Abstract
Measuring adherence to 2015 US Preventive Services Task Force (USPSTF) diabetes prevention guidelines can inform implementation efforts to prevent or delay type 2 diabetes. A retrospective cohort was used to study patients without a diagnosis of diabetes attributed to primary care clinics within two large healthcare systems in our state to study adherence to: 1) screening at-risk patients and 2) referring individuals with confirmed prediabetes to participate in an intensive behavioral counseling intervention, defined as a CDC-recognized Diabetes Prevention Program (DPP). Among 461,866 adults attributed to 79 primary care clinics, 45.7% of patients were screened, yet variability at the level of the clinic ranged from 14.5% to 83.2%. Very few patients participated in a CDC-recognized DPP (0.52%; range 0%-3.53%). These findings support the importance of a systematic implementation strategy to specifically target barriers to diabetes prevention screening and referral to treatment.
Keywords: adherence, evidence-based guidelines, US Preventive Services Task Force, diabetes prevention, diabetes screening, Diabetes Prevention Program
Introduction
Type 2 diabetes mellitus (T2DM) is preventable, expensive, and impacts many American lives. The Diabetes Prevention Program (DPP) demonstrated sustained effectiveness in decreasing T2DM incidence through lifestyle change1,2 and it has been translated into community-based and primary care settings. However, data to guide benchmarking of diabetes screening and participation in intensive behavioral counseling are lacking. While a recent report suggests the longest decline of new US diabetes cases since 2009,3 high-risk groups continue to experience higher incidence.
The US Preventive Services Task Force (USPSTF) recommends screening every 3 years for abnormal blood glucose in adults aged 40-70 years who are overweight/obese while referring individuals with abnormal glucose values to intensive behavioral counseling.4 Research studies have documented health5 and cost benefits6 to patients with implementation of USPSTF guidelines,7,8 but lack of knowledge among providers persists for screening, diagnosing and managing prediabetes.9
This study combines screening and DPP participation data from two healthcare systems delivering most of the clinical care in our state. The objective is to report baseline adherence to USPSTF guidelines and provide the foundation for future research that utilizes quality improvement and implementation science methods to improve fidelity to evidence-based best practices for prediabetes.
Methods
Participating Clinics
Clinical data were collected from two healthcare systems in our state. This included a community-based, non-profit, integrated healthcare delivery system that provides more than half of all healthcare services within our state and an academic healthcare system with an affiliated health plan and community-based outpatient clinics. Together, they deliver 85% of care in our state. Eligible primary care clinics included family medicine, internal medicine, and geriatrics. Patients attributed to other medical specialties (e.g., cardiology), pediatric clinics or clinics with < 100 patients were excluded.
Target Patient Population
Data from adults (aged ≥ 18 years) who received care from either healthcare system between 2016-2018 were abstracted from the respective Enterprise Data Warehouses. Individuals attributed to a primary care clinic without a diagnosis of diabetes were considered eligible. This study was approved by both healthcare system institutional review boards (IRB #1050695).
Adherence to US Preventive Services Task Force Guidelines measures
In 2015, USPSTF recommended two evidence-based diabetes prevention guidelines: 1) screening at-risk patients and 2) referring individuals with prediabetes to intensive behavioral counseling intervention.4 Both guidelines were grade B evidence level indicating “there is high certainty that the net benefit is moderate to substantial”.4 Commercial health plans typically reimburse grade B indications.
Screening for diabetes:
Eligible patients were aged 40-70 years with Body Mass Index ≥25 kg/m2 and ≥1 outpatient encounter during the 36-month measurement period. Screening was defined as having ≥ 1 screening test (HbA1C or Fasting Plasma Glucose) during the 3-year period.
Participation in Intensive Behavioral Counseling:
Eligible patients were individuals with an outpatient encounter during the study period and documentation of confirmed prediabetes (HbA1c 5.7-6.4% or Fasting Plasma Glucose 100-125 mg/dL). Participation in an Intensive Behavioral Counseling program was defined by those that who participated in a CDC-recognized DPP—a program that is the most universal form of intensive behavioral counseling for individuals with prediabetes across the country.
An additional measure was calculated for the community-based, integrated healthcare delivery system patients only. This institution offers 3 different DPP interventions: CDC-recognized DPP and two lower intensity, evidence-based behavioral counseling interventions.10,11 DPP interventions have previously been described and evaluated.12,13 For this measure, we counted patients who participated in any of 3 DPP interventions.
Other demographic data variables
Patient demographic data within each clinic were collected and averaged among patients meeting study criteria. Data included risk factors for diabetes: aged 40-70 years, male sex, high risk race/ethnicity, body mass index ≥ 25 kg/m2, Medicare insurance, and individuals with confirmed prediabetes.
Statistical Analysis.
Descriptive statistics within each clinic are presented. For each, we calculated an adherence rate to each USPSTF evidence-based guidelines. Rates were visualized by patient panel size to determine if variation could be explained by this variable. Analyses were conducted using Stata 12.0 (Stata Corp, College Station, TX).
Results
Study Population
A total of 581,900 patients were identified with an outpatient encounter during 2016-2018 with 461,866 (79.4%) served by the community-based, integrated healthcare delivery system and 120,034 (20.6%) by the academic healthcare system (Figure 1). Of these, 489,444 patients among 79 clinics met inclusion criteria. Of the study population, 151,981 (31.5%) were eligible for diabetes screening and 37,443 (7.7%) had confirmed prediabetes. Less than half were aged 40-70 years (41.7%), male (45.5%), and identified as a high-risk race/ethnicity (12.7%) (Supplemental Digital Content1).
Figure 1:
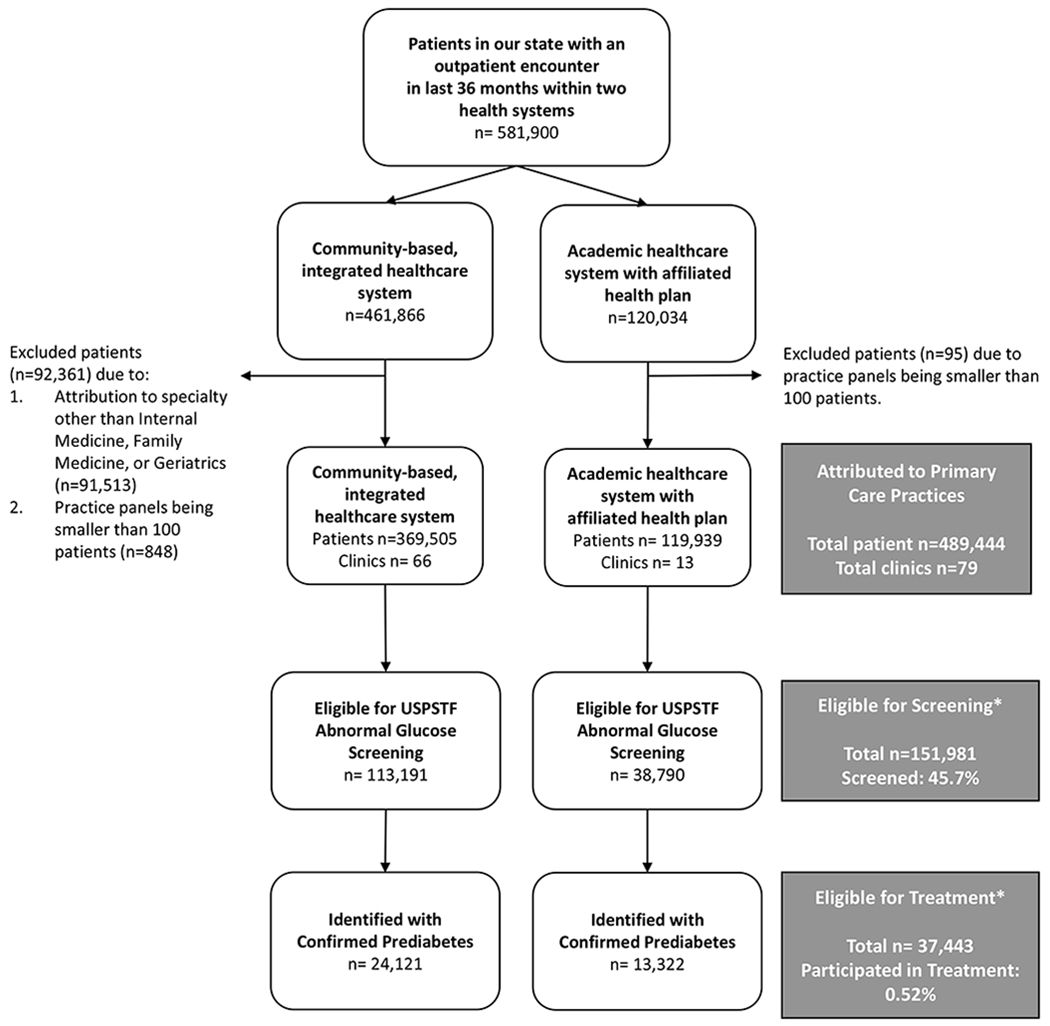
Consort Diagram. Includes eligible population from two healthcare systems in our state who are attributed to a primary care practice, and eligible for screening and diabetes prevention treatment according to the US Preventive Services Task Force guidelines.
*According to 2015 US Preventive Services Task Force (USPSTF) Abnormal Blood Glucose Guidelines
Adherence Rates to US Preventive Services Task Force Guidelines measures
The median percentage of patients who received diabetes screening was 45.7% (range 14.5%-83.2%) and 0.52% with prediabetes (range 0%-3.53%) participated in CDC-recognized DPP program. Clinics varied substantially in diabetes screening rates (Figure 2) and DPP program participation (Figure 3), but no clear pattern was seen by panel size. When including the additional interventions delivered by the community-based, integrated healthcare delivery system, the median participation was 12.7% (range 01%-30.4%) (Figure 4).
Figure 2-. Variation in panel size of patients and diabetes screening adherence according to US Preventive Services Task Force (USPSTF) guidelines across 79 primary care clinics.
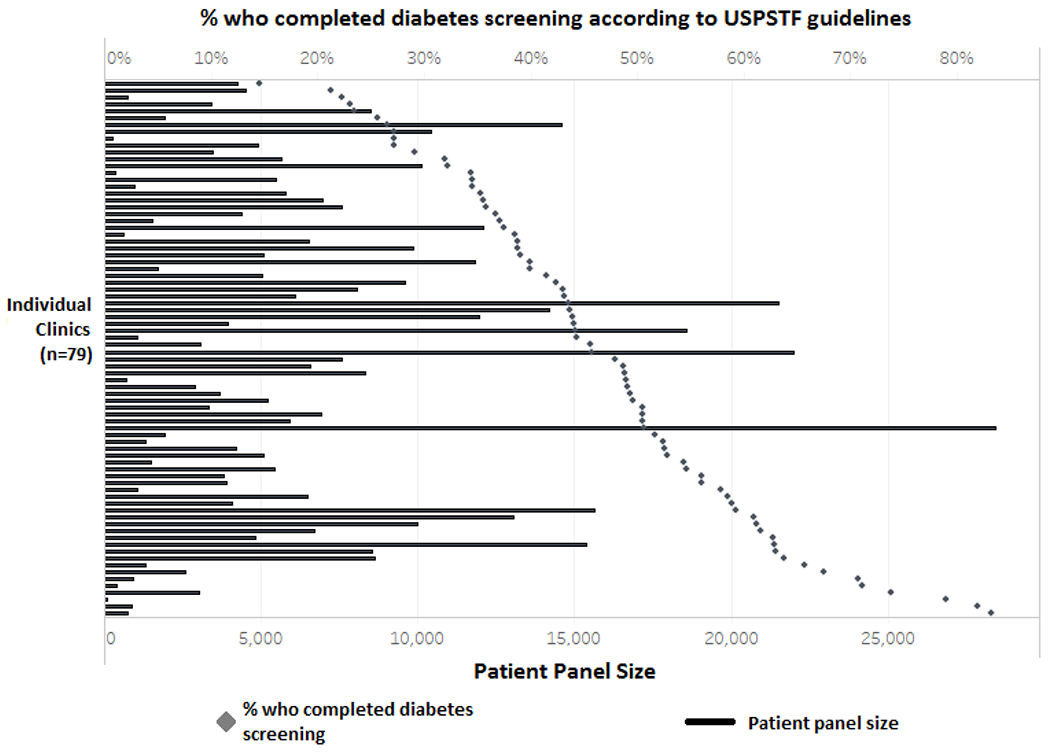
Each clinic’s panel size is indicated by the black line, with the percentage of patients who complete diabetes screening by clinic as indicated by the gray diamond. USPSTF diabetes screening adherence was defined by receiving at least 1 screening test (either HbA1C or Fasting Plasma Glucose) during the 3 years prior to their first outpatient encounter date among patients 40-70 years of age who have a body mass index ≥25 kg/m2.
Figure 3. Variation in panel size of patients and percentage of patients who participate in an Intensive Behavioral Counseling program according to US Preventive Services Task Force (USPSTF) guidelines across 79 primary care clinics.
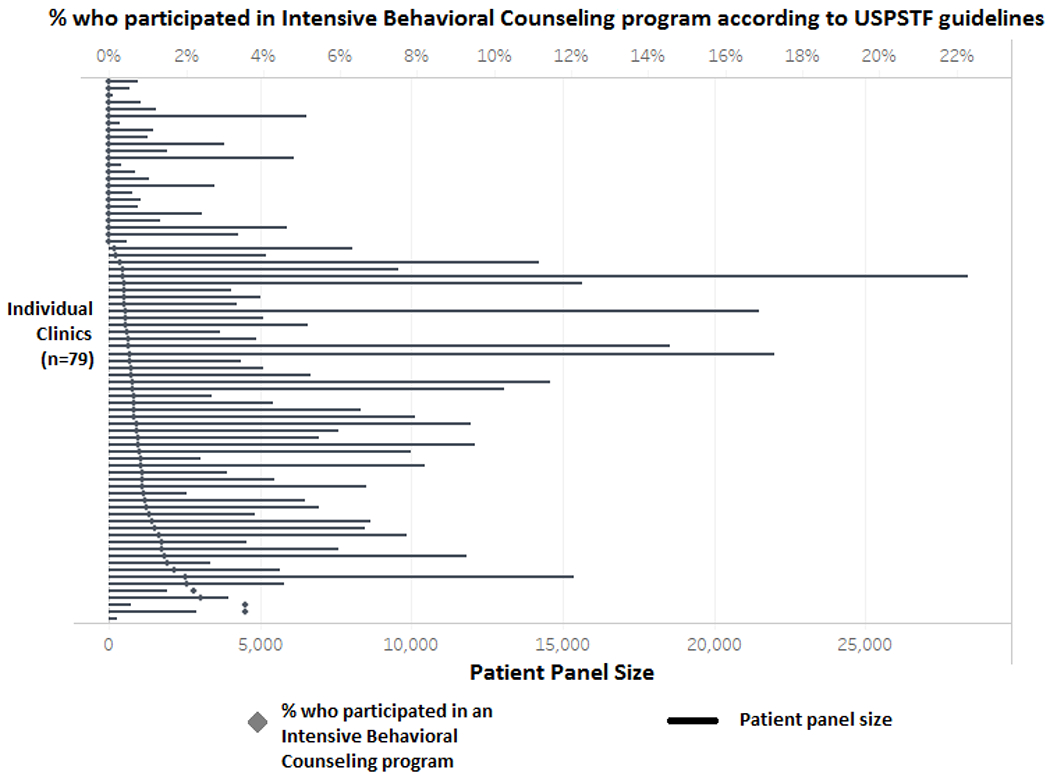
Each clinic’s panel size is indicated by the black line, with the percentage of patients who participate in an Intensive Behavioral Counseling program by clinic indicated by the gray diamond. Participation in an Intensive Behavioral Counseling program was defined by participating in a CDC-recognized Diabetes Prevention Program among patients with confirmed prediabetes in accordance to USPSTF diabetes prevention guidelines.
Figure 4-.
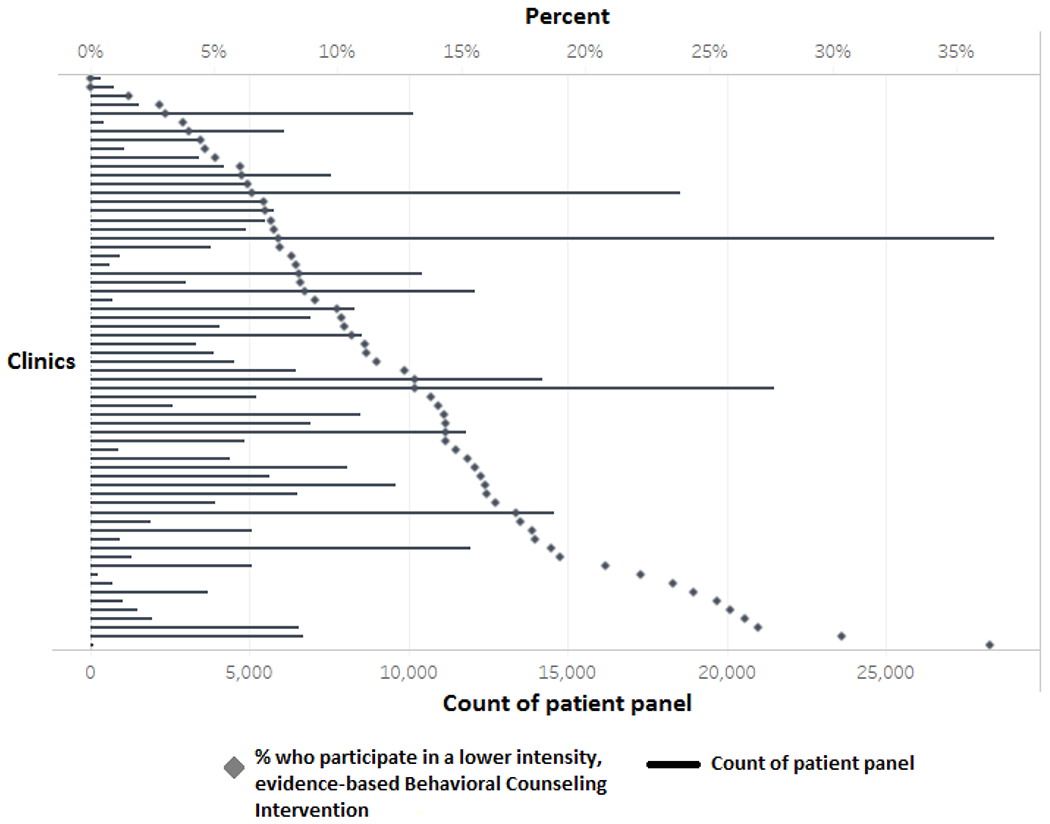
Variation in panel size of patients and percentage of patients who participate in lower intensity, evidence-based Behavioral Counseling Interventions across only primary care clinics within the community-based, integrated healthcare delivery system (n=66). Each clinic’s panel size is indicated by the black line, with the percentage of patients who participate in a lower-intensity, evidence-based Behavioral Counseling Intervention by clinic indicated by the black diamond. Lower-intensity, evidence-based Behavioral Counseling Intervention was defined by participation in one of three different DPP intervention modalities (including either CDC-recognized Diabetes Prevention Program, Medical Nutrition Therapy, or Prediabetes 101).
Limitations
Data for screening and participation services delivered outside of the two healthcare systems were not available. Because we used data from two institutions, there may be misclassification due to coding differences. There was an inability to account for a patient’s readiness to engage or insurance coverage for screening or intervention, both factors that could participation rates. Other clinic or institution level factors were not assessed.
Discussion
In this large, multi-center cohort representing the majority of care in our state, we observed substantial variation across primary care clinics in the quality of diabetes prevention services, measured by adherence to USPSTF guidelines. Participation in a CDC-recognized DPP curriculum was low (<1%) across the study population. Participation rates were higher in clinics (~13%) that also offered less intensive, evidence-based interventions. Variability was not related to clinic panel size.
Measuring adherence to USPSTF guidelines at a population level is suboptimal and benchmarking across systems does not exist. National quality indicators for health systems and payers (e.g. Medicare Stars Ratings, Merit-based Incentive Payment System) do not include diabetes prevention in their activities rather only management of diabetes post diagnosis. Previous studies have documented adherence rates of 25% to 51% to 2008 USPSTF diabetes screening guidelines recommending screening for asymptomatic adults with elevated blood pressure.14,15 We did not find comparable screening studies using 2015 USPSTF guidelines. Our participation results were consistent with a nationally representative sample of 28,354 individuals who self-reported “ever participating in a year-long program to prevent diabetes”.16 Higher participation rates for clinics that offered other, lower intensity interventions may suggest that patients prefer less intensive interventions and could be considered as an avenue to nudge participants towards higher intensity programs over time.
Conclusion:
Within a large, multi-center cohort, less than half of eligible adults were screened for diabetes and very few with prediabetes participated in treatment. Given the prevalence of prediabetes and in absence of a systematic implementation strategy, many patients are not aware of their prediabetes conditions, resulting in a health care failure to adequately prevent diabetes. Focusing efforts on surveillance of screening, referral, and participation needs to be a significant focus and a necessary investment for health systems to achieve our goal of preventing diabetes.
Implications:
Screening, diagnosing, and managing prediabetes is an effective approach to prevent or delay type 2 diabetes in people with prediabetes. Currently, eighty-four million Americans have prediabetes and 9 out 10 of these individuals are unaware that they have this condition. If left unchecked, it is estimated that there will be a 25% increase in the number of patients with type 2 diabetes that will need chronic disease management in the next 5 years—a substantial proportion of whom who will need care delivered in currently under-resourced, overburdened primary care clinics.
CDC-recognized behavior change programs are included in the health benefit plans of many private health insurers and the Medicare Diabetes Prevention Program has recently extended the insurance coverage to Medicare beneficiaries. However, no national quality measures exist in the U.S. for use at the individual physician/group practice level that would guide improvement and awareness efforts. Data to guide benchmarking of diabetes screening and participation in intensive behavioral counseling across large populations and health systems are lacking. The high prevalence of risk characteristics, patient volume and substantial provider variability in diabetes screening frequency and referral to treatment highlight the importance of using a systematic implementation strategy to improve fidelity to evidence-based best practices for prediabetes.
Supplementary Material
Supplemental Digital Content 1.pdf: Description of patient characteristics among those attributed to a primary care clinic with a provider with either an Internal Medicine, Family Medicine, or Geriatric specialty.
Acknowledgements:
Research reported in this publication was supported by the Intermountain Healthcare and the National Center for Advancing Translational Sciences for the National Institutes of Health under Award Numbers 5UL1TR002538 and KL2TR002539. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest: Dr. Kimberly D. Brunisholz received funding support for this research study through support by the Intermountain Healthcare and the National Center for Advancing Translational Sciences for the National Institutes of Health under Award Numbers 5UL1TR002538 and KL2TR002539. Dr. Molly B. Conroy, Thomas Belnap, Dr. Elizabeth A. Joy, and Dr. Raj Srivastava did not receive any funding for the work presented in this manuscript. The study sponsor did not have any role in the study design; collection; analysis; and interpretation of data; writing the report; and/or the decision to submit the report for publication.
Biographies
Biosketches:
Kimberly D. Brunisholz (PhD, MST) serves as a Senior Research Scientist within the Healthcare Delivery Institute at Intermountain Healthcare. She is affiliated with the Division of Epidemiology, at the University of Utah through an adjunct faculty position. She is a member of the Prediabetes Development team at Intermountain Healthcare in Murray, Utah.
Molly B. Conroy (MD, MPH) serves as the John Rex and Alice C. Winder Presidential Endowed Chair in Internal Medicine and the Division Chief of General Internal Medicine (GIM) with the School of Medicine at the University of Utah in Salt Lake City, Utah.
Thomas W. Belnap (MS) is a data analytics manager and holds positions at Intermountain Healthcare within the Healthcare Delivery Institute and Intermountain Research.
Elizabeth A. Joy (MD, MPH) is the Medical Director of the Office of Health Promotion and Wellness and is a member of the Prediabetes Development team at Intermountain Healthcare in Salt Lake City, Utah. She holds an adjunct faculty position through the Department of Family and Preventive Medicine at the University Utah and currently serves as the President-elect of the American College of Sports Medicine and the President of the Female Athlete Triad Coalition.
Raj Srivastava (MD, FRCP(C), MPH) is the Assistant Vice President of Research at Intermountain Healthcare. He co-directs the Intermountain Healthcare Delivery Institute where he oversees the Care Delivery Science team and serves as Medical Director of the Office of Research in Murray, Utah. In addition, Dr. Srivastava is a Professor of Pediatrics at the University of Utah in the Division of Inpatient Medicine and is a practicing hospitalist at Primary Children’s Hospital in Salt Lake City.
References
- 1.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England journal of medicine. February 7 2002;346(6):393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diabetes Prevention Program Research G. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. The lancet. Diabetes & endocrinology. November 2015;3(11):866–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benoit SR, Hora I, Albright AL, Gregg EW. New directions in incidence and prevalence of diagnosed diabetes in the USA. BMJ open diabetes research & care. 2019;7(1):e000657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siu AL, Force USPST. Screening for Abnormal Blood Glucose and Type 2 Diabetes Mellitus: U.S. Preventive Services Task Force Recommendation Statement. Annals of internal medicine. December 1 2015;163(11):861–868. [DOI] [PubMed] [Google Scholar]
- 5.O’Brien MJ, Lee JY, Carnethon MR, et al. Detecting Dysglycemia Using the 2015 United States Preventive Services Task Force Screening Criteria: A Cohort Analysis of Community Health Center Patients. PLoS Med. July 2016;13(7):e1002074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dall TM, Storm MV, Semilla AP, Wintfeld N, O’Grady M, Narayan KM. Value of lifestyle intervention to prevent diabetes and sequelae. American journal of preventive medicine. March 2015;48(3):271–280. [DOI] [PubMed] [Google Scholar]
- 7.Selph S, Dana T, Blazina I, Bougatsos C, Patel H, Chou R. Screening for type 2 diabetes mellitus: a systematic review for the U.S. Preventive Services Task Force. Annals of internal medicine. June 2 2015;162(11):765–776. [DOI] [PubMed] [Google Scholar]
- 8.Narayan KM, Weber MB. Screening for hyperglycemia: the gateway to diabetes prevention and management for all Americans. Annals of internal medicine. June 2 2015;162(11):795–796. [DOI] [PubMed] [Google Scholar]
- 9.Tseng E, Greer RC, O’Rourke P, et al. Survey of primary care providers’ knowledge of screening for, diagnosing and managing prediabetes. Journal of general internal medicine. November 2017;32(11):1172–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Briggs Early K, Stanley K. Position of the Academy of Nutrition and Dietetics: The Role of Medical Nutrition Therapy and Registered Dietitian Nutritionists in the Prevention and Treatment of Prediabetes and Type 2 Diabetes. Journal of the Academy of Nutrition and Dietetics. February 2018;118(2):343–353. [DOI] [PubMed] [Google Scholar]
- 11.Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. The New England journal of medicine. May 3 2001;344(18):1343–1350. [DOI] [PubMed] [Google Scholar]
- 12.Brunisholz KD, Joy EA, Hashibe M, et al. Stepping Back to Move Forward: Evaluating the Effectiveness of a Diabetes Prevention Program Within a Large Integrated Healthcare Delivery System. Journal for healthcare quality : official publication of the National Association for Healthcare Quality. Sep-Oct 2017;39(5):278–293. [DOI] [PubMed] [Google Scholar]
- 13.Brunisholz KD, Kim J, Savitz LA, et al. A Formative Evaluation of a Diabetes Prevention Program Using the RE-AIM Framework in a Learning Health Care System, Utah, 2013-2015. Preventing chronic disease. July 20 2017;14:E58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sheehy AM, Flood GE, Tuan WJ, Liou JI, Coursin DB, Smith MA. Analysis of guidelines for screening diabetes mellitus in an ambulatory population. Mayo Clinic proceedings. January 2010;85(1):27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bullard KM, Ali MK, Imperatore G, et al. Receipt of Glucose Testing and Performance of Two US Diabetes Screening Guidelines, 2007-2012. PloS one. 2015;10(4):e0125249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Venkataramani M, Pollack CE, Yeh HC, Maruthur NM. Prevalence and Correlates of Diabetes Prevention Program Referral and Participation. American journal of preventive medicine. March 2019;56(3):452–457. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1.pdf: Description of patient characteristics among those attributed to a primary care clinic with a provider with either an Internal Medicine, Family Medicine, or Geriatric specialty.


