INTRODUCTION
Over one third of the 47,600 opioid overdose deaths in 2017 involved prescription opioids.1 Co-prescribing naloxone—an overdose reversal agent—alongside high-risk opioid therapy has been championed as a harm reduction practice for preventing fatal overdoses.2 While naloxone co-prescribing is uncommon overall,3 little is known about trends in naloxone prescribing in the Medicare population, which has experienced recent increases in opioid overdose.4, 5 The objective of this study was to describe patterns of naloxone-prescribing engagement among frequent opioid prescribers using the Medicare Provider Utilization and Payment Data: Part D Prescriber Public Use File from 2013 to 2017.
METHODS
Part D Prescriber data provides annual frequencies of Part D–covered prescriptions for all US prescribers. The study cohort included annual cross-sections of frequent opioid prescribers, defined as prescribers with a greater-than-median Part D–covered opioid prescription counts in the year. Logistic regression was used to estimate predicted probabilities of a prescriber exhibiting naloxone-prescribing engagement (> 10 Part D–covered naloxone prescriptions), clustering on prescriber and adjusting for calendar year, prescriber sex, opioid prescription count, long-acting opioid prescription count, provider type (primary care, surgery, mid-level, or other), state fixed effects, and mean age and CMS Hierarchical Condition Category risk score of their Part D patients. Annual adjusted predicted probabilities were reported for prescribers in the top 50%, 10%, and 1% of opioid prescribers by opioid prescription volume. Using 2017 data, the prevalence of naloxone-prescribing engagement was reported within the 15 clinical specialties with the greatest number of frequent opioid prescribers (top 50%). This study was exempted from the institutional review board review.
RESULTS
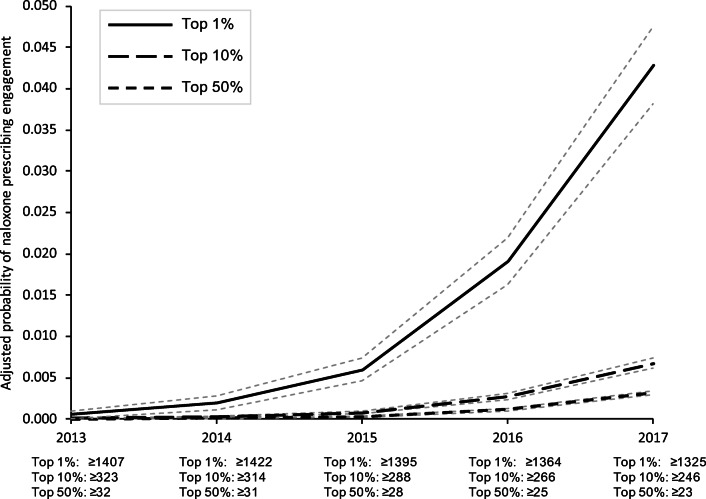
The adjusted probability of naloxone-prescribing engagement increased from 0% in 2013 to 0.32% (95% confidence interval (CI), 0.30–0.34%) and 0.68% (95% CI, 0.62–0.73%) in 2017 among prescribers in the top 50% and top 10% of opioid prescribers by prescription volume, respectively. Providers in the top 1% of opioid prescribers had an adjusted predicted probability of naloxone-prescribing engagement of 4.3% in 2017 (95% CI, 3.8–4.8%) (Fig. 1). Table 1 reports the prevalence of naloxone-prescribing engagement in 2017 among all frequent opioid prescribers (those in the top 50th percentile of opioid prescriptions written) and by provider type/specialty. Less than 1% of frequent opioid prescribers in most provider specialty groups exhibited naloxone-prescribing engagement. The highest prevalence of naloxone-prescribing engagement occurred in pain specialists (2.99%) and anesthesiologists (2.59%). These providers also wrote the most opioid prescriptions on average-per-prescriber of all specialties.
Figure 1.
Annual adjusted predicted probability of naloxone-prescribing engagement among frequent opioid prescribers in Medicare Part D, 2013–2017. Analyses were derived from the Medicare Provider Utilization and Payment Data: Part D Prescriber dataset from the Centers for Medicare and Medicaid Services. “Top 1%,” “Top 10%,” and “Top 50%” groups represent providers whose Part D–covered opioid prescription volume in a given year were above the 99th percentile, 90th percentile, and 50th percentile, respectively, of all Part D opioid prescribers. Opioid prescription counts/prescriber at the 99th, 90th, and 50th percentile in a given year are reported under the calendar year label on the X-axis. The naloxone-prescribing engagement outcome measure was defined as > 10 Part D covered prescriptions of a naloxone product in a given year. Predicted probabilities were estimated using logistic regression, clustered on prescriber, and adjusting for calendar year, prescriber sex, opioid prescription count, long-acting opioid prescription count, provider type (primary care, surgery, mid-level, or other), state fixed effects, and mean age and CMS Hierarchical Condition Category risk score of their Part D patients. Gray dotted lines indicate bounds for 95% confidence intervals.
Table 1.
Prevalence of Naloxone Prescribers Among Frequent Opioid Prescribers in Medicare Part D in 2017, Overall and by Clinical Specialty
| Top 50% opioid prescribers | Part D–covered opioid prescriptions-per-prescriber | Part D beneficiaries receiving opioids-per-prescriber | Prescribers with > 10 naloxone fills | ||||
|---|---|---|---|---|---|---|---|
| Prescriber type/specialtya | n | Mean | (SD) | Mean | (SD) | n | (%) |
| All prescribers | 342,817 | 205 | (454) | 60 | (72) | 1078 | (0.31%) |
| Primary careb | 134,218 | 255 | (360) | 60 | (58) | 207 | (0.15%) |
| Mid-level providersc | 76,538 | 168 | (383) | 54 | (66) | 470 | (0.61%) |
| Emergency medicine | 24,802 | 71 | (135) | 57 | (39) | 6 | (0.02%) |
| Surgery, non-orthopedic | 19,916 | 75 | (117) | 52 | (38) | 4 | (0.02%) |
| Surgery, orthopedic | 17,547 | 161 | (228) | 80 | (66) | 3 | (0.02%) |
| Dentistry/oral surgery | 9755 | 68 | (58) | 57 | (50) | 0 | (0.00%) |
| Oncology | 9350 | 112 | (118) | 33 | (25) | 0 | (0.00%) |
| Pain/physical medicine/rehabilitation | 9084 | 889 | (1548) | 157 | (217) | 272 | (2.99%) |
| Rheumatology | 5899 | 71 | (62) | 55 | (35) | 2 | (0.03%) |
| Podiatry | 4695 | 59 | (52) | 32 | (21) | 0 | (0.00%) |
| Neurology | 4064 | 213 | (570) | 36 | (77) | 17 | (0.42%) |
| Rheumatology | 3549 | 342 | (504) | 72 | (80) | 4 | (0.11%) |
| Otolaryngology | 2872 | 45 | (36) | 35 | (21) | 0 | (0.00%) |
| Anesthesiology | 2704 | 1045 | (1652) | 182 | (234) | 70 | (2.59%) |
| Nephrology | 2083 | 89 | (126) | 26 | (27) | 0 | (0.00%) |
Analyses and specialty categories were derived from the Medicare Provider Utilization and Payment Data: Part D Prescriber dataset from the Centers for Medicare and Medicaid Services. “Top 50% opioid prescribers” represents providers for whom the total number of Part D–covered opioid prescriptions they wrote in in 2017 was above the median among all Part D opioid prescribers in 2017
aThese 15 clinical specialty categories captured 95% of all providers in the top 50% of Part D opioid prescribers by opioid prescription volume in 2017
bPrimary care included family medicine, general practice, internal medicine, geriatric medicine, and pediatric medicine subspecialties
cMid-level providers consists of providers designated in study data as nurse practitioners or physician assistants. No further clinical subspecialty was noted for these mid-level providers
DISCUSSION
Naloxone-prescribing engagement has increased among frequent opioid prescribers since 2013, when it was practically nonexistent. The greatest uptake of naloxone prescribing occurred after 2015 and in the top 1% of opioid prescribers by volume, who had a 4% adjusted probability of naloxone-prescribing engagement by 2017. However, regular naloxone prescribing remained rare overall. Even among pain specialists and anesthesiologists, whom frequently manage intensive opioid therapy, less than 3% of frequent opioid prescribers exhibited regular naloxone prescribing. While Medicare patients account for over one third of all dispensed naloxone prescriptions6—compared to privately insured (51%) and Medicaid recipients (11%)—broader adoption of naloxone co-prescribing is needed. Implementing automated naloxone co-prescription order sets for high-risk prescription opioid therapy, and removing cost-sharing6 for naloxone prescriptions can promote naloxone availability.
Study limitations include a lack of patient- or prescription-level information to assess detailed opioid prescribing patterns or patient-level opioid overdose risk in Part D Prescriber data. This data also censors naloxone fill records for prescribers with < 11 Part D–covered naloxone prescriptions. However, this study sought to examine trends in regular naloxone-prescribing engagement (≥ 11 prescriptions/year) among frequent opioid prescribers. This approach is supported by prior evidence showing a high prevalence of high-risk opioid use among providers’ Part D populations necessitating consideration of naloxone co-prescription.7 Additionally, study data did not capture naloxone receipt through non-prescription means or instances where patients received a naloxone prescription but did not fill it. Lastly, analyses adjusted for state and year fixed effects but did not adjust for specific state-level naloxone access policies.
Despite recent growth in naloxone prescribing in Medicare Part D, this important harm reduction practice remains rare among frequent opioid prescribers across all specialties. Clinicians who frequently prescribe opioid therapy to Part D patients at high risk of opioid overdose should strongly consider incorporating regular naloxone co-prescribing into their practices.
Acknowledgments
Dr. Roberts was supported by a career development award from the National Center for Advancing Translational Sciences to the Frontiers: University of Kansas Clinical and Translational Science Institute (no. KL2TR002367).
Compliance with Ethical Standards
Conflict of Interest
The author declares that he does not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centers for Disease Control and Prevention. Wide-ranging online data for epidemiologic research (WONDER). 2019; http://wonder.cdc.gov.
- 2.US Department of Health and Human Services. The Opioid Reversal Drug that Saves Lives: How Healthcare Providers and Patients Can Better Utilize this Life-Saving Drug. December 19, 2018; https://www.hhs.gov/opioids/sites/default/files/2018-12/naloxone-coprescribing-guidance.pdf.
- 3.Jones CM, Compton W, Vythilingam M, Giroir B. Naloxone Co-prescribing to Patients Receiving Prescription Opioids in the Medicare Part D Program, United States, 2016-2017. JAMA. 2019;322(5):462–464. doi: 10.1001/jama.2019.7988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuo YF, Raji MA, Goodwin JS. Association of Disability With Mortality From Opioid Overdose Among US Medicare Adults. JAMA Netw Open. 2019;2(11):e1915638. doi: 10.1001/jamanetworkopen.2019.15638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weiss AJ, Heslin KC, Barrett ML, Izar R, Bierman AS. Opioid-Related Inpatient Stays and Emergency Department Visits Among Patients Aged 65 Years and Older, 2010 and 2015: Statistical Brief #244. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006. [PubMed]
- 6.Guy GP, Jr, Haegerich TM, Evans ME, Losby JL, Young R, Jones CM. Vital Signs: Pharmacy-Based Naloxone Dispensing - United States, 2012-2018. MMWR Morb Mortal Wkly Rep. 2019;68(31):679–686. doi: 10.15585/mmwr.mm6831e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raman SR, Bush C, Karmali RN, Greenblatt LH, Roberts AW, Skinner AC. Characteristics of New Opioid Use Among Medicare Beneficiaries: Identifying High-Risk Patterns. J Manag Care Spec Pharm. 2019;25(9):966–972. doi: 10.18553/jmcp.2019.25.9.966. [DOI] [PMC free article] [PubMed] [Google Scholar]