Abstract
Objective:
To compare the effectiveness of non-pharmacological interventions on depressive symptoms in people after stroke.
Data Sources:
A literature search was performed through the following databases from January 2000 to August 2018: MEDLINE; CINAHL Plus; Scopus; Academic Search Complete; Cochrane Central Register of Controlled Trials; Scopus; and Library, Information Science and Technology Abstracts. Search terms included depression, stroke, non-pharmacologic, and intervention.
Study Selection:
We included randomized controlled trials comparing non-pharmacological interventions to control conditions for depressive symptoms in people following stroke. Of 1703 identified articles, 22 trials were included in narrative synthesis, of which 13 were eligible for meta-analysis. All trials were included once their outcome assessments were blinded.
Data Extraction:
Two reviewers were involved in the data extraction process. Characteristics of participants, interventions, and methods and results (means and standard deviations) were extracted from all included trials.
Data Synthesis:
Thirteen non-pharmacological interventions were categorized into four types: complementary and alternative therapy (five trials, 228 participants), exercise (four trials, 263 participants), psychosocial therapy (two trials, 216 participants), and multifactorial therapy (two trials, 358 participants). Overall beneficial effects of non-pharmacological interventions on depressive symptoms were found both post-intervention (effect size [ES] = −0.24, 95% confidence Interval [CI]: −0.37 to −0.11, p < 0.05) and at follow-up (ES = −0.22, CI: −0.36 to −0.07, p < 0.05). We found individual beneficial effects for complementary and alternative therapy (ES = −0.29, CI: −0.55 to −0.02, p < 0.05) and psychosocial therapy (ES = − 0.33, CI: −0.60 to −0.06, p < 0.05) post-intervention.
Conclusions:
Non-pharmacological interventions can be effective in addressing depressive symptoms in people after stroke. Complementary and alternative therapy and psychosocial therapy appear to be promising strategies for improving post-stroke depressive symptoms. Future studies are required to identify a personalized approach for people with specific conditions such as cognitive impairment.
Keywords: Non-pharmacological interventions, Stroke, Depression, Meta-analysis, Neuropsychiatry, Psychosocial Therapy
Introduction
Stroke is the most common cause of complex disability.1 Neuropsychiatric symptoms are often associated with stroke; among them, depression is the most prevalent. Prevalence of major depression in people after stroke is 25% at the acute stage and 31% at 3 months post-stroke2; however, few individuals receive effective management for depressive symptoms post-stroke.3 Unaddressed depressive symptoms can lead to devastating effects; not only do they stunt progress in therapy, but they can also negatively affect stroke outcomes, with increased morbidity, mortality, and poorer functional recovery.4
Previous studies have been conducted to identify appropriate interventions for post-stroke depression; two common types are pharmacological interventions and non-pharmacological interventions (NPIs).5–9 Three meta-analyses have been conducted to provide synthesized evidence on the effectiveness of pharmacological interventions for depressive symptoms following stroke, but results were mixed.5,6,9 Chen et al. demonstrated the efficacy of antidepressants in reducing depressive symptoms in this population.5 Hackett et al. also provided evidence for antidepressants but reported only small effects on the amelioration of depressive symptoms.6 Conversely, a recent review performed a network meta-analysis of nine types of antidepressants to determine their efficacy, acceptability, and tolerability. Although three antidepressants, doxepin, paroxetine, and nortriptyline, were more effective than a placebo, the review noted that the extent to which symptom reduction of these antidepressants was clinically meaningful is uncertain because diverse results were found in their acceptability and tolerability.9 With mixed conclusions, the effectiveness of pharmacological interventions for post-stroke depressive symptoms has not yet been determined. Moreover, it is recognized that the application of pharmacological interventions might be further limited due to adverse effects, long response times, potential medication adverse events, and low adherence rates.8,10,11 For these reasons, an alternative, or addition, to pharmaceutical options is essential to ensure effective management of depressive symptoms after stroke.
NPIs, which are defined as science-based and non-invasive interventions on human health, may provide an alternative to ameliorate depressive symptoms. Several NPIs for depression exist, such as complementary and alternative therapy (CAT), exercise, psychosocial therapy, non-invasive cranial stimulation, and multifactorial behavioral treatment.12 Currently, an abundance of evidence supports the effectiveness of NPIs for depression in other clinical populations.10,13 Three reviews have identified several NPIs for post-stroke depression and have qualitatively provided evidence.8,11,14 In particular, the latest review indicated that therapies demonstrating a reduction in depressive symptoms include problem-solving therapy, acupuncture, repetitive transcranial magnetic stimulation, music therapy, exercise, light therapy, motivational interviewing, and robotic-assisted therapy.8 However, none of these reviews quantitatively demonstrated the effectiveness of different types of NPIs. Therefore, to address this research gap, this study aimed to conduct a meta-analysis to synthesize and compare the available evidence regarding the effectiveness of various NPIs for treating depression in people following stroke.
Methods
Search Strategy
The search strategy utilized in this review consisted of three parts. First, an initial search of MEDLINE and CINAHL was performed to compile a comprehensive list of NPIs for post-stroke individuals with depressive symptoms. Keywords used in the initial search were depres*, stroke*, interven*, and nonpharmacologic*. Next, a second search using all identified interventions was performed across the following major online databases: Academic Search Complete; CINAHL Plus; MEDLINE; Cochrane Central Register of Controlled Trials; Scopus; and Library, Information Science and Technology Abstracts. Trials published between January 2000 and August 2018 were considered for inclusion; this date range reflects findings from an initial search in MEDLINE and CINAHL, which showed no relevant trials before 2000. The search strategy for the second search included a combination of population, intervention, and outcome keywords and Medical Subject Heading (MeSH) terms (Appendix A). Last, the reference lists of all identified trials were used to identify any additional trials that might have been missed in database searching. All search processes were performed with the assistance of an academic librarian. This review followed the procedures outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidleines15,16 (Figure 1). The entire procedure of selecting included trials was independently carried out by two reviewers (YL & BC), and any discrepancies between the two reviewers were resolved by a third reviewer (AW).
Figure 1.
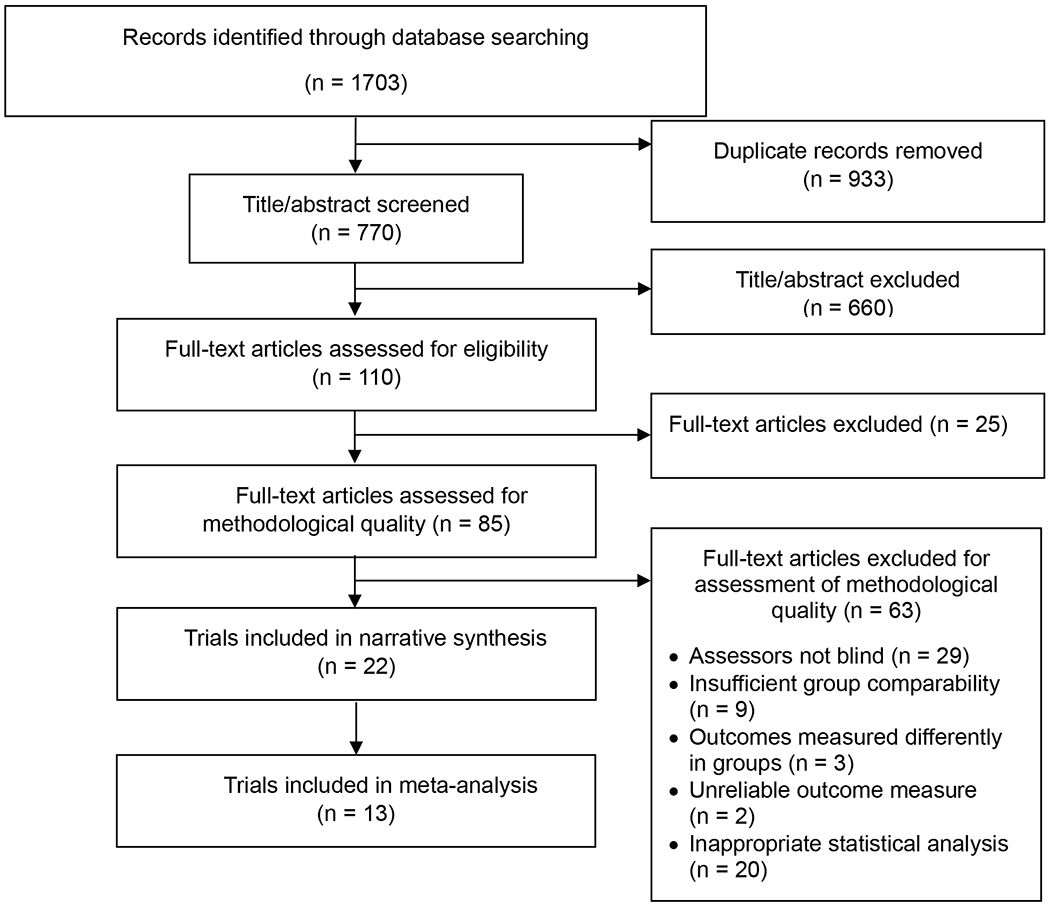
Flowchart of selection process
Study Selection
The search was restricted to randomized controlled trials (RCTs) written in English and published in peer-reviewed journals. The PICOS (Participants, Interventions, Comparisons, Outcomes, Study Designs) checklist was used to identify the inclusion criteria in this review.17
Participants (P):
This review included trials if they targeted persons with stroke (ischemic and hemorrhagic), regardless of comorbidities and any previous treatments, but excluded those with manic or psychotic episodes/symptoms in order to reduce biases associated with non-target symptoms. Participants were included whether or not they received pharmacological interventions (any dosage or duration) for depression or other illnesses.
Interventions (I) and controls (C):
This review considered trials that compared the effects of NPIs for post-stroke individuals with depressive symptoms (eg, music therapy, massage therapy, behavioral therapy, or physical exercise with any frequency, intensity, or duration) to control conditions, such as usual treatment.
Outcomes (O):
The primary outcome of this review was depressive symptoms, measured by any validated depression scale.
Study designs (S):
This review considered any RCT with a pre-post design, meaning that outcomes were measured at pre-intervention, post-intervention, and follow-up.
Methodological Quality
The trials selected for potential inclusion were assessed for methodological rigor prior to inclusion by two reviewers using standardized critical appraisal instruments from the Joanna Briggs Institute Meta-Analysis of Statistics Assessment and Review Instrument (JBI-MAStARI).18 JBI-MAStARI is an analytic module in the JBI System for the Unified Management, Assessment and Review of Information package. Our reviewers established minimal requirements to qualify a study for inclusion in the review and progression to data extraction; inclusion required “yes” answers to five mandatory questions on the JBI-MAStARI standardized critical appraisal instrument. The five mandatory questions were Q5, Q6, Q8, Q9, and Q10. These five mandatory questions were chosen to avoid potential detection bias (Q5, Q8, Q9), decrease selection bias (Q6), and ensure the use of appropriate statistical analysis (Q10). More detailed definitions of each question are provided in Appendix B. Any disagreements between the reviewers were resolved through discussion with the third reviewer.
Data Extraction
Data were extracted from the included trials using the standardized data extraction tool from JBI-MAStARI.18 Extracted data included specific details about interventions (eg, names, intensity, contents), participants (eg, age, stroke type), study methods, and significant outcomes. In addition, the number of participants and the means and standard deviations (SDs) of results were abstracted from all included trials to calculate effect sizes for meta-analysis. If the study reported insufficient data, the corresponding author was contacted to obtain further details. Details of the eligible trials were extracted and summarized independently by two reviewers, and any discrepancies in data abstraction between the two reviewers were resolved via discussion with the third reviewer.
Meta-Analysis and Data Synthesis
Statistical analysis:
We visually inspected the potential of publication bias by a funnel plot, examining asymmetry of the graph. For the meta-analysis, we calculated effect sizes and statistical heterogeneity using Review Manager (RevMan) 5.3 software (Nordic Cochrane Centre, Cochrane Collaboration, Copenhagen 2014). We computed standardized mean differences (SMDs) based on between-group comparisons of pre-post (or follow-up) change in scores and pre-test SDs.19–21 We used pre-test SD because it does not account for the effect of interventions across different outcome measures, regardless of the experimental design. In other words, this approach is a more consistent estimate of variance between groups.21 If the study reported the pre- and post-test means in each group, we obtained the changes by subtracting the post-test outcome from the pre-test outcome within each group. Where the pre-test SD was not available, we used the change in SDs.22 In cases in which the study only reported standard errors (SEs), the SD was calculated using the following formula23: .
Calculation of effect size:
To obtain effect sizes, SMDs and 95% confidence intervals (CIs) were estimated using Cohen’s d test in which the pooled effect estimate (ie, depressive symptoms) was assessed using various measurements. The effect sizes of 0.2, 0.5, and 0.8 were classified as small, medium, and large, respectively.24 The results were interpreted as statistically significant if the 95% CI did not contain zero. A negative effect size indicated that NPIs had better effects on outcomes than control conditions.
Heterogeneity test:
We applied the random effect model in all calculations of effect size because all included trials had variations in study design, intervention methods, and population characteristics. The Chi-square test (Cochran’s Q) and I2 statistics were used to identify heterogeneity among the included trials. Heterogeneity was present if the Q value was significant (p < 0.10). I2 statistics represent the degree of heterogeneity, which provides the amount of variance among the included trials, considered low at 30%, moderate at 50%, and substantial at 75%.22
No informed consent and ethical approval were obtained because this study was a review that did not contain any research procedures with human participants performed by any of our investigators.
Results
Study Characteristics
Study selection:
A total of 1703 potentially relevant articles were identified through the search. Of those, 933 were duplicates. Of the remaining 770 articles, 660 were excluded after title and abstract assessment. From the 110 remaining articles, 25 were excluded, as full-text analysis revealed that they did not meet the inclusion criteria. After assessing the methodological quality of the remaining 85 trials, 63 trials were excluded because they did not meet the five mandatory questions of the JBI-MAStARI: Q5 (n = 29), Q6 (n = 9), Q8 (n = 3), Q9 (n = 2), and Q10 (n = 20). Finally, 22 original trials were included in this review. Figure 1 illustrates this process.
Participants:
Our search identified 22 trials. The total sample size of all trials was 2090, ranging from 24–411 per study with a median of 61. All included trials demonstrated similar between-group baseline characteristics, including baseline depressive outcomes. Participants included in all trials were at least 18 years old. The common exclusion criteria were: presence of communication problems including aphasia, cognitive impairment that was often determined using Mini-Mental State Examination, and other neurological or psychological illnesses such as dementia or multiple sclerosis. Stroke stage was acute in four trials, subacute in three trials, and chronic in six trials. Other trials reported participants with more than two stages (eg, subacute and chronic stroke, or stroke diagnosed within 6 months). Table 1 shows details of the included trials.
Table 1.
Participant characteristics of the included trials (total number of trials = 22)
| Type of intervention | Author, year | Participants | Total number | Primary inclusion criteria | Primary exclusion criteria |
|---|---|---|---|---|---|
| Complementary and alternative therapy (N = 5) | Lee et al., 2016 | Subacute or chronic stroke | 53 | - More than 4 weeks after stroke - Aged 20 years or older |
- Presence of cognitive impairment - Presence of another central nervous disease or severe neurological or psychiatric symptoms - Taking antipsychotic medication - Communication difficulties |
| Man et al., 2014 | Stroke within 6 months | 43 | - Diagnosed as ischemic or hemorrhagic stroke within 6 months - Aged 35–80 years - Developed significant depressive episode |
- Presence of severe aphasia - Presence of severe cognitive dysfunction - History of psychiatric illness other than depression - Presence of another chronic disorder |
|
| Särkämö et al., 2008 | Acute ischemic middle cerebral artery stroke | 36 | - Acute ischemic middle cerebral artery stroke - Aged 75 years or older |
- Presence of any prior neurological or psychiatric disease - Presence of drug or alcohol abuse - Presence of hearing deficit |
|
| Raglio et al., 2017 | Post-acute stroke | 38 | - Aged 40 years or older | - Presence of cognitive dysfunction - Presence of aphasia or amusia - Presence of previous neurological or psychiatric diseases |
|
| Menghan et al., 2017 | Stroke within 6 months | 58 | - Cerebral infarction attacks for the first time and the course is less than 6 months - Aged 40–80 years |
- Has been treated by other antidepressant treatment within 2 weeks - Presence of a cognitive disorder or obvious hypophrenia and severe aphasia - Personal history of positive psychonosema, including depression, in medical history |
|
| Exercise (N = 6) | Lai et al., 2006 | Subacute stroke | 93 | - Stroke within 30–150 days - Mild-to-moderate stroke deficits |
- Presence of cognitive dysfunction - Presence of serious cardiac conditions, oxygen dependence - Presence of other serious organ system disease |
| Mead et al., 2007 | Stroke survivors | 66 | - Independently ambulatory | - Presence of dysphasia or confusion severe enough to prevent informed consent - Presence of medical contraindications to exercise training |
|
| Zedlitz et al., 2012 | 4 months after stroke | 83 | - Sustained a stroke > 4 months before recruitment - Reported severe fatigue - Aged 18–70 years |
- Presence of severe cognitive deficits - Presence of severe comorbidity such as cardiac disease, pulmonary disease, or depression |
|
| Vahlberg et al., 2017 | Chronic stroke | 57 | - Verified stroke of any type within the previous 1–3 years | - Presence of cognitive deficits - Presence of dementia diagnosis, severe communication problems |
|
| Rowe et al., 2017 | Chronic stroke | 30 | - History of unilateral stroke at least 6 months prior - Aged 18–80 years |
- None | |
| Topcuoglu et al., 2015 | Subacute stroke | 40 | - A diagnosis with hemiplegia associated with a cerebrovascular event that took place at least 1 month and at most 6 months prior to the study | - Presence of severe aphasia, serious mental disorder, a history of fracture | |
| Psychosocial therapy (N = 6) | Mitchell et al., 2009 | Stroke within 6 months | 101 | - Within 4 months of an ischemic stroke - Screened positive for depressive symptoms and whose diagnosis of clinical depression was verified by a diagnostic interview |
- None |
| Watkins et al., 2009 | Acute stroke | 411 | - Aged 18 years or older | - Presence of severe cognitive or communication problems preventing participation in interviews | |
| Aben et al., 2013 | Chronic stroke | 153 | - 8 months or more elapsed since first and only stroke - Aged 18–80 years - Reported subjective memory complaints |
- Presence of progressive neurological disorders such as dementia or multiple sclerosis - Presence of alcohol or drug abuse - Presence of subdural hematomas or subarachnoid hemorrhages |
|
| Visser et al., 2016 | Outpatient stroke | 166 | - Had a stroke (including subarachnoid hemorrhage) - Aged 18–75 years - Received outpatient stroke rehabilitation treatment |
- Presence of progressive neurological disorder, subdural hematomas, moderate or severe aphasia, or partook in excessive drinking or drug abuse | |
| Kirkness et al., 2017 | Stroke within 4 months | 63 | - Scored ≥ 11 on the 30-item Geriatric Depression Scale | - None | |
| Kootker et al., 2017 | Stroke at least 3 months earlier | 61 | - Sustained any type of clinically confirmed stroke at least 3 months earlier - Score > 7 on the Hospital Anxiety Depression Scale depression subscale - Aged 18 years and older |
- Presence of pre-stroke major depression requiring psychiatric care - Presence of moderate or severe cognitive impairments - Presence of premorbid disability as reflected in a Barthel Index score < 19 - Presence of post-stroke major depression requiring medication |
|
| Multifactorial therapy (N = 3) | Ihle-Hansen et al., 2014 | Acute stroke | 172 | - Survived the acute phase (days 7–10) | - Presence of subarachnoid hemorrhage, known cognitive decline, previous stroke, or transient ischemic attack |
| Rochette et al., 2013 | Mild stroke | 186 | - Sustained a first mild stroke - Ability to understand basic instructions and express basic needs |
- Presence of moderate or severe cognitive deficits | |
| Wong et al., 2015 | Outpatient stroke | 108 | - Ability to communicate - Cerebral hemorrhage - Cerebral infarction - Slight-to-moderate neurological deficits - Slight-to-moderate level of disability |
- Presence of cognitive dysfunction - Presence of unstable comorbidity requiring active treatment |
|
| Cranial stimulation (N = 2) | Valiengo et al., 2017 | Stroke within 5 years | 48 | - Verified stroke of any type within the previous 1–3 years | - Presence of cognitive deficits, dementia diagnosis, severe communication problems |
| Gu et al., 2017 | Chronic stroke | 24 | - History of stroke - Admitted ≥ 6 months after stroke onset - Aged 21–80 years - Presence of depression |
- Presence of serious medical complications such as pneumonia or cardiac problems - Presence of depression or medication history of antidepressants before stroke onset - Presence of severe cognitive dysfunction or aphasia |
Interventions:
Table 2 shows detailed descriptions of the NPIs used in the included studies. NPIs were classified into five types: CAT (n = 5), exercise (n = 6), psychosocial therapy (n = 6), multifactorial therapy (n = 3), and cranial stimulation (n = 2) (Table 2). In this review, CAT was defined as any intervention that is not part of standard medical care that is practiced by health professionals. In particular, interventions that did not involve the other four major types of intervention were categorized into CAT. Five trials tested the effects of CAT, three of which used acupuncture, and two of which applied music therapy. The intervention intensity in this type varied from 3- to 12-week periods. Among these five trials, the results of four favored the intervention over the control condition.
Table 2.
Intervention and methods characteristics of the included trials (total number of trials = 22)
| Type of intervention | Author, year | Intervention | Control | Medication | Intensity | Depression measure | Results | Included in meta-analysis |
|---|---|---|---|---|---|---|---|---|
| Complementary and alternative therapy (N = 5) | Lee et al., 2016 | Acupuncture | Sham group | No antipsychotic medication | 3d/wk*3wk | K-BDI | Favoring intervention | Yes |
| Man et al., 2014 | Direct cranial electro-acupuncture stimulation | Body electro-acupuncture | SSRIs | 3d/wk*4wk | HRSD | Favoring intervention | Yes | |
| Särkämö et al., 2008 | Music listening | Language listening | 40.7% of participants received antidepressants (citalopram or mirtazapine) | 1h/d*2m | POMS | Favoring intervention | Yes | |
| Raglio et al., 2017 | Relational Active Music Therapy (RAMT) | Standard care | No psychotropic medications | 05h/d*20ses weekly | HADS-D | Favoring intervention | Yes | |
| Menghan et al., 2017 | Tioshen Kaiqiao acupuncture | Meds+Body acupuncture | No antidepressants | 0.3–0.5h/d, 3d/wk*12wk | HRSD | No difference | Yes | |
| Exercise (N = 6) | Lai et al., 2006 | Strength, balance, endurance, and upper extremity function | Usual care | 24.5% of Participants received antidepressants | 3d/wk*12wk for 36 ses (3months) | GDS | Favoring intervention | Yes |
| Mead et al., 2007 | Mixed endurance & resistance training | Relaxation attention control | Not reported | 1.25h/d, 3d/wk*12wk | HADS-D | No difference | No (insufficient data) | |
| Zedlitz et al., 2012 | Walking on a treadmill, strength training, homework assignments | Cognitive therapy | Not reported | 12wk | HADS-D | Favoring intervention | Yes | |
| Vahlberg et al., 2017 | Progressive resistance and balance | Usual care | Not reported | 1h and 15min/d 2d/wk*12wk | GDS-20 | No difference | Yes | |
| Rowe et al., 2017 | Robotic assistance (high assistance) | Robotic assistance (low assistance) | Not reported | 1h/d, 3d/wk*12wk | GDS | No difference | Yes | |
| Topcuoglu et al., 2015 | Upper extremity aerobic exercise | Standard treatment | Not reported | 0.5h/d, 5d/wk*16wk | BDI | Favoring intervention | No (insufficient data) | |
| Psychosocial therapy (N = 6) | Mitchell et al., 2009 | Psychosocial behavioral intervention | Usual care | Received antidepressants | 9 ses (8wk) | HRSD | Favoring intervention | No (publication bias) |
| Watkins et al., 2009 | Motivational interviewing | Usual care | Not reported | 0.5–1h/ses, 4ses | GHQ-28, Yale | Favoring intervention | No (insufficient data) | |
| Aben et al., 2013 | Memory self-efficacy training program | Attention control | Not reported | 1h/ses, 2d/wk, 9ses | CES-D | No difference | Yes | |
| Visser et al., 2016 | Problem-solving therapy | Standard rehabilitation | 19.3% of Participants received antidepressants | 1.5h/wk, 8ses | CES-D | No difference | No (publication bias) | |
| Kirkness et al., 2017 | Brief psychosocial intervention | Usual care | 44.4% of participants received antidepressants | Tel:10–80min, In-person: 26–38min | GDS, HRSD | Favoring intervention | Yes | |
| Kootker et al., 2017 | Augmented cognitive behavioral therapy | Usual care | No antidepressants | 13–16ses for 4m | HADS-D | No difference | No (insufficient data) | |
| Multifactorial therapy (N = 3) | Ihle-Hansen et al., 2014 | Multifactorial risk factor intervention program | Usual care | Not reported | Unclear | HADS-D | Favoring intervention | Yes |
| Rochette et al., 2013 | We Call: a multimodal (telephone, Internet, paper) support intervention | You Call: standard care whereby contact with medical staff is initiated by patients | Not reported | Unclear | BDI | No difference | Yes | |
| Wong et al., 2015 | Holistic care Interventions administered by a multidisciplinary team | Physical training program | Not reported | 4 wk | CES-D | Favoring intervention | No (insufficient data) | |
| Cranial stimulation (N = 2) | Valiengo et al., 2017 | Transcranial direct current stimulation | Sham control | No antidepressants | 12–30min/ses for 6 wk | HRSD | Favoring intervention | No (insufficient data) |
| Gu et al., 2017 | Repetitive transcranial magnetic stimulation | Sham control | No antidepressants | 70mm/d 5d/wk*2wk | BDI | Favoring intervention | No (publication bias) |
(K-)BDI: (Korean version) of the Beck Depression Inventory, HRSD: The 17-item Hamilton Rating Scale for Depression, POMS: The Profile of Mood States, HADS-D: The Hospital Anxiety and Depression Scale-Depression Subscore, GDS: The 15-item Geriatric Depression Scale, GHQ-28: 28-Item General Health Questionnaire, Yale: Yale Depression Screen, CES-D: The Center of Epidemiological Studies–Depression Scale, MES: The Bech–Rafaelsen Melancholia Scale
Exercise refers to any physical activity or movement performed to increase physical fitness, which can also be assisted by machines or other devices. Six trials tested the effects of exercise interventions. These six trials involved any type of exercise, such as strength, balance, endurance, resistance, aerobic, walking, and/or robotic assistance. Five of six exercise trials carried out the intervention for 12-week periods, while one trial carried out the intervention for 16-week periods. Half of the included exercise trials reported effects favoring the intervention group, while others showed no significant difference between the two groups.
Psychosocial therapy refers to any intervention that emphasizes psychological, behavioral, or social factors rather than biological factors. Six trials tested the effects of different types of psychosocial therapy, including psychosocial behavioral intervention, motivational interviewing, memory self-efficacy training, problem-solving therapy, brief psychosocial intervention, and augmented cognitive behavioral therapy (CBT). Detailed descriptions for each type of therapy are illustrated in Appendix C. Intensities varied, with a range of 4–24 sessions. Among these six interventions, the psychosocial behavioral intervention, motivational interviewing, and brief psychosocial intervention showed beneficial effects on post-stroke depression, while memory self-efficacy, problem-solving therapy, and augmented CBT showed no significant group difference.
Three trials tested the effects of multifactorial therapy, which refers to any intervention with more than two main categories—including biological, physical, and psychological—supported by a multidisciplinary team, or a trial in which multiple components or tools of intervention such as pen-and-paper, Internet, and phone are provided to participants. Two trials of this type did not report the exact intervention period, while one trial was implemented for 4 weeks. Two of three trials reported effects favoring interventions of this type.
Finally, cranial stimulation, defined as an intervention that stimulates nerve cells in the brain, included two trials. One study used transcranial direct-current stimulation, and the other used repetitive transcranial magnetic stimulation. Although their intensities differed, both trials favored the intervention over the control condition.
Controls:
Nine trials compared an intervention to an active control, such as non-invasive acupuncture, body acupuncture, language listening, relaxation attention control, cognitive therapy, robotic assistance (low assistance), attention control, general discussion, or a physical training program. Thirteen trials compared an intervention to a non-active control, such as usual care, standard treatment, or sham group (Table 2).
Outcome:
The outcome was depressive symptoms. To measure depressive symptoms, nine measures were used in the included trials, with the most common being the 17-item Hamilton Rating Scale for Depression (Table 2).
Methodological Quality
Two independent reviewers assessed 85 trials. We excluded 63 trials after thorough review and assessment of the methodological quality. Methodological quality was measured using the JBI-MAStARI, with a total range of possible scores from 0 ‒ 10. Appendix B illustrates the results of the methodological quality assessment of the included 22 trials. The mean score was 8.27 (SD 1.16), with a range of 7–10 points. In appraising methodological quality, information related to the blinding of participants (Q2 = 36%) and the allocator (Q3 = 45%) was often unclear or not addressed. Information related to the comparability of groups, outcomes, and use of appropriate statistical analysis was clearly found in all included trials. Three trials25–27 met all 10 items in the methodological quality assessment.
Meta-Analysis
Of 22 included trials, we excluded three trials indicating publication bias and six trials reporting insufficient data. Reasons for insufficient data were: (1) authors of three trials did not respond to emails for the requested information,28–30 (2) authors of one trial refused to provide data,31 (3) authors from one trial did not keep the data,26 and (4) authors of one trial did not have the requested information.32 Thus, 13 trials were included in the final meta-analysis. These trials were grouped into four types: CAT (n = 5), exercise (n = 4), psychosocial therapy (n = 2), and multifactorial therapy (n = 2) (Table 2).
Heterogeneity:
Overall, our findings indicated low heterogeneity among the included trials (p > 0.1). No variance (0%) was found for depressive symptoms among all included studies, both at pre- and post-tests. Due to low heterogeneity, we did not run meta-regression analyses to understand the cause of heterogeneity.33
Publication bias:
To assess any potential publication bias, we constructed a funnel plot for the primary outcome (ie, depressive symptoms), and we visually inspected the symmetry of the plot. In the plot, three notable outliers were observed,27,34,35 which caused asymmetry of the funnel plot (Appendix D). We excluded these trials from the final meta-analysis. The plot appeared to be symmetrical after excluding these trials.
Depressive symptoms post-intervention:
Although depressive symptoms were measured in all 13 trials, only 12 trials were included in the comparison of post-intervention effects of NPIs to control conditions; one trial provided the follow-up data but no immediate post-intervention data for calculation of the effect size.36 These 12 trials consisted of four types of NPI: (1) CAT (five trials, 228 participants), (2) exercise (four trials, 263 participants), (3) psychosocial therapy (two trials, 216 participants), and (4) multifactorial therapy (one trial, 186 participants). Overall results, combining the outcomes of all included NPIs, showed a significant effect size on depressive symptoms post-intervention (SMD: −0.24; 95% CI: −0.37 to −0.11; p = 0.0004; I2 = 0%), which can be interpreted as a small effect size. In particular, beneficial effects favoring CAT (SMD: −0.29; 95% CI: −0.55 to −0.02; p = 0.03; I2 = 0%) and psychosocial therapy (SMD: − 0.33; 95% CI: −0.60 to −0.06; p < 0.02; I2 = 42%) were observed, which can be interpreted as a small effect. Exercise and multifactorial therapy did not show any beneficial effects (p > .05) (Figure 2).
Figure 2.
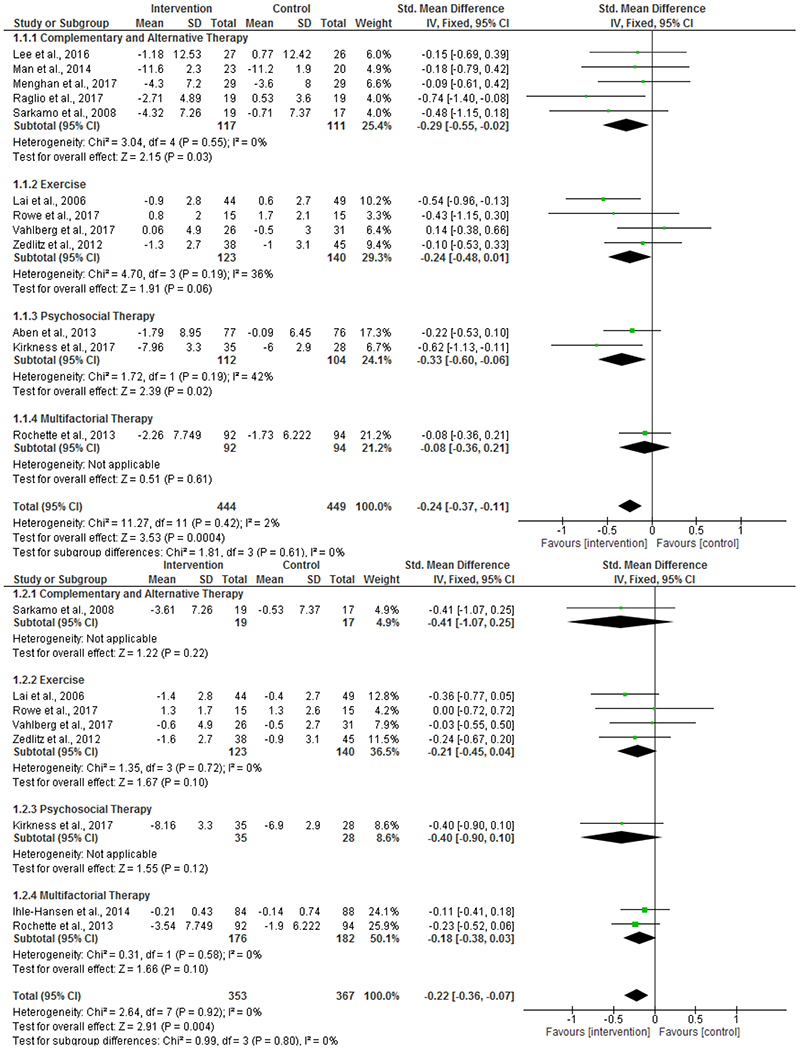
Forest plot comparing intervention and control group on depressive symptoms at post-intervention (upper) and follow-up (lower)
In order to investigate individual effects of acupuncture and music therapy on decreased depressive symptoms post-intervention, we divided CAT into two types: acupuncture (three trials, 154 participants) and music therapy (two trials, 74 participants). The effect size was statistically significant in favor of music therapy (SMD: −0.61; 95% CI: −0.18 to −0.14; p = 0.01; I2 = 0%), which can be interpreted as a medium effect, while acupuncture showed no significant effect (Appendix E).
Depressive symptoms at follow-up:
Among the 13 trials, eight trials were included to compare the effect of NPIs to control conditions at follow-up. Follow-up periods varied from 1 month to 12 months post-intervention. Overall results showed a significant but small effect size on depressive symptoms at follow-up (SMD: −0.22; 95% CI: −0.36 to −0.07; p = 0.004; I2 = 0%) (Figure 2). However, there were no significant SMDs when comparing CAT, exercise, psychosocial therapy, and multifactorial therapy to control conditions (p > .05).
Discussion
This review explored the effectiveness of NPIs on depressive symptoms among people following stroke. Twenty-two trials were identified to meet the inclusion criteria of this review through the literature search. Interventions in the included trials were classified into five different types, consisting of CAT, exercise, psychosocial therapy, multifactorial therapy, and cranial stimulation. Our findings found small effects of NPIs on depressive symptoms at both post-intervention (SMD = −0.24, p < 0.05) and follow-up (SMD = −0.22, p < 0.05), with individual beneficial effects for CAT (SMD = −0.29, p < 0.05) and psychosocial therapy (SMD = −0.33, p < 0.05) at post-intervention. The sub-group analysis of CAT further showed the beneficial effect of music therapy (SMD: −0.61, p = 0.01) but not of acupuncture on depressive symptoms. These identified interventions appear to be similar to interventions described in previous systematic reviews.8,11,14 Yet, to the best of our knowledge, none of the previous reviews have applied meta-analyses to pool information on different intervention types; this is the first meta-analysis study quantifying the effectiveness of NPIs and comparing the impact of each intervention type on depressive symptoms after stroke.
Overall, our results showed beneficial effects for NPIs in treating depressive symptoms at both post-intervention and follow-up periods. Our study is consistent with previous stroke-specific reviews that have qualitatively supported the effect of NPIs in reducing the severity of depressive symptoms.8,11,13 Our findings add to the knowledge by providing new evidence that further quantifies the benefit of NPIs on post-stroke depression. Although significantly beneficial effects of NPIs were observed, these effects were small. Small effects are commonly found in reviews examining the effect of behavioral treatments on depression in other adult populations, especially reviews that only include high-quality studies.37,38 We used a standardized critical appraisal instrument to select only trials with methodologically high quality in this review. Thus, Thus, it is not surprising to find a comparable (small) effect size for treating post-stroke depression. The benefits of NPIs are particularly important for post-stroke individuals who experience adverse effects or contraindications to the use of antidepressants.39
Regarding the impact of each intervention type, our findings revealed a small effect of CAT on post-stroke depressive symptoms post-intervention. CAT included acupuncture (n = 3) and music therapy (n = 2) in our meta-analysis. To further investigate the benefit of each therapy, we performed sub-group analysis and found a medium effect for music therapy but not for acupuncture. Previous reviews have shown positive effects of music therapy on depressive symptoms in other populations, such as people with cancer40 and dementia.41 A recent review reported a similar positive effect of music therapy on mood in neurological populations.42 Our findings harmonize these reviews, supporting the use of music therapy to alleviate depressive symptoms after stroke. In this review, two music therapy approaches were included: relational active music therapy (RAMT) 43 and self-directed music listening.44 The RAMT approach was designed on the basis of free interactions between patients and music therapists using rhythmical-melodic instruments (eg, xylophones, glockenspiels, drums, bongos, ethnic percussions) in a non-verbal setting in order to facilitate the expression, modulation, and sharing of patients’ emotions, as well as to promote communication and motor rehabilitation. Self-directed music listening consists of patients listening to their favorite music. Although the two trials appeared to use different music therapy approaches, both trials provided evidence that music therapy activates areas related to emotion, motivation, and cognition. Hence, music therapy can benefit post-stroke individuals by promoting relaxation, pleasant mood, and clear thinking.43,45 Additionally, music therapy was found to have high tolerance and compliance, low cost, and few side effects.46 These converging findings support music therapy as an effective alternative for alleviating depressive symptoms in the stroke population.
More importantly, our findings showed benefits of psychosocial therapy on post-stroke depression. In particular, we found that psychosocial therapy had a small effect on depressive symptoms at post-intervention. These findings are incongruent with two earlier reviews. The first review, conducted in 2000, reported that research on psychosocial therapy for post-stroke depression remains unsophisticated and has methodological limitations to establishment of its effects.47 The second review, conducted in 2008, revealed no effect of psychosocial therapy for the treatment of post-stroke depression.6 The inconsistency between these findings and ours is likely due to the inclusion of different studies for synthesis of the evidence. It is likely that some trials demonstrating the positive impact of psychosocial therapy were published after the release of the two earlier reviews. Aligning with this explanation, our findings concur with results from a recent review performed in 2013.48 This review demonstrated positive effects of psychosocial therapy on depressive symptoms in long-term rehabilitation (more than 1 year) after an acquired brain injury, including stroke and traumatic brain injury.
All converging findings indicate that psychosocial therapy could be a favorable treatment option for depression after acquired brain injury. A recent observational cohort study also echoes the importance of emotional health management for community-dwelling adults with neurological conditions, including stroke, traumatic brain injury, and spinal cord injury.49 Psychosocial functioning can be defined as attitudes and beliefs toward disease, body image, coping with disease, and self-efficacy.50 Psychosocial functioning encompasses multidimensional factors including mood status (eg, anxiety and depression), cognitive behavioral responses (eg, satisfaction, self-efficacy, self-esteem, and locus of control), and social factors (eg, social support).51 In this context, psychosocial therapy can address these multidimensional factors. This review included psychosocial behavioral interventions, motivational interviewing, memory self-efficacy training, problem-solving therapy, brief psychosocial intervention, and CBT. Although evidence clearly supports the role of psychosocial therapy for post-stroke depression, future meta-analyses are needed so that specific theory-based interventions (eg, CBT-based interventions) can be evaluated to test their efficacy.
Our meta-analysis showed that NPIs are beneficial, but overall effect sizes were small. One possible explanation for the small effect is that we included studies involving persons with stroke regardless of having a diagnosis of depression (eg, major depressive disorder) or a certain threshold (eg, clinically significant depressive symptoms). Another reason is that we included all studies with varying types of control conditions, including both active and non-active controls, possibly lessening the effect size estimates. It is possible that NPIs may have a small effect size per se, as small effect sizes are also reported in other psychological interventions for depression in general.31,32
In order to identify which treatment options may work best for patients, we conducted sub-group analyses and found that music therapy and psychosocial therapy are two major interventions with small-to-medium effects. However, among these effective NPIs, there is insufficient evidence to determine which patients are likely to benefit from what specific therapies. Also, we recommend that factors such as patient preference be evaluated and taken under consideration for treatment optimization. In addition, our results suggest no significant evidence for exercise and multifactorial interventions. It is important to note that exercise had a possible trend toward significance (CI: −0.48 to 0.01, p = 0.06). Multifactorial therapy only included one study at post-intervention and two studies at follow-up. Therefore, the non-significant effect for multifactorial therapy should be interpreted with great caution.
Our study provides promising results for the use of NPIs for post-stroke depressive symptoms. However, we do not make any recommendation for NPIs as a replacement for medication. Instead, more research is needed to understand whether combinations of pharmacological interventions and NPIs are associated with increased benefits compared to the benefits of any individual intervention. Also, testing to determine which combinations and sequences of treatments are the most effective should be conducted.
Study Limitations
This review provides meaningful evidence in clinical research and practice; however, it has a few limitations resulting from the research design of the included trials. First, the majority of the included trials narrowed their selection criteria to people without communication problems/aphasia, cognitive impairments, and other neurological or psychiatric disorders. Considering the high prevalence of aphasia, cognitive impairments, and/or other comorbid conditions among people after stroke, this narrow selection criteria may cause study bias and limit the generalizability of study findings. Despite this limitation, these criteria might be justifiable for psychosocial therapy, because participants are required to have certain levels of cognitive and communicative function to actively participate in the therapy. Given that cognitive impairments and communication problems are major risk factors for depressive symptoms after stroke,52,53 it is important to design interventions based on the patient profile, with a customized and personalized approach. For example, the use of music therapy may be more relevant to a person with severe cognitive impairments, as music therapy provides a means of nonverbal expression of emotion and inner feelings.54 Additionally, post-stroke depressive symptoms are heterogeneous in their symptom presentation.55 Thus, we suggest that future studies examine which NPIs are more effective for individuals with cognitive impairments, communication problems/aphasia, or those presenting differing depressive symptoms in order to develop interventions based on a customized and personalized approach.
Second, study characteristics, such as the number of intervention sessions, interventions for the control conditions, and the stage of stroke recovery, varied across all included studies. All of these differences can increase heterogeneity, affect estimation of the effect size, and bias study findings. Fortunately, our study showed low heterogeneity across all included trials, suggesting that the impact of these variations was minimal. This review attempted to group many disparate and diverse therapeutic interventions into one category of NPI. This review also compared evidence-based interventions to those that have not been empirically validated, which likely decreases the power of detecting the real effect. We suggest (1) that all potential confounding factors can be analyzed using meta-regression in future studies and (2) inclusion of a larger number of studies. Last, the number of trials used to test the effects of specific intervention types may be inadequate. The interpretation of these study results should be cautious. Future studies should include more trials with structured research designs, if available, to precisely investigate the effectiveness of the intervention.
Conclusions
Depression is a major health problem following stroke that affects about one-third of the stroke population. Management of depressive symptoms includes both pharmacological interventions and NPIs. Our research has shown that NPIs may help address post-stroke depressive symptoms. In particular, psychosocial therapy and music therapy are likely the most promising approaches, as both have demonstrated beneficial effects in ameliorating depressive symptoms for individuals after stroke. Rehabilitation professionals should consider incorporating psychosocial therapy—such as motivational interviewing, problem-solving therapy, or CBT—into the treatment plan to increases skills in the management of emotional problems and, eventually, improve functional independence and quality of life in people after stroke. Music therapy can be considered, in particular, for post-stroke individuals with limited abilities to manage emotional problems due to communication problems/aphasia or cognitive impairments. Future studies are needed to identify personalized interventions for persons experiencing specific vulnerable conditions such as cognitive impairments, communication problems/aphasia, or those presenting differing depressive symptoms after stroke.
Acknowledgements:
The contents of this article do not necessarily represent the policies of the funding agency. We would like to thank Megen Devine at Washington University School of Medicine for her editorial assistance with this manuscript.
Funding:
This study was supported by the National Institute of Child Health and Human Development/National Center for Medical Rehabilitation Research [K01HD095388].
Conflict of interest disclosures:
AW reported grants from the National Institutes of Health (NIH) during the conduct of the study; grants from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR), and Craig H. Neilsen Foundation outside of the submitted work.
JL reported grants from the NIH outside of the submitted work.
GN reported grants from the NIH, Washington University Center for Diabetes Translational Research & Institute for Clinical Translational Science, Alkermes, and Otuska American, Inc. She also serves as a consultant for Sunovion, Alkermes, and Supernus Pharmaceuticals, Patient-Centered Outcomes Research Institute, McKnight Brain Research Foundation, Taylor Family Institute for Innovative Psychiatric Research, Barnes Jewish Foundation, MagStim, Takeda, Johnson & Johnson, and Lundbeck outside of the submitted work; grants and personal fees from Janssen, and personal fees from Jazz Pharmaceuticals outside of the submitted work.
EL reported grants from the NIH, US Food and Drug Administration, Patient-Centered Outcomes Research Institute, McKnight Brain Research Foundation, Taylor Family Institute for Innovative Psychiatric Research, Barnes Jewish Foundation, Takeda, Alkermes, Aptinyx, Johnson & Johnson, and Lundbeck outside of the submitted work; grants and personal fees from Janssen, and personal fees from Jazz Pharmaceuticals outside of the submitted work.
CB reported grants from the National Center for Advancing Translational Sciences and Schultz Family Support Fund outside of the submitted work.
YL, BC, MF, and LC reported the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
No other disclosures were reported.
Appendix A. Medical Subject Headings (MeSH) terms
Academic Search Complete
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*) ) AND ( TI (“non pharmacologic*” OR nonpharmacologic*) OR AB (nonpharmacologic* OR “non pharmacologic*”) ) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“self-worth therapy”) OR AB (“self-worth therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“music therapy”) OR AB (“music therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (yoga) OR AB (yoga)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“psychosocial interventions”) OR AB (“psychosocial interventions”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“problem solving therapy”) OR AB (“problem solving therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* “OR stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“cognitive behavioral therapy”) OR AB (“cognitive behavioral therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (cognitive therapy) OR AB (cognitive therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“interpersonal psychotherapy”) OR AB (“interpersonal psychotherapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“reminiscence therapy”) OR AB (“reminiscence therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“brief psychodynamic therapy”) OR AB (“brief psychodynamic therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“humour therapy”) OR AB (“humour therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (art therapy) OR AB (art therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (psychotherapy) OR AB (psychotherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“physical exercise”) OR AB (“physical exercise”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“hope interventions”) OR AB (“hope interventions”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“friendly visitors”) OR AB (“friendly visitors”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (phototherapy) OR AB (phototherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“light therapy”) OR AB (“light therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“talk therapy”) OR AB (“talk therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“biking therapy”) OR AB (“biking therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (aromatherapy) OR AB (aromatherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (massage) OR AB (massage)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (relaxation therapy) OR AB (relaxation therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“guided imagery”) OR AB (“guided imagery”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“health status acupressure”) OR AB (“health status acupressure”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (acupuncture) OR AB (acupuncture)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“cognitive-behavioural breathlessness”) OR AB (“cognitive-behavioural breathlessness”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (mindfulness) OR AB (mindfulness)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (family therapy)) OR AB (family therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“mindfulness based cognitive therapy”)) OR AB (“mindfulness based cognitive therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“self help”)) OR AB (“self help”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (mind-body therapies)) OR AB (mind-body therapies)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“reiki”)) OR AB (“reiki”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (tai chi)) OR AB (tai chi)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“music-movement therapy”)) OR AB (“music-movement therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (dance therapy)) OR AB (dance therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (psycho-education)) OR AB (psycho-education)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (sleep deprivation)) OR AB (sleep deprivation)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (behavioral activation)) OR AB (behavioral activation)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
CINAHL Plus with Full Text
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*) ) AND ( TI (“non pharmacologic*” OR nonpharmacologic*) OR AB (nonpharmacologic* OR “non pharmacologic*”) ) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“self-worth therapy”) OR AB (“self-worth therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“music therapy”) OR AB (“music therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (yoga) OR AB (yoga)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“psychosocial interventions”) OR AB (“psychosocial interventions”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“problem solving therapy”) OR AB (“problem solving therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* “OR stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“cognitive behavioral therapy”) OR AB (“cognitive behavioral therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (cognitive therapy) OR AB (cognitive therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“interpersonal psychotherapy”) OR AB (“interpersonal psychotherapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“reminiscence therapy”) OR AB (“reminiscence therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“brief psychodynamic therapy”) OR AB (“brief psychodynamic therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“humour therapy”) OR AB (“humour therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (art therapy) OR AB (art therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (psychotherapy) OR AB (psychotherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“physical exercise”) OR AB (“physical exercise”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“hope interventions”) OR AB (“hope interventions”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“friendly visitors”) OR AB (“friendly visitors”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (phototherapy) OR AB (phototherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“light therapy”) OR AB (“light therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“talk therapy”) OR AB (“talk therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“biking therapy”) OR AB (“biking therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (aromatherapy) OR AB (aromatherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (massage) OR AB (massage)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (relaxation therapy) OR AB (relaxation therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“guided imagery”) OR AB (“guided imagery”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“health status acupressure”) OR AB (“health status acupressure”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (acupuncture) OR AB (acupuncture)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“cognitive-behavioural breathlessness”) OR AB (“cognitive-behavioural breathlessness”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (mindfulness) OR AB (mindfulness)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (family therapy)) OR AB (family therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“mindfulness based cognitive therapy”)) OR AB (“mindfulness based cognitive therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“self help”)) OR AB (“self help”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (mind-body therapies)) OR AB (mind-body therapies)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“reiki”)) OR AB (“reiki”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (tai chI)) OR AB (tai chi)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“music-movement therapy”)) OR AB (“music-movement therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (dance therapy)) OR AB (dance therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (psycho-education)) OR AB (psycho-education)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (sleep deprivation)) OR AB (sleep deprivation)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (behavioral activation)) OR AB (behavioral activation)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
MEDLINE with Full Text
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*) ) AND ( TI (“non pharmacologic*” OR nonpharmacologic*) OR AB (nonpharmacologic* OR “non pharmacologic*”) ) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“self-worth therapy”) OR AB (“self-worth therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“music therapy”) OR AB (“music therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (yoga) OR AB (yoga)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“psychosocial interventions”) OR AB (“psychosocial interventions”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“problem solving therapy”) OR AB (“problem solving therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* “OR stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“cognitive behavioral therapy”) OR AB (“cognitive behavioral therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (cognitive therapy) OR AB (cognitive therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“interpersonal psychotherapy”) OR AB (“interpersonal psychotherapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“reminiscence therapy”) OR AB (“reminiscence therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“brief psychodynamic therapy”) OR AB (“brief psychodynamic therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“humour therapy”) OR AB (“humour therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (art therapy) OR AB (art therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (psychotherapy) OR AB (psychotherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“physical exercise”) OR AB (“physical exercise”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“hope interventions”) OR AB (“hope interventions”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“friendly visitors”) OR AB (“friendly visitors”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (phototherapy) OR AB (phototherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“light therapy”) OR AB (“light therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“talk therapy”) OR AB (“talk therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“biking therapy”) OR AB (“biking therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (aromatherapy) OR AB (aromatherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (massage) OR AB (massage)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (relaxation therapy) OR AB (relaxation therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“guided imagery”) OR AB (“guided imagery”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“health status acupressure”) OR AB (“health status acupressure”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (acupuncture) OR AB (acupuncture)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“cognitive-behavioural breathlessness”) OR AB (“cognitive-behavioural breathlessness”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (mindfulness) OR AB (mindfulness)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (family therapy)) OR AB (family therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“mindfulness based cognitive therapy”)) OR AB (“mindfulness based cognitive therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“self help”)) OR AB (“self help”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (mind-body therapies)) OR AB (mind-body therapies)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“reiki”)) OR AB (“reiki”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (tai chI)) OR AB (tai chi)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“music-movement therapy”)) OR AB (“music-movement therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (dance therapy)) OR AB (dance therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (psycho-education)) OR AB (psycho-education)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (sleep deprivation)) OR AB (sleep deprivation)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (behavioral activation)) OR AB (behavioral activation)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
PubMed
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*) ) AND ( TI (“non pharmacologic*” OR nonpharmacologic*) OR AB (nonpharmacologic* OR “non pharmacologic*”) ) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“self-worth therapy”) OR AB (“self-worth therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“music therapy”) OR AB (“music therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (yoga) OR AB (yoga)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“psychosocial interventions”) OR AB (“psychosocial interventions”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“problem solving therapy”) OR AB (“problem solving therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* “OR stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“cognitive behavioral therapy”) OR AB (“cognitive behavioral therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (cognitive therapy) OR AB (cognitive therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“interpersonal psychotherapy”) OR AB (“interpersonal psychotherapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“reminiscence therapy”) OR AB (“reminiscence therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“brief psychodynamic therapy”) OR AB (“brief psychodynamic therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“humour therapy”) OR AB (“humour therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (art therapy) OR AB (art therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (psychotherapy) OR AB (psychotherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“physical exercise”) OR AB (“physical exercise”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“hope interventions”) OR AB (“hope interventions”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“friendly visitors”) OR AB (“friendly visitors”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (phototherapy) OR AB (phototherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“light therapy”) OR AB (“light therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“talk therapy”) OR AB (“talk therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“biking therapy”) OR AB (“biking therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (aromatherapy) OR AB (aromatherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (massage) OR AB (massage)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (relaxation therapy) OR AB (relaxation therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“guided imagery”) OR AB (“guided imagery”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“health status acupressure”) OR AB (“health status acupressure”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (acupuncture) OR AB (acupuncture)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“cognitive-behavioural breathlessness”) OR AB (“cognitive-behavioural breathlessness”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (mindfulness) OR AB (mindfulness)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (family therapy)) OR AB (family therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“mindfulness based cognitive therapy”)) OR AB (“mindfulness based cognitive therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“self help”)) OR AB (“self help”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (mind-body therapies)) OR AB (mind-body therapies)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“reiki”)) OR AB (“reiki”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (tai chI)) OR AB (tai chi)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“music-movement therapy”)) OR AB (“music-movement therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (dance therapy)) OR AB (dance therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (psycho-education)) OR AB (psycho-education)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (sleep deprivation)) OR AB (sleep deprivation)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (behavioral activation)) OR AB (behavioral activation)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
Cochrane Central Register of Controlled Trials
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*) ) AND ( TI (“non pharmacologic*” OR nonpharmacologic*) OR AB (nonpharmacologic* OR “non pharmacologic*”) ) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“self-worth therapy”) OR AB (“self-worth therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“music therapy”) OR AB (“music therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (yoga) OR AB (yoga)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“psychosocial interventions”) OR AB (“psychosocial interventions”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“problem solving therapy”) OR AB (“problem solving therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* “OR stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“cognitive behavioral therapy”) OR AB (“cognitive behavioral therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (cognitive therapy) OR AB (cognitive therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“interpersonal psychotherapy”) OR AB (“interpersonal psychotherapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“reminiscence therapy”) OR AB (“reminiscence therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“brief psychodynamic therapy”) OR AB (“brief psychodynamic therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“humour therapy”) OR AB (“humour therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (art therapy) OR AB (art therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (psychotherapy) OR AB (psychotherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“physical exercise”) OR AB (“physical exercise”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“hope interventions”) OR AB (“hope interventions”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“friendly visitors”) OR AB (“friendly visitors”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (phototherapy) OR AB (phototherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“light therapy”) OR AB (“light therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“talk therapy”) OR AB (“talk therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“biking therapy”) OR AB (“biking therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (aromatherapy) OR AB (aromatherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (massage) OR AB (massage)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (relaxation therapy) OR AB (relaxation therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“guided imagery”) OR AB (“guided imagery”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“health status acupressure”) OR AB (“health status acupressure”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (acupuncture) OR AB (acupuncture)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“cognitive-behavioural breathlessness”) OR AB (“cognitive-behavioural breathlessness”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (mindfulness) OR AB (mindfulness)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (family therapy)) OR AB (family therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“mindfulness based cognitive therapy”)) OR AB (“mindfulness based cognitive therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“self help”)) OR AB (“self help”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (mind-body therapies)) OR AB (mind-body therapies)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“reiki”)) OR AB (“reiki”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (tai chI)) OR AB (tai chi)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“music-movement therapy”)) OR AB (“music-movement therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (dance therapy)) OR AB (dance therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (psycho-education)) OR AB (psycho-education)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (sleep deprivation)) OR AB (sleep deprivation)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (behavioral activation)) OR AB (behavioral activation)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
SCOPUS
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“non pharmacologic*” OR nonpharmacologic*)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“self-worth therapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“music therapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (yoga)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“psychosocial interventions”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (problem solving therapy)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“cognitive behavioral therapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“cognitive therapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“interpersonal psychotherapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“reminiscence therapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“brief psychodynamic therapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“humour therapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (art therapy)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (psychotherapy)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“physical exercise”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“hope interventions”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“friendly visitors”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (phototherapy)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“light therapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“talk therapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“biking therapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (aromatherapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (massage)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (relaxation therapy)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“guided imagery”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“health status acupresure”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (acupuncture)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“cognitive-behavioral breathlessness”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (mindfulness)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“family therapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“mindfulnes based cognitive therapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (self-help)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“mind-body therapies”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“reiki”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (tai chi)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“music-movement therapy”)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (dance therapy)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (psycho-education)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (sleep deprivation)) AND PUBYEAR > 1999
TITLE-ABS-KEY((depres* OR mood OR negative affect*) AND (stroke* OR “stroke survivor*”) AND (“behavioral activation”)) AND PUBYEAR > 1999
Library, Information Science and Technology Abstracts
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*) ) AND ( TI (“non pharmacologic*” OR nonpharmacologic*) OR AB (nonpharmacologic* OR “non pharmacologic*”) ) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“self-worth therapy”) OR AB (“self-worth therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“music therapy”) OR AB (“music therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (yoga) OR AB (yoga)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“psychosocial interventions”) OR AB (“psychosocial interventions”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“problem solving therapy”) OR AB (“problem solving therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* “OR stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“cognitive behavioral therapy”) OR AB (“cognitive behavioral therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (cognitive therapy) OR AB (cognitive therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“interpersonal psychotherapy”) OR AB (“interpersonal psychotherapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“reminiscence therapy”) OR AB (“reminiscence therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“brief psychodynamic therapy”) OR AB (“brief psychodynamic therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“humour therapy”) OR AB (“humour therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (art therapy) OR AB (art therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (psychotherapy) OR AB (psychotherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“physical exercise”) OR AB (“physical exercise”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“hope interventions”) OR AB (“hope interventions”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“friendly visitors”) OR AB (“friendly visitors”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (phototherapy) OR AB (phototherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“light therapy”) OR AB (“light therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“talk therapy”) OR AB (“talk therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“biking therapy”) OR AB (“biking therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (aromatherapy) OR AB (aromatherapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (massage) OR AB (massage)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (relaxation therapy) OR AB (relaxation therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“guided imagery”) OR AB (“guided imagery”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“health status acupressure”) OR AB (“health status acupressure”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (acupuncture) OR AB (acupuncture)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“cognitive-behavioural breathlessness”) OR AB (“cognitive-behavioural breathlessness”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (mindfulness) OR AB (mindfulness)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (family therapy)) OR AB (family therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“mindfulness based cognitive therapy”)) OR AB (“mindfulness based cognitive therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“self help”)) OR AB (“self help”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (mind-body therapies)) OR AB (mind-body therapies)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“reiki”)) OR AB (“reiki”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (tai chi)) OR AB (tai chi)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (“music-movement therapy”)) OR AB (“music-movement therapy”)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (dance therapy)) OR AB (dance therapy)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (psycho-education)) OR AB (psycho-education)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (sleep deprivation)) OR AB (sleep deprivation)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
(TI (depres* OR mood OR negative affect*) OR AB (depres* OR mood OR negative affect*)) AND (TI (behavioral activation)) OR AB (behavioral activation)) AND (TI (stroke* OR “stroke survivor*”) OR AB (stroke* OR “stroke survivor*”))
Appendix B. Summary of methodological quality (Total number of trials = 22)
| Type of intervention | Author, year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Complementary and alternative therapy (N = 5) | Lee et al., 2016 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Man et al., 2014 | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | 9 | |
| Särkämö et al., 2008 | Y | N | N | Y | Y | Y | Y | Y | Y | Y | 8 | |
| Raglio et al., 2017 | Y | U | N | Y | Y | Y | Y | Y | Y | Y | 8 | |
| Menghan et al., 2017 | Y | Y | N | N | Y | Y | Y | Y | Y | Y | 8 | |
| Exercise (N = 6) | Lai et al., 2006 | U | N | U | Y | Y | Y | N | Y | Y | Y | 6 |
| Mead et al., 2007 | N | N | N | Y | Y | Y | Y | Y | Y | Y | 7 | |
| Topcuoglu et al., 2015 | Y | N | U | N | Y | Y | Y | Y | Y | Y | 7 | |
| Zedlitz et al., 2012 | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 9 | |
| Vahlberg et al., 2017 | Y | U | Y | Y | Y | Y | N | Y | Y | Y | 8 | |
| Rowe et al., 2017 | Y | Y | U | Y | Y | Y | Y | Y | Y | Y | 9 | |
| Psychosocial therapy (N = 6) | Aben et al., 2013 | Y | Y | U | Y | Y | Y | Y | Y | Y | Y | 9 |
| Mitchell et al., 2009 | Y | U | U | Y | Y | Y | Y | Y | Y | Y | 8 | |
| Visser et al., 2016 | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 8 | |
| Watkins et al., 2011 | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 8 | |
| Kirkness et al., 2017 | Y | U | N | N | Y | Y | N | Y | Y | Y | 6 | |
| Kootker et al., 2017 | Y | U | Y | Y | Y | Y | Y | Y | Y | Y | 9 | |
| Multifactorial therapy (N = 3) | Ihle-Hansen et al., 2014 | Y | U | Y | Y | Y | Y | Y | Y | Y | Y | 9 |
| Rochette et al., 2013 | N | N | Y | N | Y | Y | Y | Y | Y | Y | 7 | |
| Wong et al., 2017 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 | |
| Cranial stimulation (N = 2) | Valiengo et al., 2017 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Gu et al., 2017 | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | 9 | |
| Percentage | 77% | 36% | 45% | 82% | 100% | 100% | 86% | 100% | 100% | 100% | Mean=8.27 SD=1.16 |
|
Q1: Was the assignment to treatment groups truly random? Q2: Were participants blinded to treatment allocation? Q3: Was allocation to treatment groups concealed from the allocator? Q4: Were the outcomes of people who withdrew described and included in the analysis? Q5: Were those assessing outcomes blind to the treatment allocation? Q6: were the control and treatment groups comparable at entry? Q7: Were groups treated identically other than for the named interventions? Q8: Were outcomes measured in the same way for all groups? Q9: Were outcomes measured in a reliable way? Q10: Was appropriate statistical analysis used?
U: Unclear
Appendix C. Detailed descriptions for psychosocial therapy
| Author, year | Name of therapy | Descriptions |
|---|---|---|
| Mitchell et al., 2009 | Psychosocial behavioral intervention | Identification of pleasant events, planning and scheduling pleasant events, identifying problems and planning, and applying problem-solving techniques to manage depressive symptoms, cope with caregiving, change negative thoughts and behaviors, and maintain gains and generalize to other situations |
| Watkins et al., 2009 | Motivational interviewing, a patient-centered counseling technique | Setting patients’ personal and realistic goals for recovery and recognizing perceived barriers to attaining those goals. By working through patients’ dilemmas and ambivalence, and by supporting and reinforcing optimism and self-efficacy, therapists enable patients to identify their own solutions |
| Aben et al., 2013 | Memory self-efficacy training program | Focusing on altering negative beliefs regarding memory functioning by using training in internal and external memory strategies to improve compensating abilities (eg, visualization, diary use, and taking notes) and providing psychoeducation on the influence of beliefs, anxiety, memory-related worries, and motivation on memory performance |
| Visser et al., 2016 | Problem-solving therapy | The problem-solving process followed four steps: (1) define the problem and goal, (2) generate multiple solutions, (3) select a solution, and (4) implement and evaluate |
| Kirkness et al., 2017 | Brief psychosocial–behavioral intervention | Scheduling pleasant events, identifying problems and planning, managing depression behaviors, learning problem-solving techniques, changing negative thoughts and behaviors, and review of skills, generalization, and strategies for maintaining skills |
| Kootker et al., 2017 | Augmented cognitive behavioral therapy (CBT) | Goals for attaining daily life activities were primarily set together by the patient and the therapist using pictures from the Activity Card Sort. Concurrently with the psychological sessions, the CBT intervention was augmented with three sessions of occupational therapy or movement therapy |
Appendix D. Funnel plots: (a) a funnel plot including all included trials; (b) a funnel plot excluding three trials that showed publication bias on plot (a)
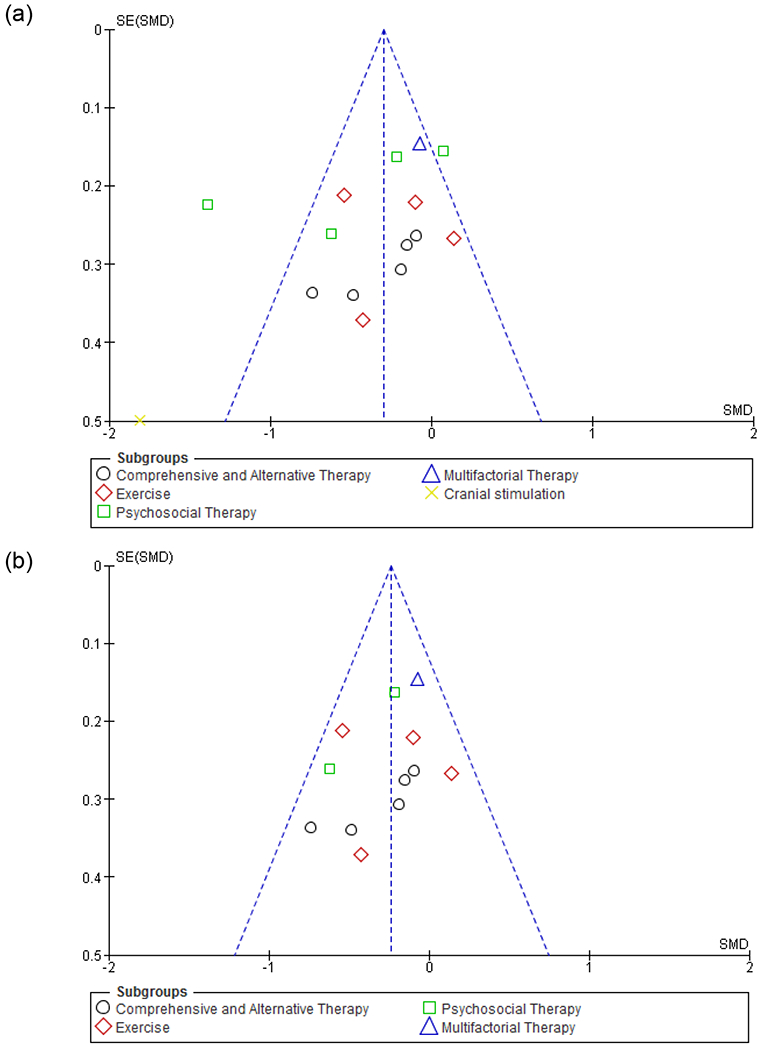
Appendix E. Forest plot comparing specific complementary and alternative therapy interventions and control groups on depressive symptoms (post-intervention)
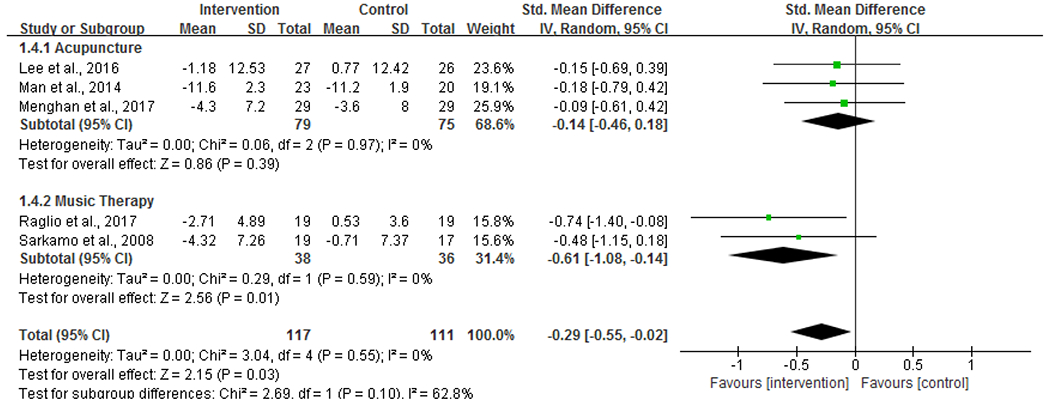
Footnotes
Reprints are not available from the authors. Part of this research has been presented at the 2018 American Congress of Rehabilitation Medicine Annual Conference.
References
- 1.Adamson J, Beswick A, Ebrahim S. Is stroke the most common cause of disability? Journal of stroke and cerebrovascular diseases 2004;13(4):171–177. [DOI] [PubMed] [Google Scholar]
- 2.Hackett ML, Yapa C, Parag V, Anderson CS. Frequency of depression after stroke: a systematic review of observational studies. Stroke. 2005;36(6):1330–1340. [DOI] [PubMed] [Google Scholar]
- 3.Kutlubaev MA, Hackett ML. Part II: predictors of depression after stroke and impact of depression on stroke outcome: an updated systematic review of observational studies. International journal of stroke. 2014;9(8):1026–1036. [DOI] [PubMed] [Google Scholar]
- 4.Loubinoux I, Kronenberg G, Endres M, et al. Post-stroke depression: mechanisms, translation and therapy. Journal of cellular and molecular medicine. 2012;16(9):1961–1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen Y, Guo JJ, Zhan S, Patel NC. Treatment effects of antidepressants in patients with post-stroke depression: a meta-analysis. Annals of pharmacotherapy. 2006;40(12):2115–2122. [DOI] [PubMed] [Google Scholar]
- 6.Hackett ML, Anderson CS, House A, Xia J. Interventions for treating depression after stroke. Cochrane database of systematic reviews. 2008(4). [DOI] [PubMed] [Google Scholar]
- 7.Ramasubbu R Therapy for prevention of post-stroke depression. Expert opinion on pharmacotherapy 2011;12(14):2177–2187. [DOI] [PubMed] [Google Scholar]
- 8.Hadidi NN, Wagner RLH, Lindquist R. Nonpharmacological treatments for post-stroke depression: an integrative review of the literature. Research in gerontological nursing 2017;10(4):182–195. [DOI] [PubMed] [Google Scholar]
- 9.Qin B, Chen H, Gao W, et al. Efficacy, acceptability, and tolerability of antidepressant treatments for patients with post-stroke depression: a network meta-analysis. Brazilian journal of medical and biological research. 2018;51(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Apóstolo J, Queirós P, Rodrigues M, Castro I, Cardoso D. The effectiveness of nonpharmacological interventions in older adults with depressive disorders: a systematic review. JBI database of systematic reviews and implementation reports 2015;13(6):220–278. [DOI] [PubMed] [Google Scholar]
- 11.Lökk J, Delbari A. Management of depression in elderly stroke patients. Neuropsychiatric disease and treatment. 2010;6:539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Farah WH, Alsawas M, Mainou M, et al. Non-pharmacological treatment of depression: a systematic review and evidence map. BMJ evidence-based medicine. 2016;21(6):214–221. [DOI] [PubMed] [Google Scholar]
- 13.Lett HS, Davidson J, Blumenthal JA. Nonpharmacologic treatments for depression in patients with coronary heart disease. Psychosomatic medicine. 2005;67:S58–S62. [DOI] [PubMed] [Google Scholar]
- 14.De Man-van Ginkel JM, Gooskens F, Schuurmans MJ, Lindeman E, Hafsteinsdottir TB, Group RGSW. A systematic review of therapeutic interventions for poststroke depression and the role of nurses. Journal of clinical nursing. 2010;19(23-24):3274–3290. [DOI] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine. 2009;151(4):264–269. [DOI] [PubMed] [Google Scholar]
- 16.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS medicine 2009;6(7):e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoogendam A, de Vries Robbe PF, Overbeke AJP. Comparing patient characteristics, type of intervention, control, and outcome (PICO) queries with unguided searching: a randomized controlled crossover trial. Journal of the medical library association: JMLA 2012;100(2):121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schultz T, Florence Z. Joanna Briggs institute meta-analysis of statistics assessment and review instrument. Adelaide: Joanna Briggs Institute; 2007. [Google Scholar]
- 19.Morris SB. Estimating effect sizes from pretest-posttest-control group designs. Organizational research methods 2008;11(2):364–386. [Google Scholar]
- 20.Morris SB, DeShon RP. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychological methods 2002;7(1):105. [DOI] [PubMed] [Google Scholar]
- 21.Becker BJ. Synthesizing standardized mean-change measures. British Journal of mathematical and statistical psychology. 1988;41(2):257–278. [Google Scholar]
- 22.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. 2008. [Google Scholar]
- 23.Higgins J, Green S. Handbook for systematic reviews of interventions version 5.1. 0 [updated March 2011]. The Cochrane collaboration. 2011. [Google Scholar]
- 24.Cohen J Statistical power analysis for the behavioral sciences 2nd edn. Hillsdale, New Jersey: Erlbaum Associates; 1988. [Google Scholar]
- 25.Lee GE, Son C, Lee J, et al. Acupuncture for shoulder pain after stroke: A randomized controlled clinical trial. European journal of integrative medicine 2016;8(4):373–383. [Google Scholar]
- 26.Wong FKY, Yeung SM. Effects of a 4-week transitional care programme for discharged stroke survivors in Hong Kong: a randomised controlled trial. Health & social care in the community. 2015;23(6):619–631. [DOI] [PubMed] [Google Scholar]
- 27.Gu SY, Chang MC. The effects of 10-Hz repetitive transcranial magnetic stimulation on depression in chronic stroke patients. Brain stimulation. 2017;10(2):270–274. [DOI] [PubMed] [Google Scholar]
- 28.Topcuoglu A, Gokkaya NKO, Ucan H, Karakuş D. The effect of upper-extremity aerobic exercise on complex regional pain syndrome type I: a randomized controlled study on subacute stroke. Topics in stroke rehabilitation. 2015;22(4):253–261. [DOI] [PubMed] [Google Scholar]
- 29.Watkins CL, Wathan JV, Leathley MJ, et al. The 12-month effects of early motivational interviewing after acute stroke: a randomized controlled trial. Stroke. 2011;42(7):1956–1961. [DOI] [PubMed] [Google Scholar]
- 30.Valiengo LC, Goulart AC, de Oliveira JF, Benseñor IM, Lotufo PA, Brunoni AR. Transcranial direct current stimulation for the treatment of post-stroke depression: results from a randomised, sham-controlled, double-blinded trial. Journal of neurol neurosurg psychiatry. 2017;88(2):170–175. [DOI] [PubMed] [Google Scholar]
- 31.Mead GE, Greig CA, Cunningham I, et al. Stroke: a randomized trial of exercise or relaxation. Journal of the american geriatrics society. 2007;55(6):892–899. [DOI] [PubMed] [Google Scholar]
- 32.Kootker JA, Rasquin SM, Lem FC, van Heugten CM, Fasotti L, Geurts AC. Augmented cognitive behavioral therapy for poststroke depressive symptoms: a randomized controlled trial. Archives of physical medicine and rehabilitation 2017;98(4):687–694. [DOI] [PubMed] [Google Scholar]
- 33.Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I² index? Psychological methods 2006;11(2):193. [DOI] [PubMed] [Google Scholar]
- 34.Visser MM, Heijenbrok-Kal MH, van’t Spijker A, Lannoo E, Busschbach JJ, Ribbers GM. Problem-solving therapy during outpatient stroke rehabilitation improves coping and health-related quality of life: randomized controlled trial. Stroke. 2016;47(1):135–142. [DOI] [PubMed] [Google Scholar]
- 35.Mitchell PH, Veith RC, Becker KJ, et al. Brief psychosocial–behavioral intervention with antidepressant reduces poststroke depression significantly more than usual care with antidepressant: living well with stroke: randomized, controlled trial. Stroke. 2009;40(9):3073–3078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ihle-Hansen H, Thommessen B, Fagerland MW, et al. Effect on anxiety and depression of a multifactorial risk factor intervention program after stroke and TIA: a randomized controlled trial. Aging and mental health. 2014;18(5):540–546. [DOI] [PubMed] [Google Scholar]
- 37.Cuijpers P, Clignet F, van Meijel B, van Straten A, Li J, Andersson G. Psychological treatment of depression in inpatients: a systematic review and meta-analysis. Clinical psychology review 2011;31(3):353–360. [DOI] [PubMed] [Google Scholar]
- 38.Cuijpers P, van Straten A, Bohlmeijer E, Hollon S, Andersson G. The effects of psychotherapy for adult depression are overestimated: a meta-analysis of study quality and effect size. Psychological medicine 2010;40(2):211–223. [DOI] [PubMed] [Google Scholar]
- 39.Starkstein SE, Mizrahi R, Power BD. Antidepressant therapy in post-stroke depression. Expert opinion on pharmacotherapy 2008;9(8):1291–1298. [DOI] [PubMed] [Google Scholar]
- 40.Tsai HF, Chen YR, Chung MH, et al. Effectiveness of music intervention in ameliorating cancer patients’ anxiety, depression, pain, and fatigue: A meta-analysis. Cancer nursing 2014;37(6):E35–E50. [DOI] [PubMed] [Google Scholar]
- 41.Zhang Y, Cai J, An L, et al. Does music therapy enhance behavioral and cognitive function in elderly dementia patients? A systematic review and meta-analysis. Ageing research reviews 2017;35:1–11. [DOI] [PubMed] [Google Scholar]
- 42.Raglio A, Attardo L, Gontero G, Rollino S, Groppo E, Granieri E. Effects of music and music therapy on mood in neurological patients. World journal of psychiatry. 2015;5(1):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Raglio A, Fazio P, Imbriani C, Granieri E. Neuro-scientific basis and effectiveness of music and music therapy in neuromotor rehabilitation. OA Alternat ive medicine 2013;1(1):8. [Google Scholar]
- 44.Särkämö T, Tervaniemi M, Laitinen S, et al. Music listening enhances cognitive recovery and mood after middle cerebral artery stroke. Brain. 2008;131(3):866–876. [DOI] [PubMed] [Google Scholar]
- 45.Hanser SB. A music therapy strategy for depressed older adults in the community. Journal of applied gerontology. 1990;9(3):283–298. [Google Scholar]
- 46.Siamouli M, Magiria S, Panagiotidis P, et al. Advances in the treatment of geriatric depression. 2007. [Google Scholar]
- 47.Kneebone II, Dunmore E. Psychological management of post-stroke depression. British Journal of clinical psychology. 2000;39(1):53–65. [DOI] [PubMed] [Google Scholar]
- 48.Stalder-Lüthy F, Messerli-Bürgy N, Hofer H, Frischknecht E, Znoj H, Barth J. Effect of psychological interventions on depressive symptoms in long-term rehabilitation after an acquired brain injury: a systematic review and meta-analysis. Archives of physical medicine and rehabilitation. 2013;94(7):1386–1397. [DOI] [PubMed] [Google Scholar]
- 49.Babakhanyan I, Carlozzi NE, McKenna BS, Casaletto KB, Heinemann AW, Heaton RK. NIH Toolbox Emotion Battery: Application of Summary Scores to Adults with Spinal Cord Injury, Traumatic Brain Injury, and Stroke. Archives of physical medicine and rehabilitation 2019. [DOI] [PubMed] [Google Scholar]
- 50.Della Vecchia C, Viprey M, Haesebaert J, et al. Contextual determinants of participation after stroke: a systematic review of quantitative and qualitative studies. Disability and rehabilitation. 2019:1–13. [DOI] [PubMed] [Google Scholar]
- 51.Suzuki S-i, Takei Y. Psychosocial Factors and Traumatic Events. In: Gellman MD, Turner JR, eds. Encyclopedia of behavioral medicine. New York, NY: Springer New York; 2013:1582–1583. [Google Scholar]
- 52.Hackett ML, Anderson CS. Predictors of depression after stroke: a systematic review of observational studies. Stroke. 2005;36(10):2296–2301. [DOI] [PubMed] [Google Scholar]
- 53.Johnson JL, Minarik PA, Nyström KV, Bautista C, Gorman MJ. Poststroke depression incidence and risk factors: an integrative literature review. LWW; 2006. [DOI] [PubMed] [Google Scholar]
- 54.Chan MF, Chan EA, Mok E, Kwan Tse FY. Effect of music on depression levels and physiological responses in community-based older adults. International journal of mental health nursing. 2009;18(4):285–294. [DOI] [PubMed] [Google Scholar]
- 55.Fried EI, Nesse RM. The impact of individual depressive symptoms on impairment of psychosocial functioning. PloS one. 2014;9(2):e90311. [DOI] [PMC free article] [PubMed] [Google Scholar]


