Abstract
Purpose
Posterior fracture-dislocation of shoulder is an infrequent traumatic event; however, most orthopaedic surgeons may face the challenge of treating it. The aim of this study is to review and summarise systematically the current principles of the management of this complex injury, and create a treatment algorithm.
Methods
Both PubMed and Scopus Databases were systematically searched for the terms “posterior shoulder fracture-dislocation” or “posterior glenohumeral fracture-dislocation” or “posterior glenoid fracture-dislocation” for articles written in English and published in the last decade.
Results
A total of 900 articles were identified, of which 13 were retained for analysis. A total of 153 patients (161 shoulders) were identified. These patients were treated either with open reduction and internal fixation, modified McLaughlin procedure, allograft/autograft humeral head reconstruction or shoulder arthroplasty. The mean age was 40.15 years. The mean postoperative Constant score in cases treated by open reduction and internal fixation was 86.45, whereas by bone graft was 84.18. Further, the mean postoperative Constant score was between 79.6 and 67.1 in those that were managed by modified McLaughlin and arthroplasty procedure, respectively.
Conclusion
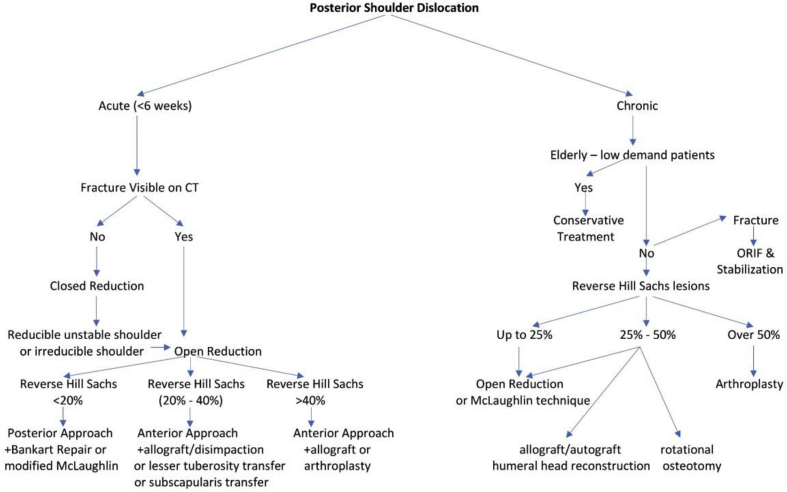
The management of posterior shoulder fracture-dislocation may be challenging, and the best surgical option depends on many variables such as the chronicity of the injury, the presence of a fracture at the level of the surgical neck or tuberosities and the extend of the Hill-Sachs lesion if any. A treatment algorithm is proposed, based on the current literature in an effort to create a consensus for these injuries. For the acute shoulder fracture-dislocations, an open reduction should be performed. For the chronic fracture/dislocations in the elderly low-demand patients, conservative treatment should be performed. For the rest of the patients, depending on the severity of the Hill-Sachs lesion different surgical options are available such as the McLaughlin technique, the use of an allograft, osteotomy or arthroplasty.
Keywords: Treatment algorithm, Shoulder injury, Posterior dislocation, Fracture-dislocation, Shoulder dislocation
Introduction
Traumatic posterior shoulder dislocation was firstly described in 1838 by Sir Astley Cooper, as a challenging and unusual clinical problem.1 This injury accounts for 2%–5% of all traumatic shoulder dislocations.1, 2, 3 Anterior shoulder dislocations are 15.5–21.7 times more common than posterior ones. However, posterior fracture-dislocation is even less frequent, and according to Neer and Foster,4 it represents 0.9% of 1500 shoulder fracture-dislocations, with the annual prevalence being 0.6/100,000.5 Seizures, high-energy trauma, and electrocution are some of the most common causes of this injury.1,2,6 Appropriate physical and radiologic examination should be performed to confirm the diagnosis, which is missed or delayed in up to 79% of the cases.2,3,7 Specifically, the posterior dislocation has been found to occur after trauma in 67% of cases, after seizure in 31% and after electrocution in 2%.8 Robinson et al.8 suggested that anteroposterior (AP) combined with Velpeau radiographic views in the emergency department resulted in diagnoses in 102 of 112 patients with posterior shoulder dislocation.
The shoulder offers a remarkable range of motion (ROM) such as adduction, abduction, flexion, extension, internal rotation, external rotation, and 360° circumduction in the sagittal level.9 Furthermore, the shoulder contributes to scapular continuation, retraction, elevation, and depression. This extensive ROM also makes the shoulder joint unstable. This instability is counteracted by rotator cuff muscles, tendons, ligaments, and the glenoid labrum.10 Therefore, it is relatively easy to disarticulate. There are three main types of dislocation, characterized by the direction of the humeral head movement: anterior, posterior and inferior.
The aim of the present systematic review is to summarize the current principles of management for posterior shoulder fracture-dislocation and create an algorithm for the management of this challenging condition.
Methods
A systematic review was performed to identify all published articles describing clinical outcomes of posterior shoulder fracture-dislocation using different techniques. A comprehensive literature search was performed via an electronic-based search within the online Medline/PubMed Database (US National Library of Medicine, National Institutes of Health) and the online Scopus Database. Both databases were searched using the terms “posterior shoulder fracture-dislocation” or “posterior glenohumeral fracture-dislocation” or “posterior glenoid fracture-dislocation”.
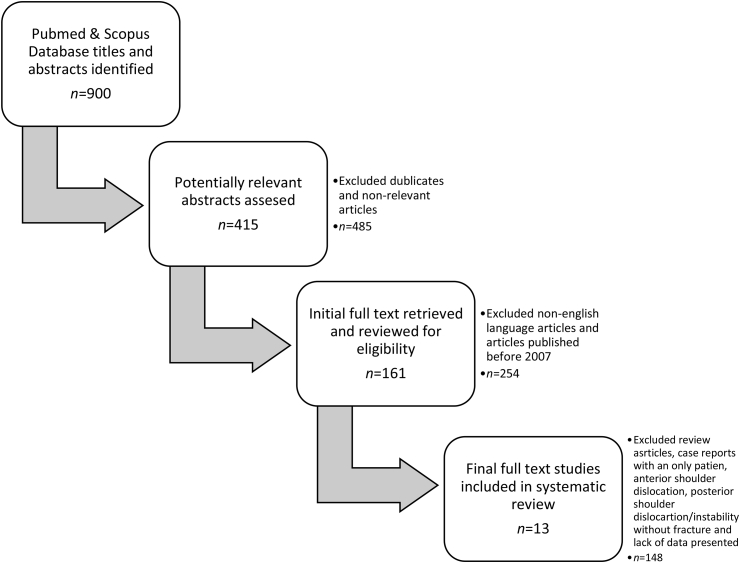
Study selection for inclusion in the systematic review was determined by examining the title and abstract of all articles obtained from the database search. Firstly, duplicates and non-relevant articles were excluded; non-English language articles and published articles over 10 years (between January 2007 and December 2016) were also excluded. The first and the senior author (Polyzois I) analyzed each included study for data extraction. This was performed according to the PRISMA flowchart and it is included below in Fig. 1.
Fig. 1.
PRISMA flow chart.
Results
A total of 900 references were evaluated (Fig. 1) to yield 13 eligible articles. Review articles and case reports with only one patient were excluded. Furthermore, articles referring to patients, who sustained anterior shoulder dislocation, posterior shoulder dislocation and shoulder instability without fracture were excluded. Studies containing no specific clinical and functional outcome scores did not match the inclusion criteria and were also excluded. Finally, all the remaining references (13 articles) were cross-checked to find any missing relevant articles. The included articles were all obtained and evaluated by two different authors. Table 1 lists the demographic and baseline characteristics as well as follow-up details of component studies. All data reflect the potential presence of clinical diversity across included studies.
Table 1.
Demographic details, treatment details, follow-up characteristics, and functional outcome scores.
| Study | Number of patients (shoulders) | Mean age (year) | Type of surgery | Mean follow-up (month) | Mean Constant scorea |
|---|---|---|---|---|---|
| Robinson et al.5 (2007) | 22 (24) | 53 | Open reduction with internal fixation | 83.5 | 24 |
| Castagna et al.30 (2009) | 16 | 41.9 | Modified McLaughlin procedure | 75.2 | 62.8 |
| Kokkalis et al.31 (2013) | 5 (6) | 53.2 | Modification of the McLaughlin technique | 84 | 20 |
| Aksekili et al.32 (2016) | 7 (10) | 42.4 | Iliac autograft with glenoid augmentation | 40.6 | 81.25 |
| Diklic et al.33 (2010) | 13 | 42 | Allograft reconstruction | 86.2 | 54 |
| Martinez et al.34 (2013) | 6 | 31.7 | Allograft reconstruction | 69.2 | 122 |
| Struck et al.35 (2016) | 13 (15) | 20 | Open posterior bone block procedure | 82 | 53.5 |
| Barbier et al.36 (2009) | 8 | 28.7 | Iliac bone-block autograft | 96.3 | 34.3 |
| Servien et al.37 (2007) | 20 (21) | 24.8 | Iliac crest graft | 93.3 | 72 |
| Bock et al.38 (2007) | 6 | 52.5 | Autograft, allograft and the combination of allograft/autograft | 88.2 | 62.7 |
| Gerber et al.39 (2014) | 21 (19) | 44 | Reconstruction with segmental femoral head allograft | 77 | 128 |
| Fiorentino et al.40 (2016) | 5 | 47 | Open reduction with internal fixation | 24 | 89.4 |
| Gavriilidis et al.41 (2010) | 11 (12) | 49.8 | 9 uncemented hemiarthroplasties/1 cemented hemiarthroplasty/2 total cemented shoulder arthroplasty | 67.1 | 37.4 |
Constant score is a widely used shoulder functional scale composed by the level of pain and the ability to carry out the normal daily activities of the patient. It ranges from 0 to 100, with higher scores showing better function.
A range of different treatment options for posterior shoulder fracture-dislocation were used by authors of primary studies. All options were categorized, grouped and involved in the treatment algorithm below. These options were open reduction with internal fixation (ORIF), modified McLaughlin, allograft/autograft humeral head reconstruction and shoulder arthroplasty.
The mean age was 40.15 years. The mean postoperative Constant score in cases treated by ORIF was 86.45, whereas by bone graft was 84.18. Further, the mean postoperative Constant score was between 79.6 and 67.1 in those that were managed by modified McLaughlin and arthroplasty procedure, respectively.
Discussion
Posterior dislocations of the shoulder are less common than the anterior ones accounting for approximately 2%–5% of all shoulder dislocations.1, 2, 3 The most recent review performed by Robinson and Aderinto11 indicates that this number is close to 3%. Recognition of this injury is often challenging with 60%–79% of posterior shoulder dislocations being missed on initial examination.1,3,7 According to Robinson et al.,8 the incidence of posterior dislocation is 1.1 per 100,000 population per year, with spikes in male patients between 20 and 49 years old, and in the elderly over 70 years old. Isolated dislocations of the proximal humerus are a rare phenomenon.12 Historically, bony and soft tissue injuries were identified in 49% of the cases.13 However, Rouleau and Hebert-Davies.12 reported that up to 65% of the posterior shoulder dislocations are associated with bony or soft tissue injuries.
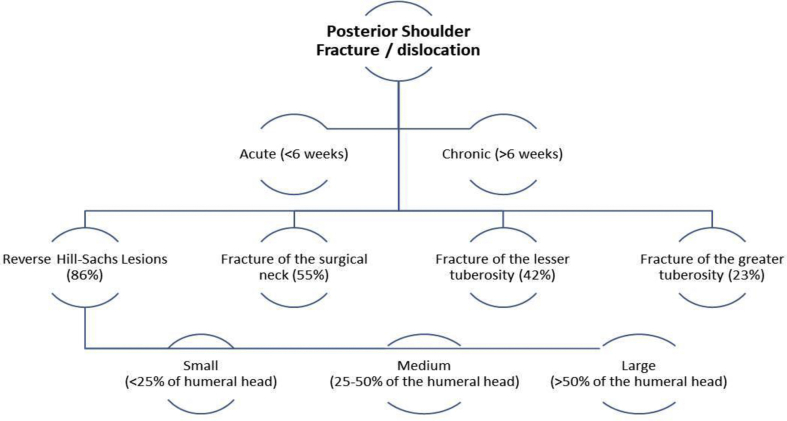
According to Robinson et al.,5 the incidence of complex posterior fracture-dislocation has been estimated at 0.6 per 100,000 population per year, while Neer and Foster4 noted that this complex injury accounts for 0.9% of all fractures and dislocations of the shoulder. Other authors have stated that posterior fracture-dislocations involving the surgical neck may account up to 50% of all posterior glenohumeral dislocations. Most of these may include fracture of the tuberosities or the anatomic neck, alone or in combination. Simple or multiple fractures were present in 34% of shoulders, with the most common fracture site being the surgical neck (55%), followed by the lesser (42%) and greater (23%) tuberosities.12 Open fractures are caused by high energy trauma in a motor – vehicle accident and associated with a brachial plexopathy.14
Reverse Hill Sachs lesions are reported in 86% of low-demand patients, whilst rotator cuff tears may occur in 13% of patients, according to MRI findings.12
Nerve injuries are unusual and may occur concomitantly with a profound injury to the capsulolabral complex rotator cuff, long head of the biceps tendon.15 Nerve palsy may occur in less than 1% of patients with posterior fracture-dislocation and the most commonly injured nerve is the axillary, but the suprascapular can be also affected.12 Fig. 2 summarizes the possible combinations of the posterior shoulder fracture/dislocation.
Fig. 2.
Posterior shoulder fracture/dislocation.
Risk factors & mechanism of injury
Glenoid retroversion as well as hypoplasia and ligamentous laxity have been implicated as risk factors. Moreover, the flexed, adducted, and internally rotated arm has been shown to be the position at high-risk.2,5 Most dislocations are produced by a traumatic incident, with the most of the remainder produced by seizures.8,12 Most of the dislocations have associated injuries. Fracture is the most common followed by reverse Hill-Sachs and cuff tears.8,12 Strength imbalance of the rotator cuff muscles can lead to these dislocations as well.16
According to Roberts and Wickstrom,17 traumatic shoulder posterior dislocation may happen after an axial force applied to the upper limb in the conquerable position of internal rotation, adduction, and forward elevation. As a result of the structure of the intense internal rotators of the shoulder that surmounts the motionless and the dynamic posterior stabilizers, seizure activity might also cause this injury. Metabolic abnormalities such as hypoglycemia and hypocalcemia could be possible risk factors. Moreover, intense muscle contraction secondary to electric shock or electroconvulsive shock therapy may cause posterior glenohumeral dislocation.
Clinical presentation
Patients typically hold their arm in a flexed, adducted, and internally rotated position. They demonstrate also marked limitations with respect to passive external rotation and abduction.7 On patient inspection, posterior shoulder protrusion and leveling of the anterior deltoid with a prominent coracoid process can be observed. Moreover, a skin dimple, which represents a tether of the posteromedial deltoid, may be found inferior and medial to the posterolateral edge of the acromion.3 The patients present with limited external rotation as well, while the locked shoulder in an internally rotated position is quite common in undiagnosed posterior dislocations. The latter may not be recognized, specifically in an elderly patient and in the insensitive trauma patient. However, early diagnosis and treatment can help avoid sequelae such as chronic posterior dislocation, degenerative disease of the shoulder and avascular necrosis of the humeral head.18
Physical examination may reveal a springy or a soft endpoint or a block to external rotation,1, 2, 3,13,19 as well as the subtle sign of diminished supination of the forearm.7
Radiographic evaluation
Insufficient radiographic assessment is possibly the greatest pitfall of the prompt diagnosis of the posterior shoulder dislocation. The recommended views are the AP in the scapular plane, the scapular lateral and the axillary view.20 Even though the AP view is not reliable, it may reveal a light bulb sign.15
Hawkins et al.13 has clearly expressed that the axillary view alone is adequate to confirm the diagnosis of posterior dislocation. If the patient cannot abduct his/her arm for the axillary view, a Velpeau view can be implemented instead.21
CT scan is another option for the diagnosis of the dislocation. The extent and location of bone loss can be analyzed in the chronic dislocations (2–3 weeks) using CT scan.22
MRI is particularly useful in the assessment of a suspected correlated rotator cuff tear. Another indication for MRI scan is the Kim lesion, a concealed avulsion of the postero-inferior labrum.23
Classification systems
There are several classification systems to describe the posterior shoulder dislocations. The classification of May et al.24 was based on the possible cause of this injury, such as habitual, traumatic, obstetric or recurrent subluxation. Detenbeck.25 reported a system, which was based on the chronicity as a factor to consider in the natural history and management. He distinguished acute, chronic, and persistent posterior instability and supplementary partitioned recurrent instability into traumatic and atraumatic variants. Hawkins and Belle26 expanded this classification system further. They distinguished acute posterior dislocations associated with an impression defect or not. Moreover, they categorized persistent subluxation as a form of chronic dislocation and classified this modification from a locked, or missed, chronic dislocation related to an impression defect. Furthermore, they distinguished between voluntary and involuntary recurrent subluxation.
Heller et al.27 described an anatomic system that classified subacromial, subglenoid, and subspinous posterior dislocation. They proposed another system that was based on the fundamental cause. They did include all clinically relevant parameters in their classification: traumatic versus atraumatic, acute versus persistent, recurrent (post-traumatic versus atraumatic), and voluntary (post-traumatic versus atraumatic). This system was grounded on a review of 300 publications of 750 cases. However, another classification method separated these injuries according to the period of time after the dislocation (acute < 6 weeks or chronic > 6 months), while splitting up the pure dislocations from the fracture-dislocation (i.e. reverse Hill-Sachs).11
Robinson and Aderinto11 defined posterior dislocation of the shoulder as small (<25%), medium (25%–50%) and large (>50%) using the humeral head defect and further classified this disease entity into simple type and complex type. Considering the complex dislocation, it consists of two-part of the lesser tuberosity, three-part of the anatomic neck and three-part and four-part fractures of the proximal humerus.4,5,11
Non-surgical treatment
Acute posterior instability with a reverse Hill-Sachs lesion of <20% and no associated fractures may be stable after the closed reduction.15 According to Robinson et al.,8 33% of the dislocations among 112 patients were successfully reduced using in-line gentle manipulation (level of evidence (LoE): IV). Moreover, the subsequent treatment method that Robinson and his colleagues8 used was the immobilization in a sling for four weeks with the shoulder in a so-called gunslinger brace in neutral rotation, abduction, and flexion. After the removal of the brace at four weeks, patients were consulted to receive a rehabilitation program under the supervision of a physiotherapist. At this stage, patients started to do active-assisted shoulder ROM exercises and were allowed unrestricted range of movement. Isometric rotator cuff strengthening exercises were commenced at four weeks, progressing to isotonic exercises at eight weeks. Patients were advised to continue strengthening exercises within the first year after the injury, while the physically active patients could return to general fitness training, including running, and noncontact sports at twelve weeks, but were advised to avoid competitive collision sports until sixteen weeks after the injury.
Surgical treatment
Following unsuccessful closed reduction, an open reduction can be conducted through either a deltopectoral, deltoid split lateral or a posterior approach. The approach is determined based on preoperative planning. Isolated closed reduction can be successful in acute dislocations with reverse Hill-Sachs lesions measuring <20%.15
Hill-Sachs lesion
The patients with severe Hill-Sachs lesions (<20%) may be operated using McLaughlin procedure, while the modified McLaughlin procedure is more appropriate for individuals with Hill-Sachs lesions 20%–40%.15 Castagna et al.28 used the modified McLaughlin procedure as the treatment method for 16 patients with a neglected posterior shoulder dislocation. The average follow-up was 62.8 months where no intraoperative or postoperative complications occurred, while a statistically significant improvement of functional outcomes scores (Constant score and ROM) was observed (LoE: IV). This surgical technique was presented in another case series of 5 patients (6 shoulders) with neglected locked posterior dislocation of the shoulder (LoE: IV). Mean follow-up was 20 months after the surgery and at last follow-up, all patients reported no symptoms, whilst all shoulders were stable without apprehension or recurrence of instability. Postoperative mean Constant score was satisfactory (84), while the ROM was excellent.29
Significant acute reverse Hill-Sachs lesions (20%–40%) can also be treated using a deltopectoral approach and bone grafting or allograft. The ideal patient for these techniques is young, with good healing potential. An iliac crest bone graft can be inserted under the cartilage for support, following fracture disimpaction.15
Aksekili et al.30 performed a retrospective analysis (LoE: IV) of seven patients (ten shoulders) who underwent iliac autograft with glenoid augmentation for chronic posterior disarticulation of the glenohumeral joint. All these patients were male with a mean follow-up period of 40.6 months. During the clinical evaluation, all of them had locked posterior shoulder dislocation. The mean postoperative Constant score was 81.25. Two shoulders were evaluated as excellent, three as good, four as moderate and one as poor, while at final follow-up all shoulders were stable.
Diklic et al.31 reviewed 13 patients (13 shoulders) with a mean follow-up of 54 months (LoE: IV). At that time, 12 had a stable, functional shoulder after allograft reconstruction; however, one developed spontaneous osteonecrosis of the humeral head and had an unsatisfactory result. Only nine patients were free of pain. Of the remaining, three reported occasional mild night pain without the need for analgesia and the patient with spontaneous osteonecrosis had moderate slight pain that required the use of oral analgesics. In relation to the postoperative functional outcome scoring system, the observed mean Constant score was 86.8.
Martinez and co-workers32 performed allograft reconstruction of segmental defects of the humeral head combined with posterior dislocation of the shoulder in six patients (LoE: IV). All these cases were clinically and radiologically assessed at a mean of 122 months after surgery. Of these six men, three had excellent postoperative results with no pain, instability, clicking or catching, whereas three complained of pain, stiffness, clicking, and catching. The mean postoperative Constant score at the last follow-up was 69.2. The authors concluded that posterior dislocations of the shoulder treated by allograft reconstruction associated with the segmental defects of the humeral head, had a good long-term follow-up result in 50% of the patients in their study. In addition, Struck et al.33 examined a series of 13 patients (15 shoulders) with persistent posterior dislocation (LoE: IV), who underwent posterior bone block procedure. At follow-up, these patients were divided in two separate groups; nine patients were assessed at short-term follow-up (mean follow-up: 17.5 months) and six ones at long-term follow-up (mean follow-up: 89.5 months). The results after clinical evaluation were not significantly different between the two groups, while the overall results in the subjective and the objective scores (the Constant score was noted at 82) were good or very good. There was no significant alteration in pain between the two groups, whereas active ranges of movement and strength evaluations were normal in all cases.
Barbier et al.34 reported eight cases that underwent a posterior iliac bone-block procedure (LoE: IV). The mean follow-up was 34 months. The mean postoperative Constant score was 96.25, while any functional, mobility and strength assessments were normal in all cases.
Servien and his colleagues35 performed a retrospective analysis of 20 patients (21 shoulders), that were treated by a posterior bone block reconstruction procedure (LoE: IV). At an average follow-up of 72 months, the mean Constant score was 93.3. All the patients were satisfied with the results. Nevertheless, only 15 patients came back to sports at their pre-injury level. Two shoulders had glenohumeral arthritis on radiographs at the latest follow-up.
Bock et al.36 reported a series of six patients treated by elevation of the defect, filling it with graft and fixation thereafter (LoE: IV). At a mean follow-up of 62.7 months, the result was found to be excellent for two patients and good for four patients with a mean Constant score of 88.2. Gerber et al.37 described a series of nineteen cases treated by reconstruction with segmental femoral head allograft (LoE: IV). Eighteen shoulders were appraised as subjectively excellent; none were rated as good, and one as fair. At a mean follow-up of 128 months, the final Constant score averaged 77.
Osteosynthesis
Another treatment method that has been described in the literature is the ORIF. Fiorentino et al.38 reported five cases that treated with ORIF through double approaches: a posterior approach for the reduction of the humerus and the fixation of the posterior capsule and an anterior deltopectoral for the osteosynthesis (LoE: IV). Out of five patients, no one complained about having pain at 24 months follow-up and all of them have come back to their previous avocation, while the postoperative Constant score at the last follow-up was 89.4.
Robinson et al.5 performed another examination on a consecutive series of 24 patients (24 shoulders) who had a combined acute posterior dislocation of the humeral head with a Neer two, three, or four-part fracture (LoE: IV). All of them were treated by an open relocation of the humeral head, bone grafting of humeral head defects and internal fixation of the fracture and involved in a 24 months follow-up evaluation program. At two years after surgery, 19 patients reported no pain in their shoulders, two complained of mild pain, which was not correlated with activities, and one reported moderate pain on use of the arm, whereas the mean Constant score was 83.5.
Arthroscopy
Arthroscopic posterior Bankart repair could be a treatment option of acute reducible dislocations with little or no humeral head impaction (20%) and with recurrent instability.15 Concerning the inclusion criteria of the present systematic review, there was no relevant article with arthroscopic repair as a treatment method for the posterior shoulder fracture-dislocation.
Arthroplasty
Massive humeral head impaction and a head defect over >40% can be treated using shoulder arthroplasty (hemiarthroplasty or reverse total shoulder arthroplasty). Hemiarthroplasty can be an appropriate treatment option for patients, who are not good candidates for graft incorporation.15 A case series of 11 patients (12 shoulders) was retrospectively reviewed by Gavriilidis and colleagues39 (LoE: IV). They performed nine uncemented hemiarthroplasties, one cemented hemiarthroplasty and two total cemented shoulder arthroplasties. Mean follow-up was 37.4 months and the mean postoperative Constant score was 67.1. There was a significant improvement in ROM for flexion, abduction and external rotation, whereas the researchers noticed negative correlation (Pearson's coefficient) between the related Constant score and number of previous operations, pain, and duration of symptoms.
Recurrent instability in the first year can occur in 18% of the cases.8 Some of the important risk factors are age (<40 years), seizures and the large reverse Hill-Sachs lesion (<1.5 cm3). Persistent functional impairment has been observed 2 years after the initial trauma, even without recurrent instability.8
Reverse shoulder arthroplasty on the other hand has shown satisfactory results and it is used when significant rotator cuff defect is present in elderly patients (LoE: V).40 Raiss et al.41 reported four chronic posterior shoulder dislocations treated with reverse shoulder arthroplasty leading to satisfactory results (LoE: IV).
It is clear that all the above-mentioned studies are either case series or case reports with LoE of IV and V. The lack of high LoE studies about this subject demonstrates the rarity of this condition and the difficulty to extract reliable information.
Considering the above-mentioned studies, a treatment algorithm is proposed, in order to help summarize the findings of the present study. The factors that the surgeons should examine are the chronicity of the injury, the presence of a fracture at the level of the surgical neck or tuberosities and the extend of the Hill-Sachs lesion if any, as these will determine the final operative technique.
The proposed algorithm is divided into two group of cases; the acute (<6 weeks) and the chronic posterior shoulder dislocation. The acute shoulder fracture-dislocations, if the fracture is visible on CT or if the shoulder after reduction is unstable or unreducible, an open reduction should be performed. However, the fixation method has to be amended according to the percentage of Hill-Sachs lesion. In the chronic group (>6 weeks), the elderly low-demand patients should be treated conservatively. For the rest of the patients, depending on the severity of the Hill-Sachs lesion different surgical options are available, including the McLaughlin technique, the use of an allograft, osteotomy or arthroplasty (hemiarthroplasty or reverse shoulder arthroplasty). These can be found in Fig. 3, where this algorithm is demonstrated.
Fig. 3.
Treatment algorithm.
Posterior shoulder fracture-dislocations are rare injuries that can be easily missed during the first assessment. Their treatment can be challenging, and the optimum surgical option depends on many variables. A treatment algorithm has been proposed by the authors based on the current literature in the effort to create a consensus to these injuries.
Funding
Nil.
Ethical statement
Not applicable.
Declaration of competing interest
The authors declare no competing financial interests.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Kowalsky M.S., Levine W.N. Traumatic posterior glenohumeral dislocation: classification, pathoanatomy, diagnosis, and treatment. Orthop Clin N Am. 2008;39:519–533. doi: 10.1016/j.ocl.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 2.McLaughlin H. Posterior dislocation of the shoulder. J Bone Jt Surg. 1952;34:584–590. [PubMed] [Google Scholar]
- 3.Hatzis N., Kaar T.K., Wirth M.A. The often overlooked posterior dislocation of the shoulder. Tex Med. 2001;97:62–67. [PubMed] [Google Scholar]
- 4.Neer C.S., Foster C.R. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. A preliminary report. J Bone Jt Surg Am. 1980;62:897–908. [PubMed] [Google Scholar]
- 5.Robinson C.M., Akhtar A., Mitchell M. Complex posterior fracture-dislocation of the shoulder: epidemiology, injury patterns, and results of operative treatment. J Bone Joint Surg Am. 2007;89:1454–1466. doi: 10.2106/JBJS.F.01214. [DOI] [PubMed] [Google Scholar]
- 6.Hawkins R.J. Unrecognized dislocations of the shoulder. Instr Course Lect. 1985;34:258–263. [PubMed] [Google Scholar]
- 7.Rowe C.R., Zarins B. Chronic unreduced dislocations of the shoulder. J Bone Joint Surg Am. 1982;64:494–505. [PubMed] [Google Scholar]
- 8.Robinson C.M., Orth F., Seah M. The epidemiology, risk of recurrence, and functional outcome after an acute traumatic posterior dislocation of the shoulder. J Bone Joint Surg Am. 2011;93:1605–1613. doi: 10.2106/JBJS.J.00973. [DOI] [PubMed] [Google Scholar]
- 9.Quillen D.M., Wuchner M., Hatch R.L. Acute shoulder injuries. Am Fam Physician. 2004;70:1947–1954. [PubMed] [Google Scholar]
- 10.Moore K.L., Anne M.R. fourth ed. Lippincott Williams & Wilkins; Philadelphia, PHL: 2007. Upper Limb. Essential Clinical Anatomy. [Google Scholar]
- 11.Robinson C.M., Aderinto J. Posterior shoulder dislocations and fracture-dislocations. J Bone Joint Surg Am. 2005;87:639–650. doi: 10.2106/JBJS.D.02371. [DOI] [PubMed] [Google Scholar]
- 12.Rouleau D.M., Hebert-Davies J. Incidence of associated injury in posterior shoulder dislocation: systematic review of the literature. J Orthop Trauma. 2012;26:246–251. doi: 10.1097/BOT.0b013e3182243909. [DOI] [PubMed] [Google Scholar]
- 13.Hawkins R.J., Neer C.S., 2nd, Pianta R.M. Locked posterior dislocation of the shoulder. J Bone Joint Surg Am. 1987;69:9–18. [PubMed] [Google Scholar]
- 14.Moeller J.C. Compound posterior dislocation of the glenohumeral joint. Case report. J Bone Joint Surg Am. 1975;57:1006–1007. [PubMed] [Google Scholar]
- 15.Rouleau D.M., Hebert-Davies J., Robinson C.M. Acute traumatic posterior shoulder dislocation. J Am Acad Orthop Surg. 2014;22:145–152. doi: 10.5435/JAAOS-22-03-145. [DOI] [PubMed] [Google Scholar]
- 16.Page P. Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes. Int J Sports Phys Ther. 2011;6:51–58. [PMC free article] [PubMed] [Google Scholar]
- 17.Roberts A., Wickstrom J. Prognosis of posterior dislocaiton. Acta Orthop Scand. 1971;42:328–337. doi: 10.3109/17453677108989053. [DOI] [PubMed] [Google Scholar]
- 18.Ogawa K., Yoshida A., Inokuchi W. Posterior shoulder dislocation associated with fracture of the humeral anatomic neck: treatment guidelines and long-term outcome. J Trauma. 1999;46:318–323. doi: 10.1097/00005373-199902000-00020. [DOI] [PubMed] [Google Scholar]
- 19.Walch G., Boileau P., Martin B. Unreduced posterior luxations and fractures-luxations of the shoulder. Apropos of 30 cases. Rev Chir Orthop Reparatrice Appar Mot. 1990;76:546–558. [PubMed] [Google Scholar]
- 20.Neer C.S., 2nd Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 21.Bloom M.H., Obata W.G. Diagnosis of posterior dislocation of the shoulder with use of Velpeau axillary and angle-up roentgenographic views. J Bone Joint Sur Am. 1967;49:943–949. [PubMed] [Google Scholar]
- 22.Wadlington V.R., Hendrix R.W., Rogers L.F. Computed tomography of posterior fracture-dislocations of the shoulder: case reports. J Trauma. 1992;32:113–115. doi: 10.1097/00005373-199201000-00024. [DOI] [PubMed] [Google Scholar]
- 23.Kim S.H., Ha K.I., Yoo J.C. Kim's lesion: an incomplete and concealed avulsion of the posteroinferior labrum in posterior or multidirectional posteroinferior instability of the shoulder. Arthroscopy. 2004;20:712–720. doi: 10.1016/j.arthro.2004.06.012. [DOI] [PubMed] [Google Scholar]
- 24.May V.R., Jr. Posterior dislocation of the shoulder: habitual, traumatic, and obstetrical. Orthop Clin N Am. 1980;11:271–285. [PubMed] [Google Scholar]
- 25.Detenbeck L.C. Posterior dislocations of the shoulder. J Trauma. 1972;12:183–192. doi: 10.1097/00005373-197203000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Hawkins R.J., Belle R.M. Posterior instability of the shoulder. Instr Course Lect. 1989;38:211–215. [PubMed] [Google Scholar]
- 27.Heller K.D., Forst J., Forst R. Posterior dislocation of the shoulder: recommendations for a classification. Arch Orthop Trauma Surg. 1994;113:228–231. doi: 10.1007/BF00441838. [DOI] [PubMed] [Google Scholar]
- 28.Castagna A., Delle Rose G., Borroni M. Modified MacLaughlin procedure in the treatment of neglected posterior dislocation of the shoulder. Chir Organi Mov. 2009;93(Suppl. 1):S1–S5. doi: 10.1007/s12306-009-0001-y. [DOI] [PubMed] [Google Scholar]
- 29.Kokkalis Z.T., Mavrogenis A.F., Ballas E.G. Modified McLaughlin technique for neglected locked posterior dislocation of the shoulder. Orthopedics. 2013;36:e912–e916. doi: 10.3928/01477447-20130624-22. [DOI] [PubMed] [Google Scholar]
- 30.Aksekili M.A., Uğurlu M., Işık Ç. Posterior bone block of chronic locked posterior shoulder dislocations with glenoid augmentation: a retrospective evaluation of ten shoulders. Int Orthop. 2016;40:813–820. doi: 10.1007/s00264-015-2907-3. [DOI] [PubMed] [Google Scholar]
- 31.Diklic I.D., Ganic Z.D., Blagojevic Z.D. Treatment of locked chronic posterior dislocation of the shoulder by reconstruction of the defect in the humeral head with an allograft. J Bone Joint Surg Br. 2010;92:71–76. doi: 10.1302/0301-620X.92B1.22142. [DOI] [PubMed] [Google Scholar]
- 32.Martinez A.A., Navarro E., Iglesias D. Long-term follow-up of allograft reconstruction of segmental defects of the humeral head associated with posterior dislocation of the shoulder. Injury. 2013;44:488–491. doi: 10.1016/j.injury.2012.10.027. [DOI] [PubMed] [Google Scholar]
- 33.Struck M., Wellmann M., Becher C. Results of an open posterior bone block procedure for recurrent posterior shoulder instability after a short- and long-time follow-up. Knee Surg Sports Traumatol Arthrosc. 2016;24:618–624. doi: 10.1007/s00167-014-3495-2. [DOI] [PubMed] [Google Scholar]
- 34.Barbier O., Ollat D., Marchaland J.P. Iliac bone-block autograft for posterior shoulder instability. Orthop Traumatol Surg Res. 2009;95:100–107. doi: 10.1016/j.otsr.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 35.Servien E., Walch G., Cortes Z.E. Posterior bone block procedure for posterior shoulder instability. Knee Surg Sports Traumatol Arthrosc. 2007;15:1130–1136. doi: 10.1007/s00167-007-0316-x. [DOI] [PubMed] [Google Scholar]
- 36.Bock P., Kluger R., Hintermann B. Anatomical reconstruction for Reverse Hill-Sachs lesions after posterior locked shoulder dislocation fracture: a case series of six patients. Arch Orthop Trauma Surg. 2007;127:543–548. doi: 10.1007/s00402-007-0359-y. [DOI] [PubMed] [Google Scholar]
- 37.Gerber C., Catanzaro S., Jundt-Ecker M. Long-term outcome of segmental reconstruction of the humeral head for the treatment of locked posterior dislocation of the shoulder. J Shoulder Elbow Surg. 2014;23:1682–1690. doi: 10.1016/j.jse.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 38.Fiorentino G., Cepparulo R., Lunini E. Posterior shoulder fracture-dislocation: double approach treatment. Our experience. Acta Biomed. 2016;87:184–190. [PubMed] [Google Scholar]
- 39.Gavriilidis I., Magosch P., Lichtenberg S. Chronic locked posterior shoulder dislocation with severe head involvement. Int Orthop. 2010;34:79–84. doi: 10.1007/s00264-009-0762-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hyun Y.S., Huri G., Garbis N.G. Uncommon Indications for reverse total shoulder arthroplasty. Clin Orthop Surg. 2013;5:243–255. doi: 10.4055/cios.2013.5.4.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Raiss P., Edwards B.T., Bruckner T. Reverse arthroplasty for patients with chronic locked dislocation of the shoulder (type 2 fracture sequela) J Shoulder Elbow Surg. 2017;26:279–287. doi: 10.1016/j.jse.2016.05.028. [DOI] [PubMed] [Google Scholar]