Abstract
Background:
Pediatric healthcare institutions are increasingly implementing food insecurity (FI) screens, but there is limited information about participant interest in referral and engagement with resources provided.
Methods:
In this descriptive cross-sectional study, we recruited participants from a consecutive sample of adult caregivers arriving with pediatric patients in the ED at an urban, freestanding children’s hospital. Caregivers completed a validated, two-question screen for FI. All participants received a list of food access resources. Direct referral to a partnered community food resource agency was offered to those who screened positive for FI; that agency completed a phone call to the participant for resource provision within 2 weeks.
Results:
Among the 1818 participants recruited, 20.6% (375) screened positive for FI, consistent with the area’s reported child FI rate. Of those who screened positive, 54.9% (206) opted to receive a direct-referral via phone call to a food resource agency, and 35.9% (74) of these were reached by phone. 31.1% (23) of those contacted were no longer interested in food resource referrals, 10.8% (8) were signed up for the Supplemental Nutrition Assistance Program, and 59.5% (44) were referred to local food pantries.
Conclusions:
Through hospital-community partnership in an initial attempt to screen and offer direct-referral for FI, we elicited considerable interest among families for connection to resource agencies. However, there was a substantial gap between referral acceptance and ultimate connection with the resource agency stemming from two major sources: inability to re-contact and loss of interest after contact.
Keywords: Food Insecurity, Resource Referral
Introduction:
Children living in poverty experience significant economic hardships that negatively impact their health and wellbeing into adulthood.1 Food insecurity (FI), defined as limited or uncertain access to adequate food due to a lack of money or other resources, is associated with poverty and can result in serious physical, behavioral, and developmental health outcomes in children.2 Children who live in food insecure households suffer from increased rates of anxiety, aggression, anemia, asthma, cognitive delay, and increased rates of hospitalizations, among other adverse health outcomes.3–9 As of 2017, 21.3% of children living in Philadelphia County experience FI, surpassing the national average of 17%.10
Recognizing the significance of these adverse outcomes, several medical organizations now recommend routine screens for FI and other social risk factors.11,12 The American Academy of Pediatrics (AAP) recommends screening for FI at all scheduled health maintenance visits, and the Center for Medicare and Medicaid Services developed a tool for universal health-related social needs screening, including FI, of all individuals seeking care.12–14 The Emergency Department (ED) of academic medical centers often serves as a point of care entry for impoverished and high-risk families; as such, it has emerged as another prime location for screening and interventions to address social risk for those who may not have regular follow up with primary care, or when primary care screening has not yet been implemented.15–18
Despite the shift toward increased screening, there is limited information about participant interest in referral and engagement with resources provided.19,20 Studies have shown surprisingly low concordance between those to identify social risk and those who desire resources.23,21 Additionally, systematic reviews of interventions to tackle FI highlight the limitations in the existing evidence base, with studies focusing primarily on provision of referrals as an outcome measure rather than participant uptake.20,22
Two major types of resource referral processes are described in the pediatric literature, each with their own set of potential benefits and limitations. Low-touch interventions to address FI, such as distribution of a food resource sheet, are the simplest to employ, and have been implemented in multiple settings.23,24 However, this model confers the responsibility of resource navigation to an already stressed family, which may result in low rates of resource utilization. In one cluster-randomized study comparing screening with participant driven referral vs. usual care, there was a marginal increase in resource connection for the treatment group, with 39% enrolling in a new resource after paper referral, as compared to 24% in the control group, at 1- month follow-up.25 High-touch interventions, such as care navigation models, provide the most comprehensive and individualized care, but given the time and resource-intensive nature of program operation, there has been limited implementation of these models across institutions, and there is substantial reported patient dropout during intervention periods.26 A randomized controlled trial directly comparing use of a care navigation model to participant driven referral showed a decrease in the number of social needs reported in the care navigation group after 4 months; however, 40% of participants were lost to follow-up, and it is unclear whether this reduction in social need was the effect of resource connection or some other effect of care navigation.27
In an effort to maximize reach and benefit to patients while minimizing administrative burden to healthcare institutions, this study investigates the acceptance and outcome of a “medium-touch” intervention that offers direct connection by phone to a partnered community food resource agency, in combination with a resource sheet, on food resource engagement.
Methods:
Setting, Participants, and Eligibility Criteria
Participants were drawn from a consecutive sample of adult caregivers accompanying pediatric patients in the emergency department (ED) of a large, urban children’s hospital in Philadelphia. In 2017 this ED saw 66,952 unique patients over a total of 99,369 encounters; 55% were African American and 9% Latino; 3% were non-English speaking. Prior to initiation of study procedures, there were no FI screening or referral protocols. Eligibility criteria for participation included English-speaking caregivers who brought patients age <18 years to the ED, excluding those in critical condition.
Study Design and Procedures
This is a descriptive cross-sectional study of an opt-in resource referral process offered within a randomized trial comparing verbal and tablet-based screening for FI, and exploring caregiver preferences regarding screening modality and location.28 Four-hour periods between the hours of 8am and 11pm, 7 days a week from June-November 2017, were pre-assigned for study recruitment. Caregivers were approached in room order (1 through 47), with an attempt to enroll all eligible patients. Because patients are randomly allocated to rooms in our ED, the ordinal approach was expected to ensure consecutive sampling while minimizing selection bias.
Screening was completed in individual clinical rooms between medical evaluations, during waiting periods, or after discharge. We verbally consented caregivers who met eligibility criteria and assigned them to a study group using block randomization that was predetermined and allocated by a computer program (REDCap).29 Participants completed a two-question validated FI screen either by face-to-face interview or via tablet-based self-completed questionnaire with an optional audio assist by text-to-voice functionality. Face-to-face interviews were performed by research assistants with training in medical interviewing techniques. Those randomized to the tablet-based group were given a brief tutorial regarding use of the tablet and text-to-voice functionality. Identical surveys were used for both study arms and were written at the fifth-grade reading level. We conducted all study procedures on a designated study tablet (iPad), with information recorded directly into REDCap. All respondents were provided with a paper-based list of food resources including information about federal programs, local emergency food assistance, and free and reduced-price produce by the research assistant following the questionnaire. Those who reported FI were additionally offered direct telephone-contact within 2 weeks after the ED visit by the Philadelphia Coalition Against Hunger, a food resource agency that assists with enrollment in federal programs and provides navigation to emergency food assistance; this option was provided at the time of positive screen in the same modality as the remainder of the questionnaire. Per the hospital’s routine protocol, a social worker was always available on premises to assist families by request. All study procedures were deemed exempt from review by the hospital’s Committee for the Protection of Human Subjects.
Measures
Participant Demographics
We collected information on patient age and level of acuity based on the 5-level Emergency Severity Index system for each patient.30 Respondents self-reported race and ethnicity.
Food Insecurity Reporting:
We measured FI using the validated two-question “Hunger Vital Sign” screening tool, with yes/no responses.31 These two questions are: within the past 12 months “we worried whether our food would run out before we got money to buy more” and “the food we bought just didn’t last and we didn’t have money to get more.”
Interest in Direct Connection to Food Agency
Respondents who screened positive for FI indicated “yes” or “no” to the following question: Would you like a staff member from the Philadelphia Coalition Against Hunger to call you to help you find food assistance? For those responding “yes,” we documented a preferred phone number and the Philadelphia Coalition Against Hunger called the family within 2 weeks of their ED visit. We subsequently collected data from the Philadelphia Coalition Against Hunger regarding the ability to complete the call and types of resources offered.
Data Analysis
Sample size calculation was based on 2-sided Fisher’s exact test comparing two independent proportions with type I error rate of 0.05. The primary study sample size of at least 1808 caregivers was determined to address comparison of disclosed FI by screening modality. We used T-tests and chi square tests to compare demographic variables and screening modality preference related to acceptance of FI referral resources. Statistical analysis was preformed using Stata 14.2.
Results:
Of 2154 approached patients, 130 were excluded as there was no caregiver present and 204 (10%) declined participation, therefore 1820 caregivers were enrolled in the study. Two tablet- based questionnaires (0.2%) were incomplete, leading to an overall response rate of 89.9% for eligible respondents. Of the 1818 participants, 20.6% screened positive for FI. There were no significant differences in patient age or level of acuity between FI and non-FI groups. Rates of reported FI were lower among caregivers identifying as White and not Hispanic or Latino (Table 1).
Table 1:
Characteristics of Participants by Reported Food Insecurity
| Total (N=1818) | Food Insecure (N=375) | NOT Food Insecure (N=1441) | |
|---|---|---|---|
| Patient Age, Mean (SD) | 10.04 (6.9) | 9.15 (6.9) | 10.27 (6.9) |
| Race, N(%) | |||
| American Indian/Alaska | 16 (0.9) | 5 (1.3) | 11 (0.8) |
| Asian* | 73 (4.0) | 7 (1.9) | 66 (4.6) |
| Hawaiian/Pacific Islander | 4 (0.2) | 1 (0.3) | 3 (0.2) |
| Black/African | 764 (42.0) | 236 (69.2) | 528 (36.7) |
| American** | 783 (43.1) | 74 (19.7) | 709 (49.2) |
| White** | 64 (3.5) | 17 (4.5) | 47 (3.3) |
| More than one | 111 (6.1) | 35 (9.3) | 76 (5.3) |
| Not listed** | |||
| Ethnicity, N(%) | |||
| Hispanic or Latino** | 150 (8.3) | 51 (13.6) | 99 (6.9) |
| Not Hispanic or Latino* | 1583 (87.1) | 298 (79.7) | 1285 (89.2) |
| Unknown/Not Reported** | 81 (4.5) | 25 (6.7) | 56 (3.9) |
| Level of Acuity, N(%) | |||
| 1 (sickest) | 4 (0.2) | 1 (0.3) | 3 (0.2) |
| 2 | 642 (35.3) | 141 (37.6) | 501 (34.7) |
| 3 | 925 (50.9) | 173 (46.1) | 752 (52.1) |
| 4 | 236 (13.0) | 55 (14.7) | 181 (12.5) |
| 5 (least sick) | 11 (0.6) | 5 (1.3) | 6 (0.4) |
p<0.01,
p<0.05
Of those who reported FI, 54.9% (206) opted to receive a direct-referral via phone call to a food resource agency (hereafter defined as “referral acceptance”). There was a higher rate of referral acceptance among individuals identifying as Black/African American and lower rates of referral acceptance among those identifying as White (p=0.005). There were no significant differences in patient age, level of acuity, ethnicity, or screening modality used between those who accepted or declined referral. However, regardless of which type of screening modality they received, those who declined referral were significantly more likely to report a preference for tablet-based screening as compared to face-to-face screening for FI (p=0.002; Table 2).
Table 2:
Characteristics of Participants by Acceptance or Refusal of Direct Referral
| Total Food Insecure (N=375) | Accepted Referral (N=206) | Declined Referral (N=169) | |
|---|---|---|---|
| Patient Age, Mean (SD) | 9.15 (6.9) | 9.30 (6.86) | 8.96 (6.95) |
| Race, N(%)** | |||
| American Indian/Alaska | 5 (1.3) | 5 (2.4) | 0 (0.0) |
| 2 (1.0) | 5 (3.0) | ||
| Asian | 7 (1.9) | 1 (0.5) | 0 (0.0) |
| 142 (68.9) | 94 (55.6) | ||
| Hawaiian/Pacific Islander | 1 (0.3) | ||
| 28 (13.6) | 46 (27.2) | ||
| Black/African American | 236 (69.2) | ||
| 10 (4.9) | 7 (4.1) | ||
| White | 74 (19.7) | ||
| 18 (8.7) | 17 (10.1) | ||
| More than one | 17 (4.5) | ||
| Not listed | (9.3) | ||
| Ethnicity, N(%) | 51 (13.6) | 27 (13.2) | 24 (14.2) |
| Hispanic or Latino | 298 (79.7) | 167 (81.5) | 131 (77.5) |
| Not Hispanic or Latino | 25 (6.7) | 11 (5.4) | 14 (8.3) |
| Unknown/Not Reported | |||
| Level of Acuity, N(%) | |||
| 1 (sickest) | 1 (0.3) | 0 (0.0) | 1 (0.6) |
| 2 | 141 (37.6) | 70 (34.0) | 71 (42.0) |
| 3 | 173 (46.1) | 98 (47.6) | 75 (44.4) |
| 4 | 55 (14.7) | 36 (17.5) | 19 (11.2) |
| 5 (least sick) | 5 (1.3) | 2 (1.0) | 3 (1.8) |
| Screening Modality Used | |||
| Verbal | 161 (42.9) | 93 (45.1) | 68 (40.2) |
| Tablet | 214 (57.1) | 113 (54.9) | 101 (59.8) |
| Preferred Screening Modality** | (N=162, 43%) | (N=82, 40%) | (N=80, 47%) |
| Verbal | 25 (15.4) | 20 (24.4) | 5 (0.3) |
| Tablet | 265 (84.6) | 62 (75.6) | 75 (93.7) |
p<0.01
Among the 206 who accepted direct referral, 74 (35.9%) were reached by phone. 23 (31.1%) of those contacted were no longer interested in food resources, 8 (10.8%) received assistance signing up for the Supplemental Nutrition Assistance Program (SNAP), and 44 (59.5%) were referred to local food pantries. The Philadelphia Coalition Against Hunger left voicemails for the remainder of participants when possible (Figure 1).
Figure 1:
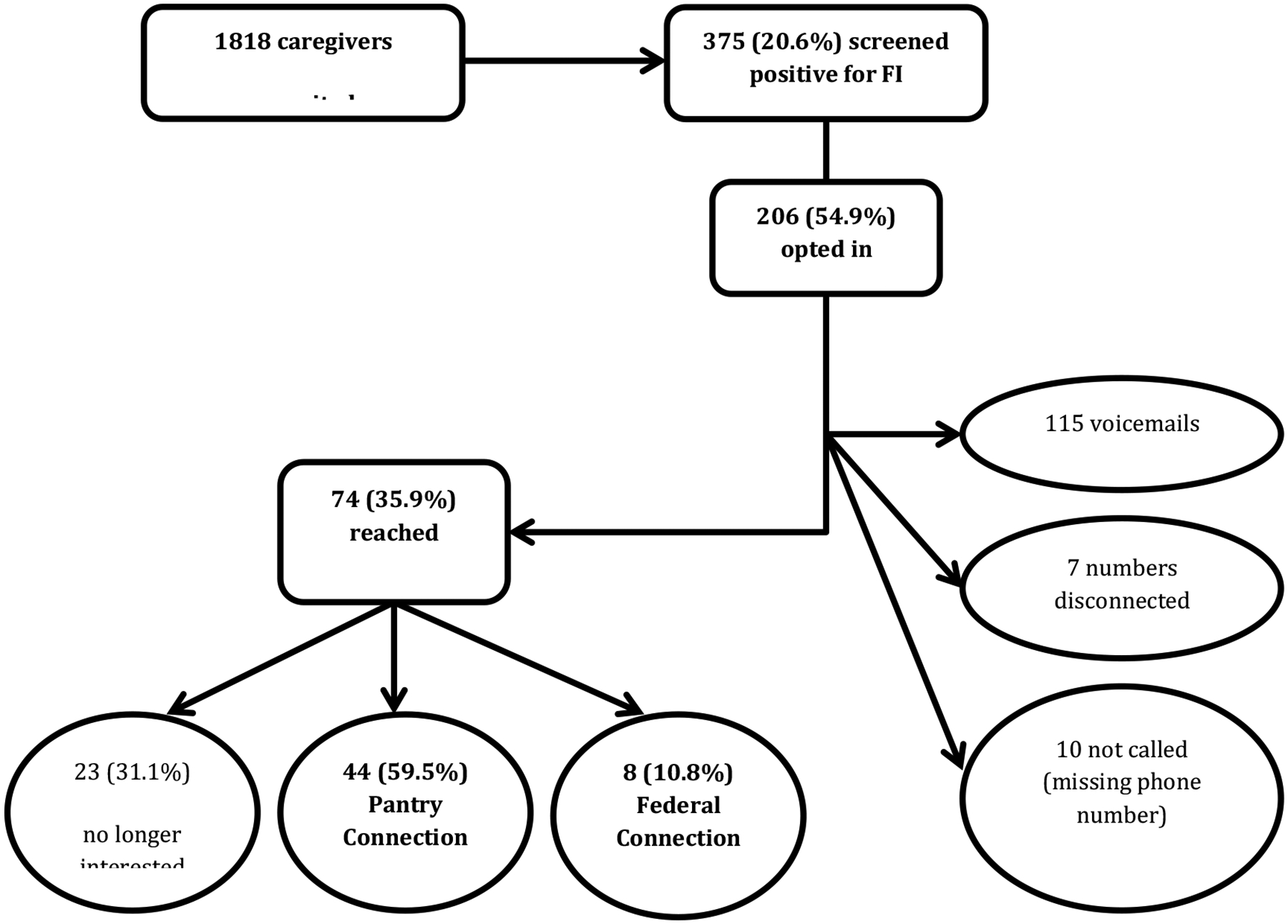
Interest and Outcome of Direct Connection to Food Resource Agency
Discussion
Screening for social risk, and FI in particular, has been recognized as an important component of the pediatric medical encounter. While there has been increasing awareness of the importance of FI screening, limited research describes caregiver interest in food assistance and the extent of resource engagement among caregivers who screen positive.20 Through this hospital-community partnership to provide a “medium-touch” intervention, we found that although the majority of caregivers in a pediatric ED showed interest in connecting to resource agencies, consistent with previous literature, there was a gap between interest and ultimate engagement with resource agencies.21,
There were two major sources of participant loss between initial referral acceptance and eventual engagement with the resource agency: inability to re-contact and loss of interest after contact. First, our partner resource agency could reach only 35.9% of caregivers who requested telephone follow up. This is consistent with previous literature examining research with socially disadvantaged groups.32 One systematic review described difficulty contacting participants due to frequent changes in phone numbers and addresses as the most common barrier related to follow-up data collection.33 In other efforts with difficult-to-reach patient populations, researchers have suggested using multiple methods of contact,34 cash and gift incentives,35 and keeping in regular contact with participants;36 however, these may not be feasible for efforts aimed at social resource provision. Connecting participants directly to a resource agency with either 1) on-site representatives, or 2) a phone call arranged in the exam room at the point-of-care could be an alternative to relying on a follow-up phone call.
The second point of participant loss in this study occurred when nearly one-third of those reached by phone were no longer interested in resource connection at the time of contact. While a subset of the population may have had urgent needs that were already met either through the paper resource or through other means, we suspect that there was loss of interest once resource options were provided. Our qualitative exploration of barriers to resource acceptance, discussed in detail elsewhere37, elucidated multiple reasons for declining resources initially and subsequent participant loss, including: negative past experiences with social assistance, perception of need as compared to others, accepting resources when “someone else could use it more,” and deprioritization of FI within a milieu of other life stressors, including those associated with medical acuity in the ED setting. It is possible that participants expected new or different resources to be offered through direct referral, and that they became disillusioned at the point of phone contact when familiar resources were offered. Additionally, phone contact requires relaying personal information verbally, reducing the ability to provide anonymity in responses. Our findings demonstrate that preference for a tablet-based screening modality was greatest in the group that declined referral. It may be that efforts that preserve anonymity in the resource referral process—such as use of electronic application, text message, or internet- based referrals—could increase referral uptake and ultimate resource connection, especially in the ED setting. Further research is needed to explore caregiver preferences in the resource referral and connection process, and to define best practices that close the gap between social need, interest, and ultimate engagement with resources.
Our study adds to a small but growing body of research that investigates results of interventions to address social need. The findings highlight that health policy, which to-date focuses on the implementation of social needs screening, should further emphasize the development of evidence-based interventions to improve engagement with social resources.
Limitations:
Limitations of the study include the inability to verify the self-reported data, including experience of FI and self-report of race/ethnicity. This could result in under or over-reporting of FI, potentially biasing the self-selection into or out of direct referral, as this option was only offered to those reporting FI. Furthermore, non-English speaking families were excluded from this study as follow up from our partner organization could not be assured to have multilingual capabilities. Although mitigated by the overall low prevalence (3%) of non-English speaking families in the Children’s Hospital of Philadelphia ED, we acknowledge that the exclusion of this population, which is known to be at increased risk for food insecurity, limits the generalizability of our results.2
In an effort to protect the identities of vulnerable families while working with a community-based organization, we do not know how many caregivers returned the resource agency’s phone call after receiving a voicemail. This may have resulted in an artificially low reported rate of resource engagement. Future studies integrating closed-loop referral processes to community agencies are important to identify the most comprehensive population of patients connected with resources.
Although we did not directly assess education or literacy, the food insecurity questions are written at a fifth-grade literacy level, and audio-assist was available to reduce this limitation. We mitigated selection bias by using consecutive sampling during pre-selected time-periods, and ultimately the study sample reflected the racial and ethnic demographics of our larger ED population.
Conclusions:
Through a hospital-community partnership offering a “medium-touch” intervention of direct- referral to a community agency for FI, we elicited considerable interest among families for connection to resources. However, there was a substantial gap between FI identification, referral acceptance, and ultimate resource engagement. This study highlights the need to further explore caregiver preferences in the development of resource referral processes to improve engagement with social resources.
What’s New:
We identified two major sources of participant loss between referral acceptance and resource engagement. Our findings highlight opportunities for improvements in social needs interventions, and suggests that health policy should emphasize the development of evidence-based interventions to improve resource engagement.
Funding source:
University of Pennsylvania Leonard Davis Institute of Health Economics
Ruth L. Kirschstein National Research Service Award (NRSA)- T32-HP10026
The funding sources had no role in study design; data collection, analysis, or interpretation; writing of the report, or submission of the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of Interest: None
References
- 1.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998; 14(4), 245–258. 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- 2.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2016. Washington, DC: US Department of Agriculture, Economic Research Service; 2017. [Google Scholar]
- 3.Whitaker RC, Phillips S, Orzol S. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics. 2006;118:e859–e868. [DOI] [PubMed] [Google Scholar]
- 4.Eicher-Miller HA, Mason A, Weaver C, et al. Food insecurity is associated with iron deficiency anemia in U.S. adolescents. Am J Clin Nutr. 2009;90:1358–1371. [DOI] [PubMed] [Google Scholar]
- 5.Skalicky A, Meyers A, Adams W, et al. Child food insecurity and iron deficiency anemia in low-income infants and toddlers in the United States. Matern Child Health J. 2006;10:177–185. [DOI] [PubMed] [Google Scholar]
- 6.Mangini Lauren D, Hayward Mark D, Dong Yong Quan, Forman Michele R. Household Food Insecurity Is Associated with Childhood Asthma. J Nutr. 2015;145(12):2756–2764. DOI: 10.3945/jn.115.215939 [DOI] [PubMed] [Google Scholar]
- 7.Rose-Jacobs R, Black MM, Casey PH, et al. Household food insecurity: associations with at-risk infant and toddler development. Pediatrics. 2008;121:65–72. [DOI] [PubMed] [Google Scholar]
- 8.Alaimo K, Olson CM, Frongillo EA. Food insufficiency and American school-aged children’s cognitive, academic, and psychosocial development. Pediatrics. 2001;108:44–53 [PubMed] [Google Scholar]
- 9.Cook JT, Frank DA, Berkowitz C, et al. Food insecurity is associated with adverse health outcomes among human infants and toddlers. J Nutr. 2004;134:1432–1438. [DOI] [PubMed] [Google Scholar]
- 10.Gundersen CA, Dewey A, Crumbaugh M, et al. Map the meal gap: a report on county and congressional district food insecurity and county food cost in the United States in 2016. Available at: http://map.feedingamerica.org/. Accessed March 15, 2020.
- 11.EveryONE project unveils social determinants of health tools. American Academy of Family Physicians. https://www.aafp.org/news/health-of-the-public/20180109sdohtools.html.) Published Jan 9, 2018. Accessed March 15, 2020.
- 12.Council on Community Pediatrics; Committee on Nutrition. Promoting food security for all children. Pediatrics. 2015; 136(5): e1431–e1438. [DOI] [PubMed] [Google Scholar]
- 13.Hager E, et al. Development and Validity of a 2-Item Screen to Identify Families at Risk for Food Insecurity. Pediatrics. 2010;126(1):e26–32. [DOI] [PubMed] [Google Scholar]
- 14.Billioux A, Verlander K, Anthony S, Alley D. Standardized screening for health-related social needs in clinical settings: The Accountable Health Communities Screening Tool. Washington, D.C.: National Academy of Medicine;2017. [Google Scholar]
- 15.Baker DW, Stevens CD, Brook RH. Regular source of ambulatory care and medical care utilization by patients presenting to a public hospital emergency department. JAMA. 1994;271:1909–1912. [PubMed] [Google Scholar]
- 16.Pane GA, Farner MC, Salness KA. Health care access problems of medically indigent emergency department walk-in patients. Ann Emerg Med. 1991;20:730–733. [DOI] [PubMed] [Google Scholar]
- 17.Hirshon JM, Morris DM. Emergency medicine and the health of the public: the critical role of emergency departments in US public health. Emerg Med Clin N Am. 2006;24(4):815–819. [DOI] [PubMed] [Google Scholar]
- 18.Garg A, Cull W, Olson L, Boyd AF, Federico SG, Dreyer B, Racine AD. Screening and referral for low-income families’ social determinants of health by US pediatricians. Academic Pediatrics. 2019. November 1;19(8):875–83. [DOI] [PubMed] [Google Scholar]
- 19.Torres J, De Marchis E, Fichtenberg C, et al. Identifying food insecurity in health care settings: a review of the evidence. Available at: https://sirenetwork.ucsf.edu/tools-resources/resources/identifyingfood-insecurity-health-care-settings-review-evidence. Accessed March 15, 2020. [DOI] [PubMed]
- 20.De Marchis EH, Torres JM, Benesch T, et al. Interventions addressing food insecurity in health care settings: a systematic review. Ann Fam Med. 2019;17(5):436–447. DOI: 10.1370/afm.2412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marchis E, Alderwick H, Gottleib L. Do Patients Want Help Addressing Social Risks? J Am Board Fam Med 2020;33:170–175. [DOI] [PubMed] [Google Scholar]
- 22.Holley CE, Mason CA. A Systematic Review of the Evaluation of Interventions to Tackle Children’s Food Insecurity. Curr Nutr Rep. 2019; 8:11–27. 10.1007/s13668-019-0258-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bottino CJ, Rhodes ET, Kreatsoulas C, et al. Food insecurity screening in pediatric primary care: can offering referrals help identify families in need? Acad Pediatr. 2017;17:497–503. [DOI] [PubMed] [Google Scholar]
- 24.Garg A, Butz AM, Dworkin PH, et al. Improving the management of family psychosocial problems at low- income children’s well-child care visits: the WE CARE Project. Pediatrics. 2007;120(3):547–558. [DOI] [PubMed] [Google Scholar]
- 25.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics. 2015;135(2):e296–e304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garg A, Sarkar S, Marino M, Onie R, Solomon BS. Linking urban families to community resources in the context of pediatric primary care. Patient Educ Couns. 2010;79(2):251–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gottlieb L, et al. Effects of Social Needs Screening and In-Person Service Navigation on Child Health. JAMA Pediatrics. 2016; 170(11):e162521. [DOI] [PubMed] [Google Scholar]
- 28.Cullen D, Woodford A and Fein J, 2019. Food for thought: a randomized trial of food insecurity screening in the emergency department. Academic pediatrics, 19(6), pp.646–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harris Paul A., Taylor Robert, Thielke Robert, Payne Jonathon, Gonzalez Nathaniel, Conde Jose G., Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support, J Biomed Inform. 2009. April;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tanabe P, Gimbel R, Yarnold PR, Kyriacou DN, & Adams JG (2004). Reliability and Validity of Scores on the Emergency Severity Index Version 3. Academic Emergency Medicine, 11(1), 59–65. DOI: 10.1197/j.aem.2003.06.013 [DOI] [PubMed] [Google Scholar]
- 31.Hager E, et al. Development and Validity of a 2-Item Screen to Identify Families at Risk for Food Insecurity. Pediatrics. 2010;126(1):e26–32. [DOI] [PubMed] [Google Scholar]
- 32.Signorello LB, Hargreaves MK, Steinwandel MD, Zheng W, Cai Q, Schlundt DG, Buchowski MS, Arnold CW, McLaughlin JK, Blot WJ. Southern community cohort study: establishing a cohort to investigate health disparities. J Natl Med Assoc. 2005;97(7):972–978. [PMC free article] [PubMed] [Google Scholar]
- 33.Bonevski B, Randell M, Paul C, et al. Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med Res Methodol. 2014;14:42. Published 2014 Mar 25. doi: 10.1186/1471-2288-14-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eakin EG, Bull SS, Riley K, Reeves M, Gutierrez S, McLaughlin P. Recruitment and retention of Latinos in a primary care-based physical activity and diet trial: the Resources for Health study. Health Educ Res. 2006;22(3):361–371. doi: 10.1093/her/cyl095. [DOI] [PubMed] [Google Scholar]
- 35.Festinger DS, Marlowe DB, Dugosh KL, Croft JR, Arabia PL. Higher magnitude cash payments improve research follow-up rates without increasing drug use or perceived coercion. Drug Alcohol Depend. 2008;96:128–135. doi: 10.1016/j.drugalcdep.2008.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Escobar-Chaves SL, Tortolero SR, Masse LC, Watson KB, Fulton JE. Recruiting and retaining minority women: findings from the Women On The Move study. Ethn Dis. 2002;12:242–251. [PubMed] [Google Scholar]
- 37.Cullen D, Attridge M, Fein JA. Food for Thought: A Qualitative Evaluation of Caregiver Preferences for Food Insecurity Screening and Resource Referral [published online ahead of print, 2020 Apr 14]. Acad Pediatr. 2020;S1876–2859(20)30170–4. doi: 10.1016/j.acap.2020.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]


