Abstract
Objectives:
The link between dysregulated positive affect and binge-eating behavior in youth with obesity is poorly understood. In addition, it is unclear how putative associations differ across developmental periods of rapid biological and emotional change, such as puberty, and in racial and ethnic minority youth, who are more likely to be overweight but are underrepresented in the literature.
Method:
This study used a two-week ecological momentary assessment protocol to examine independent and interactive effects of positive affect intensity/instability, and pubertal stage on two components of binge-eating behavior, loss of control eating (LOCE) and overeating.
Results:
Participants were 38 youth with overweight/obesity (ages 8-14 years; 78% African-American/Hispanic). Positive affect instability was calculated using probability of acute change (PAC), representing the likelihood of extreme affective changes, and mean squared successive difference (MSSD), representing the average change in affect over successive recordings. There were no main effects of positive affect intensity on LOCE or overeating, but positive affect instability was negatively associated with overeating severity using both MSSD (p=.005) and PAC metrics (p=.001). However, moderation analyses including interactions with pubertal status revealed more extreme changes in positive affect (i.e., higher PAC) were related to greater overeating (p=.001) and LOCE severity (p=.043) in mid-late pubertal youth but not in pre-early pubertal youth.
Discussion:
Pubertal status may influence the association between disruptions in positive affect and dysregulated eating in youth, and positive affect instability may be important to consider in order to understand the emotional correlates of binge eating in youth with overweight/obesity.
Pediatric obesity is a major public health concern affecting approximately 20% of youth in the United States, with higher rates in African-American and Hispanic youth (Ogden et al., 2016). Although the causes of pediatric obesity are multifaceted, for some children, obesity has important psychological correlates. Binge eating, eating an objectively large amount of food while experiencing a sense of loss of control over eating (LOCE) (American Psychiatric Association, 2013), occurs in approximately 20% of children with obesity (He et al., 2017) and is prospectively associated with psychological distress and depressive symptoms (Goldschmidt, 2017). As such, research investigating the emotional mechanisms underlying binge eating has focused on the role of negative affect (e.g., Elliott et al., 2010). However, there is emerging evidence that dysregulated positive affect may play an important role (Selby et al., 2019).
Although LOCE and overeating are independent constructs associated with unique psychological correlates and weight gain, much of the research on binge eating in youth has focused on the experience of LOCE (Goldschmidt, 2017; Goldschmidt et al., 2014, 2018). This is likely due to evidence that, regardless of episode size, LOCE is a predictor of present and future psychosocial impairment (Hilbert et al., 2013). Retrospective data indicate that LOCE is associated with high levels of positive affect intensity in youth, such as during social events and parties (Tanofsky-Kraff, Goosens, et al., 2007). There is also evidence in youth that happiness is associated with emotional eating urges (Tanofsky-Kraff, Theim, et al., 2007), which have been found to predict later onset of binge eating (Stice et al., 2002).
One theory to explain the proposed link between positive affect and binge eating is that food is a primary reinforcer that may serve to as a way to increase positive affect. In particular, foods that are high in sugar and carbohydrates are known to elevate mood (Rosenstein & Oster, 1988). For some youth, the consumption of these foods may also lead to LOCE. Indeed, youth often endorse eating more snack foods and desserts during LOCE episodes as compared with normal eating episodes (Theim et al., 2007), which may explain why LOCE often occurs during events when such foods are readily available (Tanofsky-Kraff, Goosens, et al., 2007). Even when LOCE does not occur, the use of food to improve positive affect may also be associated with overeating. In particular, youth at risk for obesity may find highly palatable foods more rewarding than youth not at risk for obesity, and thus be more likely to eat more (Stice et al., 2011). As such, they may be driven to use food as a way to increase and maintain positive affect, even without experiencing a sense of LOCE.
Most research investigating positive affect and binge eating in youth has relied on retrospective recall through cross-sectional data collection, making it difficult to assess links between affect and eating behaviors in the moment. To address this limitation, methods like ecological momentary assessment (EMA) allow for the repeated collection of data in near real-time in an individual’s natural environment, minimizing the time between the event and recall. Only one study to date has used EMA to investigate the link between positive affect and LOCE in youth. Hilbert et al. (2009) found that German youth ages 8-13 with LOCE reported less happiness prior to any eating episode than they did when sampled randomly. Therefore, it is possible that these youth may have engaged in an eating episode in order to increase their happiness levels. However, there is a dearth of research utilizing EMA to examine the link between positive affect and LOCE, and no studies to date have examined positive affect and overeating. This gap in the literature is problematic in light of contrasting findings between momentary and retrospective negative affect and their link to LOCE. Unlike retrospective research, EMA findings suggest that the association between momentary negative affect and LOCE in youth may not be significant, across samples representing youth with overweight, normal weight, and ethnic and racial diversity (Goldschmidt et al., 2018; Hilbert, Rief, Tuschen-Caffier, de Zwaan, & Czaja, 2009; Ranzenhofer et al., 2014). These findings highlight the complex relation between emotional processes and binge-eating behaviors in youth and underscore the importance of investigating the role of momentary positive affect to gain a more comprehensive understanding of these processes.
In addition to the need to examine the momentary link between binge eating and positive affect intensity in youth, positive affect instability may also play a role given its association with poor emotion regulation (Trull et al., 2008). One theory is that, similar to those who experience low positive affect intensity, individuals who experience large fluctuations in positive affect may engage in dysregulated behaviors to regulate their affect. Although positive affect instability has been traditionally studied in the domain of bipolar disorder (Ebner-Priemer et al., 2007), large fluctuations in positive affect have also been found found in adults with symptoms of bulimia nervosa, including binge-eating episodes (Santangelo et al., 2014). An EMA study by Berner and colleagues (2017) found that for adults, on days where binge eating and/or purging were reported, extreme increases in positive affect occurred more often after these behaviors than at the same time period on days when these behaviors did not occur. Taken together, it is possible that the association between positive affect instability and binge eating and/or purging is reciprocal, such that individuals with high positive affect instability engage in these behaviors with the goal of stabilizing their positive emotions, but these behaviors in turn lead to more positive affect instability. However, the role of positive affect instability in binge eating has not been examined outside of the context of bulimia nervosa, therefore, the specific role of LOCE and overeating, in the absence of compensatory behaviors, is unknown. Additionally, positive affect instability has not been examined in youth, who experience more frequent fluctuations in emotional states as a normative component of development (Heller & Casey, 2016).
There is evidence that the transition to puberty is associated with both higher levels of emotional reactivity (Dahl & Gunnar, 2009) and the development of binge eating (Culbert, Sisk, & Klump, 2018). Fluctuations in positive affect may be more intense during this time, leading youth to turn to food to regulate these emotions (Gilbert, 2012). This may partially explain the increase in binge eating seen during adolescence. This increase may also be partially due to the pubertal moderation of etiological factors that contribute to binge eating, such as sex hormones and their modulation of genetic vulnerabilities to influence individual differences in risk for binge eating post-puberty (Culbert, Burt, & Klump, 2017; Culbert, Burt, Sisk, Nigg, & Klump, 2014; Klump et al., 2018). Nevertheless, it is unclear how pubertal changes may influence the relation between either positive affect instability or intensity and binge eating.
Finally, the discussion on positive affect and dysregulated eating in youth must be seen not only through a developmental lens, but also through the lens of diversity. Qualitative research suggests that African-American adolescent girls associate LOCE with a range of both positive and negative emotions, including high levels of intense positive affect (Cassidy et al., 2013). However, virtually nothing is known about the momentary relation between positive affect and LOCE in racially/ethnically diverse youth. Additionally, it is important to investigate the link between positive affect and overeating in this population, especially in those with overweight or obesity. For example, it is more likely for minority youth to endorse eating because they want to gain weight, as larger bodies may be more valued in their communities, or who report overeating as a way to signal enjoyment of the food (Neumark-Sztainer et al., 2002; Vander Wal, 2004). Therefore, although overeating is important to consider in any discussion of binge eating, it may be especially so in minority youth with obesity.
The current study sought to assess the association between positive affect and two components of binge eating, LOCE and overeating, through the use of EMA. We investigated the role of both positive affect intensity and instability, as well as pubertal stage as a potential moderator, in a sample composed largely of racial/ethnic minority youth with overweight/obesity. Consistent with theory that maladaptive eating may be driven by desire to increase/sustain positive affect, we hypothesized that regardless of episode size, 1) positive affect intensity would be negatively associated with LOCE, and 2) both overall variability in positive affect and extreme fluctuations in positive affect would be positively associated with LOCE. Finally, we hypothesized that the relation between both LOCE and 1) positive affect intensity, 2) overall variability in positive affect, and 3) extreme fluctuations in positive affect would be moderated by pubertal status. That is, all three associations would be stronger for individuals later in puberty given the established associations between dysregulated positive affect and the onset of psychopathology with advancing pubertal maturation (Gilbert, 2012). We hypothesized that overeating may share similar mechanisms with LOCE in this population, reflecting a behavior meant to increase or sustain positive affect, therefore, the association between positive affect and overeating would be similar to that of LOCE described above.
Method
Participants
Participants were 38 youth ages 8-14 (Mage=11.16±1.94 years) with overweight/obesity (BMI > 85th percentile for age/sex; MzBMI = 2.07±0.49; Kuczmarski et al., 2000). Approximately half of participants were female, and the majority self-identified as African-American (63%) or Hispanic (15%). Participants were recruited from both the community as well as from a sample of participants who participated in previous studies at two U.S. academic institutions and consented to be contacted for future studies (Goldschmidt et al., 2018). Individuals were excluded if they met criteria for an eating disorder other than binge eating disorder or had a medical condition or receiving treatment (pharmacological or behavioral) known to influence appetite or weight. All participants were fluent English speakers. Of the 92 participants who met preliminary criteria based on phone screening, 44 participated in a baseline face-to-face assessment. Four participants did not provide adequate data (i.e., at least one week of EMA recordings, which was required to increase the representativeness of the data collected, and to ensure that both weekends and weekdays were adequately sampled), and two did not report their pubertal stage bringing the total number of participants in final analyses to 38.
Procedure
Institutional approval and informed consent/assent were obtained prior to data collection. During the baseline assessment, participants received height and weight measurement, assessment of eating behaviors and psychological functioning, and, along with their parents, training on how to complete EMA recordings. Consistent with previous EMA studies of youth with overweight (Hilbert et al., 2009; Ranzenhofer et al., 2014), recordings were completed on an event-contingent (i.e., after any type of eating behavior), interval-contingent (i.e., every night before bed), and signal-contingent (i.e., 3-5 semi-random times per day) basis. On weekdays, signaled prompts were administered at times that avoided interfering with school schedules. On weekends, prompts were given every 2-3 hours between 8:00am-9:00pm. During each recording, participants were asked about current affect as well as characteristics of any recent eating episode that had not been previously recorded. Participants first completed a one-day practice period, not used in analyses, and if adherence was at least 70%, they were qualified to begin the full 14-day protocol.
Measures
Body Mass Index.
Height and weight were measured at baseline using a stadiometer and calibrated digital scale. Body mass index was calculated using CDC growth charts to obtain standardized scores (Kuczmarski et al., 2000).
Demographics.
Demographic data, including child’s age, gender, race, and ethnicity, were collected at baseline.
Child Eating Disorder Examination.
Version 12.0 of the Child Eating Disorder Examination (Child EDE; (Bryant-Waugh et al., 1996) was used at baseline to assess for both current and lifetime LOCE and other eating disorders. The Child EDE is a modified version of the EDE, a semi-structured interview used to diagnose eating disorders, that includes simplified language suitable for children. The Child EDE has good reliability and validity (Watkins et al., 2005) and has some evidence of use in racial minorities (Burke et al., 2017) and in youth with overweight/obesity (Decaluwe & Braet, 2003; Tanofsky-Kraff et al., 2004).
Tanner scale.
A modified Tanner scale was used to assess pubertal development (Tanner, 1962). The full Tanner scale provides separate schematics for boys and girls, each of which include detailed drawings corresponding to stages of pubic development and hair growth (for boys) and breast development and pubic hair growth (for girls), to assess for changes in secondary sex characteristics. In this study, only pubic hair growth was assessed due to concerns about the validity of the stages of breast development in girls with overweight/obesity, where it may be difficult to differentiate between breast tissue and adipose tissue, making assessment less reliable (Bonat et al., 2002; Raman et al., 2011). Participants were asked to select which drawing was most representative of their current development. Consistent with prior pubertal status research (e.g., Culbert, Burt, McGue, Iacono, & Klump, 2009; Culbert et al., 2014; Klump et al., 2012; Suisman et al., 2014), participants were categorized into two pubertal groups: pre-to-early (Tanner stages 1-2) or mid-to-late (Tanner stages 3-5) puberty. There is modest-to-high agreement between self-report and physician reported Tanner staging in adolescents (Campisi et al., in press; Duke et al., 1980).
EMA Measures.
The Positive and Negative Affect Schedule (PANAS; (Watson et al., 1988) was used during all EMA recordings to assess momentary positive affect. The PANAS includes 10 negative and 10 positive items that are each rated on a scale from 1 (“not at all”) to 5 (“extremely”). Positive items were summed to form a composite score (range = 0-50).
At every recording where an eating episode was reported, participants responded to questions about what kind of eating episode they experienced (i.e., meal, snack, binge) as well as key features of those episodes. overeating was assessed via the question, “To what extent did you feel that you overate?” and LOCE was assessed via several questions such as, “While you were eating, did you… feel a sense of loss of control?” and “…feel like a car without brakes, you just kept eating and eating?”. Participants rated each question on a 1(“no, not at all) to 5 (“yes, extremely) scale. For LOCE, all questions were summed to form a total score ranging from 4-20 due to good internal consistency (alpha = .91). LOCE and overeating were not considered mutually exclusive.
Statistical Analysis
Generalized estimating equations (GEEs) were used to examine the independent and interactive effects of positive affect dimensions and puberty stage on LOCE and overeating severity ratings, measured continuously. That is, GEE models assessed (1) momentary associations between positive affect intensity and LOCE/overeating, (2) daily associations between positive affect intensity and LOCE/overeating, (3) daily associations between positive affect instability and LOCE/overeating, and (4) the extent to which pubertal status moderated these associations. Consistent with previous research (e.g., Scott et al., 2018), we focused on the highest daily LOCE or overeating ratings to tap into the most “severe” behavior given our community-based sample of youth who were not selected on the basis of reporting eating pathology, and there was concern that low base rates of maladaptive eating might obscure findings of significance. However, to ensure that our use of the highest daily LOCE or overeating rating did not unduly impact our results, we also conducted post-hoc analyses with mean daily LOCE and overeating ratings as dependent variables.
Momentary relationships between positive affect and eating behaviors were assessed concurrently (i.e., associations between positive affect and LOCE/overeating EMA ratings at the same EMA signal) as well prospectively (i.e., associations between lagged positive affect ratings at the most proximal previous EMA rating and subsequent LOCE/overeating ratings). Consistent with previous EMA research (Berner et al., 2017), time-lagged positive affect ratings were limited to the same day as the LOCE/overeating ratings. To examine mean daily positive affect intensity, positive affect ratings were aggregated within each day for each participant. Instability in positive affect was assessed by two indices: the mean squared successive difference (MSSD) and the probability of acute change (PAC), metrics previously used to assess affective instability in eating disorders and other psychiatric conditions (e.g., Berner et al., 2017; Santangelo et al., 2014; Snir, Bar-Kalifa, Berenson, Downey, & Rafaeli, 2017; Trull et al., 2008). MSSD measures the differences in positive affect between consecutive EMA ratings and thus provides an average measure of variance in positive affect. The PAC calculates the likelihood of an acute increase or decrease between successive positive affect ratings, with “acute” changes defined as those above the 90th percentile of all differences for an individual. MSSD and PAC indices were calculated within each day for each person (i.e., not lagging ratings between days). Participants received one positive affect PAC and one positive affect MSSD score for each day, based on that day’s multiple EMA ratings of positive affect.
Separate GEE models were conducted for each positive affect index (i.e., concurrent momentary positive affect, lagged momentary positive affect, daily positive affect intensity, daily positive affect MSSD, and daily positive affect PAC) and dependent variable (i.e., LOCE and overeating severity). Dependent variables in the momentary models were concurrent or subsequent EMA ratings of LOCE or overeating severity, while dependent variables in the daily models were the highest LOCE or overeating ratings that the participant made that day. GEE models included within- and between-person effects of continuous independent variables (i.e., positive affect indices) as well as their interactions with puberty stage. Within-person effects reflect the degree to which positive affect momentary or daily values differed from an individual’s average level, whereas between-person effects reflect the degree to which an individual’s average level of positive affect (overall intensity, MSSD, PAC across the EMA protocol) deviated from the total sample means of these indices. Each GEE employed an AR1 serial autocorrelation given the dependence within the nested data, and a gamma link function to account for skewed distribution of dependent variables. Analyses were conducted using available data without imputation in SPSS version 25.
Results
Approximately 25% of participants reported experiencing LOCE over the past three months and 5% reported overeating, according to the Child EDE. With regards to pubertal status, 10 boys and 10 girls were classified as pre-early puberty and 5 boys and 12 girls were classified as mid-late puberty, consistent with the expected lag in pubertal onset in boys compared to girls (Grumbach & Styne, 2003).
Participants completed an average of 13.83 (SD = 1.74) days of EMA recordings, including 67.6% signal-contingent (1,119 total), 9.1% event-contingent (151 total), and 23.3% bedtime recordings (387 total). On each day, participants completed an average of 3.01 (SD = 1.37) total recordings per day (range = 0.86–7.43), including 2.03 (SD = 0.86) signal-contingent (range = 0.64–3.43), 0.50 (SD = 0.69) event-contingent (range = 0.06–3.00), and 0.70 (SD = 0.24) bedtime recordings per day (range = 0.15–1.00). This represented 266 signal-contingent (56.5%) and 124 event-contingent (26.3%) eating episodes, along with 81 eating episodes (17.2%) reported in bedtime recordings.
Results of GEE models are shown in Table 1. There were no main effects of momentary positive affect (concurrent or lagged) or daily positive affect intensity on LOCE or overeating, and puberty stage did not emerge as a significant moderator in these models. However, significant effects emerged when analyzing positive affect instability. For overeating but not LOCE, there was a main effect of between-subjects positive affect MSSD (B<−.01, SE<.01, p=.005), such that individuals with less overall variability in positive affect (i.e., lower positive affect MSSD), relative to the sample mean, reported greater overall overeating severity. However, there was a negative main effect of positive affect PAC on overeating severity (B=−2.27, SE=1.12, p=.042) and interactions of between-subjects positive affect PAC and puberty stage predicting overeating (B=3.81, SE=1.16, p=.001) and LOCE severity (B=1.45, SE=.72, p=.043). That is, a greater degree of acute changes in positive affect (i.e., higher overall positive affect PAC) was related to greater LOCE and overeating and among participants in the mid-late pubertal group, while in the pre-early pubertal group, the association between positive affect PAC and LOCE was not significant (see Figures 1&2). When post-hoc analyses were conducted with mean daily LOCE and overeating ratings as dependent variables, the pattern of findings was identical with the exception of an attenuated interaction of positive affect PAC and puberty status predicting LOCE (p=.063).
Table 1.
Generalized estimating equation results
| Loss of control eating (LOCE) |
Overeating (OE) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% confidence interval |
95% confidence interval |
||||||||||||
| Momentary concurrent PA |
B | SE | Lower | Upper | Wald χ2 | P | Momentary concurrent PA |
B | SE | Lower | Upper | Wald χ2 | P |
| Intercept | 1.52 | 0.06 | 1.39 | 1.64 | 567.30 | <0.001 | Intercept | 0.22 | 0.07 | 0.08 | 0.36 | 9.29 | 0.002 |
| Tanner stage | −0.04 | 0.08 | −0.20 | 0.12 | 0.26 | 0.613 | Tanner stage | −0.09 | 0.09 | −0.26 | 0.08 | 1.17 | 0.279 |
| PA (between) | 0.01 | 0.01 | −0.01 | 0.02 | 0.60 | 0.438 | PA (between) | 0.01 | 0.01 | −0.01 | 0.02 | 1.47 | 0.225 |
| Concurrent PA (within) | <0.01 | <0.01 | −0.01 | 0.00 | 1.26 | 0.262 | Concurrent PA (within) | <0.01 | 0.01 | −0.01 | 0.01 | 0.10 | 0.747 |
| Tanner X PA (between) | <0.01 | 0.01 | −0.02 | 0.01 | 0.23 | 0.634 | Tanner X PA (between) | −0.01 | 0.01 | −0.02 | 0.01 | 0.90 | 0.343 |
| Tanner X concurrent PA (within) | 0.01 | 0.01 | <0.01 | 0.02 | 1.31 | 0.253 | Tanner X concurrent PA (within) | <0.01 | 0.01 | −0.01 | 0.01 | 0.14 | 0.704 |
| Momentary lagged PA |
Momentary lagged PA |
||||||||||||
| Intercept | 1.50 | 0.06 | 1.39 | 1.62 | 676.09 | <0.001 | Intercept | 0.22 | 0.07 | 0.08 | 0.37 | 8.91 | 0.003 |
| Tanner stage | −0.05 | 0.06 | −0.18 | 0.07 | 0.74 | 0.391 | Tanner stage | −0.09 | 0.09 | −0.27 | 0.10 | 0.86 | 0.354 |
| PA (between) | 0.01 | 0.01 | −0.01 | 0.02 | 0.83 | 0.363 | PA (between) | 0.01 | 0.01 | −0.01 | 0.02 | 1.35 | 0.245 |
| Lagged PA (within) | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | 0.974 | Lagged PA (within) | <0.01 | <0.01 | −0.01 | 0.01 | 0.18 | 0.671 |
| Tanner X PA (between) | −0.01 | 0.01 | −0.02 | 0.01 | 1.06 | 0.303 | Tanner X PA (between) | −0.01 | 0.01 | −0.02 | 0.01 | 0.53 | 0.467 |
| Tanner X lagged PA (within) | <0.01 | <0.01 | −0.01 | <0.01 | 0.53 | 0.465 | Tanner X lagged PA (within) | <0.01 | <0.01 | −0.01 | <0.01 | 0.85 | 0.358 |
| Loss of control eating (LOCE) |
Overeating (OE) |
||||||||||||
| 95% confidence interval |
95% confidence interval |
||||||||||||
| Daily PA intensity | B | SE | Lower | Upper | Wald χ2 | P | Daily PA intensity | B | SE | Lower | Upper | Wald χ2 | P |
| Intercept | 1.55 | 0.07 | 1.41 | 1.69 | 468.40 | <0.001 | Intercept | 0.34 | 0.11 | 0.13 | 0.55 | 10.22 | 0.001 |
| Tanner stage | −0.05 | 0.09 | −0.22 | 0.13 | 0.27 | 0.602 | Tanner stage | −0.16 | 0.12 | −0.39 | 0.08 | 1.66 | 0.198 |
| PA (between) | 0.01 | 0.01 | −0.01 | 0.02 | 0.72 | 0.396 | PA (between) | <0.01 | 0.01 | −0.01 | 0.02 | 0.17 | 0.676 |
| Daily PA (within) | 0.01 | <0.01 | <0.01 | 0.02 | 3.21 | 0.073 | Daily PA (within) | <0.01 | 0.01 | −0.01 | 0.02 | 0.23 | 0.631 |
| Tanner X PA (between) | −0.01 | 0.01 | −0.02 | 0.01 | 0.50 | 0.480 | Tanner X PA (between) | <0.01 | 0.01 | −0.02 | 0.01 | 0.24 | 0.627 |
| Tanner X daily PA (within) | <0.01 | 0.01 | −0.02 | 0.01 | 0.45 | 0.504 | Tanner X daily PA (within) | −0.01 | 0.01 | −0.04 | 0.01 | 1.26 | 0.262 |
| Daily PA MSSD | Daily PA MSSD | ||||||||||||
| Intercept | 1.57 | 0.08 | 1.42 | 1.72 | 399.63 | <0.001 | Intercept | 0.49 | 0.14 | 0.22 | 0.76 | 12.52 | <0.001 |
| Tanner stage | −0.02 | 0.11 | −0.23 | 0.19 | 0.04 | 0.833 | Tanner stage | −0.17 | 0.16 | −0.50 | 0.15 | 1.12 | 0.290 |
| PA MSSD (between) | <0.01 | <0.01 | <0.01 | <0.01 | 1.25 | 0.265 | PA MSSD (between) | < −0.01 | <0.01 | <0.01 | <0.01 | 7.90 | 0.005 |
| PA MSSD (within) | <0.01 | <0.01 | <0.01 | <0.01 | 0.80 | 0.370 | PA MSSD (within) | <0.01 | <0.01 | <0.01 | <0.01 | 0.71 | 0.398 |
| Tanner X PA MSSD (between) | <0.01 | <0.01 | <0.01 | <0.01 | 0.17 | 0.682 | Tanner X PA MSSD (between) | <0.01 | <0.01 | <0.01 | 0.01 | 0.90 | 0.344 |
| Tanner X PA MSSD (within) | <0.01 | <0.01 | <0.01 | <0.01 | 0.17 | 0.682 | Tanner X PA MSSD (within) | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | 0.961 |
| Daily PA PAC | Daily PA PAC | ||||||||||||
| Intercept | 1.57 | 0.09 | 1.41 | 1.74 | 338.06 | <0.001 | Intercept | 0.51 | 0.14 | 0.25 | 0.78 | 14.16 | <0.001 |
| Tanner stage | −0.03 | 0.11 | −0.25 | 0.18 | 0.09 | 0.769 | Tanner stage | −0.22 | 0.15 | −0.51 | 0.07 | 2.18 | 0.140 |
| PA PAC (between) | −0.33 | 0.62 | −1.54 | 0.88 | 0.28 | 0.597 | PA PAC (between) | −2.27 | 1.12 | −4.47 | −0.08 | 4.12 | 0.042 |
| PA PAC (within) | 0.01 | 0.01 | −0.01 | 0.03 | 0.51 | 0.474 | PA PAC (within) | 0.03 | 0.02 | −0.01 | 0.06 | 2.14 | 0.143 |
| Tanner stage X PA PAC (between) | 1.45 | 0.72 | 0.04 | 2.85 | 4.09 | 0.043 | Tanner stage X PA PAC (between) | 3.81 | 1.16 | 1.53 | 6.09 | 10.75 | 0.001 |
| Tanner stage X PA PAC (within) | <0.01 | 0.04 | −0.08 | 0.09 | 0.01 | 0.934 | Tanner stage X PA PAC (within) | −0.03 | 0.05 | −0.13 | 0.07 | 0.26 | 0.607 |
Note. PA=positive affect; LOCE=loss of control eating; OE=overeating; between=grand-mean centered variable (between-subjects effect); within=person-mean centered variable (within-subjects effect); MSSD=mean squared successive difference; PAC=probability of acute change.
Tanner stage was coded such that early (i.e., stages 1 and 2) was the reference category.
Within-subjects effects in concurrent models reflect relationships between momentary PA and LOCE/OE ratings measured at the same EMA signal. Within-subjects effects in lagged models reflect relationships between momentary PA and subsequent LOCE/OE ratings measured at the next EMA signal. Within-subjects effects for the daily PA models reflect associations between mean daily PA intensity, MSSD, and PAC and peak daily LOCE/OE.
Although sex was not a significant covariate, when analyses were adjusted for sex the overall pattern of effects remained the same: (1) between-subjects PA MSSD was related to OE severity (B<−.01, SE<.01, p=.034); (2) there was a negative main effect of between-subjects PA PAC on OE severity (B=−2.50, SE =1.09, p=.021); and (3) the interaction of between-subjects PA PAC and puberty stage predicted OE (B=4.40, SE =1.29, p=.001) and trended similarly for LOCE severity (B=1.13, SE =.64, p=.077).
Figure 1. Interaction of Pubertal Status and PA Instability on Loss of Control Eating.
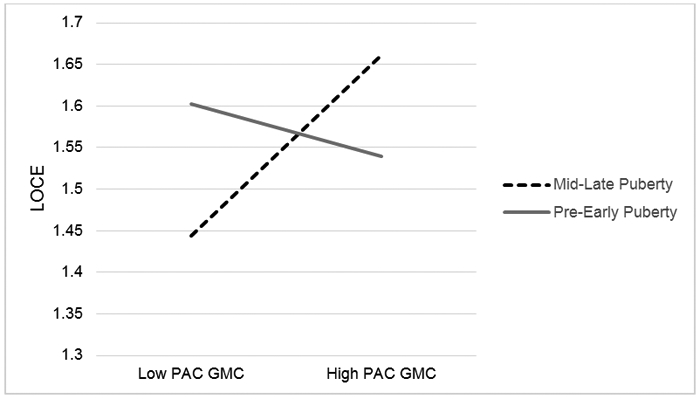
Note: LOCE = Loss of control eating; PAC = probability of acute change; GMC = grand mean centered, representing between-subjects effects
Mid-late puberty (p < .05); Pre-early puberty (n.s.)
Figure 2. Interaction of Pubertal Status and PA Instability on Overeating.
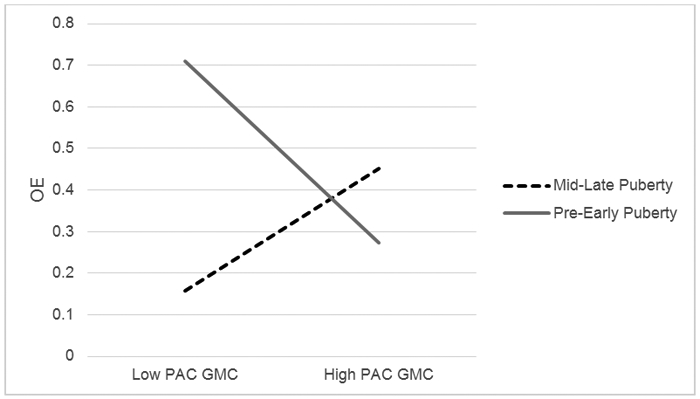
Note: LOCE = Loss of control eating; PAC = probability of acute change; GMC = grand mean centered, representing between-subjects effects
Mid-late puberty (p < .05); Pre-early puberty (p < .05)
Discussion
The current study examined associations between positive affect and two components of binge eating, LOCE and overeating, and the degree to which these associations were moderated by pubertal status in a racial/ethnic minority sample of youth with obesity. Contrary to hypotheses, positive affect intensity was not associated with either LOCE or overeating. There was a significant association between positive affect instability and overeating, such that youth with lower overall variability in positive affect and fewer acute changes in positive affect exhibited greater overeating severity. However, pubertal status moderated the relation between acute changes in positive affect and both overeating and LOCE; for youth in mid-late puberty, more acute changes in positive affect were associated with greater overeating and LOCE severity, while the association between positive affect and LOCE was no longer significant in pre-early puberty. Taken together, this study underscores the importance of examining multiple facets of positive affect, including positive affect instability, in relation to binge eating constructs. Additionally, puberty may play an important role in how affect and binge eating relate to one another in youth.
Overall, our findings add to the growing literature suggesting that momentary affective intensity may not be a key correlate of binge eating in youth. Importantly, our research extends this finding to positive affect. Although we hypothesized that there would be a negative association between positive affect intensity and LOCE given previous findings (i.e., Hilbert et al., 2009), our results must be considered in light of the demographic composition of the current sample. Very little research has been conducted on the binge-eating patterns of racial and ethnic minority youth. However, research that does exist suggests that LOCE does not have only one emotional face in this population; instead, it may occur in response to a variety of different emotions, both positive and negative (Cassidy et al., 2013). Additionally, it is possible that positive affect intensity is differentially related to LOCE in youth with obesity as it is in youth across the spectrum of weight status, like those in Hilbert et al., 2009.
In contrast to positive affect intensity, we found that momentary positive affect instability was associated with both LOCE and overeating, albeit in different ways. For both LOCE and overeating, there was a distinct difference between youth in different stages of puberty. The positive relation between positive affect instability and both LOCE and overeating in mid-late puberty was consistent with the adult literature (Berner et al., 2017; Santangelo et al., 2014). However, in pre-early puberty, our findings for LOCE and overeating were inconsistent with both each other and with our results from later in puberty. It is possible that the differences between LOCE and overeating are more salient prior to puberty, when children are younger and have less control over the amount that they eat, regardless of their emotional state. Additionally, LOCE may be more context-dependent than emotion-dependent prior to puberty. Our results underscore the importance of considering developmental stage when assessing affect in youth, as findings for both LOCE and overeating became more consistent in mid-late puberty. Puberty is often a time of intense emotional fluctuation, and there is evidence that the hormonal changes that occur during puberty may serve as a trigger for the maturation of areas of the brain responsible for regulating reward and emotion (Silk et al., 2009). This may help to explain why in mid-late puberty, when emotion regulation skills should be more developed, youth who continue to experience extreme fluctuations in positive affect relative to their peers also display more dysregulation in other areas, such as their eating behavior. Overall, the results of the current study partially support the theory that both LOCE and overeating are associated with high levels of positive affect fluctuation, at least for more mature adolescents.
In addition to our findings on pubertal moderation, we also found unique associations between positive affect instability and overeating, such that less positive affect instability (acute and overall) was associated with higher overeating. One explanation for this finding is that youth with overeating may struggle to identify changes in emotion and/or exhibit fewer normative fluctuations in positive affect, on average, than youth who do not experience overeating. It is also possible that parents may be more attuned to the behavior of youth who experience positive affect instability, due to the need to regulate that behavior, which may minimize the child’s opportunity to overeat. This may be especially salient for younger, less mature adolescents who have less independence over their food choices, which could explain why the affective correlates of overeating are different in mid-late puberty. These findings were contrary to our hypothesis, but may help to shed light on the emotional differences between LOCE and overeating in youth.
Strengths and Limitations
This study has several strengths, including the use of EMA to investigate momentary correlates of binge-eating constructs in youth in the natural environment. The study sample is also a strength, as it included a majority of youth who identified as African-American and/or Hispanic, a population that is often understudied in eating disorders research, as well as a balanced sample of girls and boys. However, one limitation is that, although the Eating Disorder Examination is considered a psychometrically-valid measurement, there is evidence that it may not be as appropriate for racial/ethnic minority youth, whose experience of eating pathology may not be fully captured by the EDE (Burke et al., 2017; Perez & Warren, 2013). Other limitations of the study include the small sample size and the use of self-report measures to assess variables of interest. Specifically, self-reported pubic hair development was used to assess pubertal status, which could be less reliable than physician-based Tanner staging (Bonat et al., 2002; Raman et al., 2011). Additionally, a single-item self-report measure was used to assess for overeating, potentially impacting the reliability of the findings. Additionally, the low base rates of overeating in this sample precluded us from distinguishing between overeating with LOCE and overeating without LOCE. This study also reported mainly on concurrent associations between binge eating and positive affect, therefore we cannot speak to the temporal nature of this relation. Additionally, we cannot generalize the findings to lower weight minority youth who endorse LOCE or overeating due to lack of a control group. Because of the small proportion of youth who endorsed any LOCE or overeating (~25%), this study used the highest LOCE or overeating ratings that a participant made each day instead of using mean ratings. Although the pattern of findings was consistent whether mean or highest LOCE/overeating ratings were used, the use of mean ratings did attenuate the moderating impact of puberty on the association between acute changes in positive affect and LOCE, likely due to the low base rates of LOCE in the sample. Therefore, these findings should be replicated using mean levels in samples with higher rates of LOCE. Finally, compliance rates in responding to EMA prompts and completing event-contingent recordings were modest, and this likely impacted our power to detect significant findings.
Future Directions
Research is needed to elucidate the temporal role of positive affect instability in binge eating in youth, and the results from this study require replication. Future studies should investigate whether the association between positive affect and binge eating differs based on timing and onset of puberty, using hormonal and physician-based measurements of pubertal status. Additionally, research should investigate whether associations between binge eating and ego-syntonic psychiatric conditions involving high levels of positive affect intensity/variability or positive-affect-seeking (e.g., bipolar disorder, substance use disorders), may be partially explained by extreme fluctuations in positive affect, and whether different facets of positive affect may be more or less salient in the experience of LOCE and/or overeating.
In sum, this study illustrates the importance of evaluating positive affect instability in the momentary assessment of LOCE and overeating . Results suggest that puberty may be an important inflection point that is associated with alterations in how positive affect instability contributes to the experience of LOCE and overeating, especially in racial/ethnic minority youth. This study also indicates the need to further elucidate the role of positive affect in LOCE and overeating and for clinicians to assess positive affect in the context of binge eating to inform prevention and intervention efforts aimed at youth.
Acknowledgements:
Funding Sources include The National Center for Advancing Translational Sciences, Grant Number: UL1-TR000430; The National Institute of Diabetes and Digestive and Kidney Diseases, Grant Number: K23-DK105234
Data Availability:
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub. [Google Scholar]
- Berner LA, Crosby RD, Cao L, Engel SG, Lavender JM, Mitchell JE, & Wonderlich SA (2017). Temporal associations between affective instability and dysregulated eating behavior in bulimia nervosa. Journal of Psychiatric Research, 92, 183–190. 10.1016/j.jpsychires.2017.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonat S, Pathomvanich A, Keil MF, Field AE, & Yanovski JA (2002). Self-assessment of pubertal stage in overweight children. Pediatrics, 110(4), 743–747. 10.1542/peds.110.4.743 [DOI] [PubMed] [Google Scholar]
- Bryant-Waugh RJ, Cooper PJ, Taylor CL, & Lask BD (1996). The use of the eating disorder examination with children: A pilot study. International Journal of Eating Disorders, 19(4), 391–397. [DOI] [PubMed] [Google Scholar]
- Burke NL, Tanofsky-Kraff M, Crosby R, Mehari RD, Marwitz SE, Broadney MM, Shomaker LB, Kelly NR, Schvey NA, Cassidy O, Yanovski SZ, & Yanovski JA (2017). Measurement invariance of the Eating Disorder Examination in black and white children and adolescents. International Journal of Eating Disorders, 50(7), 758–768. 10.1002/eat.22713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campisi SC, Marchand J, Siddiqui FJ, Islam M, Bhutta ZA, & Palmert MR (in press). Can we rely on adolescents to self-assess puberty stage? The Journal of Clinical Endocrinology & Metabolism. 10.1210/clinem/dgaa135 [DOI] [PubMed] [Google Scholar]
- Cassidy OL, Sbrocco T, Vannucci A, Nelson B, Jackson-Bowen D, Heimdal J, Mirza N, Wilfley DE, Osborn R, Shomaker LB, Young JF, Waldron H, Carter M, & Tanofsky-Kraff M (2013). Adapting interpersonal psychotherapy for the prevention of excessive weight gain in rural African American girls. Journal of Pediatric Psychology, 38(9), 965–977. 10.1093/jpepsy/jst029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culbert KM, Burt SA, & Klump KL (2017). Expanding the developmental boundaries of etiologic effects: The role of adrenarche in genetic influences on disordered eating in males. Journal of Abnormal Psychology, 126(5), 593–606. 10.1037/abn0000226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culbert KM, Burt SA, McGue M, Iacono WG, & Klump KL (2009). Puberty and the genetic diathesis of disordered eating attitudes and behaviors. Journal of Abnormal Psychology, 118(4), 788–796. 10.1037/a0017207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culbert KM, Burt SA, Sisk CL, Nigg JT, & Klump KL (2014). The effects of circulating testosterone and pubertal maturation on risk for disordered eating symptoms in adolescent males. Psychological Medicine, 44(11), 2271–2286. 10.1017/S0033291713003073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culbert KM, Sisk CL, & Klump KL (2018). Sex steroid hormones and differential risk for eating pathology: A review of genetic and phenotypic effects across development. Current Opinion in Behavioral Sciences, 23, 124–130. 10.1016/j.cobeha.2018.06.005 [DOI] [Google Scholar]
- Dahl RE, & Gunnar MR (2009). Heightened stress responsiveness and emotional reactivity during pubertal maturation: Implications for psychopathology. Development and Psychopathology, 21(1), 1–6. 10.1017/S0954579409000017 [DOI] [PubMed] [Google Scholar]
- Decaluwe V, & Braet C (2003). Prevalence of binge-eating disorder in obese children and adolescents seeking weight-loss treatment. International Journal of Obesity & Related Metabolic Disorders, 27(3), 404. [DOI] [PubMed] [Google Scholar]
- Duke PM, Litt IF, & Gross RT (1980). Adolescents’ self-assessment of sexual maturation. Pediatrics, 66(6), 918–920. [PubMed] [Google Scholar]
- Ebner-Priemer UW, Kuo J, Kleindienst N, Welch SS, Reisch T, Reinhard I, Lieb K, Linehan MM, & Bohus M (2007). State affective instability in borderline personality disorder assessed by ambulatory monitoring. Psychological Medicine, 37(7), 961–970. 10.1017/S0033291706009706 [DOI] [PubMed] [Google Scholar]
- Elliott CA, Tanofsky-Kraff M, Shomaker LB, Columbo KM, Wolkoff LE, Ranzenhofer LM, & Yanovski JA (2010). An examination of the interpersonal model of loss of control eating in children and adolescents. Behaviour Research and Therapy, 48(5), 424–428. 10.1016/j.brat.2009.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert KE (2012). The neglected role of positive emotion in adolescent psychopathology. Clinical Psychology Review, 32(6), 467–481. 10.1016/j.cpr.2012.05.005 [DOI] [PubMed] [Google Scholar]
- Goldschmidt AB (2017). Are loss of control while eating and overeating valid constructs? A critical review of the literature. Obesity Reviews, 18(4), 412–449. 10.1111/obr.12491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB, Crosby RD, Cao L, Engel SG, Durkin N, Beach HM, Berg KC, Wonderlich SA, Crow SJ, & Peterson CB (2014). Ecological momentary assessment of eating episodes in obese adults. Psychosomatic Medicine, 76(9), 747–752. 10.1097/PSY.0000000000000108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB, Smith KE, Crosby RD, Boyd HK, Dougherty E, Engel SG, & Haedt-Matt A (2018). Ecological momentary assessment of maladaptive eating in children and adolescents with overweight or obesity. International Journal of Eating Disorders, 51(6), 549–557. 10.1002/eat.22864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grumbach MM, & Styne DM (2003). Puberty: Ontogeny, Neuroendocrinology, Physiology, and Disorders In Larsen PR, Kronenberg HM, Melmed S, & Polonsky KS (Eds.), Williams textbook of endocrinology (10th ed., pp. 1115–1286). Elsevier. [Google Scholar]
- He J, Cai Z, & Fan X (2017). Prevalence of binge and loss of control eating among children and adolescents with overweight and obesity: An exploratory meta-analysis. International Journal of Eating Disorders, 50(2), 91–103. 10.1002/eat.22661 [DOI] [PubMed] [Google Scholar]
- Heller AS, & Casey B. j. (2016). The neurodynamics of emotion: Delineating typical and atypical emotional processes during adolescence. Developmental Science, 19(1), 3–18. 10.1111/desc.12373 [DOI] [PubMed] [Google Scholar]
- Hilbert A, Hartmann AS, Czaja J, & Schoebi D (2013). Natural course of preadolescent loss of control eating. Journal of Abnormal Psychology, 122(3), 684–693. 10.1037/a0033330 [DOI] [PubMed] [Google Scholar]
- Hilbert A, Rief W, Tuschen-Caffier B, de Zwaan M, & Czaja J (2009). Loss of control eating and psychological maintenance in children: An ecological momentary assessment study. Behaviour Research and Therapy, 47(1), 26–33. 10.1016/j.brat.2008.10.003 [DOI] [PubMed] [Google Scholar]
- Klump KL, Culbert KM, Slane JD, Burt SA, Sisk CL, & Nigg JT (2012). The effects of puberty on genetic risk for disordered eating: Evidence for a sex difference. Psychological Medicine, 42(3), 627–637. 10.1017/S0033291711001541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klump KL, Fowler N, Mayhall L, Sisk CL, Culbert KM, & Burt SA (2018). Estrogen moderates genetic influences on binge eating during puberty: Disruption of normative processes? Journal of Abnormal Psychology, 127(5), 458–470. 10.1037/abn0000352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, & Johnson CL (2000). CDC growth charts: United States. Advance Data, 314, 1–27. [PubMed] [Google Scholar]
- Neumark-Sztainer D, Croll J, Story M, Hannan PJ, French SA, & Perry C (2002). Ethnic/racial differences in weight-related concerns and behaviors among adolescent girls and boys: Findings from Project EAT. Journal of Psychosomatic Research, 53(5), 963–974. 10.1016/S0022-3999(02)00486-5 [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, & Flegal KM (2016). Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA, 315(21), 2292–2299. 10.1001/jama.2016.6361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez M, & Warren CS (2013). Assessing eating pathology in Hispanic Americans In Benuto LT (Ed.), Guide to Psychological Assessment with Hispanics (pp. 201–214). Springer. [Google Scholar]
- Raman A, Lustig RH, Fitch M, & Fleming SE (2011). Accuracy of self-assessed Tanner staging against hormonal assessment of sexual maturation in overweight African-American children. Journal of Pediatric Endocrinology and Metabolism, 22(7), 609–622. 10.1515/JPEM.2009.22.7.609 [DOI] [PubMed] [Google Scholar]
- Ranzenhofer LM, Engel SG, Crosby RD, Anderson M, Vannucci A, Cohen LA, Cassidy O, & Tanofsky-Kraff M (2014). Using ecological momentary assessment to examine interpersonal and affective predictors of loss of control eating in adolescent girls. International Journal of Eating Disorders, 47(7), 748–757. 10.1002/eat.22333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstein D, & Oster H (1988). Differential facial responses to four basic tastes in newborns. Child Development, 59(6), 1555–1568. JSTOR. 10.2307/1130670 [DOI] [PubMed] [Google Scholar]
- Santangelo P, Reinhard I, Mussgay L, Steil R, Sawitzki G, Klein C, Trull TJ, Bohus M, & Ebner-Priemer UW (2014). Specificity of affective instability in patients with borderline personality disorder compared to posttraumatic stress disorder, bulimia nervosa, and healthy controls. Journal of Abnormal Psychology, 123(1), 258–272. 10.1037/a0035619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott CK, Dennis ML, & Gustafson DH (2018). Using ecological momentary assessments to predict relapse after adult substance use treatment. Addictive Behaviors, 82, 72–78. 10.1016/j.addbeh.2018.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby EA, Panza E, & Plasencia M (2019). Positive emotion dysregulation in eating disorders and obesity In Gruber J (Ed.), The Oxford Handbook of Positive Emotion and Psychopathology (pp. 424–443). Oxford University Press. [Google Scholar]
- Silk JS, Siegle GJ, Whalen DJ, Ostapenko LJ, Ladouceur CD, & Dahl RE (2009). Pubertal changes in emotional information processing: Pupillary, behavioral, and subjective evidence during emotional word identification. Development and Psychopathology, 21(1), 7–26. 10.1017/S0954579409000029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snir A, Bar-Kalifa E, Berenson KR, Downey G, & Rafaeli E (2017). Affective instability as a clinical feature of avoidant personality disorder. Personality Disorders, 8(4), 389–395. 10.1037/per0000202 [DOI] [PubMed] [Google Scholar]
- Stice E, Presnell K, & Spangler D (2002). Risk factors for binge eating onset in adolescent girls: A 2-year prospective investigation. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 21(2), 131–138. [PubMed] [Google Scholar]
- Stice E, Yokum S, Burger KS, Epstein LH, & Small DM (2011). Youth at risk for obesity show greater activation of striatal and somatosensory regions to food. Journal of Neuroscience, 31(12), 4360–4366. 10.1523/JNEUROSCI.6604-10.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suisman JL, Thompson JK, Keel PK, Burt SA, Neale M, Boker S, Sisk C, & Klump KL (2014). Genetic and environmental influences on thin-ideal internalization across puberty and preadolescent, adolescent, and young adult development. International Journal of Eating Disorders, 47(7), 773–783. 10.1002/eat.22321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner JM (1962). Growth at adolescence (2nd ed.). Blackwell Scientific Publications. [Google Scholar]
- Tanofsky-Kraff M, Goossens L, Eddy KT, Ringham R, Goldschmidt A, Yanovski SZ, Braet C, Marcus MD, Wilfley DE, Olsen C, & Yanovski JA (2007). A multisite investigation of binge eating behaviors in children and adolescents. Journal of Consulting and Clinical Psychology, 75(6), 901–913. 10.1037/0022-006X.75.6.901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Theim KR, Yanovski SZ, Bassett AM, Burns NP, Ranzenhofer LM, Glasofer DR, & Yanovski JA (2007). Validation of the emotional eating scale adapted for use in children and adolescents (EES-C). International Journal of Eating Disorders, 40(3), 232–240. 10.1002/eat.20362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, & Yanovski JA (2004). Eating-disordered behaviors, body fat, and psychopathology in overweight and normal-weight children. Journal of Consulting and Clinical Psychology, 72(1), 53–61. 10.1037/0022-006X.72.1.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theim KR, Tanofsky-Kraff M, Salaita CG, Haynos AF, Mirch MC, Ranzenhofer LM, Yanovski SZ, Wilfley DE, & Yanovski JA (2007). Children’s descriptions of the foods consumed during loss of control eating episodes. Eating Behaviors, 8(2), 258–265. 10.1016/j.eatbeh.2006.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ, Solhan MB, Tragesser SL, Jahng S, Wood PK, Piasecki TM, & Watson D (2008). Affective instability: Measuring a core feature of borderline personality disorder with ecological momentary assessment. Journal of Abnormal Psychology, 117(3), 647–661. 10.1037/a0012532 [DOI] [PubMed] [Google Scholar]
- Vander Wal JS (2004). Eating and body image concerns among average-weight and obese African American and Hispanic girls. Eating Behaviors, 5(2), 181–187. 10.1016/j.eatbeh.2004.01.007 [DOI] [PubMed] [Google Scholar]
- Watkins B, Frampton I, Lask B, & Bryant-Waugh R (2005). Reliability and validity of the child version of the eating disorder examination: A preliminary investigation. International Journal of Eating Disorders, 38(2), 183–187. 10.1002/eat.20165 [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


