Abstract
Implementation science is focused on developing and evaluating methods to reduce gaps between research and practice. As healthcare organizations become increasingly accountable for equity, quality, and value, attention has been directed to identifying specific implementation strategies that can accelerate the adoption of evidence-based therapies into clinical practice. In this perspective, we offer three simple, practical strategies that can be used by frontline healthcare providers who are involved in on-the-ground implementation: people (stakeholder) engagement, process mapping, and problem solving. As a use case example, we describe the iterative application of these strategies to the implementation of a new home sleep apnea testing program for patients in the Veterans Health Administration (VA) healthcare system.
INTRODUCTION
During the past two decades, implementation science has emerged as a prominent field broadly defined as the “study of methods to promote the adoption and integration of evidence-based practices, interventions, and policies into routine health care and public health settings1.” In practice, implementation science blends theories from sociology and psychology with the methods of traditional research, quality improvement, and business change management2. Much of the existing literature has focused on the development of theories and frameworks to guide the design, evaluation, and dissemination of effective strategies3. However, the evolving theories, constructs, domains, and classification schemes4, 5 can sometimes introduce unintended barriers for practical application by the very individuals (frontline clinicians and staff) who are responsible for day-to-day implementation.
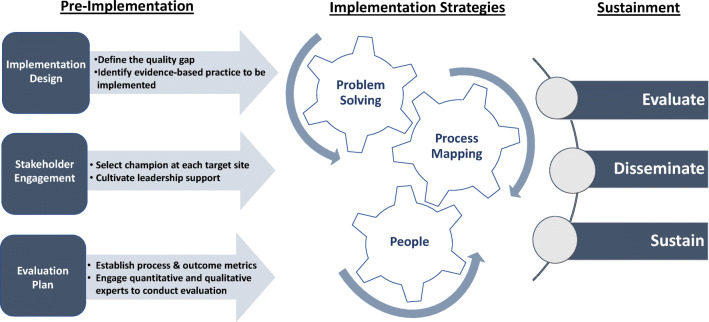
As described in the Veterans Health Administration (VA) Quality Enhancement Research Initiative Roadmap,6 implementation involves three phases: (1) pre-implementation, (2) implementation, and (3) sustainment. Pre-implementation consists of defining a quality gap, identifying an evidence-based practice to reduce this gap, selecting local champions to lead implementation at each target site, and planning how to evaluate the impact of these efforts. During this pre-implementation phase, frontline healthcare professionals often serve as valuable opinion leaders and operational stakeholders but, given the complex and competing demands facing many healthcare leaders, may have limited control over the plan to achieve organizational objectives. Partnering with implementation scientists brings rigor and expertise to the operational approach, selection of outcome metrics, and dissemination of effective strategies.
As a project enters the implementation phase, frontline teams play a critical role in shaping its trajectory and successful sustainment. For the practicing healthcare professional, we propose a simple and practical approach to on-the-ground implementation that involves three essential strategies (people engagement, process mapping, and problem solving) with continuously iterative cycles across these elements during the lifespan of a project. In our experience with national implementation efforts, this approach has proven indispensable for aligning scientists, operational leaders, and frontline staff at local sites. Figure 1 shows how these tools fit into the overall roadmap. As a use case, we describe its application to the implementation of an enterprise-wide home sleep apnea testing initiative.
Figure 1.
Implementation requires iterative cycles of process mapping, problem solving, and stakeholder engagement (people).
Process Mapping
Since its origins in the manufacturing industry, process mapping has become a familiar tool used to visually represent the inputs, outputs, and steps of healthcare improvement7. Although process mapping has not been a prominent feature in the implementation science literature, it has a well-established place in many quality improvement methods such as the Institute for Healthcare Improvement’s Model for Improvement8 and Lean in Healthcare9. The beginning and end of a process map define the boundaries of a specific change initiative. The steps in between highlight key events and the sequence in which they occur. Additional information regarding the operators involved in parallel processes (e.g., swim lane diagrams10) or the potential value associated with each step (e.g., value stream mapping11) may be provided to enhance clarity.
In the pre-implementation phase of a project, process mapping of the existing structures and practices at each site identifies potential adaptations of the intervention that may be necessary and helps delineate important metrics for future tracking. Process maps can identify workflow nodes that are likely to introduce barriers or serve as facilitators. Understanding local processes can also point to strategic adaptations that may be necessary to meet local needs. Sharing process maps with evaluation partners is also helpful for defining metrics (e.g., number of days required to hire necessary personnel, obtain equipment, seek document approvals) to track progress and evaluate outcomes at the completion of a project.
Once the current state has been determined and agreed upon by relevant stakeholders, mapping the envisioned future state articulates the change initiative to everyone involved and may identify new stakeholders who need to be engaged. Implementation ventures typically involve multiple departments and services, including human resources, information technology, supply chain management, facilities operation, and clinical staff. Process mapping allows the site champion to ensure fidelity to essential elements of the evidence-based intervention while identifying potential adaptations to fit local needs. Finally, seeking input from frontline staff on the future state map communicates the importance of their roles and increases their ownership of the new process.
People (Stakeholder) Engagement
Just as identification of a local champion is the most critical aspect of pre-implementation, stakeholder engagement sits at the core of successful implementation. Ideally, the local champion will be a provider embedded in the clinical setting whose workflow will be directly affected by the proposed intervention. Early involvement of leadership and endorsement of the project as an organizational priority is another crucial element in the successful launch of a new initiative. Continuous involvement of stakeholders (including ancillary and support staff) and repeated tailoring of implementation strategies to new stakeholders throughout a project are also key factors in achieving sustained adoption of evidence-based practices.
Although the value of stakeholder engagement has been clearly demonstrated in the literature12, there is surprisingly little evidence to support best practices for the identification and alignment of stakeholders in a proposed initiative, or practical guides for how to gather their valuable input before and during the implementation process3. Frameworks such as the Consolidated Framework for Implementation Research13 and the 7Ps14 (Patients, Providers, Purchasers, Payers, Policymakers, Product Makers, and Principal Investigators) suggest stakeholder categories to consider at the outset of a project. Practically speaking, whoever is touched by the process map, its inputs or its outputs, is a stakeholder. If not invested in a project’s success, stakeholders can (consciously or unconsciously) introduce barriers that make it difficult to implement an intervention. Accordingly, we recommend an intuitive approach: (1) identify “who,” (2) determine “what” they must do for the project to be successful, and (3) articulate “why” or “how” this might align with their interests (Table 1). If a stakeholder is reluctant to embrace the new initiative, focus on how it might align with the interests of his or her supervisor.
Table 1.
Key Questions for People (Stakeholder) Engagement
| Identify “Who” | Establish “What” they must do for successful implementation | Articulate “Why” or “How” the intervention aligns with their interests |
|---|---|---|
|
• Who will implement the change? • Who will be (directly or indirectly) impacted by the change? • Who else might feel ownership in this space? |
• What specifically is each person being asked to do? • How will success be monitored and measured? • Where can cross-training occur? |
• What do they care about? • How does the proposed project align with their interests? • What reservations might they have? • To whom do they report? |
Once active implementation is underway, stakeholder engagement takes on a more dynamic form. Repeatedly engaging frontline champions who are viewed as local thought leaders can generate urgency and encourage others to adopt the intervention15. Providing brief monthly updates refreshes stakeholders about the goals of the initiative, highlights the project’s importance amidst competing demands, and reminds them that their progress is being monitored. Whenever possible, cross-training individuals for different roles such as the implementer, evaluator, and team leader can help mitigate the substantial loss of momentum resulting from unanticipated personnel changes during the fragile early stages of implementation. Finally, celebrating victories both large and small boosts moral and ensures sustained engagement.
Problem Solving
While many useful frameworks, theories, and strategies are available to guide implementation, no playbook will ever anticipate all the challenges that can arise. Successful implementation relies on motivated people crafting innovative solutions16 or workarounds to solve problems as they arise in real-time. When frontline staff are committed to an initiative, problems are recognized early and solutions are implemented quickly. Given the idiosyncrasies of local culture and customs, however, isolating a problem and identifying potential solutions often require iterative cycles of process mapping and new stakeholder engagement. Revisiting the existing process map can help localize the source, identify potential downstream consequences, and discover new processes to bypass barriers. Depending on how and why the problem is occurring, additional stakeholders and their interests may need to be considered and leveraged. Potential solutions can then be tested in small Plan-Do-Study-Act (PDSA) cycles17 before further scale up and spread. Regularly scheduled meetings with the program evaluation team are important for communicating any delays or process changes that may affect data collection or analysis.
Case Example: Implementation of Home Sleep Apnea Testing
Over the past decade, the number of veterans referred for suspected sleep apnea has markedly increased resulting in limited access to timely sleep testing. By 2015, Sleep Medicine had become the second most backlogged clinical service in the VA nationally. One factor contributing to the backlog was the model for diagnosing sleep apnea. Historically, patients underwent overnight in-laboratory polysomnography (PSG), but space and insufficient staffing often limited the number of PSGs that could be performed. Home sleep apnea testing (HSAT) is an alternative method to PSG that was being promoted within VA as a best practice for diagnosing sleep apnea. Yet, as of 2016, few VA facilities offered HSAT. Faced with increasing demands for sleep services and finite resources, an initiative to integrate HSAT into standard practice was created. The San Francisco VA was one of 54 VA facilities involved in this initiative.
Process Mapping
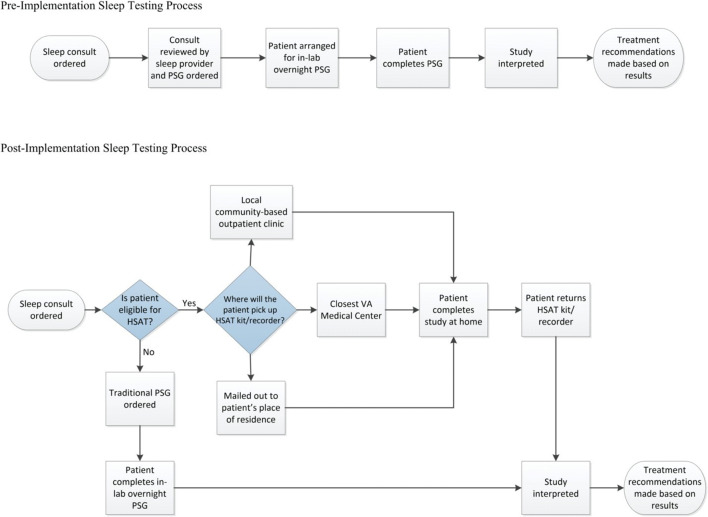
Process mapping of complex patient and provider workflows was critical in establishing how to transition from PSG to HSAT. A simplified pre- and post-implementation diagram (Fig. 2) was developed to begin communication with stakeholders. Process mapping itself is an iterative endeavor; input from dynamic groups of stakeholders helped refine and improve the workflow diagrams over time. Additional maps, which detailed specific operator swim lanes and identified ways to capture workload, were developed to align frontline staff and delineate individual responsibilities at specific nodes. For example, the use of the HSAT devices required process maps for purchasing, testing, storing, provisioning, tracking, returning, and cleaning the equipment. Scheduling grids had to be created and populated with appointments; referring providers and patients had to be educated about the new system. Sleep clinicians established processes for determining patient eligibility for HSAT and interpreting the sleep test recordings. Documentation of each step provided a useful template for implementation at subsequent deployment sites.
Figure 2.
Simplified process maps for implementation of Home Sleep Apnea Testing (HSAT). Transition from polysomnography (PSG) to HSAT eliminated the need for Veterans to spend a night in the hospital, increased capacity for sleep testing, and reduced the amount of time between referral and diagnosis of sleep apnea.
People (Stakeholder) Engagement
Several VA program offices provided resources and technical support for HSAT expansion and promoted the initiative as an organizational priority. This alignment of stakeholders at the outset allowed for expedited development of infrastructure. At the San Francisco VA, groups of local and regional stakeholders also played key roles including the (1) facility director and leadership team, (2) sleep clinicians, (3) respiratory therapists, (4) sleep technologists, (5) scheduling clerks, (6) human resource specialists, (7) procurement staff, (8) mailroom personnel, (9) biomedical engineers, (9) information technologists, and (11) patients. Engaging each of these groups required an understanding of local organizational structure and roles.
The local clinical champion started by arranging one-on-one meetings with each of the service chiefs or clinical leads responsible for organizational units that would be affected by the intervention. That service chief or clinical lead would then identify who in their organizational unit should be involved in subsequent meetings with the local champion. For example, planning meetings with procurement and mailroom staff were required to arrange purchasing, receiving, cataloging, and testing of the HSAT devices. Separate planning meetings with clinical staff were required for respiratory therapists and sleep technologists to learn how to mail HSAT devices to patients, educate patients on usage, upload study results, and clean recorders for reuse.
Problem Solving
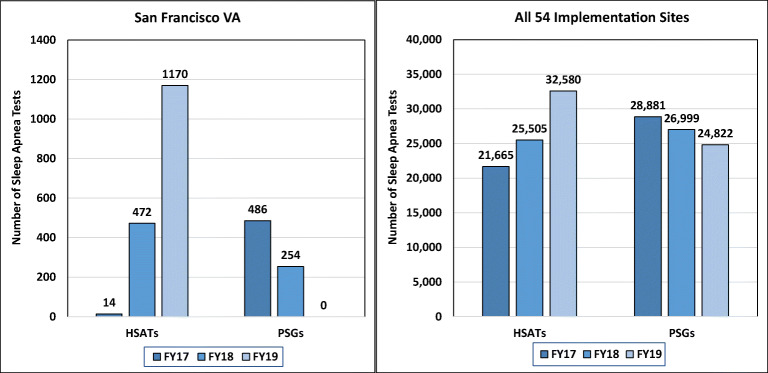
Several problems arose during HSAT implementation. Initially, negotiating contracts with HSAT vendors led to significant delays in equipment acquisition. After procurement, equipment had to be categorized and inventoried by local biomedical device offices. A new workflow had to be established for mailing HSAT devices to patients, enclosing postage-paid return packaging to ensure device retrieval and downloading and interpreting recordings. At each step, a new set of stakeholders were engaged, and new process mapping cycles were required to understand workflows and develop targeted solutions. As a result, the number of HSATs sharply increased between fiscal years 17 and 19, and the number of PSGs was reduced to zero (Fig. 3). A national contract for purchasing and distributing HSAT devices at the San Francisco VA was eventually established to streamline implementation and enhance further dissemination.
Figure 3.
Number of overnight sleep tests completed using home sleep apnea testing (HSAT) or polysomnography (PSG) during fiscal years 17, 18, and 19.
In summary, successful implementation relies on the following: (1) people (stakeholder) engagement, (2) process mapping, and (3) problem solving. It involves motivated individuals working together to engage stakeholders, understand workflow processes, and overcome barriers in the delivery of evidence-based care. These three strategies are straightforward, intuitive, and do not require extensive training in implementation science. We hope that frontline teams will be empowered to apply these tools to their daily practice and embrace continued efforts to improve the efficiency and effectiveness of Learning Healthcare Systems.
Funding
Dr. Lu is supported by the VA Quality Scholars Program funded through the VA Office of Academic Affiliations (Grant AF-3Q-09-2019-C), Department of Veterans Affairs, Veterans Health Administration. This work was funded by the VA Health Services Research & Development Quality Enhancement Research Initiative (QUERI) and by the VA Office of Rural Health.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Implementation Science Information and Resources - Fogarty International Center @ NIH. https://www.fic.nih.gov/ResearchTopics/Pages/ImplementationScience.aspx. Accessed May 12, 2019.
- 2.Bauer MS, Kirchner J. Implementation science: What is it and why should I care? Psychiatry Res. April 2019:112376. 10.1016/j.psychres.2019.04.025 [DOI] [PubMed]
- 3.Kirchner JE, Smith JL, Powell BJ, Waltz TJ, Proctor EK. Getting a clinical innovation into practice: An introduction to implementation strategies. Psychiatry Res. July 2019:112467. 10.1016/j.psychres.2019.06.042 [DOI] [PMC free article] [PubMed]
- 4.Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10(1):21. doi: 10.1186/s13012-015-0209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leeman J, Birken SA, Powell BJ, Rohweder C, Shea CM. Beyond “implementation strategies”: classifying the full range of strategies used in implementation science and practice. Implement Sci. 2017;12(1):125. doi: 10.1186/s13012-017-0657-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kilbourne AM, Goodrich DE, Miake-Lye I, Braganza MZ, Bowersox NW. Quality Enhancement Research Initiative Implementation Roadmap: Toward Sustainability of Evidence-based Practices in a Learning Health System. Med Care. 2019;57:S286–S293. doi: 10.1097/MLR.0000000000001144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Antonacci G, Reed JE, Lennox L, Barlow J. The use of process mapping in healthcare quality improvement projects. Health Serv Manage Res. 2018;31(2):74–84. doi: 10.1177/0951484818770411. [DOI] [PubMed] [Google Scholar]
- 8.Langley GJ, Moen RD, Nolan KM, Nolan TW, Norman CL, editors. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2. ed. San Francisco, Calif: Jossey-Bass; 2009. [Google Scholar]
- 9.D’Andreamatteo A, Ianni L, Lega F, Sargiacomo M. Lean in healthcare: A comprehensive review. Health Policy. 2015;119(9):1197–1209. doi: 10.1016/j.healthpol.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 10.George ML, Maxey J, Rowlands DT, Upton M. David. Lean Six Sigma Pocket Toolbook. New York, USA: McGraw-Hill Professional Publishing; 2004. [Google Scholar]
- 11.Nowak M, Pfaff H, Karbach U. Does Value Stream Mapping affect the structure, process, and outcome quality in care facilities? A systematic review. Syst Rev. 2017;6(1):170. doi: 10.1186/s13643-017-0563-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goodman MS, Sanders Thompson VL. The science of stakeholder engagement in research: classification, implementation, and evaluation. Transl Behav Med. 2017;7(3):486–491. doi: 10.1007/s13142-017-0495-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4(1):50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Concannon TW, Meissner P, Grunbaum JA, et al. A New Taxonomy for Stakeholder Engagement in Patient-Centered Outcomes Research. J Gen Intern Med. 2012;27(8):985–991. doi: 10.1007/s11606-012-2037-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miech EJ, Rattray NA, Flanagan ME, Damschroder L, Schmid AA, Damush TM. Inside help: An integrative review of champions in healthcare-related implementation. SAGE Open Med. 2018;6:205031211877326. doi: 10.1177/2050312118773261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roberts JP, Fisher TR, Trowbridge MJ, Bent C. A design thinking framework for healthcare management and innovation. Healthcare. 2016;4(1):11–14. doi: 10.1016/j.hjdsi.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 17.Christoff P. Running PDSA cycles. Curr Probl Pediatr Adolesc Health Care. 2018;48(8):198–201. doi: 10.1016/j.cppeds.2018.08.006. [DOI] [PubMed] [Google Scholar]