Abstract
Meta-analyses have shown that digital mental health apps can be efficacious in reducing symptoms of depression and anxiety. However, real-world usage of apps is typically not sustained over time, and no studies systematically examine which features increase sustained engagement with apps or the relationship between engagement features and clinical efficacy. We conducted a systematic search of the literature to identify empirical studies that (1) investigate standalone apps for depression and/or anxiety in symptomatic participants and (2) report at least one measure of engagement. Features intended to increase engagement were categorized using the persuasive system design (PSD) framework and principles of behavioral economics. Twenty-five studies with 4159 participants were included in the analysis. PSD features were commonly used, whereas behavioral economics techniques were not. Smartphone apps were efficacious in treating symptoms of anxiety and depression in randomized controlled trials, with overall small-to-medium effects (g = 0.2888, SE = 0.0999, z(15) = 2.89, p = 0.0119, Q(df = 14) = 41.93, p < 0.0001, I2 = 66.6%), and apps that employed a greater number of engagement features as compared to the control condition had larger effect sizes (β = 0.0450, SE = 0.0164, t(15) = 2.7344, p = 0.0161). We observed an unexpected negative association between PSD features and engagement, as measured by completion rate (β = −0.0293, SE = 0.0121, t(17) = 02.4142, p = 0.0281). Overall, PSD features show promise for augmenting app efficacy, though engagement, as reflected in study completion, may not be the primary factor driving this association. The results suggest that expanding the use of PSD features in mental health apps may increase clinical benefits and that other techniques, such as those informed by behavioral economics, are employed infrequently.
Subject terms: Anxiety, Depression, Psychology
Introduction
Digital mental health interventions are proliferating rapidly, garnering heightened interest from the public as well as the scientific community. Well over 10,000 mental health apps are now available for download1, and multiple meta-analyses demonstrate that apps are modestly efficacious in treating symptoms of depression and anxiety2–5. However, an analysis of real-world usage of mental health apps show that user engagement over time is low, with a median 15-day retention of only 3.9%6. Apps with features that increase engagement have generally been associated with greater reductions in depression and anxiety symptoms than apps that lack engagement features5. No study systematically examines which features increase engagement with apps or the relationship between the number of engagement features and clinical efficacy.
Persuasive system design (PSD) is a framework that identifies four mechanisms through which app features increase user engagement: facilitating the primary purpose of the app, promoting user-app interactions, leveraging social relationships, and increasing app credibility7 (Supplementary Table 1). PSD is rooted in research on human-computer interaction and computer-mediated communication and is in part adapted from concepts of persuasive technology7,8. These categories allow for comprehensive and objective consideration of the characteristics of technologies. Specific PSD features predict adherence among internet-based health and lifestyle interventions, which suggests that incorporating PSD features may improve adherence in health apps as well 7.
Behavioral economics is focused on understanding ways that human decision-making differs from what would be expected in traditional economic models of “rational” actors9. A comprehensive list of behavioral economics techniques has not been delineated, but common findings include that people are motivated by avoiding losses10, “starting fresh,”11 committing to action12, and by lotteries13 (Supplementary Table 2). These techniques from behavioral economics can be applied to “gamification,” the use of game-like experiences in non-game services, to further improve user engagement14–17. Gamification features, including points, badges, levels, and avatars, are used to increase engagement and may enhance apps’ intended effects16. In one head-to-head comparison of a gamified vs non-gamified versions of a smartphone app for anxiety, the gamified app was found to elicit significantly greater engagement, demonstrating the potential of behavioral economics for improving engagement with mental health apps18. PSD, behavioral economics, and gamification often overlap and identify a wide variety of techniques that increase engagement with smartphone apps.
Though smartphone apps show potential for treating depression and anxiety, a barrier to their real-world efficacy may be a lack of sustained user engagement19. Understanding the extent to which the engagement features of PSD techniques, behavioral economics, and/or gamification translate into improvements in engagement and mood outcomes may inform the development and deployment of more efficacious apps for anxiety and depression. We therefore conducted a systematic review of the literature and meta-analysis on smartphone apps for depression and anxiety with the aim of evaluating the impact of persuasive design and behavioral economics techniques on both engagement and clinical outcomes.
Results
Included studies
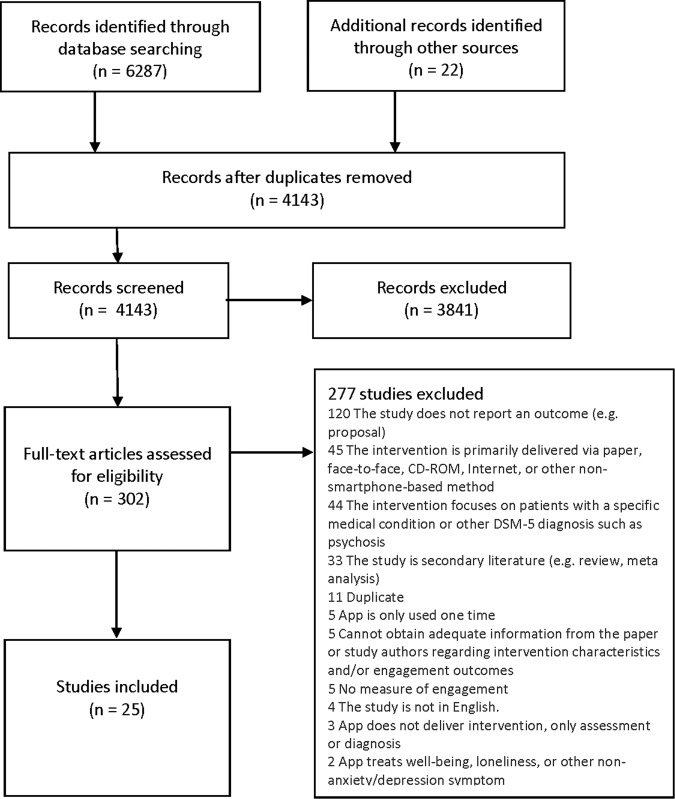
The full systematic search retrieved a total of 6287 results. Following the removal of duplicate articles and the later addition of articles cited by included studies, 4143 articles were screened by the title and abstract for relevance. After title and abstract screening, 302 articles were identified as potentially eligible and were screened in full. Full-text screening excluded 277 articles for reasons specified in Fig. 1, which details the full PRISMA search and screening process.
Fig. 1. PRISMA flowchart.
Flow diagram of article selection process.
After full text screening, 25 independent studies were found to be eligible for inclusion in the systematic review (Table 1)20–44. Ten studies were non-randomized trials, while 15 were randomized controlled trials. In addition, 3 of the trials were unpublished, including one pre-print and two dissertations. Across all studies, there were 4159 participants total, with 2905 participants using 29 unique smartphone apps. The participants ranged from 13 to 76 years old, with an average age of 32.9. The majority of participants were female (66.6%). The majority of studies required participants to report significant symptoms of major depressive disorder (19) or generalized anxiety disorder (5), and symptoms were most commonly identified by scoring above a predetermined threshold on a validated self-assessment questionnaire.
Table 1.
Study characteristics.
| Type of study (N = 25) | |
| RCT | 15 articles |
| Pilot/quasi experimental | 10 articles |
| Gray literature (N = 3) | |
| Dissertation | 2 articles |
| Pre-Print | 1 article |
| Apps (N = 29) | |
| Participant demographics (N = 4159) | |
| Average age (Min–Max) (years) | 32.9 (13–76) |
| Female (%) | 66.6 |
| Diagnosis of study participants | |
| Major depressive disorder | 19 studies |
| Generalized anxiety disorder | 5 studies |
| Social anxiety disorder | 3 studies |
| Dysthymia | 1 study |
| Other depressive disorder | 1 study |
| Method of symptom evaluation | |
| Self-identification | 2 studies |
| Validated self-assessment measure | 19 studies |
| Clinician-administered measure or medical record | 8 studies |
| Study length (Weeks) | |
| Average Length of Intervention (Min–Max) | 5.82 (2–12) |
Control conditions included waitlist, treatment as usual, non-app control intervention, or placebo app control conditions (Supplementary Table 3). Average intervention duration was 5.8 weeks (standard deviation 2.8 weeks), with a range of 2–12 weeks. Most studies accounted by drop out by conducting an intention to treat analysis or by removing missing cases (Supplementary Table 4).
Quality assessment
According to the Joanna Briggs Institute critical appraisal checklist for quasi-experimental studies45, among the 10 quasi-experimental studies, 2 were rated to be high quality, 6 were medium quality, and 2 were low quality. According to the Cochrane Collaboration Revised Risk of Bias tool46, among the 15 randomized controlled trials, 0 were judged to have an overall low risk of bias, 8 were judged to raise some concerns for bias, and 7 were judged to be at high risk of bias.
App content
Across all studies, 29 unique smartphone apps were used, including experimental and control apps. The apps offered a variety of content (Supplementary Table 5), the most common being behavioral techniques (76%), cognitive techniques (72%), and psychoeducation (69%). Some apps provided means to track behavior (45%), mood (38%), or thoughts (21%). Relaxation techniques and mindfulness techniques were each used in 31% of apps. Fewer apps tracked physiological parameters such as sleep or exercise (10%) or tracked clinical symptoms of anxiety or depression (7%).
Safety and privacy
Safety features such as assessing for suicidality and providing resources for suicidality were reported in a minority of apps (14% and 17%, respectively). For 20% of apps, a privacy policy was available as specified in the study. Additional privacy and security features such as encryption and password protection were reported for 27% of apps (Supplementary Table 6).
Accessibility
Of the 29 apps assessed, 41% were available to the public through the Apple App Store, Google Play, or both (Supplementary Table 7). The remaining apps were accessible to research participants only, or their accessibility was not specified. The majority of apps were free or had free versions available.
Persuasive system design
Overall, apps used an average of 6.5 out of the 28 total features of PSD and 2.5 of the 4 total categories of PSD (Tables 2 and 3). Primary task support was most commonly used, with an average of 3.30 (SD 1.26) out of 7 total features. Social support was least commonly used, with an average of 0.37 (SD 0.93) out of 7 total features.
Table 2.
Components of persuasive design.
| App | Primary task support | Dialogue support | Social support | Credibility support |
|---|---|---|---|---|
| Aptivate27 | X | X | ||
| BA Intervention33 | X | X | X | |
| Be Good to Yourself31 | X | X | X | |
| Boost Me40 | X | X | ||
| Calm37 | X | X | ||
| CBMA28 | X | X | ||
| CBMA Control28 | X | X | ||
| El Buen Consejo Movil24 | X | X | X | X |
| EVO20,38 | X | X | X | |
| FOCUS22 | X | X | X | |
| Get Happy Program43 | X | X | X | |
| Health Tips20,38 | X | X | ||
| iCBT41 | X | |||
| iCouch CBT27 | X | |||
| Intellicare25,36 | X | X | X | |
| Mindfulness App33 | X | X | ||
| Mobile Sensing and Support42 | X | X | ||
| Moodivate26 | X | X | ||
| MoodKit26 | X | X | ||
| MoodMission21 | X | X | ||
| MT-Phoenix32 | X | X | ||
| Pacifica23,35 | X | X | X | X |
| Plus Connect44 | X | X | X | X |
| PUSH-D34 | X | X | ||
| Superbetter CBT39 | X | X | X | X |
| Superbetter General39 | X | X | X | X |
| Thought Challenger41 | X | |||
| Todac Todac29 | X | X | X | |
| Wysa30 | X | X | X |
Table 3.
Average persuasive system design features and categories.
| Persuasive system design feature | Mean (SD) | Min | Max |
|---|---|---|---|
| Primary task support | 3.30 (1.26) | 1 | 6 |
| Dialogue support | 1.93 (1.20) | 0 | 4 |
| Social support | 0.37 (0.93) | 0 | 4 |
| Credibility support | 0.90 (1.24) | 0 | 4 |
| Total features | 6.50 (2.60) | 2 | 12 |
| Total categories | 2.50 (0.90) | 1 | 4 |
Total features in each category = 7; total categories = 4.
Table 4 describes the number and percentage of apps that used each PSD feature or category. Of note, features of credibility support were most difficult to evaluate as most articles did not describe these features in detail, and 81.4% of ratings were marked as “unable to assess.” The most frequently used features (reduction − 86.7%, self-monitoring − 70.0%, personalization − 53.3%) all belonged to the primary task support category. The least frequently used features were not used in any of the apps (cooperation, competition, recognition, third-party endorsements, and verifiability) and belonged to the dialogue support category or credibility support category.
Table 4.
Frequency of PSD features.
| Feature | App with feature | % apps with feature |
|---|---|---|
| Reduction | 26 | 86.7% |
| Tunneling | 11 | 36.7% |
| Tailoring | 12 | 40.0% |
| Personalization | 16 | 53.3% |
| Self-monitoring | 21 | 70.0% |
| Simulation | 1 | 3.3% |
| Rehearsal | 12 | 40.0% |
| Total primary task support features across all apps | 99 | |
| Praise | 7 | 23.3% |
| Rewards | 7 | 23.3% |
| Reminders | 15 | 50.0% |
| Suggestion | 16 | 53.3% |
| Similarity | 5 | 16.7% |
| Liking | 6 | 20.0% |
| Social role | 2 | 6.7% |
| Total dialogue support features across all apps | 58 | |
| Social learning | 3 | 10.0% |
| Social comparison | 2 | 6.7% |
| Normative influence | 1 | 3.3% |
| Social facilitation | 5 | 16.7% |
| Cooperation | 0 | 0% |
| Competition | 0 | 0% |
| Recognition | 0 | 0% |
| Total social support features across all apps | 11 | |
| Trustworthiness | 7 | 23.3% |
| Expertise | 7 | 23.3% |
| Surface credibility | 10 | 33.3% |
| Real-world feel | 1 | 3.3% |
| Authority | 2 | 6.7% |
| Third party endorsements | 0 | 0% |
| Verifiability | 0 | 0% |
| Total credibility support features across all apps | 27 |
Behavioral economics
Overall, apps used an average of 0.17 out of the 4 total behavioral economics features (Supplementary Table 8). The most commonly used was the pre-commitment pledge, which was used in 4 apps. One app used loss aversion, whereas none of the apps used the fresh start effect or lottery.
Meta-analysis of effect of smartphone apps on depressive or anxiety symptoms
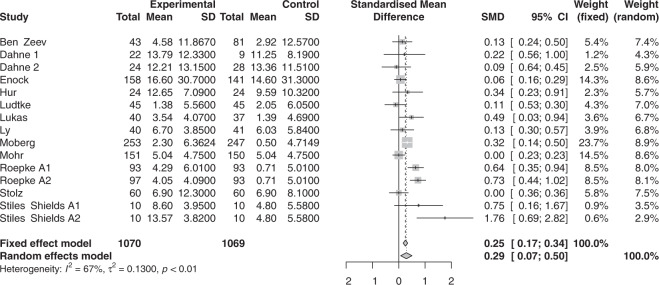
A random-effects meta-analysis of the effect of smartphone apps on depression and anxiety symptoms demonstrated a moderate positive effect size of smartphone apps for reducing pre versus post scores on depression and anxiety questionnaires (g = 0.6217, SE = 0.0669, t(25) = 9.2982, p < 0.001) (Fig. 2). Heterogeneity across studies was substantial (Q(df = 24) = 87.8894, p < 0.0001, I2 = 82.70%). Egger’s regression test indicated significant publication bias (p = 0.0135). A trim-and-fill analysis identified six missing studies (g = 0.5184, SE = 0.0803, z(31) = 6.4589, p < 0.001, Q(df = 30) = 125.7114, p < 0.0001, I2 = 87.57%).
Fig. 2. Random effects meta-analysis of app efficacy comparing pre-intervention to post-intervention change on an anxiety or depression symptoms.
Forest plot of random effects meta-analysis of app efficacy comparing pre-intervention to post-intervention change on an anxiety or depression symptoms.
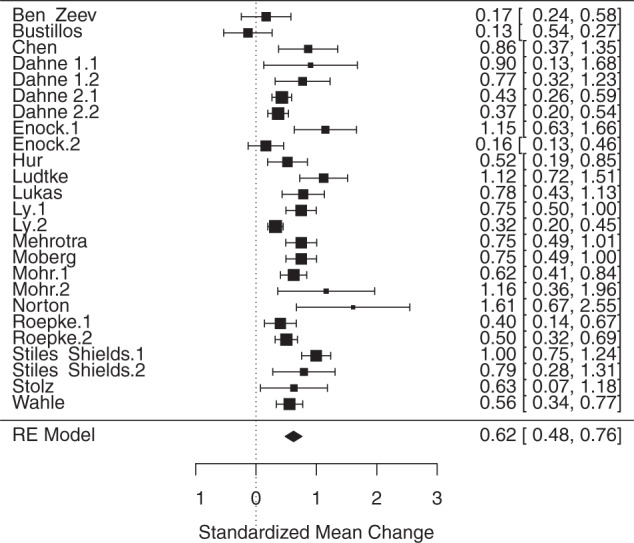
Figure 3 displays the pooled and individual effect sizes of smartphone apps on depression or anxiety when compared to control conditions in randomized controlled trials. A random-effects meta-analysis demonstrated a similar pattern as the pre/post meta-analysis of the full sample albeit with a smaller effect size (g = 0.2888, SE = 0.0999, z(15) = 2.89, p = 0.0119, Q(df = 14) = 41.93, p < 0.0001, I2 = 66.6%). Egger’s regression test indicated no publication bias (p = 0.47091). A trim-and-fill analysis identified one missing study (g = 0.2473, SE = 0.1254, t(16) = 1.97, p = 0.0672, Q(df = 15) = 49.72, p < 0.0001, I2 = 69.8%).
Fig. 3. Random effects meta-analysis in RCTs of app efficacy comparing change in anxiety or depression symptoms in apps vs. control.
Forest plot of random effects meta-analysis in RCTs of app efficacy comparing change in anxiety or depression symptoms in apps vs. control.
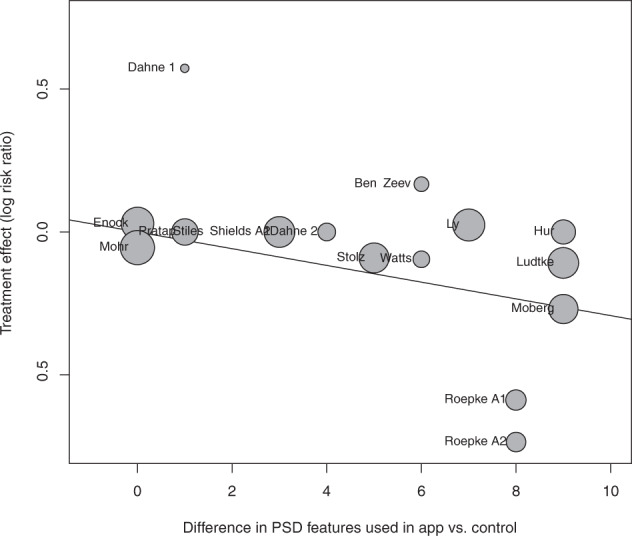
Meta-regression of PSD features and efficacy
Meta-regression analysis demonstrated that the magnitude of the effect size of improvement in mood in active relative to control conditions had a significant positive relationship with the difference in number of PSD features used in the app (β = 0.0450, SE = 0.0164, t(15) = 2.7344, p = 0.0161; Fig. 4), as well as with the difference in number of PSD categories (β = 0.1249, SE = 0.0362, t(15) = 3.4522, p = 0.0039).
Fig. 4. Mixed effects meta-regression analysis of difference in PSD features and efficacy for app vs control.
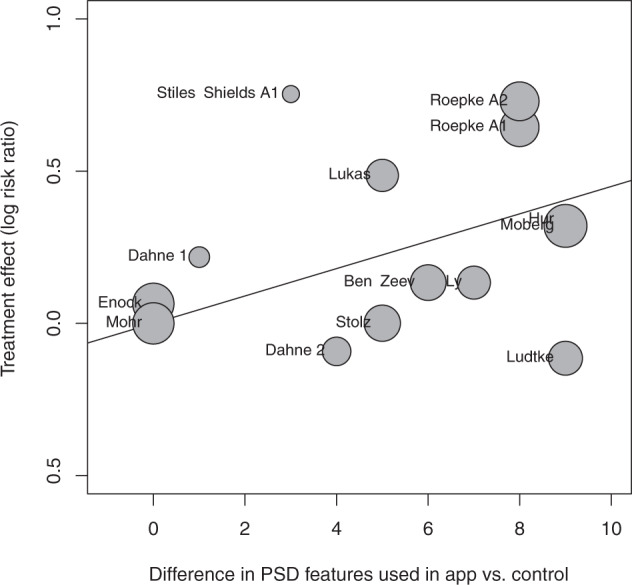
Bubble plot of mixed effects meta-regression analysis of difference in PSD features and efficacy for app vs control.
Meta-analysis of study completion rate
A random-effects meta-analysis of the study completion rate of app vs control conditions in randomized controlled trials revealed a significant effect, and heterogeneity was moderate to substantial (g = 0.8730, SE = 0.0761, z(17) = −1.79, p = 0.0931, Q(df = 16) = 41.33, p = 0.0005, I2 = 61.3%). Egger’s regression test indicated no publication bias (p = 0.2738). A trim-and-fill analysis identified no missing studies.
Meta-regression of PSD features and study completion rate
The study completion rate in the intervention compared to control condition had a significant negative relationship with the difference in number of PSD features (β = −0.0293, SE = 0.0121, t(17) = 02.4142, p = 0.0281; Fig. 5), as well as with the difference in number of PSD categories (β = −0.0830, SE = 0.0292, t(17) = −2.8472, p = 0.0116).
Fig. 5. Mixed effects meta-regression analysis of difference in PSD features and study completion rate for app vs control.
Bubble plot of mixed effects meta-regression analysis of difference in PSD features and study completion rate for app vs control.
Removal of outliers did not significantly impact any of the results (Supplementary Note 1).
Exploratory analyses
No direct association was found between efficacy and completion rate (g = −0.2134, SE = 0.1442, t(15) = −1.4806, p = 0.1609). Efficacy also did not meaningfully change the association between completion rate and PSD features (β = −0.0649, SE = 0.1434, p = 0.6588, F(df1 = 2, df2 = 12) = 0.8320, p = 0.4588). Including a regressor for the type of control condition (waitlist vs. active control) also did not meaningfully change the association between PSD features and study completion rate (β = −0.1900, SE = 0.1254, t(17) = −1.5150, p = 0.1520). Including a regressor for initial symptom severity did not meaningfully change the association between PSD features and study completion rate (β = −0.0949, SE = 0.0820, t(16) = −1.1566, p = 0.2682).
Discussion
The principal findings of this meta-analysis indicate that standalone smartphone apps for depression and anxiety are efficacious, with modest overall effects in randomized controlled trials (g = 0.2888). The efficacy findings are consistent with those shown in previous meta-analyses2–5. This meta-analysis is the first to demonstrate that apps that use a greater number of engagement features have larger clinical effects. Thus, the findings extend the extant literature by demonstrating the importance of engagement techniques to improve efficacy of app-based interventions for depression and anxiety. These findings can inform development and implementation of future apps.
A lack of engagement with mental health apps has been reported as a key limitation for realizing the potential of apps to broadly disseminate mental health treatments47. Apps that include guidance (i.e., from a therapist or coach) have generally been found to have larger effects than standalone interventions5,19,48. Given that standalone mental health apps require fewer resources than guided apps, identifying factors that might increase engagement and efficacy without therapist involvement could greatly improve dissemination efforts. “Engagement features” such as those elements of PSD have been found to increase engagement with mental health apps as measured by duration of use and completion of interventions7,49. Our review indicates that engagement features also are associated with increased clinical efficacy and therefore should be included in standalone mental health apps to increase their impact for broader dissemination.
The number of engagement features used in a given app had a significant negative association with study completion rate. The negative association between PSD features and engagement as measured by completion rate was contrary to our a priori hypothesis that PSD features would be associated with increased app completion and thereby increase efficacy. One possible interpretation of the negative association between PSD features and completion rates is that participants using apps with more PSD features may use the app more frequently, benefit more quickly, and lose motivation to continue using the app once their symptoms have improved compared to participants using less engaging apps; however, our exploratory analyses suggest that this is not the case. Additionally, we found that these results were not driven by the type of control condition or initial symptom severity. In subsequent studies, analyses of interim symptom change could help to better understand the association between PSD features and completion rates. Additionally, while completion rate was the most readily available measure of engagement, other engagement outcomes such as minutes spent using the app or self-reported user experience of the usefulness, usability, and satisfaction with the app50 might yield more meaningful information about PSD features and engagement.
We found that some PSD features were incorporated into all apps (e.g., primary task support), while others were less commonly used (e.g., social support), and behavioral economics features such as pre-commitment pledges, loss aversion, and lotteries, were rarely incorporated. The reason may be, in part, because of the historical roots of these literatures. PSD is well-established as an approach to development of new technologies and therefore may be more naturally incorporated into app development7,8. Behavioral economics has traditionally focused on economic decision-making51, then was applied to behavioral health52 but has only more recently been used in the context of mental health interventions53. The results of our meta-analysis suggest that increasing the number of engagement techniques may be beneficial, and so it is likely that designers may need to draw from a range of engagement approaches to maximize the impact of app-based interventions. Furthermore, elements such as social support, which span both the PSD and behavioral economics literatures, may be particularly promising6. Incorporating social support may also be the mostly likely way to engage patients without the use of therapists or coaches and, in itself, is a predictor of mental health outcomes 54.
There are several important limitations of the current review. The literature on mental health apps is heterogenous, and a number of studies included samples without psychiatric diagnoses and/or were used in combination with other interventions to varying degrees. Clearer standards for reporting on app content in research studies could help subsequent syntheses of the literature. In our review, all available information about app content, design elements, privacy and security features, and accessibility were extracted from descriptions and screenshots of the apps in the papers, appendices and supplementary materials. However, additional features may have been included in apps that were not described in these materials. Another limitation is the use of completion rate as the primary metric of engagement. While this approach has been used previously in mental health app engagement literature19 and is an accessible metric because it is reported in most studies, it may be a crude measure of engagement. The number of minutes spent using the app, number of logins, or number of modules completed (if applicable) may measure engagement more meaningfully55. Furthermore, the quality of engagement may be more likely to affect clinical outcomes as much as or even more than the duration of engagement. The issue of defining meaningful engagement has been gaining attention and will likely influence the next steps in measuring app engagement 56.
Overall, smartphone apps appear to be efficacious in decreasing anxiety and depression symptoms. The use of persuasive design features is associated with larger effect sizes and may be useful in increasing clinical efficacy. Relatively few mental health apps used non-PSD behavioral economics techniques, which have shown promise for increasing outcomes in app-based interventions for smoking cessation57, increasing physical activity for obese patients58, and adherence to diabetes medication59. Incorporating additional PSD and behavioral economics techniques that have been rarely used, but have shown promise (e.g., social support7) may further improve outcomes in mental health treatments.
Methods
Literature search
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for transparent, comprehensive reporting of methodology and results60. The review adhered to a strict protocol submitted for registration with PROSPERO on April 1, 2020 (ID 171194) before the start of analyses. The protocol review was ongoing as of December 4, 2020 (CRD42020171194): https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020171194.
A systematic search was performed of the following databases: Ovid Medline (ALL − 1946 to present); Ovid Embase (1974 to present); The Cochrane Library (Wiley); the Cumulative Index to Nursing and Allied Health Literature (CINAHL; EBSCO interface); PsycINFO (EBSCO); PsycArticle (EBSCO); and Ovid Allied and Complementary Medicine (AMED). Since the focus of the study was on published research trials conducted on the apps, searches were not carried out directly in the Google Play or the Apple App Store. Our search terms included combinations, truncations, and synonyms of “depression,” “social anxiety,” or “anxiety,” in combination with “mobile application” or “smartphone.” The search terms were adapted for use with all chosen bibliographic databases. Additional records were retrieved by checking the bibliographies of studies that met inclusion criteria. No language, article type, or publication date restrictions were used. Searches were completed in March and April 2020.
Eligibility criteria
Included articles were English-language empirical studies published in peer-reviewed publications, conference presentations, dissertations, and gray literature/unpublished work. The intervention was required to be delivered by smartphone app alone and to be delivered over time with the purpose of treating depression and/or anxiety (major depressive disorder, dysthymia, other depressive disorder, generalized anxiety disorder, and/or social anxiety disorder). Study participants could be any age but needed to identify as having depression and/or anxiety, either through clinical diagnosis or self-endorsement. To be included, studies had to report at least one measure of participant engagement (i.e., attrition, adherence, engagement, dropout).
Studies were excluded if: a) the intervention was delivered in part or entirely by a non-smartphone method; b) the study population was required to have a specific medical condition, other DSM-5 diagnosis, no diagnosis (healthy), or unspecified diagnosis, unless the study included a subgroup analysis of participants with depression and/or anxiety only; and c) adequate information regarding intervention characteristics and/or engagement outcomes could not be obtained from the paper or from contacting the study authors.
Data collection and analysis
Two of three raters (E.B., J.B., or A.W.) independently completed each of the following steps, and conflicts were resolved by another rater (M.S.).
Selection of articles
Titles and abstracts were evaluated against the inclusion and exclusion criteria. Studies that were deemed potentially relevant were next evaluated by their full text. Reasons for exclusion were recorded. When more than one publication of a study was found, the study with the most information was used for data analysis.
Data extraction
Data extracted included study identifiers, study characteristics, intervention characteristics, techniques to increase engagement, engagement measures, efficacy measures, app content, app modality, accessory interventions, and usability features. Techniques to increase engagement are described further in Supplementary Information. Only data that were explicitly reported in the publications were extracted. App profiles in the Google Play or Apple App Store were not accessed as we could not verify that features identified in the app profile were available in the version of the app referenced in the paper.
Study Identifiers: the first author’s last name and the publication year.
Study Characteristics: the population, comparator (if applicable), outcome, and study design. Participant demographics such as age and gender.
Intervention Characteristics: the intervention or cohort name, number of trial arms, primary condition, duration of intervention, duration of follow-up, modules to be completed, automated or guided delivery, format of delivery, and outcome measures.
Techniques to Increase Engagement: components of PSD as outlined in Kelders et al.7 include: primary task support (reduction, tunneling, tailoring, personalization, self-monitoring, simulation, and rehearsal), dialogue support (praise, rewards, reminders, suggestion, similarity, liking, and social role), and credibility support (trustworthiness, expertise, surface credibility, real-world feel, authority, third-party endorsements, and verifiability). Non-PSD behavioral economics techniques included loss aversion, fresh start effect, pre-commitment pledges, and financial incentives including lotteries. Each component or technique had a predefined definition and guideline for being coded as present. Additional information can be found in Supplementary Tables 1 and 2.
Measures of Engagement: adherence to study protocol, completion rate, amount of time spent in app, modules completed, features or exercises accessed, duration of use of app, or other. All available measures of engagement were recorded for each study.
Measures of Efficacy: change in score on a validated scale for depression or anxiety.
App Content: app content was categorized based on categories identified in previously published systematic evaluations of publicly available mental health apps6,61. App content included psychoeducation, cognitive techniques, behavioral techniques, mindfulness, relaxation, mood expression, tracking of mood patterns, tracking of thought patterns, tracking of behavior, tracking of symptoms, and tracking of physiological parameters.
App Modality: information on app modality was recorded when available. App modalities included text, graphs, photos, illustrations, videos/films, and others.
Safety, Privacy, and Accessibility Features: integration and accessibility features such as cost, availability to the public, safety features, and privacy protection features. These features were adapted from a framework for evaluating mobile mental health apps62.
Inter-rater agreement
At the title and abstract screening stage, inter-rater agreement was 93.8%. At the full-text screening stage, inter-rater agreement was 90.1%. At the engagement feature rating stage, inter-rater agreement was 82.6%. Disagreements were resolved by a third rater (M.S.) at the screening stages and by consensus at the feature rating stage.
Assessment of risk of bias
Non-randomized experimental studies were evaluated based on the Joanna Briggs Institute critical appraisal checklist for quasi-experimental studies to assess quality45. Because the Joanna Briggs Institute checklist does not assign specific ratings (“high,” “medium,” or “low”) to studies based on the number of criteria met, we adapted a rating system used in previously published systematic evaluations of mental health apps6,61. The methodological quality of each study was rated as: high (7–9 criteria have been fulfilled), medium (4–6 criteria have been fulfilled), or low (0–3 criteria have been fulfilled).
The Cochrane Collaboration Revised Risk of Bias tool was applied to randomized controlled trials46. Each RCT was assessed against five bias domains in order to produce a summary risk of bias assessment score for each domain and overall (low risk, some concerns, or high risk of bias) 46.
Data analysis
A meta-analysis was conducted to calculate a pooled effect size of treatment efficacy. To test pre- and post-test change scores on anxiety and depression questionnaires, we applied a random-effects model to account for the expected heterogeneity among the studies, given the variety of types of apps, duration of intervention, and other factors. If a study used multiple measures of anxiety and/or depression symptoms, then the instrument most frequently used among all studies was used to calculate efficacy so as to reduce heterogeneity. If an app was used in multiple independent studies, it was included multiple times. In supplementary analyses, we removed outliers, defined as studies with a 95% confidence interval of the effect size that did not overlap with the 95% confidence interval of the pooled effect size63. We compared analyses with and without outliers to determine whether the presence of outliers changed the observed results. Risk of publication bias was examined using Eggers’ regression, and Duval and Tweedie’s trim-and-fill analysis was used to re-calculate pooled dropout rates after statistically accounting for any studies that may have introduced publication bias64. The degree of statistical heterogeneity was quantified using I² values, with <25% representing low heterogeneity, 25–50% for low-to-moderate heterogeneity, 50–75% for moderate-to-substantial heterogeneity, and >75% for substantial heterogeneity63. τ2 was calculated using the Hartung–Knapp–Sidik–Jonkman (HKSJ) method, which is appropriate when there is a large degree of heterogeneity between studies.
A second meta-analysis was run to examine efficacy of apps compared to control conditions in randomized controlled trials. A random-effects model was again used given the expected heterogeneity among the studies. Efficacy was calculated as the pre/post change on a depression or anxiety scale. When a study had multiple control conditions, the active control condition was selected, as opposed to a waitlist or treatment-as-usual control. If an app was used in multiple studies, it was included multiple times. If a study used multiple apps, both apps were included if there was a non-app control condition. Otherwise, the intervention app was compared to the control app. To examine whether risk of bias score affected the efficacy, a subgroup analysis stratifying studies by risk of bias score was performed (Supplementary Note 1). Independent mixed-effects meta-regression models were run to examine how app efficacy was affected by the number of PSD features used in the app compared to the control condition, the number of PSD categories used in the app compared to the control condition, and the study completion rate of app users compared to the control condition. As the number of PSD features or categories denoted levels as opposed to continuous variables, the intercept was set to “false.”
A third meta-analysis examined the study completion rate of apps compared to control conditions in randomized controlled trials. Study completion rate was calculated as the proportion of enrolled and/or randomized study participants who remained in the study at the time the intervention ended. A random-effects model was again used given the expected heterogeneity among the studies. Procedures were otherwise the same as for the second meta-analysis and the meta-regression. In addition, in order to further explore the association between PSD features and completion rates, exploratory control analyses were conducted. An independent mixed-effects meta-regression model was run to examine how app efficacy affected study completion rate. Multiple meta-regressions were conducted to examine the relationship of various covariates to study completion rate: PSD features and efficacy, PSD features and type of control condition (waitlist vs. active control), and PSD features and initial symptom severity. Initial symptom severity was rated numerically based on the interpretation of the instrument used, with minimal or none rated as 0, mild as 1, moderate as 2, moderately severe as 3, and severe as 4. All analyses were conducted in R.
Supplementary information
Acknowledgements
This study was supported by the Weill Cornell Medicine Children’s Health Council Investigator Fund, the Pritzker Consortium, the Khoury Foundation, the Paul and Jenna Segal Family Foundation, and the Saks Fifth Avenue Foundation. A.W. conducted this research as part of the Areas of Concentration (AOC) Program of the Weill Cornell MD curriculum. The authors would like to thank Michelle Demetres for suggestions on crafting the initial systematic search criteria.
Author contributions
A.W., M.S., E.B., A.F., and F.G. formed the search strategy and inclusion and exclusion criteria. A.W. performed the database searches. A.W., E.B., and J.B. reviewed all records for eligibility and extracted the data, and conflicts were resolved by M.S. Data analysis was conducted by A.W. in collaboration with M.S. and consultation with F.G. All authors contributed to writing the manuscript. A.W. and M.S. are co-first authors.
Data availability
The data used in this study are publicly available. The extracted data are available in the following github repository: https://github.com/ashlwu/SmartphoneAppsDepressionAnxiety. Of note, the data were analyzed in.csv format but have been converted to.xlsx format to allow the data to be password protected. The password is “Engage.”
Code availability
Meta-analyses and meta-regressions were conducted using the Meta, Metafor, and Dmetar packages in R65–67. The code is publicly available in the following github repository: https://github.com/ashlwu/SmartphoneAppsDepressionAnxiety.
Competing interests
The authors declare no competing interests. The Weill Cornell Department of Psychiatry has developed an app for the treatment of anxiety in youth. The app is not commercially available.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Ashley Wu, Matthew A. Scult.
Contributor Information
Matthew A. Scult, Email: mas9591@med.cornell.edu
Faith M. Gunning, Email: fgd2002@med.cornell.edu
Supplementary information
The online version contains supplementary material available at 10.1038/s41746-021-00386-8.
References
- 1.Torous J, Roberts LW. Needed innovation in digital health and smartphone applications for mental health: transparency and trust. JAMA Psychiatry. 2017;74:437–438. doi: 10.1001/jamapsychiatry.2017.0262. [DOI] [PubMed] [Google Scholar]
- 2.Weisel KK, et al. Standalone smartphone apps for mental health-a systematic review and meta-analysis. npj Digital Med. 2019;2:118. doi: 10.1038/s41746-019-0188-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Firth J, et al. Can smartphone mental health interventions reduce symptoms of anxiety? A meta-analysis of randomized controlled trials. J. Affect. Disord. 2017;218:15–22. doi: 10.1016/j.jad.2017.04.046. [DOI] [PubMed] [Google Scholar]
- 4.Firth J, et al. The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiatry. 2017;16:287–298. doi: 10.1002/wps.20472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Linardon J, Cuijpers P, Carlbring P, Messer M, Fuller-Tyszkiewicz M. The efficacy of app-supported smartphone interventions for mental health problems: a meta-analysis of randomized controlled trials. World Psychiatry. 2019;18:325–336. doi: 10.1002/wps.20673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baumel A, Muench F, Edan S, Kane JM. Objective user engagement with mental health apps: systematic search and panel-based usage analysis. J. Med. Internet Res. 2019;21:e14567. doi: 10.2196/14567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kelders SM, Kok RN, Ossebaard HC, Van Gemert-Pijnen JEWC. Persuasive system design does matter: a systematic review of adherence to web-based interventions. J. Med. Internet Res. 2012;14:e152. doi: 10.2196/jmir.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oinas-Kukkonen H, Harjumaa M. Persuasive systems design: key issues, process model, and system features. CAIS. 2009;24:485–500. [Google Scholar]
- 9.Kahneman D. Maps of bounded rationality: psychology for behavioral economics. Am. Econ. Rev. 2003;93:1449–1475. doi: 10.1257/000282803322655392. [DOI] [Google Scholar]
- 10.Patel MS, Asch DA, Volpp KG. Framing financial incentives to increase physical activity among overweight and obese adults. Ann. Intern. Med. 2016;165:600. doi: 10.7326/L16-0280. [DOI] [PubMed] [Google Scholar]
- 11.Dai H, Milkman KL, Riis J. The fresh start effect: temporal landmarks motivate aspirational behavior. Manag. Sci. 2014;60:2563–2582. doi: 10.1287/mnsc.2014.1901. [DOI] [Google Scholar]
- 12.Rogers T, Milkman KL, Volpp KG. Commitment devices: using initiatives to change behavior. JAMA. 2014;311:2065–2066. doi: 10.1001/jama.2014.3485. [DOI] [PubMed] [Google Scholar]
- 13.Patel MS, et al. A randomized, controlled trial of lottery-based financial incentives to increase physical activity among overweight and obese adults. Am. J. Health Promot. 2018;32:1568–1575. doi: 10.1177/0890117118758932. [DOI] [PubMed] [Google Scholar]
- 14.Huotari, K. & Hamari, J. Defining gamification: a service marketing perspective. in Proceeding of the 16th International Academic MindTrek Conference on - MindTrek ’12 17 (ACM Press, 2012). 10.1145/2393132.2393137.
- 15.Kelders SM, Sommers-Spijkerman M, Goldberg J. Investigating the direct impact of a gamified versus nongamified well-being intervention: an exploratory experiment. J. Med. Internet Res. 2018;20:e247. doi: 10.2196/jmir.9923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheng VWS, Davenport T, Johnson D, Vella K, Hickie IB. Gamification in apps and technologies for improving mental health and well-being: systematic review. JMIR Ment. Health. 2019;6:e13717. doi: 10.2196/13717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cotton V, Patel MS. Gamification use and design in popular health and fitness mobile applications. Am. J. Health Promot. 2019;33:448–451. doi: 10.1177/0890117118790394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pramana G, et al. Using mobile health gamification to facilitate cognitive behavioral therapy skills practice in child anxiety treatment: open clinical trial. JMIR Serious Games. 2018;6:e9. doi: 10.2196/games.8902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Torous J, Lipschitz J, Ng M, Firth J. Dropout rates in clinical trials of smartphone apps for depressive symptoms: a systematic review and meta-analysis. J. Affect. Disord. 2020;263:413–419. doi: 10.1016/j.jad.2019.11.167. [DOI] [PubMed] [Google Scholar]
- 20.Anguera JA, Jordan JT, Castaneda D, Gazzaley A, Areán PA. Conducting a fully mobile and randomised clinical trial for depression: access, engagement and expense. BMJ Innov. 2016;2:14–21. doi: 10.1136/bmjinnov-2015-000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bakker D, Rickard N. Engagement with a cognitive behavioural therapy mobile phone app predicts changes in mental health and wellbeing: MoodMission. Aust. Psychol. 2019;54:245–260. doi: 10.1111/ap.12383. [DOI] [Google Scholar]
- 22.Ben-Zeev D, et al. mHealth for schizophrenia: patient engagement with a mobile phone intervention following hospital discharge. JMIR Ment. Health. 2016;3:e34. doi: 10.2196/mental.6348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bustillos, D. The effects of using pacifica on depressed patients. https://search.proquest.com/docview/2172401714?pq-origsite=primo (2018).
- 24.Caplan S, Sosa Lovera A, Reyna Liberato P. A feasibility study of a mental health mobile app in the Dominican Republic: the untold story. Int. J. Ment. Health. 2018;47:311–345. doi: 10.1080/00207411.2018.1553486. [DOI] [Google Scholar]
- 25.Chen AT, Wu S, Tomasino KN, Lattie EG, Mohr DC. A multi-faceted approach to characterizing user behavior and experience in a digital mental health intervention. J. Biomed. Inform. 2019;94:103187. doi: 10.1016/j.jbi.2019.103187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dahne J, et al. Pilot randomized trial of a self-help behavioral activation mobile app for utilization in primary care. Behav. Ther. 2019;50:817–827. doi: 10.1016/j.beth.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dahne J, et al. Pilot randomized controlled trial of a Spanish-language Behavioral Activation mobile app (¡Aptívate!) for the treatment of depressive symptoms among united states Latinx adults with limited English proficiency. J. Affect. Disord. 2019;250:210–217. doi: 10.1016/j.jad.2019.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Enock PM, Hofmann SG, McNally RJ. Attention bias modification training via smartphone to reduce social anxiety: a randomized, controlled multi-session experiment. Cogn. Ther. Res. 2014;38:200–216. doi: 10.1007/s10608-014-9606-z. [DOI] [Google Scholar]
- 29.Hur J-W, Kim B, Park D, Choi S-W. A scenario-based cognitive behavioral therapy mobile app to reduce dysfunctional beliefs in individuals with depression: a randomized controlled trial. Telemed. J. E Health. 2018;24:710–716. doi: 10.1089/tmj.2017.0214. [DOI] [PubMed] [Google Scholar]
- 30.Inkster B, Sarda S, Subramanian V. An empathy-driven, conversational artificial intelligence agent (Wysa) for digital mental well-being: real-world data evaluation mixed-methods study. JMIR Mhealth Uhealth. 2018;6:e12106. doi: 10.2196/12106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lüdtke T, Pult LK, Schröder J, Moritz S, Bücker L. A randomized controlled trial on a smartphone self-help application (Be Good to Yourself) to reduce depressive symptoms. Psychiatry Res. 2018;269:753–762. doi: 10.1016/j.psychres.2018.08.113. [DOI] [PubMed] [Google Scholar]
- 32.Lukas, C. A., Eskofier, B. & Berking, M. A gamified smartphone-based intervention for depression: results from a randomized controlled pilot trial. Preprint 10.2196/preprints.16643 (2019). [DOI] [PMC free article] [PubMed]
- 33.Ly KH, et al. Behavioural activation versus mindfulness-based guided self-help treatment administered through a smartphone application: a randomised controlled trial. BMJ Open. 2014;4:e003440. doi: 10.1136/bmjopen-2013-003440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mehrotra S, Sudhir P, Rao G, Thirthalli J, Srikanth TK. Development and pilot testing of an internet-based self-help intervention for depression for indian users. Behav. Sci. 2018;8:36. doi: 10.3390/bs8040036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moberg C, Niles A, Beermann D. Guided self-help works: randomized waitlist controlled trial of pacifica, a mobile app integrating cognitive behavioral therapy and mindfulness for stress, anxiety, and depression. J. Med. Internet Res. 2019;21:e12556. doi: 10.2196/12556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mohr DC, et al. Comparison of the effects of coaching and receipt of app recommendations on depression, anxiety, and engagement in the intellicare platform: factorial randomized controlled trial. J. Med. Internet Res. 2019;21:e13609. doi: 10.2196/13609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Norton, V. P. The CALM project: teaching mindfulness meditation in primary care using computer-based application (ProQuest, 2017).
- 38.Pratap A, et al. Using mobile apps to assess and treat depression in hispanic and latino populations: fully remote randomized clinical trial. J. Med. Internet Res. 2018;20:e10130. doi: 10.2196/10130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Roepke AM, et al. Randomized controlled trial of superbetter, a smartphone-based/internet-based self-help tool to reduce depressive symptoms. Games Health J. 2015;4:235–246. doi: 10.1089/g4h.2014.0046. [DOI] [PubMed] [Google Scholar]
- 40.Stiles-Shields C, Montague E, Kwasny MJ, Mohr DC. Behavioral and cognitive intervention strategies delivered via coached apps for depression: pilot trial. Psychol. Serv. 2019;16:233–238. doi: 10.1037/ser0000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stolz T, et al. A mobile app for social anxiety disorder: a three-arm randomized controlled trial comparing mobile and PC-based guided self-help interventions. J. Consult. Clin. Psychol. 2018;86:493–504. doi: 10.1037/ccp0000301. [DOI] [PubMed] [Google Scholar]
- 42.Wahle F, Kowatsch T, Fleisch E, Rufer M, Weidt S. Mobile sensing and support for people with depression: a pilot trial in the wild. JMIR Mhealth Uhealth. 2016;4:e111. doi: 10.2196/mhealth.5960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Watts S, et al. CBT for depression: a pilot RCT comparing mobile phone vs. computer. BMC Psychiatry. 2013;13:49. doi: 10.1186/1471-244X-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lim MH, et al. A pilot digital intervention targeting loneliness in youth mental health. Front. Psychiatry. 2019;10:604. doi: 10.3389/fpsyt.2019.00604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Aromataris, E. & Munn, Z. Joanna Briggs Institute reviewer’s manual. The Joanna Briggs Institutehttps://reviewersmanual.joannabriggs.org (2017).
- 46.Sterne JAC, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 47.Torous J, Nicholas J, Larsen ME, Firth J, Christensen H. Clinical review of user engagement with mental health smartphone apps: evidence, theory and improvements. Evid. Based Ment. Health. 2018;21:116–119. doi: 10.1136/eb-2018-102891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baumeister H, Reichler L, Munzinger M, Lin J. The impact of guidance on Internet-based mental health interventions — a systematic review. Internet Interv. 2014;1:205–215. doi: 10.1016/j.invent.2014.08.003. [DOI] [Google Scholar]
- 49.Baumel A, Yom-Tov E. Predicting user adherence to behavioral eHealth interventions in the real world: examining which aspects of intervention design matter most. Transl. Behav. Med. 2018;8:793–798. doi: 10.1093/tbm/ibx037. [DOI] [PubMed] [Google Scholar]
- 50.Graham AK, Lattie EG, Mohr DC. Experimental therapeutics for digital mental health. JAMA Psychiatry. 2019 doi: 10.1001/jamapsychiatry.2019.2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kahneman D. A psychological perspective on economics. Am. Econ. Rev. 2003;93:162–168. doi: 10.1257/000282803321946985. [DOI] [Google Scholar]
- 52.Vlaev I, King D, Darzi A, Dolan P. Changing health behaviors using financial incentives: a review from behavioral economics. BMC Public Health. 2019;19:1059. doi: 10.1186/s12889-019-7407-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Beidas RS, et al. Transforming mental health delivery through behavioral economics and implementation science: protocol for three exploratory projects. JMIR Res Protoc. 2019;8:e12121. doi: 10.2196/12121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang J, Mann F, Lloyd-Evans B, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. 2018;18:156. doi: 10.1186/s12888-018-1736-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Donkin L, et al. A systematic review of the impact of adherence on the effectiveness of e-therapies. J. Med. Internet Res. 2011;13:e52. doi: 10.2196/jmir.1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Torous J, Michalak EE, O’Brien HL. Digital health and engagement-looking behind the measures and methods. JAMA Netw. Open. 2020;3:e2010918. doi: 10.1001/jamanetworkopen.2020.10918. [DOI] [PubMed] [Google Scholar]
- 57.Volpp KG, et al. A randomized, controlled trial of financial incentives for smoking cessation. N. Engl. J. Med. 2009;360:699–709. doi: 10.1056/NEJMsa0806819. [DOI] [PubMed] [Google Scholar]
- 58.Patel, M. S. et al. Effectiveness of behaviorally designed gamification interventions with social incentives for increasing physical activity among overweight and obese adults across the united states: the STEP UP randomized clinical trial. JAMA Intern. Med. 1–9, 10.1001/jamainternmed.2019.3505 (2019). [DOI] [PMC free article] [PubMed]
- 59.Wong CA, et al. Effect of financial incentives on glucose monitoring adherence and glycemic control among adolescents and young adults with type 1 diabetes: a randomized clinical trial. JAMA Pediatr. 2017;171:1176–1183. doi: 10.1001/jamapediatrics.2017.3233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Qu C, Sas C, Daudén Roquet C, Doherty G. Functionality of top-rated mobile apps for depression: systematic search and evaluation. JMIR Ment. Health. 2020;7:e15321. doi: 10.2196/15321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chan S, Torous J, Hinton L, Yellowlees P. Towards a framework for evaluating mobile mental health apps. Telemed. J. E Health. 2015;21:1038–1041. doi: 10.1089/tmj.2015.0002. [DOI] [PubMed] [Google Scholar]
- 63.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 65.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1–48. doi: 10.18637/jss.v036.i03. [DOI] [Google Scholar]
- 66.Harrer M, Cuijpers P, Furukawa T, Ebert D. Doing meta-analysis in R: a hands-on guide. Zenodo. 2019 doi: 10.5281/zenodo.2551803. [DOI] [Google Scholar]
- 67.Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid. Based Ment. Health. 2019;22:153–160. doi: 10.1136/ebmental-2019-300117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used in this study are publicly available. The extracted data are available in the following github repository: https://github.com/ashlwu/SmartphoneAppsDepressionAnxiety. Of note, the data were analyzed in.csv format but have been converted to.xlsx format to allow the data to be password protected. The password is “Engage.”
Meta-analyses and meta-regressions were conducted using the Meta, Metafor, and Dmetar packages in R65–67. The code is publicly available in the following github repository: https://github.com/ashlwu/SmartphoneAppsDepressionAnxiety.