%)**,b |
| 1 sector | 24.2% (23.9%−24.5%) | 31.5% (30.0%−32.9%)** | 37.2%(31.7%−42.6%)**,a | 29.0% (24.6%−33.4%)* |
| 2 or more sectors | 6.4% (6.2%−6.6%) | 15.9% (14.7%−17.1%)** | 33.9% (29.4%−38.4%)**,b | 49.4% (44.1%−54.7%)**,b |
| Adjusted (95% CI)α | ||||
| 0 sectors | 69.0% (68.6%−69.5%) | 58.4% (56.9%−59.9%)** | 41.3% (56.9%−59.9%)**,b | 36.0% (31.1%−40.8%)**,b |
| 1 sector | 24.4% (24.0%−24.7%) | 28.7% (27.4%−30.0%)** | 29.7% (24.4%−35.1%) | 21.2% (17.5%−24.8%)b |
| 2 or more sectors | 6.6% (6.3%−6.8%) | 11.6% (10.7%−12.6%)** | 19.8% (17.3%−22.3%)**,b | 27.6% (23.5%−31.7%)**,b |
Notes: Estimates reflect weighted proportions based on survey methodology.
- adjusted for age, race/ethnicity, gender, poverty, rurality, serious psychological distress, and self-reported health
P=.03 compared to no past year illicit opioid or methamphetamine use
P≤.001 compared to no past year illicit opioid or methamphetamine use
P=.04 compared to illicit opioid use
P≤.001 compared to illicit opioid use
People who reported involvement in 2 or more sectors were significantly more likely to live below 200% (adjusted odds ratio (aOR) 4.34, 95% CI 3.92–4.57) or 100% of the federal poverty level (aOR 9.58, 95% CI: 8.89–10.31) compared to those who lived at >200% the federal poverty level (Table, Supplemental Digital Content 3). They were also more likely to report serious psychological distress (aOR 2.03, 95% CI 1.90–2.17) or have self-reported fair or poor health (aOR 2.77, 95% CI: 2.58–2.97).
Discussion:
In this national sample of US adults, we found that people who reported co-use of opioids and methamphetamine or use of methamphetamine only in the past year were significantly more likely to report higher levels of involvement in health care, housing, and social service sectors and more involvement with the criminal justice system compared with people who reported opioid use only or no opioid/methamphetamine use in the past year. In an era of rising methamphetamine use, with and without opioids, aggregated societal costs related to methamphetamine use are likely to be large.(35) A coordinated response across sectors is needed to decrease the burden of methamphetamine use and co-use on individuals, families, and communities and especially address heatlh-related harms.
Our results add to the existing literature of characteristics among people who frequently use acute health care services. While substance use in general is associated with high use of acute health care,(23, 36, 37) the literature on health care use associated with methamphetamine use is limited. Our results demonstrate that people who use methamphetamine have higher rates of acute health care use than people who use opioids. Although our data cannot identify the causes of hospitalization, possible causes are cardiovascular toxicity(9, 13, 21) or psychiatric symptoms, such as acute psychosis and mood disorders,(13, 38) associated with methamphetamine use. Finally, people who use methamphetamine may preferentially access health care in acute settings, as beliefs and attitudes among health professionals about people who use methamphetamine can create barriers to non-acute health care for this population.(39)
In line with other work on cross-sector service analysis, our results reinforce that people who frequently use health care services also frequently are involved in services in other sectors.(23) Along with high acute health care use, we found higher rates of housing instability and social service use. The associations between involvement, substance use, and our covariates are complex, and the directionality of relationships cannot be elucidated in this cross-sectional study. Qualitative work has found that people experiencing homelessness report methamphetamine use to increase safety in tenuous living conditions,(27, 40) whereas methamphetamine use itself may also lead to financial instability and subsequent homelessness. We also found that poverty, self-reported fair or poor health, and serious psychological distress were independently associated with increased cross-sector involvement. Further research should focus on elucidating the causal mechanisms of cross-sector use.
Our findings build on reports of increased jail and prison admissions related to methamphetamine,(41) and single-site studies that have reported high rates of housing instability among people who use methamphetamine.(42, 43) The high prevalence of housing instability and criminal justice involvement likely reinforces the cycle of high acute care use.(26, 44, 45) Thus, reducing methamphetamine use only, without attention to other social determinants, may not reduce acute care use once someone has entered a cycle of homelessness and incarceration.
Collaborations that account for the cross-sector usage patterns may be a more effective approach than siloed sector specific interventions. Of note, cross-sector interventions are already being piloted to address morbidity and mortality associated with opioid use disorder.(46) Our work highlights that similar cross-sector work may also have a role in addressing the fourth wave of the opioid crisis; although the limited number of evidence-based interventions for methamphetamine use may limit their efficacy.(3)
Limitations
Our results should be interpreted in the context of some limitations. All outcomes were measured by self-report and cannot be verified through claims or administrative data, though self-reported data on criminal justice involvement has been shown to be a valid measure in previous studies.(47) Our measure of housing instability was chosen as a proxy for housing service use and should be interpreted with this limitation in mind. Also, while there are some concerns that substance use reported in the NSDUH may be somewhat underreported, this would bias our results towards the null.(48) The NSDUH does not include data on the indication for hospitalization or emergency department visits, and therefore, we are unable to determine if those visits were associated with methamphetamine use. Finally, by design, the NSDUH does not survey adults who are institutionalized or unhoused. Given the likely higher prevalence of methamphetamine use among people who are homeless or incarcerated, these data are likely a conservative estimate of overall methamphetamine use in the past year.
Conclusion
Hospital days, emergency department visits, housing instability, social service use, and criminal justice involvement were significantly higher among US adults who reported past year use of both opioids and methamphetamine or use of methamphetamine only compared with people who reported opioid use only or neither opioid nor methamphetamine use. Cross-sector involvement was highest among individuals with both opioid and methamphetamine use, which suggests that the fourth wave of the opioid crisis may result in greater societal costs than earlier waves of the crisis. Cross-sector collaborations and investments in methamphetamine use prevention and treatment research are needed to improve public health and blunt the increasing complexity of the opioid crisis.
Supplementary Material
Supplemental Digital Content Table 1. Sociodemographic and clinical characteristics of individuals who utilized individual sectors, United States, 2015–2018
Supplemental Digital Content 2. Sociodemographic and clinical characteristics of individuals who utilized two or more service sectors, United States, 2015–2018
Supplemental Digital Content 3. Odds of individuals using services from 2 or more sectors compared to using services from less than 2 sectors by sociodemographic, clinical, and drug use characteristics, United States, 2015–2018
Funding:
Dr. Howell receives funding from by the Department of Veterans Affairs Office of Academic Affiliations through the National Clinician Scholars Program and grant number 5K12DA033312 from the National Institute on Drug Abuse. Dr. Wang receives research support through Yale University from the Bureau of Justice Administration to study reentry by linking correctional and community health system data (2015-RY-BX-K002) and the Substance Abuse and Mental Health Services Administration to study how to improve the health of women just released from corrections. Dr. Wang currently receives research support through Yale University from the National Cancer Institute of National Institute of Health (1R01CA230444), the National Heart, Lung, and Blood Institute (1R01HL137696), the National Institute of Minority Health and Disparities (1R01MD010403), and the National Institute of Drug Abuse (1UG1DA050072) to study incarceration and cancer, cardiovascular disease, gun violence, and opioid use disorder. She also receives funding from the William T. Grant Foundation to study health related barriers and facilitators to reducing criminal legal contact and from the California Health Care Foundation to evaluate the Transitions Clinic Network in California.
Footnotes
Conflict of interest statement: The authors have no conflict of interest to disclose.
Service involvement across multiple sectors among people who use opioids, methamphetamine, or both, United States - 2015–2018
References:
- 1.Kariisa M, Scholl L, Wilson N, et al. Drug Overdose Deaths Involving Cocaine and Psychostimulants with Abuse Potential—United States, 2003–2017. MMWR Morb Mortal Wkly Rep 2019;68:388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gladden RM, O’Donnell J, Mattson CL, et al. Changes in opioid-involved overdose deaths by opioid type and presence of benzodiazepines, cocaine, and methamphetamine—25 states, July–December 2017 to January–June 2018. MMWR Morb Mortal Wkly Rep 2019;68:737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hainer R Polysubstance Use and Stimulants: A Dangerous Fourth Wave in the Opioid Crisis. 2019. Available at: https://www.bmc.org/healthcity/population-health/polysubstance-use-dangerous-fourth-wave-opioid-crisis. Accessed October, 24, 2019,
- 4.Ellis MS, Kasper ZA, Cicero TJ. Twin epidemics: The surging rise of methamphetamine use in chronic opioid users. Drug Alcohol Depend 2018;193:14–20 [DOI] [PubMed] [Google Scholar]
- 5.Jones CM, Underwood N, Compton W. Increases in Methamphetamine Use among Heroin Treatment Admissions in the United States, 2008–2017. Addiction 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Tayyib A, Koester S, Langegger S, et al. Heroin and Methamphetamine Injection: An Emerging Drug Use Pattern. Subst Use Misuse 2017;52:1051–1058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Winkelman TN, Admon LK, Jennings L, et al. Evaluation of amphetamine-related hospitalizations and associated clinical outcomes and costs in the United States. JAMA Netw Open 2018;1:e183758–e183758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marshall BD, Werb D. Health outcomes associated with methamphetamine use among young people: a systematic review. Addiction 2010;105:991–1002 [DOI] [PubMed] [Google Scholar]
- 9.Herbeck DM, Brecht M-L, Lovinger K. Mortality, causes of death, and health status among methamphetamine users. J Addict Dis 2015;34:88–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shearer RD, Howell BA, Bart G, et al. Substance use patterns and health profiles among US adults who use opioids, methamphetamine, or both, 2015–2018. Drug Alcohol Depend;214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mansergh G, Purcell DW, Stall R, et al. CDC consultation on methamphetamine use and sexual risk behavior for HIV/STD infection: summary and suggestions. Public health reports 2006;121:127–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lorvick J, Browne EN, Lambdin BH, et al. Polydrug use patterns, risk behavior and unmet healthcare need in a community-based sample of women who use cocaine, heroin or methamphetamine. Addict Behav 2018;85:94–99 [DOI] [PubMed] [Google Scholar]
- 13.Darke S, Kaye S, McKetin R, et al. Major physical and psychological harms of methamphetamine use. Drug Alcohol Rev 2008;27:253–262 [DOI] [PubMed] [Google Scholar]
- 14.Admon LK, Bart G, Kozhimannil KB, et al. Amphetamine-and Opioid-Affected Births: Incidence, Outcomes, and Costs, United States, 2004–2015. Am J Public Health 2019;109:148–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meredith CW, Jaffe C, Ang-Lee K, et al. Implications of chronic methamphetamine use: a literature review. Harv Rev Psychiatry 2005;13:141–154 [DOI] [PubMed] [Google Scholar]
- 16.Larochelle MR, Bernstein R, Bernson D, et al. Touchpoints - Opportunities to predict and prevent opioid overdose: A cohort study. Drug Alcohol Depend 2019;204:107537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wakeman SE, Metlay JP, Chang Y, et al. Inpatient Addiction Consultation for Hospitalized Patients Increases Post-Discharge Abstinence and Reduces Addiction Severity. J Gen Intern Med 2017;32:909–916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.D’Onofrio G, O’Connor PG, Pantalon MV, et al. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. JAMA 2015;313:1636–1644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martin RA, Gresko SA, Brinkley-Rubinstein L, et al. Post-release treatment uptake among participants of the Rhode Island Department of Corrections comprehensive medication assisted treatment program. Prev Med 2019:105766. [DOI] [PubMed] [Google Scholar]
- 20.Meinhofer A, Anglero-Diaz Y. Trends in Foster Care Entry Among Children Removed From Their Homes Because of Parental Drug Use, 2000 to 2017. JAMA Pediatr 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh M, Doddamreddy P, Dhaliwal-Binning K, et al. Methamphetamine Abuse & Its Health Care Impact in the Central Valley of California. Am J Respir Crit Care Med 2017;195 [Google Scholar]
- 22.Morasco BJ, O’Neil ME, Duckart JP, et al. Comparison of health service use among veterans with methamphetamine versus alcohol use disorders. J Addict Med 2014;8:47–52 [DOI] [PubMed] [Google Scholar]
- 23.Vickery KD, Bodurtha P, Winkelman TN, et al. Cross-sector service use among high health care utilizers in Minnesota after Medicaid expansion. Health Aff (Millwood) 2018;37:62–69 [DOI] [PubMed] [Google Scholar]
- 24.2017 National Survey on Drug Use and Health: Methodological Resource Book. Rockville, MD: Substance Abuse and Mental Health Administration, Center for Behavorial Health Statistics and Quality; 2018 [Google Scholar]
- 25.Bodurtha P, Van Siclen R, Erickson E, et al. Cross-Sector Service Use and Costs Among Medicaid Expansion Enrollees in Minnesota’s Hennepin County. Center for Health Care Strategies; 2017 [Google Scholar]
- 26.Kushel MB, Gupta R, Gee L, et al. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med 2006;21:71–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kushel MB, Hahn JA, Evans JL, et al. Revolving doors: imprisonment among the homeless and marginally housed population. Am J Public Health 2005;95:1747–1752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cutts DB, Meyers AF, Black MM, et al. US housing insecurity and the health of very young children. Am J Public Health 2011;101:1508–1514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cox RH, Benjamin; Rodnyanksy Seva; Wenzel Suzanne; Rice Eric. Roadmap to a unified measure of housing security Working paper series. Washington, DC: Washington Center for Equitable Growth; 2017 [Google Scholar]
- 30.Bodurtha PJ, Winkelman T, Vickery KD, et al. Identification of Cross-sector Service Utilization Patterns Among Urban Medicaid Expansion Enrollees. Med Care 2019;57:123–130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giannouchos TV, Washburn DJ, Kum HC, et al. Predictors of Multiple Emergency Department Utilization Among Frequent Emergency Department Users in 3 States. Med Care 2020;58:137–145 [DOI] [PubMed] [Google Scholar]
- 32.USDA ERS. Rural-Urban Continuum Codes. 2013. Available at: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/
- 33.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry 2003;60:184–189 [DOI] [PubMed] [Google Scholar]
- 34.Norton EC, Dowd BE, Maciejewski ML. Marginal Effects—Quantifying the Effect of Changes in Risk Factors in Logistic Regression Models. JAMA 2019;321:1304–1305 [DOI] [PubMed] [Google Scholar]
- 35.Nicosia N, Pacula RL, Kilmer B, et al. The economic cost of methamphetamine use in the United States, 2005. RAND HEALTH SANTA MONICA CA; 2009 [Google Scholar]
- 36.Doupe MB, Palatnick W, Day S, et al. Frequent users of emergency departments: developing standard definitions and defining prominent risk factors. Ann Emerg Med 2012;60:24–32 [DOI] [PubMed] [Google Scholar]
- 37.Rinehart DJ, Oronce C, Durfee MJ, et al. Identifying subgroups of adult super-utilizers in an urban safety-net system using latent class analysis: Implications for clinical practice. Med Care 2018;56:e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marshall B, Grafstein E, Buxton J, et al. Frequent methamphetamine injection predicts emergency department utilization among street-involved youth. Public Health 2012;126:47–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van Boekel LC, Brouwers EP, Van Weeghel J, et al. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend 2013;131:23–35 [DOI] [PubMed] [Google Scholar]
- 40.Bungay V, Malchy L, Buxton JA, et al. Life with jib: A snapshot of street youth’s use of crystal methamphetamine. Addiction Research & Theory 2006;14:235–251 [Google Scholar]
- 41.Mannix A Even as meth offenders fuel a boom in Minnesota’s prison population, treatment resources remain scarce. 2015. Available at: https://www.minnpost.com/politics-policy/2015/11/even-meth-offenders-fuel-boom-minnesotas-prison-population-treatment-resourc/. Accessed December 27, 2019,
- 42.McKenna SA. Navigating the risk environment: Structural vulnerability, sex, and reciprocity among women who use methamphetamine. Int J Drug Policy 2014;25:112–115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nyamathi A, Dixon EL, Shoptaw S, et al. Profile of lifetime methamphetamine use among homeless adults in Los Angeles. Drug and alcohol dependence 2008;92:277–281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Frank JW, Linder JA, Becker WC, et al. Increased hospital and emergency department utilization by individuals with recent criminal justice involvement: results of a national survey. J Gen Intern Med 2014;29:1226–1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Greenberg GA, Rosenheck RA. Homelessness in the state and federal prison population. Crim Behav Ment Health 2008;18:88–103 [DOI] [PubMed] [Google Scholar]
- 46.HEALing Communities Study. 2019. Available at: https://www.nih.gov/research-training/medical-research-initiatives/heal-initiative/healing-communities-study. Accessed September 24, 2019, 2019
- 47.Wang EA, Macmadu A, Rich JD. Examining the impact of criminal justice involvement on health through federally funded, national population-based surveys in the United States. Public Health Rep 2019;134:22S–33S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Midgette G, Davenport S, Caulkins JP, et al. What America’s Users Spend on Illegal Drugs, 2006–2016. Santa Monica, CA: RAND; 2019 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content Table 1. Sociodemographic and clinical characteristics of individuals who utilized individual sectors, United States, 2015–2018
Supplemental Digital Content 2. Sociodemographic and clinical characteristics of individuals who utilized two or more service sectors, United States, 2015–2018
Supplemental Digital Content 3. Odds of individuals using services from 2 or more sectors compared to using services from less than 2 sectors by sociodemographic, clinical, and drug use characteristics, United States, 2015–2018


