Abstract
Background
In Germany as elsewhere, standardized recommendations are lacking on the avoidance of physical exertion to protect the abdominal wall in patients who have recently undergone abdominal surgery. It is unclear how much stress the abdominal wall can withstand and how long the patient should be exempted from work. The goal of this review is to determine whether there are any standardized, evidence-based recommendations for postoperative care from which valid recommendations for Germany can be derived.
Methods
We systematically searched the literature for evidence-based recommendations on exertion avoidance after abdominal surgery, as well as for information on the extent to which postoperative abdominal wall stress contributes to incisional hernia formation. We then created a questionnaire on recommendation practices and sent it to all of the chiefs of general and visceral surgery services that were listed in the German hospital registry (1078 chiefs of service as of June 2016).
Results
All 16 of the included studies on postoperative exertion avoidance contained low-level evidence that could only be used to formulate weak recommendations (“can,” rather than “should” or “must”). Some 50 000 incisional hernia repair procedures are performed in Germany each year, with a reported incidence of 12.8% in the first two years after surgery. The scientifically documented risk factors for incisional herniation are related to techniques of wound closure, the suture materials used, wound infections, and the patient risk profile. From the biological point of view, the abdominal wall regains full, normal resistance to exertional stress 30 days after a laparotomy with uncomplicated healing. Most incisional hernias (>50%) arise 18 months or more after surgery; they are more common in patients who have avoided exertion for longer periods of time (more than 8 weeks). Our questionnaire was returned by 386 surgical clinics. The responses showed that 78% of recommendations were based on personal experience only. The recommendations varied widely; exertion avoidance was recommended for as long as 6 months.
Conclusion
The dilemma of a deficient evidence base for postoperative exertion avoidance to protect the abdominal wall should be resolved with the much higher-quality evidence available from hernia research, which concerns the patient population with the biologically least favorable starting conditions. Based on our analysis of the available literature in light of the biomechanical principles of abdominal wall healing, we propose a new set of recommendations on postoperative exertion avoidance after abdominal surgery, with the goal of eliminating excessively protracted exertion avoidance and enabling a timely return to work.
cme plus
This article has been certified by the North Rhine Academy for Continuing Medical Education. Participation in the CME certification program is possible only over the Internet: http://daebl.de/RY95.
The deadline for participation is 29 October 2021.
According to the Federal Statistical Office, 885 000 general and visceral surgical procedures with an approach through the abdominal wall were performed and coded in Germany in the year 2018. These included 198 942 cholecystectomies, 124 942 appendectomies, and 241 499 procedures on the small and large bowel. There were also 319 734 hernia operations, 176 105 of them for inguinal hernia (1). Counting figures from all surgical specialties, approximately 1.4 million operations are performed through an abdominal approach in Germany each year. In the postoperative and rehabilitation phases, the avoidance of incisional herniation is an important goal of treatment. In recent years, approximately 50 000 operations for incisional hernia have been carried out in Germany each year (1). The actual incidence of incisional hernia can only be estimated. According to pertinent studies, the incidence of incisional hernia is 12.8% in the two years after the index procedure (95% confidence interval [11.4; 14.2]) (2). Dietz et al. derive this figure for Germany from the available data, with approximately 104 000 cases per year (3). According to meta-analyses, incisional hernias arise significantly less often after laparoscopic procedures than after open surgery (4.3% vs. 10.1%, risk difference -0.06 [-0.09; -0.03]; p = 0.0002) (4). The risk factors promoting incisional hernia formation have been identified in hernia research on the basis of very large case numbers.
The aim of the present review is to investigate this group of topics systematically. We examine the current state of the evidence on whether, and to what extent, postoperative strain of the abdominal wall, or its avoidance, affects the development of incisional hernias. We inquire whether any recommendations on exertion avoidance to spare the abdominal wall are already in place in other countries, and, if so, to what extent these are transparent, individualized, and evidence-based. In the absence of current recommendations for Germany, we consider what postoperative recommendations for exertion avoidance can best be derived from the available evidence. To complement this information, we have carried out our own survey of German surgical services to study the current practice of recommendations on postoperative exertion avoidance after abdominal surgery in Germany (box 1).
BOX 1. Results of a survey of surgical services across Germany on recommendations for avoiding physical exertion to protect the abdominal wall after abdominal surgery.
To obtain an overview of current recommendations on exertion avoidance, a pertinent questionnaire was sent to the chiefs of general and visceral surgery services across Germany.
• Methods of the survey
The survey was sent to every surgical service in all of the German federal states listed in the German Hospital Register (Deutsches Krankenhaus Verzeichnis) as of 30 June 2016 under the heading of general and/or visceral surgery (37). This questionnaire on postoperative recommending practices, developed on the basis of the pertinent literature, contained 17 questions with a total of 132 answering options. The 1078 chiefs of these services received the questionnaire by mail and were entered into the study for further analysis if they answered it and sent it back. Questions were asked about recommendations for postoperative exertion avoidance that were typically given to patients on the service in question in order to protect the abdominal wall after laparotomy (both longitudinal and transverse) and laparoscopy. A very important question concerned the basis for the recommendations. The original questionnaire (in German) can be seen under eFragebogen.
The statistical analysis was performed with IBM SPSS Statistics Version 25. Frequencies are reported with descriptive statistical methods, such as the numerical mean, standard deviation, median, and corresponding percentages.
• Results of the survey of surgical services
35.8% of the questionnaires were returned (386 of 1078 questionnaires). Most surgical services made recommendations to their patients for postoperative care (93% after laparotomy, 77% after laparoscopy). The recommended duration of exertion avoidance ranged from 1 to 24 weeks after laparotomy and from 0 to 12 weeks after laparoscopy. Pain-adapted restrictions on heavy lifting after surgery were recommended by26.2% of services after laparotomy and by 49.5% after laparoscopy. Even though nearly all of the surgical service gave postoperative recommendations concerning exertion avoidance, only 9.6% indicated that they did so on the basis of the current scientific evidence (this question could be answered by stating one or multiple bases for the recommendations given). 27.3% gave recommendations based on expert opinion, and more than three-quarters (78.2%) based on personal experience. The services that recommended supportive abdominal corsets after surgery did so for one in five patients who had undergone a laparotomy. 31.7% of services recommended time off from work after laparotomy, with a mean duration of 2.98 weeks (SD = 1.30) and a median duration of three weeks; other recommendations were non-uniform and involved periods of three to eight weeks. 26% recommended time off from work after laparoscopy, for periods ranging from one to four weeks. The results are summarized in Table 1 and discussed in the Results section together with the findings of the literature review.
Method of the literature search
We carried out a systematic search for recommendations regarding postoperative exertion after abdominal surgery in the PubMed (Medline) and Cochrane Library databases, according to the specifications of the PRISMA guidelines. The search was performed without any restriction on the date of publication (1 January 1962 to 8 May 2019). Two reviewers acting independently of each other sought publications in German or English with the searching strategy and searching terms (MeSH – Medical Subject Headings) indicated in Box 2.
BOX 2. Literature searching criteria in Medline/PubMed.
#1 Keyword, Abstract, Title
laparotomy OR abdominal surgery OR visceral surgery OR prostatectomy OR appendectomy OR cholecystectomy OR gynaecological surgery OR urological surgery OR hernia OR colectomy
#2 Keyword, Abstract, Title
return to work after OR recommendation OR advice OR return to normal activities OR functional convalescence OR convalescence advice OR consensus on restriction OR physical activity restriction OR postoperative activity restrictions
Results: #1 AND #2
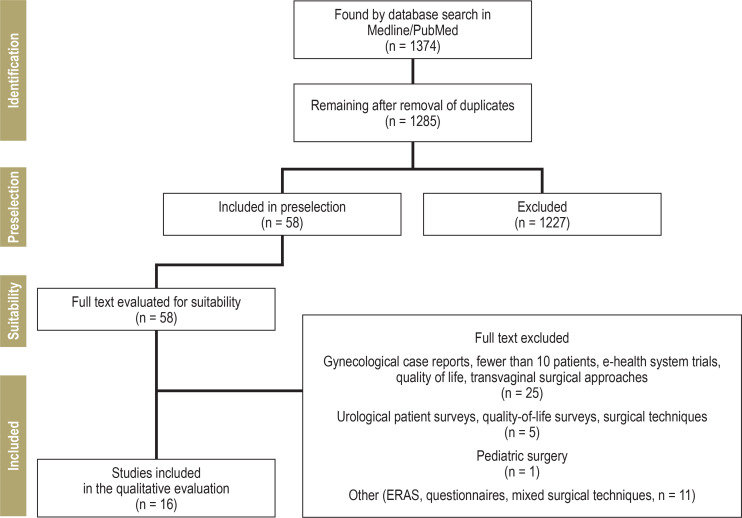
1374 studies were identified, of which 1285 remained after the removal of duplicates. The abstracts were analyzed for relevance; of the 58 selected studies, the full texts of 16 were considered suitable for inclusion. The PRISMA literature search flowchart is shown in the Diagram. In addition, an online search for information relevant to the topicwas carried out in the accessible internet sites of governmental health institutions from abroad.
Moreover, the results of the literature search on postoperative recommendations to avoid exertion were considered in conjunction with data from hernia research (including research on incisional hernias) in order to shed light on the topics of wound healing and fascial healing, abdominal wall biomechanics, and the incidence of incisional hernias and hernia recurrence.
Frequencies are reported here with descriptive statistical techniques, because the inhomogeneity of the underlying studies does not permit any valid comparative data analysis.
Results of the literature search
Recommendations on the avoidance of exertion
The literature search revealed heterogeneous proposals for postoperative recommendations on exertion avoidance. 16 studies were identified, of which 11 were from the fields of general and visceral surgery, and five were gynecological. Three studies concerned open operative techniques only, seven concerned laparoscopic techniques only, and six concerned both.
In 12 studies, the information provided on postoperative exertion avoidance was based on expert opinion and was therefore classified as low-level evidence. Two of the included studies were systematic reviews on postoperative management after inguinal hernia surgery. It was concluded in one review that 1–2 days of exertion avoidance after surgery are sufficient, and in the other that exertion should be avoided until the wound has healed (5, 6). These two inguinal hernia studies have not only the highest case numbers of all included studies, but also—because they are systematic reviews—the highest evidence level as well. A selective review of the literature on incisional hernia surgery (3) concluded with a recommendation that exertion should be avoided for three to six weeks, depending on the operative technique. Studies yielding high-level evidence were not found. In five publications on laparoscopic cholecystectomy, the recommended period of exertion avoidance ranged from an individually determined period, to 48 hours, to one or two weeks. The longest recommended periods (up to 12 weeks) were after transabdominal hysterectomy (7, 8). The findings from the included studies with respect to the recommended duration of stress avoidance after abdominal surgery are summarized in Table 2. Highly variable individual recommendations can be accessed on the websites of hospitals, surgical services, and private surgical practices in Europe and the USA; these are not listed here. No evidence-based national recommendations or guidelines of health organizations or specialty societies were found. The Internet site of the National Health Service (NHS) of the United Kingdom contains, under the heading “Get well soon,” lists of recommendations compiled by the Royal College of Surgeons with specific information on what patients should do after various types of surgery, including cholecystectomy and hernia-repair procedures (9).
Table 2. Overview of the studies included in the literature review concerning recommendations for avoiding physical exertion and staying away from work after abdominal surgery.
| Authors | Country | Year | Quality of study | Type of operation or procedure | Recommended time to avoid exertion | Recommended time away from work |
| Paasch C, Anders M, Strick W (e10) | DE | 2018 | Expert survey | Open incisional hernia repair | 4 weeks | No information |
| Dietz UA et al. (3) | DE | 2018 | Selective literature reviewExpert opinion | Laparoscopic and open incisional hernia repair | 3–6 weeks, then adapted to pain; shorter after laparoscopy | No information |
| Pommergaard HC, et al. (38) | SWE | 2014 | Expert survey | Laparoscopic colectomy Open colectomy |
0–6 weeks 0–6 weeks |
No information |
| van Vliet, DCR, et al (e3) | NL | 2016 | Expert consensus (Delphi method) |
Open hernia operation Laparoscopic cholecystectomy Laparoscopic appendectomy Open appendectomy Laparoscopic colectomy Open colectomy |
1 week 1–2 weeks 1–2 weeks 1–2 weeks 3–4 weeks 4 weeks |
2 weeks 2 weeks 2 weeks 2 weeks 6 weeks 8 weeks |
| Callesen T, et al. (e9) | DAN | 1998 | Expert opinion | Laparoscopic cholecystectomy | 48 h | 1 week |
| Oikkonen M, et al. (e11) | FIN | 2001 | Expert opinion Patient survey |
Laparoscopic cholecystectomy | Individualized | Individualized |
| Bisgaard T (e12) | DAN | 2005 | Expert opinion | Laparoscopic cholecystectomy | 1 week | 1 week |
| Royal College of Surgeons (9) | UK | 2019 | Expert opinion | Laparoscopic cholecystectomy Inguinal hernia repair |
7–13 days Light physical work: 1 –2 weeks Mild lifting: 2 – 3 weeks Heavy physical labor: 6 weeks |
10–14 days Light physical work: 1 –2 weeks Mild lifting: 2 – 3 weeks Heavy physical labor: 6 weeks |
| Buhck H, Untied M, Bechstein WO (5) | DE | 2012 | Systematic review | Inguinal hernia repair | Until the wound is healed | Depending on pain, after wound healing |
| Tolver MA, et al. (6) | DAN | 2016 | Systematic review | Laparoscopic inguinal hernia repair | 1–2 days | No information |
| Grewal P (e13) | UK | 2014 | Expert survey Insurance survey |
Inguinal hernia repair | 1–12 weeks | 1–12 weeks |
| Bouwsma EVA, et al. (e14) | NL | 2017 | Prospective cohort study | Laparoscopic gynecological operations | Individualized | Individualized |
| Deffieux X, et al. (e15) | FRA | 2011 | Expert survey | Laparoscopic sacral colopexy | 4 weeks | 4 weeks |
| Moller CM, et al. (7) | NL | 2001 | Expert survey | Open hysterectomy | 2–12 weeks | 1–12 weeks |
| Vonk Noordegraaf A, et al. (e16) | NL | 2011 | Expert consensus (Delphi method) |
Laparoscopic adnexal procedures and hysterectomies Open hysterectomies |
2 weeks 3 weeks 6 weeks |
2 weeks 3–4 weeks 6 weeks |
| Clayton M, Verow P (8) | UK | 2007 | Expert survey | Open hysterectomies | 2–12 weeks | 2–12 weeks |
Results of hernia research
Data from the literature on incisional hernia formation imply that its causes lie in the various wound closure techniques and suture materials used, wound infections, and, in particular, the patient-specific risk profile (10). With regard to wound-closure techniques, the incisional hernia rate has been found to be lower when a running suture with absorbable suture material is used (medium or slow absorption rate), sewn with the “small bites” technique in a 4:1 suture-to-wound length ratio (10– 15). Predisposing patient-specific risk factors include age over 45 years, BMI over 25 kg/m2, an increased amount of subcutaneous fat, laparotomy of the upper abdomen or multiple laparotomies, preoperative chemotherapy, diabetes, blood transfusions, abdominal aortic aneurysm surgery, bariatric procedures, and preexisting incisional hernia (2, 11, 16, 17). Moreover, many authors describe a significant correlation between postoperative wound infections and an approximately fourfold elevation of the incisional hernia rate (18– 20).
Biomechanical studies have shown that the abdominal wall regains its normal resistance to strain after four weeks of normal healing (21– 24). Everyday stresses that cannot easily be voluntarily avoided, such as coughing, pressing to defecate, and standing up from a sitting position, actually put the abdominal wall under greater stress (in terms of dynamics and maximal force development) than the lifting or carrying of moderately heavy objects (25). As early as the 1960s, Bellis and Lichtenstein reported recurrence rates comparable to those seen today with “immediate return to unrestricted work after inguinal herniorrhaphy” (26).
Bellis repeated this recommendation in 1992 in a new publication based on data from over 27 000 patients (27). It was hypothesized that shooting pains in the postoperative period arising during sudden elevations of the intra-abdominal pressure might be associated with recurrent inguinal herniation, but this could not be confirmed even in large-scale meta-analyses (28). An evaluation of the Danish hernia registry, published in 2014, with data from nearly 35,000 male patients revealed no effect of heavy lifting after surgery, or of the amount of weight lifted, on the need for reoperation for recurrent inguinal hernia (29). The analysis showed that patients who had been exempted from work for longer times (>8 weeks) were actually more likely to need surgery for a recurrence. This observation was confirmed in other studies (3, 30). Animal experiments have shown that the resistance of midline abominal incisions to tearing returns to the initial state after 28 days of uncomplicated healing (31). Other authors have also concluded that the fascia heals in approximately 30 days (21).
Incisional hernias tend to arise long after the index operation. A retrospective study showed that only 7% of the expected incisional hernias arise within the first year, and more than 50% at 18 months or later (32). Other authors have described a 60% relative increase in incisional herniation one to three years after primary laparotomy (33, 16). The frequent late occurrence of incisional herniation suggests that there is an endogenous predisposition to hernia formation, and this hypothesis is supported by studies showing an association with impaired collagen metabolism. Tissue samples from patients with incisional hernias were found to contain larger quantities of immature collagen III and an altered composition of matrix metalloproteinases (34, 35). These abnormalities, found in tissues distant from the hernia as well, suggest a genetic defect of collagen that is present independently of time and thus does not justify prolonged periods of exertion avoidance (36). There is presumably a group of patients with endogenous generalized weakness of the connective tissue who are at especially high risk of incisional herniation.
Discussion
The therapeutic objectives of any procedure that violates the integrity of the abdominal wall must include, along with the success of the primary intervention, an optimal result of treatment and rehabilitation, in which normal function is restored and incisional herniation is avoided. The findings of the literature review presented here underscore the paucity of evidence and the lack of uniform recommendations for postoperative management and exertion avoidance after abdominal surgery. As 13 of the 16 studies are based on expert opinion and expert surveys, they cannot be used to derive anything more than weak recommendations (“can” at best, rather than “should” or “must”). In Germany, non-uniform recommendations on these matters are given by surgeons and by the general practitioners and rehabilitation physicians who care for the patients after their discharge from the hospital. Yet it is precisely these doctors providing postoperative care who need to receive standardized recommendations on postoperative management from the surgeons who perform the procedures. Uncertainty in their minds about how to proceed can lead, in doubtful cases, to protracted periods of exertion avoidance, supposedly to protect the abdominal wall, and excessively long periods have indeed been documented. Moreover, publications from other countries (the United Kingdom and the Netherlands) have shown that periods of exemption from work in Germany are sometimes much longer even than the highly variable periods that are recommended (36, 38).
The state of the evidence on postoperative avoidance of physical exertion to protect the abdominal wall after abdominal surgery poses a dilemma. In Germany, a recommendation for prolonged exertion avoidance is generally said to be justified because the physicians caring for the patient afterward think this will lower the risk of incisional herniation. Yet, if one examines the scientific evidence on the causes of incisional herniation, one finds that prolonged reduction of abdominal wall stress is not an independent factor; rather, endogenous biological factors that are specific to the individual patient seem to play a leading role (32, 36). Risk factors, and patients at risk, can be identified accordingly. There are no data at all showing that avoidance of exertion for more than 30 days can lower the incisional herniation rate, nor is there any scientific evidence suggesting that the early resumption of normal physical activity raises it. In view of the long latency between the index procedure and the development of an incisional hernia, it seems clear that endogenous factors are the major cause of incisional hernias, and that avoiding exertion for more than four weeks after surgery cannot lower their incidence in patients with normal wound healing.
The weak evidence base for recommendations to avoid exertion will probably not become any stronger in the foreseeable future. Our approach to a solution involves studying a group of patients for whom high-level evidence is available, and who are presumably biologically predisposed to have greater difficulties with stable abdominal wall healing than normal persons: namely, patients with hernias.
Our survey revealed that most treating physicians in Germany (93% after laparotomy, 77% after laparoscopy) make recommendations for further management. Given the absence of scientific evidence that could serve as a guide, it is understandable that 90% of the recommendations are based on personal experience (8). Accordingly, the recommendations reported in the responses to the survey vary widely. Major variation is seen not only in the recommended periods of time in which the patient should avoid physical exertion, but also in restrictions on lifting and in the maximum weight that the patient is allowed to lift.
Two-thirds of the surgeons surveyed reported that they told their patients to lift no more than a specified weight in kilograms (5/10/15 kg). Yet in vivo pressure measurements have shown that the slow lifting of weights of up to 50 mg, in the absence of abdominal pressing, raises the intra-abdominal pressure only by a small or marginal amount; thus, the danger of controlled lifting, even of heavy weights, in the postoperative period is apparently exaggerated (39). The intra-abdominal pressure rises many times higher, and more suddenly as well, with jumping, coughing, or pressing—that is, with the scarcely avoidable exertions of everyday life (25, 39, 40). Abdominal pressing (the Valsalva maneuver) doubles the intra-abdominal pressure (40). From the socioeconomic point of view, postoperative loss of working days by patients with inguinal hernias is the most expensive component of surgical treatment (e1). It has been shown that patients themselves consider the ability to return to work after surgery to be an important goal, second only to the success of the treatment itself (e2).
We have seen that there are no uniform recommendations for postoperative exertion avoidance, or for the duration of work exemptions, for patients who have undergone cholecystectomy, appendectomy, or visceral or colonic procedures, whether laparoscopic or conventional. In view of the deficient evidence base, the guidelines of the European Hernia Society contain no recommendation on the manner or duration of postoperative exertion avoidance to prevent incisional herniation (10). As for current practice elsewhere, publications from other European countries (e3– e6) reveal that the recommended durations of exemption from work are shorter there than they are reported to be in Germany—either the durations reported in our own survey among German surgical service chiefs, or the even longer ones, of up to six months, that are mentioned in social-medicine publications (e7). In the Netherlands, expert panels have voted on standardized postoperative management regimens after uncomplicated laparoscopic cholecystectomy, appendectomy, colon surgery, and hernia surgery. Future studies are intended to investigate the efficacy and implementability of these regimens in practice (e3).
Important evidence is likely to come, in the near future, from a randomized, prospective, multicenter Swiss trial that is now in the recruitment phase, which is intended to study the effect of early postoperative abdominal wall muscle training on wound healing, pain, and incisional herniation (e8).
The limitations of the present review are due to the heterogeneity and weakness of the evidence base from international studies, which severely restrict our ability to compare the results on recommendations about avoiding exertion A higher questionnaire response rate would have been desirable as well—although a large number (386) of questionnaires were returned to us, this was only 35.8% of those sent—and it might have been informative to stratify the questionnaires by the type of institution responding (university hospital, general hospital, or certified hernia center).
In summary, we have found that no robust data exist to support a medical recommendation for avoiding physical exertion after abdominal surgery for more than four weeks after primary wound healing. There is no evidence, either, to support any specific upper limit for the amount of weight that the patient is allowed to lift during the period of restricted activity, and, in any case, the abdominal wall strain caused by lifting heavy objects is considerably less than that which accompanies coughing or sneezing. Findings from hernia research suggest that moderate physical exertion actually promotes wound healing after abdominal surgery, rather than impairing it (36). Recommendations to avoid exertion and stay away from work for excessively long periods are detrimental to the patient who is willing to work, and they in fact increase the likelihood of incisional herniation (5, 29, 30). Scientific data gathered over more than 70 years from patients undergoing hernia procedures (a group that already possesses a risk factor for incisional herniation, namely, a disturbance of endogenous collagen synthesis) show no link between early postoperative resumption of full physical activity and an increased incidence of incisional herniation or recurrent inguinal herniation. What justification remains, then, for telling patients who want to go back to work that they should avoid physical exertion and stay away from work for three to six months (e7)?
The timing of resumption of normal physical activity and of the return to work are essentially determined by the patient’s expectations as to recovery from surgery, by the physician’s recommendations, and by the degree of postoperative pain experienced (e1, e9). Thus, recommendations to avoid exertion are not wholly determinative in themselves, but they can lead, in case the physician caring for the patient after surgery is more cautious than the scientific evidence warrants, to unnecessarily restricted physical activity for months at a time, and to an inappropriate delay of the return to health. We therefore propose, in consideration of the findings reported in the literature, the recommendations that are summarized in Table 3.
Table 3. Recommendations on the duration of postoperative exertion avoidance to protect the abdominal wall*.
| Recommendation | Laparoscopy | Combined procedures | Laparotomy |
| Bed rest | None | None | None |
| Level of exertion | |||
| Physical activites of daily life | Immediately | Immediately | Immediately |
| Rehabilitative exercises and other rehabilitation measures | As soon as the wound is healed | As soon as the wound is healed | As soon as the woundis healed |
| Sports – Endurance sports – Ball sports, weight training, athletics |
1 week 2 weeks |
3 weeks 4 weeks |
4 weeks 4 weeks |
| Resumption of work | |||
| Sitting/standing | 1–2 weeks | 2–3 weeks | 4 weeks |
| Hard physical labor | 2–3 weeks | 3–4 weeks | 4 weeks |
*These recommendations apply in the setting of normal primary wound healing and should be adapted to the pain experienced by the patient.
Conclusion
Our review of the literature revealed that no evidence-based recommendations exist concerning the avoidance of physical exertion after abdominal surgery, either in Germany or in other countries. Our survey among chiefs of surgical services across Germany revealed that such recommendations are generally based on personal experience or expert opinion, as they also tended to be in the studies from Germany and abroad that we evaluated in the review. In Germany, the recommendations are remarkably variable; in the manner and duration of the restrictions that are advised, they outstrip the recommendations typically given in neighboring European countries. Fascial healing after abdominal surgery with normal primary wound healing is complete after 30 days, and incisional hernia formation presumably has endogenous causes. It follows that there is no scientific support for a recommendation to avoid exertion for more than four weeks, or to delay the return to work unnecessarily. Such measures do nothing to prevent incisional herniation even in patients who are predisposed to it. Patients, surgeons, physicians (general practitioners and others) caring for patients after their operations, medical social services, and health insurers are now in need of valid, standardized recommendations on the return to normal physical activity after surgery.
Table 1. Summarized results of the postal survey conducted across Germany,with evaluation of the 386 returned questionnaires (95% confidence intervals in brackets).
| Postoperative recommendations | After laparotomy | After laparoscopy |
|
Avoidance of exertion: yes Duration Postoperative lifting (max.): 5 kg 10 kg 15 kg adapted to pain |
358 (92.7%) [90; 95]0–24 weeks mean after longitudinal laparotomy 5.79 weeks [5.57; 6.11] transverse laparotomy 5.42 weeks [5.08; 5.75] 122 (34.1%) [29; 39] 125 (34.4%) [29; 39] 21 (5.8%) [1; 11] 95 (26.2%) [21; 31] |
296 (77.5%) [73; 82] 0–12 weeks mean after laparoscopy 2.54 [2.34; 2.73] 58 (18.4%) [14; 23] 81 (25.7%) [21; 30] 20 (6.3%) [4; 9] 156 (49.5%) [44; 55] |
|
Mode of recommendation:
– oral – written – both Based on: – scientific evidence – expert opinion – personal experience – other |
121 (33%) 4 (1.1%) 242 (65.9%) 37 (10.5%) [7; 14] 105 (29.7%) [25; 35] 276 (78.2%) [74; 83] 31 (8.8%) [6; 12] |
|
|
Abdominal corset: yes Duration in weeks (mean) Abstention from sexual intercourse: yes Duration in weeks (mean) Abstention from sports: yes Duration in weeks (mean) Recommended time off from work: yes Duration in weeks (mean) |
81 (22.2%) [18; 26] 4.28 [3.67; 4.89] 21 (5.7%) [3; 8] 3.14 [2.54; 3.74] 309 (84.2%) [80; 88] 4.70 [4.42; 4.98] 116 (31.7%) [27; 36] 2.98 [2.73; 3.22] |
2 (0.5%) [0; 1] 3.0 [not measurable] 11 (3%) [1; 5] 2.82 [1.88; 3.76] 217 (59.3%) [54; 64] 2.40 [2.22; 2.58] 100 (27.3%) [23; 32] 1.84 [1.68; 2.0] |
Figure.
DIAGRAM
PRISMA flowchart of the literature search on postoperative avoidance of physical exertion to protect the abdominal wall
ERAS, Enhanced Recovery After Surgery
Questions on the article in Issue 44/2020:
Lack of Standardized Advice on Physical Strain Following Abdominal Surgery
The submission deadline is 29 October 2021. Only one answer is possible for each question. Please select the most appropriate answer.
Question 1
How many operations for incisional hernia are performed in Germany each year?
20 000
50 000
80 000
100 000
130 000
Question 2
Which of the following are among the patient-specific risk factors for the development of an incisional hernia?
upper abdominal laparotomy or multiple laparotomies, and BMI >25 kg/m2
age under 50 and preoperative chemotherapy
preoperative parturition and age over 45
BMI >25 kg/m2 and surgery for a thoracic aortic aneurysm
a low subcutaneous fat fraction and diabetes mellitus
Question 3
According to biomechanical studies, how many weeks after surgery does the abdominal wall regain its original resistance to strain, with normal wound healing?
2
4
8
10
12
Question 4
What is known about the timing of incisional hernia development after the index procedure?
30% of incisional hernias arise in the first 10 days.
Most incisional hernias arise in the first 8 weeks by mechanical stress.
Only 30% of incisional hernias arise in the first year after surgery.
Most incisional hernias arise 18 months or more after surgery.
Incisional hernias become increasingly unlikely as time elapses.
Question 5
On what basis, according to a survey of surgical services across Germany, are recommendations generally made concerning the avoidance of exertion of abdominal surgery?
the scientific evidence
expert opinion
international guidelines
a German S3 guideline
personal experience
Question 6
What recommendation is made by more than half of the doctors in a German nationwide survey of surgical services to their patients who have undergone laparotomy or laparoscopy?
avoiding sports, generally for 2–5 weeks
wearing an abdominal corset for at least 4 weeks
avoiding sexual intercourse, generally for 2–4 weeks
staying away from work, generally for 2–3 weeks
not lifting anything heavier than 5 kg
Question 7
According to a literature review, which of the following types of procedure is associated with the longest recommended periods of avoidance of physical exertion (up to 12 weeks)?
laparoscopic cholecystectomy
open or laparoscopic appendectomy
open colectomy
open hysterectomy
laparoscopic sacral colopexy
Question 8
According to studies on tissue samples, what is presumably associated with an endogenous predisposition to hernia formation?
a fibrocyte deficiency
a deficiency of matrix metalloproteases
impaired collagen metabolism
defective cartilage formation
an adipocyte deficiency
Question 9
What do the authors of this article recommend with respect to postoperative exertion avoidance after laparoscopy, laparotomy, and combined procedures (in patients with primary wound healing, and adapted to pain in the individual case)?
Everyday activities can be resumed in 2–3 weeks, and rehabilitation can be begun in 1 week.
Rehabilitation exercises, other postoperative rehabilitative treatments, and endurance sports can be started/resumed as soon as the wound is healed.
Everyday activities can be resumed immediately, and the patient should stay home from work for 6 weeks.
Hard physical labor should not be performed for at least 8 weeks.
Everyday activities can be resumed immediately, and rehabilitation exercises and other postoperative rehabilitative treatments can be begun as soon as the wound is healed.
Question 10
Which of the following is true of the evidence base concerning the development of incisional hernias after abdominal surgery and their avoidance?
Studies have shown that suturing techniques and suture materials have no effect on the incisional hernia rate.
There is no evidence indicating that restricting physical exertion for more than 30 days after surgery lowers the incisional hernia rate.
Patient-specific endogenous biological factors play a relatively minor role, according to the available scientific evidence.
Studies have shown that early resumption of full physical activity elevates the incisional hernia rate.
There are no data indicating any way to identify risk factors or patients at risk.
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement The authors state that they have no conflict of interest.
This article contains results from Carsten Weber’s doctoral thesis. The authors thank Oberstabsarzt Dr. Ines Richardsen for her collaboration.
References
- 1.Statistisches Bundesamt. Operationen und Prozeduren der vollstationären Patientinnen und Patienten in Krankenhäusern (4-Steller) www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Krankenhaeuser/Publikationen/Downloads-Krankenhaeuser/operationen-prozeduren-5231401177014.html (last accessed on 29 March 2020) [Google Scholar]
- 2.Bosanquet DC, Ansell J, Abdelrahman T, et al. Systematic review and meta-regression of factors affecting midline incisional hernia rates: analysis of 14,618 patients. PLoS One. 2015;10 doi: 10.1371/journal.pone.0138745. e0138745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dietz UA, Menzel S, Lock J, Wiegering A. The treatment of incisional hernia. Dtsch Arztebl Int. 2018;115:31–37. doi: 10.3238/arztebl.2018.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kössler-Ebs JB, Grummich K, Jensen K, et al. Incisional hernia rates after laparoscopic or open abdominal surgery—a systematic review and meta-analysis. World J Surg. 2016;40:2319–2330. doi: 10.1007/s00268-016-3520-3. [DOI] [PubMed] [Google Scholar]
- 5.Buhck H, Untied M, Bechstein WO. Evidence-based assessment of the period of physical inactivity required after inguinal herniotomy. Langenbecks Arch Surg. 2012;397:1209–1214. doi: 10.1007/s00423-012-1008-7. [DOI] [PubMed] [Google Scholar]
- 6.Tolver MA, Rosenberg J, Bisgaard T. Convalescence after laparoscopic inguinal hernia repair: a qualitative systematic review. Surg Endosc. 2016;30:5165–5172. doi: 10.1007/s00464-016-4863-4. [DOI] [PubMed] [Google Scholar]
- 7.Moller C, Ottesen M, Kehlet H, Ottesen BS. Convalescence recommendations after hysterectomy A study of opinions among Danish physicians. Ugeskr Laeger. 2001;163:7043–7047. [PubMed] [Google Scholar]
- 8.Clayton M, Verow P. Advice given to patients about return to work and driving following surgery. Occup Med (Lond) 2007;57:488–491. doi: 10.1093/occmed/kqm063. [DOI] [PubMed] [Google Scholar]
- 9.Royal College of Surgeons. Get well soon after cholecystectomy. www.rcseng.ac.uk/patient-care/recovering-from-surgery/gall-bladder/. (last accessed on 9 July 2019) [Google Scholar]
- 10.Muysoms FE, Antoniou SA, Bury K, et al. European Hernia Society guidelines on the closure of abdominal wall incisions. Hernia. 2015;19:1–24. doi: 10.1007/s10029-014-1342-5. [DOI] [PubMed] [Google Scholar]
- 11.Höer J, Lawong G, Klinge U, Schumpelick V. Factors influencing the development of incisional hernia A retrospective study of 2,983 laparotomy patients over a period of 10 years. Chirurg. 2002;73:474–480. doi: 10.1007/s00104-002-0425-5. [DOI] [PubMed] [Google Scholar]
- 12.Diener MK, Voss S, Jensen K, Büchler MW, Seiler CM. Elective midline laparotomy closure: the INLINE systematic review and meta-analysis. Ann Surg. 2010;251:843–856. doi: 10.1097/SLA.0b013e3181d973e4. [DOI] [PubMed] [Google Scholar]
- 13.Israelsson LA, Millbourn D. Prevention of incisional hernias: how to close a midline incision. Surg Clin North Am. 2013;93:1027–1040. doi: 10.1016/j.suc.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 14.Millbourn D, Cengiz Y, Israelsson LA. Effect of stitch length on wound complications after closure of midline incisions: a randomized controlled trial. Arch Surg. 2009;144:1056–1059. doi: 10.1001/archsurg.2009.189. [DOI] [PubMed] [Google Scholar]
- 15.Deerenberg EB, Harlaar JJ, Steyerberg EW, et al. Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. Lancet. 2015;386:1254–1260. doi: 10.1016/S0140-6736(15)60459-7. [DOI] [PubMed] [Google Scholar]
- 16.Itatsu K, Yokoyama Y, Sugawara G, et al. Incidence of and risk factors for incisional hernia after abdominal surgery. Br J Surg. 2014;101:1439–1447. doi: 10.1002/bjs.9600. [DOI] [PubMed] [Google Scholar]
- 17.Yamada T, Okabayashi K, Hasegawa H, et al. Age, preoperative subcutaneous fat area, and open laparotomy are risk factors for incisional hernia following colorectal cancer surgery. Ann Surg Oncol. 2016;23(Suppl 2):236–241. doi: 10.1245/s10434-015-4462-y. [DOI] [PubMed] [Google Scholar]
- 18.Walming S, Angenete E, Block M, Bock D, Gessler B, Haglind E. Retrospective review of risk factors for surgical wound dehiscence and incisional hernia. BMC Surg. 2017;17 doi: 10.1186/s12893-017-0207-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sorensen LT, Hemmingsen UB, Kirkeby LT, Kallehave F, Jorgensen LN. Smoking is a risk factor for incisional hernia. Arch Surg. 2005;140:119–123. doi: 10.1001/archsurg.140.2.119. [DOI] [PubMed] [Google Scholar]
- 20.Llaguna OH, Avgerinos DV, Lugo JZ, et al. Incidence and risk factors for the development of incisional hernia following elective laparoscopic versus open colon resections. Am J Surg. 2010;200:265–269. doi: 10.1016/j.amjsurg.2009.08.044. [DOI] [PubMed] [Google Scholar]
- 21.Lau FH, Pomahac B. Wound healing in acutely injured fascia. Wound Repair Regen. 2014;22(Suppl 1):14–17. doi: 10.1111/wrr.12165. [DOI] [PubMed] [Google Scholar]
- 22.Dubay DA, Wang X, Kirk S, Adamson B, Robson MC, Franz MG. Fascial fibroblast kinetic activity is increased during abdominal wall repair compared to dermal fibroblasts. Wound Repair Regen. 2004;12:539–545. doi: 10.1111/j.1067-1927.2004.012506.x. [DOI] [PubMed] [Google Scholar]
- 23.Franz MG, Smith PD, Wachtel TL, et al. Fascial incisions heal faster than skin: a new model of abdominal wall repair. Surgery. 2001;129:203–208. doi: 10.1067/msy.2001.110220. [DOI] [PubMed] [Google Scholar]
- 24.Höer J, Anurov M, Titkova S, et al. Influence of suture material and suture technique on collagen fibril diameters in midline laparotomies. Eur Surg Res. 2000;32:359–367. doi: 10.1159/000052218. [DOI] [PubMed] [Google Scholar]
- 25.Weir LF, Nygaard IE, Wilken J, Brandt D, Janz KF. Postoperative activity restrictions: any evidence? Obstet Gynecol. 2006;107:305–309. doi: 10.1097/01.AOG.0000197069.57873.d6. [DOI] [PubMed] [Google Scholar]
- 26.Bellis CJ. Inguinal Herniorrhaphy: immediate return to unrestricted work Surgical techniques using local anesthesia and results in 5903 personal cases. Ind Med Surg. 1964;33:721–725. [PubMed] [Google Scholar]
- 27.Bellis CJ. Immediate return to unrestricted work after inguinal herniorrhaphy Personal experiences with 27,267 cases, local anesthesia, and mesh. Int Surg. 1992;77:167–169. [PubMed] [Google Scholar]
- 28.Hendry PO, Paterson-Brown S, de Beaux A. Work related aspects of inguinal hernia: a literature review. Surgeon. 2008;6:361–365. doi: 10.1016/s1479-666x(08)80009-1. [DOI] [PubMed] [Google Scholar]
- 29.Vad MV, Frost P, Svendsen SW. Occupational mechanical exposures and reoperation after first-time inguinal hernia repair: a prognosis study in a male cohort. Hernia. 2015;19:893–900. doi: 10.1007/s10029-014-1339-0. [DOI] [PubMed] [Google Scholar]
- 30.Svendsen SW, Frost P, Vad MV, Andersen JH. Risk and prognosis of inguinal hernia in relation to occupational mechanical exposures - a systematic review of the epidemiologic evidence. Scand J Work Environ Health. 2013;39:5–26. doi: 10.5271/sjweh.3305. [DOI] [PubMed] [Google Scholar]
- 31.Höer J, Klinge U, Schachtrupp A, Töns C, Schumpelick V. Influence of suture technique on laparotomy wound healing: an experimental study in the rat. Langenbecks Arch Surg. 2001;386:218–223. doi: 10.1007/s004230000196. [DOI] [PubMed] [Google Scholar]
- 32.Höer J, Lawong G, Klinge U, Schumpelick V. Factors influencing the development of incisional hernia A retrospective study of 2,983 laparotomy patients over a period of 10 years. Chirurg. 2002;73:474–480. doi: 10.1007/s00104-002-0425-5. [DOI] [PubMed] [Google Scholar]
- 33.Fink C, Baumann P, Wente MN, et al. Incisional hernia rate 3 years after midline laparotomy. Br J Surg. 2014;101:51–54. doi: 10.1002/bjs.9364. [DOI] [PubMed] [Google Scholar]
- 34.Klinge U, Zheng H, Si Z, et al. Expression of the extracellular matrix proteins collagen I, collagen III and fibronectin and matrix metalloproteinase-1 and -13 in the skin of patients with inguinal hernia. Eur Surg Res. 1999;31:480–490. doi: 10.1159/000008728. [DOI] [PubMed] [Google Scholar]
- 35.Rosch R, Junge K, Knops M, Lynen P, Klinge U, Schumpelick V. Analysis of collagen-interacting proteins in patients with incisional hernias. Langenbecks Arch Surg. 2003;387:427–432. doi: 10.1007/s00423-002-0345-3. [DOI] [PubMed] [Google Scholar]
- 36.Franz MG. The biology of hernia formation. Surg Clin North Am. 2008;88:1–15, vii. doi: 10.1016/j.suc.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Deutsches Krankenhausverzeichnis. www.deutsches-krankenhaus-verzeichnis.de/suche/Regional.html (last accessed on 30 June 2016) [Google Scholar]
- 38.Pommergaard HC, Burcharth J, Danielsen A, Angenete E, Haglind E, Rosenberg J. No consensus on restrictions on physical activity to prevent incisional hernias after surgery. Hernia. 2014;18:495–500. doi: 10.1007/s10029-013-1113-8. [DOI] [PubMed] [Google Scholar]
- 39.Iqbal A, Haider M, Stadlhuber RJ, Karu A, Corkill S, Filipi CJ. A study of intragastric and intravesicular pressure changes during rest, coughing, weight lifting, retching, and vomiting. Surg Endosc. 2008;22:2571–2575. doi: 10.1007/s00464-008-0080-0. [DOI] [PubMed] [Google Scholar]
- 40.Cobb WS, Burns JM, Kercher KW, Matthews BD, James Norton H, Todd Heniford B. Normal intraabdominal pressure in healthy adults. J Surg Res. 2005;129:231–235. doi: 10.1016/j.jss.2005.06.015. [DOI] [PubMed] [Google Scholar]
- E1.Bay-Nielsen M, Knudsen MS, Christensen JK, Kehlet H. Cost analysis of inguinal hernia surgery in Denmark. Ugeskr Laeger. 1999;161:5317–5321. [PubMed] [Google Scholar]
- E2.Hoang CD, Osborne MC, Maddaus MA. Return to work after thoracic surgery: an overlooked outcome measure in quality-of-life studies. Thorac Surg Clin. 2004;14:409–416. doi: 10.1016/S1547-4127(04)00026-X. [DOI] [PubMed] [Google Scholar]
- E3.van Vliet DCR, van der Meij DE, Bouwsma EV, et al. A modified Delphi method toward multidisciplinary consensus on functional convalescence recommendations after abdominal surgery. Surg Endosc. 2016;30:5583–5595. doi: 10.1007/s00464-016-4931-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E4.Vonk Noordegraaf A, Anema JR, Louwerse MD, et al. Prediction of time to return to work after gynaecological surgery: a prospective cohort study in the Netherlands. BJOG. 2014;121:487–497. doi: 10.1111/1471-0528.12494. [DOI] [PubMed] [Google Scholar]
- E5.Dahl S, Steinsvik EA, Dahl AA, Loge JH, Cvancarova M, Fossa SD. Return to work and sick leave after radical prostatectomy: a prospective clinical study. Acta Oncol. 2014;53:744–751. doi: 10.3109/0284186X.2013.844357. [DOI] [PubMed] [Google Scholar]
- E6.Kingdom GovUK. Medical guidance for DLA and AA decision makers (adult cases): staff guide. www.gov.uk/government/publications/medical-guidance-for-dla-and-aa-decision-makers-adult-cases-staff-guide (last accessed on 8 May 2019) [Google Scholar]
- E7.Vahlensiek W, Sawal O, Hoffmann H. Springer. 7. Vol. 18. Berlin, Heidelberg, New York: 2011. Urologische Erkrankungen Deutsche Rentenversicherung Bund: Sozialmedizinische Begutachtung für die gesetzliche Rentenversicherung; 415 pp. [Google Scholar]
- E8. www.clinicaltrials.gov/ct2/show/NCT03808584#contacts (last accessed on 10 April 2020) [Google Scholar]
- E9.Callesen T, Klarskov B, Mogensen TS, Kehlet H. Ambulatory laparoscopic cholecystectomy Feasibility and convalescence. Ugeskr Laeger. 1998;160:2095–2100. [PubMed] [Google Scholar]
- E10.Paasch C, Anders S, Strik MW. Postoperative-treatment following open incisional hernia repair: a survey and a review of literature. Int J Surg. 2018;53:320–325. doi: 10.1016/j.ijsu.2018.04.014. [DOI] [PubMed] [Google Scholar]
- E11.Oikkonen M, Purola-Löfstedt M, Mäkinen MT, Aromaa U. Convalescence in the first week after laparoscopic cholecystectomy: results from a detailed questionnaire on morbidity and recovery of daily activities. Surg Endosc. 2001;15:94–97. doi: 10.1007/s004640000190. [DOI] [PubMed] [Google Scholar]
- E12.Bisgaard T. Sick leave and convalescence after laparoscopic cholecystectomy? Ugeskr Laeger. 2005;167:2627–2629. [PubMed] [Google Scholar]
- E13.Grewal P. Survey of post-operative instructions after inguinal hernia repair in England in 2012. Hernia. 2014;18:269–272. doi: 10.1007/s10029-013-1075-x. [DOI] [PubMed] [Google Scholar]
- E14.Bouwsma EVA, Anema JR, Vonk Noordegraaf A, de Vet HCW, Huirne JA. Using patient data to optimize an expert-based guideline on convalescence recommendations after gynecological surgery: a prospective cohort study. BMC Surg. 2017;17 doi: 10.1186/s12893-017-0317-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E15.Deffieux XT, Thubert R, de Tayrac H, et al. Convalescence recommendations after incontinence and pelvic organ prolapse surgery: a study of opinions among French surgeons. J Gynecol Obstet Biol Reprod. 2011;40:29–35. doi: 10.1016/j.jgyn.2010.11.002. [DOI] [PubMed] [Google Scholar]
- E16.Vonk Noordegraaf A, Huirne JA, Brölmann HA, van Mechelen W, Anema JR. Multidisciplinary convalescence recommendations after gynaecological surgery: a modified Delphi method among experts. BJOG. 2011;118:1557–1567. doi: 10.1111/j.1471-0528.2011.03091.x. [DOI] [PubMed] [Google Scholar]